Part Three
| Site: | EHC | Egyptian Health Council |
| Course: | Procedural work guide for the renal unit |
| Book: | Part Three |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 5:24 PM |
Table of contents
- - Standard procedures for infection control within the dialysis unit
- - Cardiopulmonary resuscitation
- - Nursing evaluation
- - Vital Signs
- - Installing a catheter and drawing blood
- - Method of giving treatment
- - Oxygen therapy
- - Giving the patient an electric shock
- - Normal heart drawing
- - Anatomy of the circulatory system
- - Nursing care for angina patients
- - Nursing care for a heart attack patient
- - Nursing care for a heart failure patient
- - Nursing care for an unconscious patient
- - Physiological anatomy of the urinary system
- - Nursing care for patients with kidney failure
- - Kidney transplantation
- - Conducting patient reception and catheterization
- - Procedures for starting a hemodialysis session
- - Taking care of the hemodialysis machine
- - Medical terminology
- - Abbreviations
- Standard procedures for infection control within the dialysis unit
introduction:
◾ The dialysis process is performed by two basic methods: hemodialysis and peritoneal dialysis.
◾ The dialysis process entails some risks for the patient, as penetration into his blood vessels and the introduction of foreign bodies into his body may lead to an increase in the possibility of infection. This is due to the fact that the process requires dealing with naturally sterile places, such as the vascular system or the peritoneal cavity, and infection may occur due to contamination that may occur. In the procedures of various dialysis sessions, or the reason for this is the presence of contamination in any of the components of the dialysis system.
◾ The patient may also be exposed to infection with microbes or poisoning resulting from contamination of the water used to prepare for the dialysis process. The person caring for the patient may, by virtue of his profession, be exposed to infection with microbes present in the patient’s blood, as dialysis patients have an increased prevalence of blood-transmitted diseases.
◾ Infection and side effects may result from non-compliance with infection control procedures. Transmission of infection through contact is considered one of the most important ways by which microbes are transmitted in dialysis units. The process of transmission of infection from one patient to another is determined by the hands of the health care provider, where the health care provider By dealing with patients and touching the environment around them and the surfaces of dialysis machines, then the infection can be transmitted from one patient to another. The risk of infection or the occurrence of side effects in the dialysis unit can be reduced by strictly adhering to infection control recommendations, as well as by performing maintenance on the equipment used in the units and monitoring. Details of all procedures that may lead to bacterial or chemical contamination inside dialysis units.
◾ The most common types of infections associated with the dialysis process
◾ Infection with blood-borne microbes (such as human immunodeficiency virus - hepatitis B and C viruses)
◾ Bacteremia
◾ Peritonitis
◾ Infection of the site of entry into the body (the site of entry into the organ system or into the peritoneal cavity
First: blood dialysis
◾ Hemodialysis helps in getting rid of toxins, ionized mineral salts, and fluids by circulating the patient’s blood through hemodialysis (artificial kidney). The main components of the hemodialysis process are a venous-arterial connection, a system for treating water, another for distributing it, and dialysis solution ( To purify blood and its components), washing machines, and blood passage tubes (filters and connectors).
◾ Entry ports into the patient’s vascular system
◾ Access to the vascular system is achieved through some means, such as making external arteriovenous shunts, or internal arteriovenous fistula, or arteriovenous fistula using surgical grafting of blood vessels, or other temporary devices such as using a central venous catheter through the jugular vein.
◾ (Jugular vein), or subclavian vein.
Infection control measures during hemodialysis sessions
◾ Procedures for connecting the patient to the dialysis machine via the arteriovenous fistula connection and separation procedures Infection control recommendations are followed when connecting the patient to dialysis machines or a dialysis machine, taking into account the following:
◾ Wash hands or rub them with alcohol before the procedure.
◾ Wear appropriate personal protection (clean gloves - single-use plastic apron), and other tools may be required (such as eye protection - surgical mask) according to the risk assessment before the procedure.
◾ Use sterile cotton or gauze when connecting or disconnecting.
◾ Disinfect the insertion site before connection and after separation with an appropriate antiseptic (such as povidone-iodine 10% iodophore) taking into account the contact time.
◾ Follow the anti-contamination method when connecting or disconnecting the patient to the dialysis machine.
◾ Pressure is applied to the site of the fistula after separation and it is covered with sterile gauze. Then the medical tape is placed over the sterile bandage. It is not allowed to place the tape directly over the fistula.
◾ Take off personal protective equipment after completing the procedure, then wash your hands.
◾ Procedures for connecting the patient to the dialysis machine via a central venous catheter and separation procedures
◾ Wash hands hygienically or rub them with alcohol before the procedure.
