
Part Three
- Nursing care for a heart failure patient
The Definition
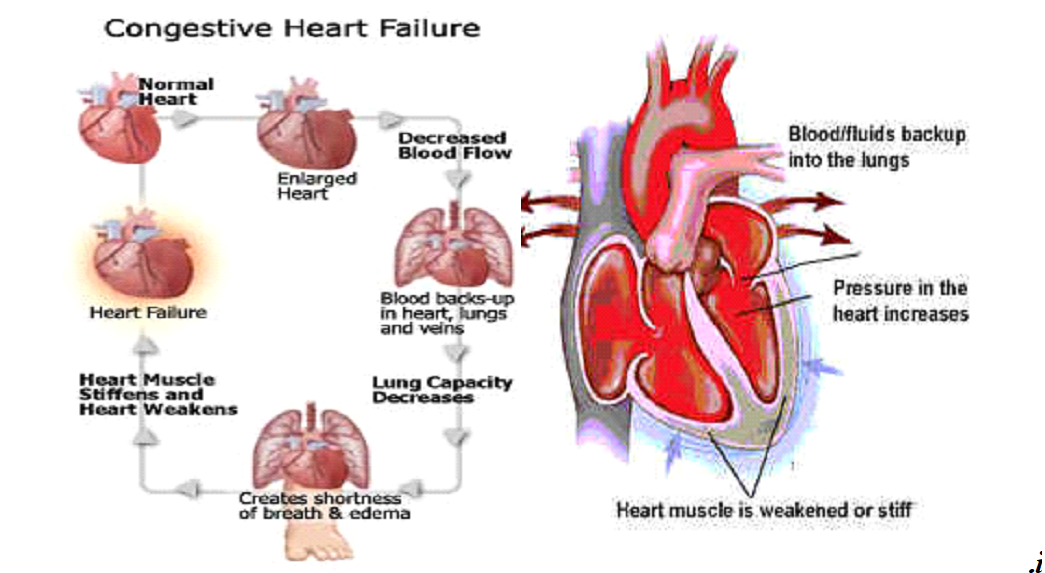
It is a failure of the heart muscle to pump an appropriate amount of blood to meet the body’s need. This decline can either be an acute decline that leads to a sudden stop of the heart muscle pumping blood, which results in blood. Or it can be a chronic decline that occurs gradually and its symptoms are mild. Heart failure is characterized by the occurrence of compensating factors to compensate for the heart failure. like
· Rapid heart rate
· Heart enlargement, especially ventricular hypertrophy
· Ventricular dilatation
· Abnormal amounts of blood accumulate in the respiratory system. Pulmonary congestion
Its causes
Heart failure occurs if one or more mechanical causes combine
1 - The amount of blood supplied to the heart is small as a result of bleeding and dehydration
2 - The amount of blood supplied to the heart exceeds what is necessary due to the large number of solutions
3 - The amount of blood entering the heart is small as a result of narrowing in one of the valves or arteries
4- Injury of any kind to the heart muscle itself
5- Increased nutritional needs of the body as a result of high fever or pregnancy
The goal of heart failure care
The main goal is to eliminate or reduce the causes that lead to the disease
1- Complete physical and muscular rest
2 - DIGITALIS Digoxin
3 - Suitable for a fatty meal, Sodium, Potassium
4- A dilator for arteries and veins
5- Reducing the accumulation of water and sodium inside the body by following the following methods
· a - Sodium in meals
· b - Diuretic
· c - Reducing the amount of fluids entering the body
· d - Reducing stress for the patient
6- Giving the patient oxygen
7- Removal of pleural effusion and peritoneal effusion
8- Tell the patient everything about his illness and how to deal with it
Section Nursing personnel towards illness
1- Place the patient in a quiet, cool room to help him sleep
2- Place all things within the patient’s reach
3- Keep the patient in a comfortable position constantly
4- Trying to reassure the patient about his health
5 - The patient talked about the importance of rest when he returns home
6 - Defining the patient's symptoms of digitalis poisoning
- Nausea - vomiting - diarrhea - headache - depression - tension - dizziness - spasms - hallucinations - memory loss - increased or decreased heart rate - urticaria.
- If any of the above symptoms occur, treatment must be discontinued
- Giving the patient potassium chloride
Must before giving digitalis
1- Taking the patient’s pulse for a full minute with the stethoscope on the patient’s chest
2 - We carefully observe the heart rate if it is regular or irregular and record it
3 - If the patient’s pulse is fast, less than 60 beats per minute, the dose should be stopped and the doctor should be informed.