◾ Wear appropriate personal protective equipment (such as sterile gloves - single-use plastic apron) before the procedure.
◾ Use sterile cotton or gauze when connecting or disconnecting.
◾ Disinfect the insertion site of the central venous catheter using sterile gauze saturated with an alcohol solution (60-95%) before connection and after disconnection, taking into account the contact time.
◾ Follow the anti-contamination method when dealing with the central venous catheter when connecting the patient to the dialysis machine or disconnecting it.
◾ The entry site of the central venous catheter is covered with sterile gauze, then the medical tape is placed over the sterile bandage. The tape is not allowed to be placed directly over the catheter.
◾ Take off personal protective equipment after completing the procedure and washing hands
Second: Washing using a peritoneum membrane
◾ Peritoneal dialysis removes toxic substances, mineral salts, and ions by spreading through the peritoneal membrane. Peritoneal dialysis requires placing a catheter in the abdominal area that reaches the peritoneal cavity, where the dialysis solution is inserted and then drained from that place successively.
◾ The main components of peritoneal dialysis include the following:
◾ Inserting a catheter into the peritoneal cavity, which can be placed without surgery or through a surgical cut.
◾ The solution is a solution available for commercial use, in glass containers, polyvinyl bags, or washing operations.
◾ Determine and organize the process of introducing the solution into the peritoneal cavity and dispensing it using a precise schedule and system for the number of hours of the dialysis process.
◾ Dispose of the patient’s fluid in the sewer.
Second: Washing using a peritoneum membrane
◾ Peritoneal dialysis removes toxic substances, mineral salts, and ions by spreading through the peritoneal membrane. Peritoneal dialysis requires placing a catheter in the abdominal area that reaches the peritoneal cavity, where the dialysis solution is inserted and then drained from that place successively.
◾ The main components of peritoneal dialysis include the following:
◾ Inserting a catheter into the peritoneal cavity, which can be placed without surgery or through a surgical cut.
◾ The solution is a solution available for commercial use, in glass containers, polyvinyl bags, or washing operations.
◾ Determine and organize the process of introducing the solution into the peritoneal cavity and dispensing it using a precise schedule and system for the number of hours of the dialysis process.
◾ Dispose of the patient’s fluid in the sewer.
|
Notice |
|
◾ There are three types of infections that may result from peritoneal dialysis, such as catheter site infection, subcutaneous catheter tract infection, or peritonitis. ◾ The sources of infection are the patient’s skin, the washing solution, or the health service provider. ◾ The cause of infection related to the catheter is due to the way it is installed and cared for. |
Precautions that must be followed when performing peritoneal dialysis:
· An anti-contamination method must be followed during the installation and connection of the peritoneal dialysis catheter, as well as during the procedures for changing the dialysis solution.
· Sterile gloves are worn while installing the peritoneal dialysis catheter and when handling it.
· A surgical mask is used during connection and separation procedures to reduce the risk of infection with Staphylococcus bacteria (Staph. Aureus) transmitted through the nose.
· The external site of the catheter should be kept clean and dry.
· The catheter should be well secured in a way that reduces the chances of it being removed spontaneously and causing wounds to the surrounding skin area.
· The patient should be made aware of the appropriate methods for caring for the external site of the catheter in the event of continuous frequent washing outside the hospital, and patients and staff should monitor early signs of infection if they occur.
Procedures to control the transmission of infection to patients and the health team in dialysis units:
· It is necessary to wash hands, disinfect them, or rub them with alcohol if they are apparently clean, before dealing with it.
· Workers in dialysis units must wear appropriate personal protection to prevent their exposure to blood when blood spills or spray occur as a result of a cut or rupture in the dialysis connections or dialysis filter membranes, as this occurs in the event of increased pressure inside these connections.
· Clean, single-use gloves must be used before performing any procedure that does not penetrate the body’s natural defenses, and when dealing with various surfaces and tools, including the dialysis machine. These gloves can be used to connect the patient to the dialysis machine, with the need to adhere to the non-touch method.
· Sterile gloves must be used when installing a central venous device or installing a peritoneal dialysis catheter.
· A member of the health team is allocated to transfer supplies from the warehouses to a central place in the dialysis halls. This member does not deal with patients during dialysis sessions.
· The central place is not handled by the person in charge of the process of connecting or disconnecting the patient to the dialysis machine, but rather through the handling nursing staff.
· In the event that nursing staff members are not available to handle them, the nursing staff prepares the delivery or separation supplies for one patient only immediately before the procedure and does not leave any supplies on the machines during the washing sessions.
· All tools used in dialysis that were handled once or were taken to a specific patient’s station must be disposed of immediately after use. (If it is intended for use again) or clean, disinfect or sterilize it before reusing it again or before storing it (if it is multi-use).
· A separate place must be allocated to install central venous catheters for patients outside the dialysis room.
· A set of sterile supplies and tools must be prepared for each patient when connecting via central venous catheters.
· Heparin must be prepared immediately before using it for the patient, and an anti-contamination method must be followed when giving it to the patient during a dialysis session.
· Patients should be instructed on the correct way to care for the insertion site of dialysis catheters.
Kidney dialysis machines
· Blood pump: The blood pump consists of two or more cylinders, and the patient’s blood is pumped through a group of tubes and a dialysis machine at constant and accurate flow rates.
· Liquid passages inside the washing machine:
There are three types of dialysis machines, which are as follows:
· Recycling machines
· These machines recycle the washing solution continuously through the washing machine during the dialysis process.
· Single-pass recycling machines:
· These machines continuously recycle the solution through the washing machine during the dialysis process, and with a continuous flow of new solution, the washing solution is partially replaced.
· Single-pass machines
· Single-pass machines produce a continuous flow of washing solution, which passes through the machine and is then disposed of without being recycled.
Recommendations
· It is preferable to use single-pass machines, as the internal fluid passages of these machines are not exposed to blood contamination unless a blood leak occurs in the single-pass machine. Contamination of single-pass machines is usually due to how well the water or other components of the solution used in washing are treated.
· Blood tubes:
To avoid blood contamination with bacteria and contamination of blood tubes, the following procedures should be followed:
· Keep intravenous tubes away from the waste container during the process of preparing the dialysis machine.
· Hands should always be washed after handling waste.
· Disinfect containers designated for disposal of waste resulting from the filtration process daily.
· Cleaning and disinfecting the outside of dialysis machines.
· Disinfecting the internal and external pipes for the washing solution.
Cleaning and disinfecting dialysis machines
· The external surfaces of the machine must be cleaned and disinfected after each patient.
· The internal and external pipes for the washing solution must be disinfected.
· The manufacturer’s instructions must be followed, provided that they are written.
· Carry out rinsing and disinfection procedures for the single-pass machine at the beginning and end of the day or according to the manufacturer’s instructions.
· For recycling machines (currently rarely used), rinsing and disinfection procedures are carried out between one patient and another.
· The same cleaning and disinfection methods are followed if blood leakage does not occur, regardless of the type of dialysis machine used.
· You must follow the instructions of the manufacturer of the disinfectant used to disinfect the dialysis machine.
· Cleanliness of the environment in the dialysis unit
· Policies and protocols must be written for cleaning and disinfecting surfaces and equipment in the dialysis unit, including careful cleaning before carrying out any disinfection process.
· The patient’s station must be cleaned and disinfected after the dialysis session, including the dialysis bed, various nearby surfaces, dialysis solution containers, and waste containers.
· Covers and bedsheets must be changed between each patient.
· The hazardous waste bag should be disposed of immediately at each session.
· Spills of blood and other fluids should be dealt with immediately when they occur.
· The rest of the standard infection control procedures regarding environmental cleanliness are followed.
· Monitoring the quality of water used in the dialysis process
· A work crew must be appointed to be responsible for the initial and routine control of the water used to perform the dialysis process. The members of this crew must be fully aware of the various aspects related to water treatment and distribution systems, and they must have the authority to investigate problems related to the quality of the water used in The dialysis process and working to solve these problems.
· The specifications of the water used in the dialysis machine must conform to the standards of the Ministry of Health stipulated in Ministerial Resolution No. 63 of 1996 and its amendments. Microbiological and chemical monitoring of the water must be carried out at least once a month in accordance with this ministerial decision.
Microbiological monitoring:
· Microbiological monitoring of treated water must be carried out at least once a month, and the number of times may increase if any problems are proven.
· Samples of water used in dialysis must be collected at the point where the water reaches the machine.
· Water samples used in dialysis must be collected during or after the end of the dialysis process.
· The total numbers of live bacteria present in the water used for dialysis must not exceed 200 bacterial colony units per milliliter. The total numbers of live bacteria present in the dialysis solution must not exceed 200 bacterial colony units per milliliter.
· The presence of coliforms and Escherichia coli (E. Coli) is not allowed in the water of dialysis units.
· The presence of Pseudomonas bacteria, Enterococcus 'Streptococcus' faecalis, and Anaerobic Sulfur Reducing Bacteria is not permitted in the water of dialysis units.