4 - The patient must be carefully observed for any symptoms of Vitalis poisoning
5-The patient should be given meals rich in potassium
Avoid giving the patient any food that contains sodium salts, such as peanuts or chips
Avoid salt at all
6- Weigh the patient every day at the same time and on the same scale, usually before breakfast
7- Take care of the patient’s skin because swollen skin is more susceptible to cracking
8- Oxygen therapy in case of difficulty breathing
9- An internal and external fluid map must be done
Shock
introduction
The main reason for shock is the lack of sufficient oxygen reaching the tissues, as well as the failure of them to get rid of harmful substances resulting from the metabolic process. Shock also occurs after accidents or injuries as a result of a decrease in blood volume or fluids in the body as a result of bleeding or severe diarrhea, which also leads to a decrease in body volume or As a result of a sudden injury accompanied by severe pain, the shock is divided according to its types into surgical shock and nervous shock. The shock is also divided according to the time of its occurrence into primary shock and bilateral shock.
Shock :
A decrease in the amount of blood that reaches the vital organs in the body, such as (the brain, heart, and kidneys), which leads to depriving the tissues of these organs of a sufficient amount of oxygen and nutrients carried by the blood.
Causes of shock
o The body loses a large amount of blood, as in cases of bleeding
o Acute heart failure
o The body loses a large amount of fluids, as in cases of severe diarrhea
o Severe pain
o Electric shock
o Poisoning and severe allergic reactions
Signs and symptoms of shock
o The affected person has a pale face
o The skin is pale or bluish in color and cool and clammy to the touch
o Increase in respiratory rate and breathing becomes shallow and irregular
o The pulse is fast, weak, or irregular
o Breathing is fast and shallow (the patient tries to take in the largest amount of oxygen from the air, which increases its speed and may be deep but irregular.
o Low blood pressure.
o A drop in temperature below 35 degrees Celsius.
o If you look at the injured person, you will find that he appears anxious and disturbed
o The victim complains of extreme thirst and may become nauseous and vomit
o In the final stages, the injured person loses consciousness
o Dilated pupils
Types of shock:
1- Surgical trauma:
It is a result of the loss of a large amount of blood, as in cases of severe bleeding, whether external, internal, or after operations, or as a result of the loss of a large amount of fluids in the body, which leads to a decrease in blood volume in the blood fraction, such as in cases of severe diarrhea?
2- Nervous shock:
It occurs in cases of severe pain, such as in first-degree burns, or as a result of emotional disturbance such as fear, or severe psychological emotions such as hearing bad news or being exposed to an accident even though there is no physical injury.
3- Initial shock:
It occurs at the time of an accident or sudden illness that is accompanied by severe pain.
4- Secondary trauma:
It may not occur until several hours after the accident or sudden illness, and usually
be dangerous.
Trauma first aid:
The injured person is treated immediately where he is located until he is transferred to the hospital or summoned
Ambulance for him.
1- Calm the patient down, do not move him, and treat any other injuries, such as fractures or wounds.
2- The injured person is placed lying on his back at the scene of the accident with his head on one side to avoid inhaling any secretions coming out of the mouth.
3- If he is in the house, raise the legs of the bed or lift the lower part of the body up so that the blood reaches the brain.
4- Loosen the ties and compressive clothing around the neck, chest and waist of the injured person and prevent crowding around him.
5- If the injured person suffers from injuries in different parts of the body, such as neck or spinal injuries, he must not be moved until he is transferred to prevent complications.
6- Warm the injured person naturally with additional blankets so that sweat secretion and loss of fluids from the body do not increase.
7- Do not give the injured person anything by mouth.
8- Alleviate the injured person’s pain by making him comfortable until he is transferred.
9- Observing the condition of the injured person and taking vital signs regularly until he is transferred to the hospital.
To treat shock, the doctor gives the injured person:
- In case of bleeding blood transfusion
- In case of burns, plasma
- In case of vomiting and diarrhea, Glucose and salt solution
Nursing care for circulatory system patients
The most important general symptoms and signs:
1- Pulse:
There may be a difference in rate, regularity, and strength. The pulse may be faster or slower than the normal rate, irregular, or its strength varies, depending on the case.
2- Breathing:
There may be a change in the rate, regularity, and depth, as well as the occurrence of abnormal sounds accompanying the breathing process. It is common in heart disease to have shortness of breath, especially when moving, or when chest pain occurs.