Kidney dialysis machines
· Blood pump: The blood pump consists of two or more cylinders, and the patient’s blood is pumped through a group of tubes and a dialysis machine at constant and accurate flow rates.
· Liquid passages inside the washing machine:
There are three types of dialysis machines, which are as follows:
· Recycling machines
· These machines recycle the washing solution continuously through the washing machine during the dialysis process.
· Single-pass recycling machines:
· These machines continuously recycle the solution through the washing machine during the dialysis process, and with a continuous flow of new solution, the washing solution is partially replaced.
· Single-pass machines
· Single-pass machines produce a continuous flow of washing solution, which passes through the machine and is then disposed of without being recycled.
Recommendations
· It is preferable to use single-pass machines, as the internal fluid passages of these machines are not exposed to blood contamination unless a blood leak occurs in the single-pass machine. Contamination of single-pass machines is usually due to how well the water or other components of the solution used in washing are treated.
· Blood tubes:
To avoid blood contamination with bacteria and contamination of blood tubes, the following procedures should be followed:
· Keep intravenous tubes away from the waste container during the process of preparing the dialysis machine.
· Hands should always be washed after handling waste.
· Disinfect containers designated for disposal of waste resulting from the filtration process daily.
· Cleaning and disinfecting the outside of dialysis machines.
· Disinfecting the internal and external pipes for the washing solution.
Cleaning and disinfecting dialysis machines
· The external surfaces of the machine must be cleaned and disinfected after each patient.
· The internal and external pipes for the washing solution must be disinfected.
· The manufacturer’s instructions must be followed, provided that they are written.
· Carry out rinsing and disinfection procedures for the single-pass machine at the beginning and end of the day or according to the manufacturer’s instructions.
· For recycling machines (currently rarely used), rinsing and disinfection procedures are carried out between one patient and another.
· The same cleaning and disinfection methods are followed if blood leakage does not occur, regardless of the type of dialysis machine used.
· You must follow the instructions of the manufacturer of the disinfectant used to disinfect the dialysis machine.
· Cleanliness of the environment in the dialysis unit
· Policies and protocols must be written for cleaning and disinfecting surfaces and equipment in the dialysis unit, including careful cleaning before carrying out any disinfection process.
· The patient’s station must be cleaned and disinfected after the dialysis session, including the dialysis bed, various nearby surfaces, dialysis solution containers, and waste containers.
· Covers and bedsheets must be changed between each patient.
· The hazardous waste bag should be disposed of immediately at each session.
· Spills of blood and other fluids should be dealt with immediately when they occur.
· The rest of the standard infection control procedures regarding environmental cleanliness are followed.
· Monitoring the quality of water used in the dialysis process
· A work crew must be appointed to be responsible for the initial and routine control of the water used to perform the dialysis process. The members of this crew must be fully aware of the various aspects related to water treatment and distribution systems, and they must have the authority to investigate problems related to the quality of the water used in The dialysis process and working to solve these problems.
· The specifications of the water used in the dialysis machine must conform to the standards of the Ministry of Health stipulated in Ministerial Resolution No. 63 of 1996 and its amendments. Microbiological and chemical monitoring of the water must be carried out at least once a month in accordance with this ministerial decision.
Microbiological monitoring:
· Microbiological monitoring of treated water must be carried out at least once a month, and the number of times may increase if any problems are proven.
· Samples of water used in dialysis must be collected at the point where the water reaches the machine.
· Water samples used in dialysis must be collected during or after the end of the dialysis process.
· The total numbers of live bacteria present in the water used for dialysis must not exceed 200 bacterial colony units per milliliter. The total numbers of live bacteria present in the dialysis solution must not exceed 200 bacterial colony units per milliliter.
· The presence of coliforms and Escherichia coli (E. Coli) is not allowed in the water of dialysis units.
· The presence of Pseudomonas bacteria, Enterococcus 'Streptococcus' faecalis, and Anaerobic Sulfur Reducing Bacteria is not permitted in the water of dialysis units.
Note:
· Immediate corrective action must be initiated to reduce bacterial contaminants if the total numbers of live bacteria present in the water used in the dialysis solution or in the dialysis solution exceed 0.5 bacterial colony units per milliliter.
· Treating the water used in the dialysis process
· The water used in the dialysis unit must be treated in order to get rid of chemical compounds, pollutants and bacterial toxins so as not to harm the patient. When water is purified from chlorine during the water treatment process to be used in the dialysis process, it is more likely to grow in bacteria. Therefore, care and care must be taken at every stage of the water treatment process to reduce the risk of bacteria penetrating the system or allowing the treated water to remain stagnant.
The processing units used consist of several stages
1) Carbon filters:
◾ It works to get rid of chlorine, chloramines, and organic materials present in drinking water, as it allows residual free chlorine in the unit’s water up to (2.0) and chloramine up to (1.0).
◾ These filters are exposed to bacterial contamination.
◾ Two carbon filters must be placed in succession to increase their effectiveness and to avoid system malfunction.
◾ When carbon filters break down, they must be replaced and not repaired to avoid the risk of pollution.
2) Molecular filters:
◾ Molecular filters are used to purify water from sediments. Bacteria may grow in these filters, causing harm to the patient and leading to fever. Therefore, these filters must be changed and disinfected in accordance with the manufacturer’s recommendations.
3) Reverse osmosis filter:
◾ Osmotic difference (reverse osmosis) and hydrostatic pressure difference on both sides of the semi-permeable membrane are used to eliminate organic and ionic compounds.
◾ Reverse osmosis filters are capable of eliminating 90% - 99% of bacteria, viruses, toxins, metals and ions.
4) Ion removal devices:
◾ These devices contain surfaces to remove ions from water, as they work to get rid of positively charged ions and negatively charged ions by attaching them to those surfaces and releasing hydrogen and hydroxide ions.
◾ Deionizing devices do not eliminate bacteria and toxins, and may contribute to significant bacterial growth.
5) Regular filters, ultra filters and ultraviolet rays:
◾ These filters work to reduce bacterial or toxic pollution to the maximum extent possible. Ultraviolet rays may be ineffective in eliminating some types of bacteria, and they do not work to get rid of toxins.
Note
◾ All filters must be changed and disinfected according to the manufacturer’s recommendations.
◾ Take into account the follow-up of the results of the analyzes of the departmental water unit and their conformity with Ministerial Resolution No. 3 6 of 1996 and its amendments regarding the percentages allowed for
◾Bacteriological examination of the water of dialysis units.
Water distribution and storage
◾ Water is distributed after treatment in plastic pipes, as pipes made of metal lead to contamination of the treated water with chemicals such as copper, lead, and zinc.
◾ Use the least possible number of curved connections (angles).
◾ The outlets must be at the highest point in the system to allow sufficient contact of all parts of the system with disinfectants.
◾ It is preferable not to use tanks to store water as much as possible because stored water is susceptible to bacterial contamination, and when using a tank take care of the following:
◾ Make the tank as small as possible.
◾ It must be designed to accommodate continuous flow without any places allowing water to stagnate.
◾ Use a tightly closed lid.
◾ To be cleaned, disinfected, and rinsed easily.
◾ All tanks and all pipes must be disinfected, including the water lines connecting to the washing machines (to prevent bacterial growth).
Note
◾ Problems that arise from the lack of microbiological conformity of water samples in dialysis units:
◾ 1- The presence of Gram-negative bacteria:
◾ Bacteria in the blood and reactions occur that lead to shivering - fever - low blood pressure - headache - muscle weakness - nausea - vomiting.
◾ 2- The presence of bacterial toxins:
◾ Fever - chills - multi-organ injury that may lead to death.
Dealing with waste from dialysis units
◾ All disposable items should be placed in bags thick enough to prevent leakage. It is possible that the waste resulting from the dialysis unit may be contaminated with blood, so it should be dealt with accordingly.
◾ Room cleaning staff members in the dialysis unit should remove waste after each session.
◾ Sharp tools are disposed of immediately after use in their safety containers. There must be a container near each patient service area
◾ Workers in dialysis units
◾ The necessary training and guidance must be provided to people who are exposed to infection by virtue of their work on a regular basis. The necessary training and guidance must also be provided to new employees before they take up work in dialysis units.
◾ All workers in dialysis units must be vaccinated against hepatitis B.
◾ Employees must wear appropriate personal protective equipment.
◾ Staff members should not consume food or drinks in the area designated for dialysis.
◾ It is not recommended to take any special measures or impose any restrictions on the work of health service providers infected with one of the blood-borne microbes (hepatitis B and C viruses and human immunodeficiency virus (HIV).
Environmental factors and design of dialysis units
◾ Basic principles of design
◾ Providing a suitable space away from the patient service area to store clean and sterile materials.
◾ Allocate halls or rooms for dialysis for patients infected with hepatitis B virus, away from the rest of the patients, and allocate a work team to deal with them during the dialysis period (so that they do not provide service to the rest of the patients during the same shift period), provided that the requirements for the dialysis process are These patients and all the necessary procedures for them are separate from those intended for other patients.