3- Pressure:
Arterial pressure is one of the important factors that shows the state of blood circulation. It is observed in heart patients a decrease in systolic pressure and an increase in diastolic pressure above the normal rate.
4- Patient’s colour:
There is a change in the color of the patient’s skin. Blueness or dullness may occur in the color, as well as blueness in the lips and nails. This condition appears as a result of a lack of oxygen in the bloodstream, which leads to a change in the color of the skin, lips and nails. The lack of oxygen may also affect mental and physical efficiency, causing dullness or dullness. Loss of feeling.
5- Chest pain:
It is noted that the occurrence of chest pain varies in type, severity, location, and cause of its occurrence from one case to another. The pain may occur when the patient exerts any effort or while resting. In some cases, the pain appears in the abdomen or stomach, and the pain may spread to the shoulder, arm, left or right hand.
6- Tumor:
It usually appears in the lower extremities, especially the feet, as a result of fluid accumulation. In some severe cases, it appears in the abdomen (ascites), which is a distinctive sign that there is pressure in the work of the heart.
7- Feeling the heartbeat:
The patient may feel and be alert to his heartbeat as a result of the change in heart function caused by the disease.
8- Cough:
The patient may develop a cough that may be wet and accompanied by a mucus secretion interspersed with air bubbles, or accompanied by blood in late cases of the disease.
The role of nurses in preventing heart disease:
1- Discovering cases among individuals who frequent it by noticing symptoms and signs of heart disease such as shortness of breath, cyanosis, swelling or swollen veins, and chest pain upon exertion.
2- Educating individuals to prevent disease by helping them form healthy habits, whether children or adults, through:
- Encouraging sports and physical activity, especially walking.
- Annual medical examination.
- Reducing the percentage of fats in food.
- Not smoking due to the high incidence of heart disease among smokers.
1- Providing the necessary care for patients, especially conditions that affect the heart, such as rheumatic fever, high blood pressure, and obesity.
2- Helping heart patients live with their disease by advising them on how to prevent the occurrence of problems or complications that may lead to heart failure, and how to organize their lives, activity, and diet, and advising them to observe moderation in work, exercise, rest, and entertainment, and to avoid mixing with infectious disease patients due to their weak resistance to disease.
3- Activate blood circulation to prevent clots by moving the lower extremities and encouraging the patient to do gradual exercises as soon as the patient’s condition allows for this.
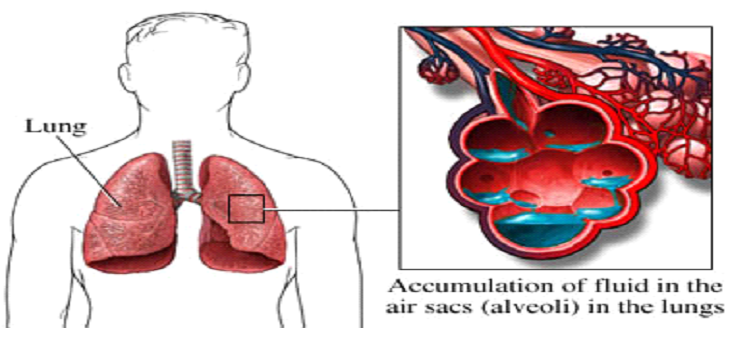
Pulmonary infiltration:
The Definition:
Pulmonary infiltration is lung congestion as a result of an increase in the amount of blood in the blood vessels in the respiratory system, which leads to great difficulty in breathing. This infiltration often occurs as a result of failure of the left part of the heart, which results in difficulty in the return of blood from the respiratory system to the heart, leading to blood accumulation in the lung. It leads to pulmonary infiltration, which leads to the end of the patient's life due to suffocation
Symptoms
◾ Severe difficulty breathing, especially in the horizontal position
◾ Paleness in the face
◾ Increased heart rate
◾ Secretion of large amounts of phlegm mixed with blood
◾ Blueness
The primary goal of our care for this patient is to help the patient take the amount of oxygen he needs
This is done with my machines
1 - The patient sleeps at an angle of 90 or 45 degrees or sits in a chair because this position facilitates the patient’s breathing process
2- Providing the patient with 8 liters of humidified oxygen
3- Giving the patient digoxin
4- Giving the patient a diuretic such as Lasix 40 gm to 120 ml intravenously slowly
5- Giving aminophylline 250 to 500 volume to dilate the bronchi
6- Sometimes the patient needs a respirator to save his life