◾ Allocate halls or rooms for dialysis for patients infected with hepatitis C virus, away from the rest of the patients, and allocate a work team to deal with them during the dialysis period (so that they do not provide service to the rest of the patients during the same shift period), provided that the requirements for the dialysis process are For these patients, all the necessary equipment for them is separate from that for other patients.
◾ In the event that there are halls or rooms for patients positive for the human immunodeficiency virus (HIV), special machines for dialysis must be allocated for them away from the rest of the patients, with a work team allocated to deal with them during the dialysis period (so that they do not provide service to the rest of the patients during the same dialysis period). Provided that the requirements for the dialysis process for these patients and all the necessary equipment for them are separate from those designated for other patients.
◾ A warehouse is allocated for all water treatment equipment and filters.
◾ A warehouse is allocated for dialysis solution containers.
◾ A place is allocated for the temporary storage of hazardous medical waste, as well as a place for storing contaminated sheets and furnishings until transport.
◾ Records that must be available in the dialysis unit
◾ A compiled record of the number and names of all dialysis patients in the unit annually.
◾ A special record for all dialysis machines in the unit, including: their types/dates they entered service/date of maintenance/emergency events for each machine. A special record for each patient containing, medical history/date of the start of dialysis sessions in the unit, pre-serological analysis of the start of dialysis in the unit, results of special serological and chemical analyses. Patient, dialysis machine number, blood transfusions, days and duration of dialysis sessions.
◾ A comprehensive record of the results of serological tests for all patients in Oujda.
◾ A combined record of blood transfusions for all patients in the unit.
◾ A special record of the results of chemical analyzes for all patients in the unit.
◾ A special record of emergency events that occur in the unit, including machine failure/
◾ Blood leakage during dialysis sessions / malfunction of dialysis filters.
◾ A record of water sample collection as well as analysis results.
◾ A record of the unit’s water treatment plant maintenance and filter change dates.
◾ A special record of the names of the unit’s health team, along with the results of their departmental serological tests and their vaccinations.
◾ A record of patients’ vaccinations against hepatitis B.
◾ A special record to investigate outbreaks of blood-borne infections or bacterial and viral infections that occur in the unit.
◾ Guidance regarding patient care
◾ Dialysis requires awareness from the patient to reduce the risk of diseases that may be caused by infections
◾ It may also result in death, and there are steps that must be taken to educate the patient, including:
◾ Educate patients on the necessity of keeping the entry site of dialysis catheters clean and dry at all times, and the importance of personal hygiene for the patient and its relationship to entry site infection should be emphasized.
◾ Educating patients about the proper way to care for the insertion site of dialysis catheters and the need for them to be aware of the symptoms and signs of infection and to report them immediately. These symptoms include fever, feeling cold, shivering, pain, redness, or the appearance of an ooze around the site.
◾ Patients are allowed to eat meals during the dialysis procedure.
Note
◾ Problems that arise from the lack of microbiological conformity of water samples in dialysis units:
◾ 1- The presence of Gram-negative bacteria:
◾ Bacteria in the blood and reactions occur that lead to shivering - fever - low blood pressure - headache - muscle weakness - nausea - vomiting.
◾ 2- The presence of bacterial toxins:
◾ Fever - chills - multi-organ injury that may lead to death.
Dealing with waste from dialysis units
◾ All disposable items should be placed in bags thick enough to prevent leakage. It is possible that the waste resulting from the dialysis unit may be contaminated with blood, so it should be dealt with accordingly.
◾ Room cleaning staff members in the dialysis unit should remove waste after each session.
◾ Sharp tools are disposed of immediately after use in their safety containers. There must be a container near each patient service area
◾ Workers in dialysis units
◾ The necessary training and guidance must be provided to people who are exposed to infection by virtue of their work on a regular basis. The necessary training and guidance must also be provided to new employees before they take up work in dialysis units.
◾ All workers in dialysis units must be vaccinated against hepatitis B.
◾ Employees must wear appropriate personal protective equipment.
◾ Staff members should not consume food or drinks in the area designated for dialysis.
◾ It is not recommended to take any special measures or impose any restrictions on the work of health service providers infected with one of the blood-borne microbes (hepatitis B and C viruses and human immunodeficiency virus (HIV).
Environmental factors and design of dialysis units
◾ Basic principles of design
◾ Providing a suitable space away from the patient service area to store clean and sterile materials.
◾ Allocate halls or rooms for dialysis for patients infected with hepatitis B virus, away from the rest of the patients, and allocate a work team to deal with them during the dialysis period (so that they do not provide service to the rest of the patients during the same shift period), provided that the requirements for the dialysis process are These patients and all the necessary procedures for them are separate from those intended for other patients.
◾ Allocate halls or rooms for dialysis for patients infected with hepatitis C virus, away from the rest of the patients, and allocate a work team to deal with them during the dialysis period (so that they do not provide service to the rest of the patients during the same shift period), provided that the requirements for the dialysis process are For these patients, all the necessary equipment for them is separate from that for other patients.
◾ In the event that there are halls or rooms for patients positive for the human immunodeficiency virus (HIV), special machines for dialysis must be allocated for them away from the rest of the patients, with a work team allocated to deal with them during the dialysis period (so that they do not provide service to the rest of the patients during the same dialysis period). Provided that the requirements for the dialysis process for these patients and all the necessary equipment for them are separate from those designated for other patients.
◾ A warehouse is allocated for all water treatment equipment and filters.
◾ A warehouse is allocated for dialysis solution containers.
◾ A place is allocated for the temporary storage of hazardous medical waste, as well as a place for storing contaminated sheets and furnishings until transport.
◾ Records that must be available in the dialysis unit
◾ A compiled record of the number and names of all dialysis patients in the unit annually.
◾ A special record for all dialysis machines in the unit, including: their types/dates they entered service/date of maintenance/emergency events for each machine. A special record for each patient containing, medical history/date of the start of dialysis sessions in the unit, pre-serological analysis of the start of dialysis in the unit, results of special serological and chemical analyses. Patient, dialysis machine number, blood transfusions, days and duration of dialysis sessions.
◾ A comprehensive record of the results of serological tests for all patients in Oujda.
◾ A combined record of blood transfusions for all patients in the unit.
◾ A special record of the results of chemical analyzes for all patients in the unit.
◾ A special record of emergency events that occur in the unit, including machine failure/
◾ Blood leakage during dialysis sessions / malfunction of dialysis filters.
◾ A record of water sample collection as well as analysis results.
◾ A record of the unit’s water treatment plant maintenance and filter change dates.
◾ A special record of the names of the unit’s health team, along with the results of their departmental serological tests and their vaccinations.
◾ A record of patients’ vaccinations against hepatitis B.
◾ A special record to investigate outbreaks of blood-borne infections or bacterial and viral infections that occur in the unit.
◾ Guidance regarding patient care
◾ Dialysis requires awareness from the patient to reduce the risk of diseases that may be caused by infections
◾ It may also result in death, and there are steps that must be taken to educate the patient, including:
◾ Educate patients on the necessity of keeping the entry site of dialysis catheters clean and dry at all times, and the importance of personal hygiene for the patient and its relationship to entry site infection should be emphasized.
◾ Educating patients about the proper way to care for the insertion site of dialysis catheters and the need for them to be aware of the symptoms and signs of infection and to report them immediately. These symptoms include fever, feeling cold, shivering, pain, redness, or the appearance of an ooze around the site.
◾ Patients are allowed to eat meals during the dialysis procedure.
Measures to control the transmission of hepatitis B virus infection
◾ The following must be followed to prevent the transmission of hepatitis B virus among patients undergoing dialysis:
◾ Vaccinating patients against this disease.
◾ Commitment to applying standard infection control precautions to all patients undergoing dialysis.
◾ Regular serological examination every 3 months for 'surface' antibodies to hepatitis B virus (HBsAg) and rapid review of the examination results.
◾ The following must be taken into account when positive seroconversion to 'surface' antibodies to hepatitis B virus (HBsAg) occurs:
◾ Reviewing the results of departmental laboratory tests for patients to identify new cases.
◾ Patients are re-tested for hepatitis B virus 'surface' antibodies (HBsAg).
◾ Isolation of positive cases.
◾ Investigate the sources and causes of possible infection to determine whether it has been transmitted inside or outside the dialysis unit, and also review the methods and procedures used in the dialysis unit.
◾ Patients are retested for “surface” antibodies to hepatitis B virus (HBsAg) after three months, along with antibody tests (Anti-HBs) to determine the need for medical consultation and evaluation.
Insulation
◾ A separate area is allocated for the treatment of patients positive for 'surface' antibodies to hepatitis B virus (HBsAg).
◾ Allocate machines, instruments, tools, supplies and medicines for these patients.
◾ Health teams are allocated to deal with dialysis patients infected with hepatitis B virus during dialysis sessions.
◾ Patients with chronic viral infection from hepatitis viruses can transmit the infection to others, in addition to the fact that these patients are more vulnerable to infection with other chronic liver diseases, and they are advised regarding ways to prevent transmission of the infection to others or members of their families and spouses, and the necessity of vaccinating the aforementioned against hepatitis. Hepatitis B virus, and the presence or development of chronic liver disease must be assessed in accordance with the guidelines followed in medical practices (this is done through medical consultation or referring the case to a specialist doctor when necessary).
Vaccination
◾ Hemodialysis patients, as well as the health team in dialysis units, should be vaccinated with the hepatitis B vaccine. This vaccination is done by injection into the deltoid muscle only, with a series of vaccinations as follows: The first dose is given, a month later the second dose is given, and the third dose is given. Six months after the first dose.
◾ Since the immune response in patients with kidney failure is weaker than that in healthy people, they are vaccinated with a double dose of the vaccine or with the dose specified by the manufacturer. They are also given a booster dose every 5 years or if the concentration of antibodies in the blood reaches less than 1 milliliter IU. / Boredom at any time0
Measures to combat the transmission of hepatitis C virus infection
◾ Transmission of the hepatitis C virus can be prevented in dialysis units by strictly adhering to standard infection control precautions with all dialysis patients. Patients infected with the hepatitis C virus must be isolated from the rest of the patients, and departmental tests for antibodies to the hepatitis C virus must be performed. Hepatitis C every 3 months, to monitor the spread of the virus within the units and ensure that precautions are implemented in an appropriate and permanent manner.
◾ When a positive seroconversion occurs for antibodies to hepatitis C virus, the following should be taken into account:
◾ Reviewing the results of departmental laboratory tests every 3 months, which were conducted for all other patients and the health team, in order to determine whether there are additional cases.
◾ Isolation of positive cases.
◾ Investigate possible sources and causes of infection to determine whether it has been transmitted inside or outside the dialysis unit, and also review the methods and procedures used in the dialysis unit.
◾ Follow up on the results of serological tests for all patients every 3 months.
Insulation
◾ Patients who are positive for antibodies to hepatitis C virus should be isolated from the rest of the negative patients.
· Allocate machines, devices, tools, supplies and medicines for these patients.
· Allocate a health team for these patients during dialysis sessions.
· Infected patients must be educated about ways in which they can prevent further damage to their private lives and the transmission of infection from them to others, by vaccinating them with the hepatitis B vaccine.
Measures to combat the transmission of hepatitis D virus infection
It is not necessary to conduct departmental tests to discover infection with hepatitis D virus, but if it is discovered that a person is infected with this disease or there are indications that it may be transmitted through a dialysis center, it is permissible to conduct an examination to confirm the presence of antibodies to the virus, and since the hepatitis D virus 'D' depends for its existence on a host already infected with the hepatitis B virus. Avoiding infection with the 'B' virus will lead to not being infected with the 'D' virus.
Preventing infection with the human immunodeficiency virus (HIV)
Infection control precautions are sufficient to prevent the transmission of the virus from one patient to another, while ensuring the isolation of infected patients in dialysis units in fever hospitals.
The following tests are performed for all kidney disease before the start of treatment and every 3 months:
HBsAg: 'surface' antibodies to hepatitis B virus
HCV Ab: Hepatitis C virus antibodies
HIV Ab: antibodies to the human immunodeficiency virus 'HIV'
Preventing bacterial diseases
Follow the instructions for the optimal use of antibiotics.
Standard infection control precautions are sufficient to prevent transmission to and from patients or those colonized with certain bacterial species, including antimicrobial-resistant strains. However, other precautions (such as contact-transmitted disease isolation precautions) must be taken when dealing with certain patients who are at high risk of transmission. Infection to others.
General Notes:
Adherence to adherence to isolation precautions for contact-transmitted diseases of patients colonized or infected with antibiotic-resistant microbes (MRSA, VRSA, VRE) during dialysis sessions for these patients is adhered to.
The staff caring for dialysis patients infected with antibiotic-resistant microbes must wear appropriate personal protective equipment, including a medical gown, and take off these protective equipment immediately after dealing with the patient, while carrying out the dialysis process for these patients in a place prepared for that, as far away from the rest of the patients as possible. (At the end of the unit or as far away from the rest of the patients as possible
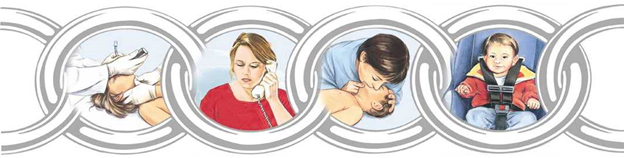
- Cardiopulmonary resuscitation
A) For an injured adult on the street
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who does not breathe, does not speak, and does not respond, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total obstruction of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Steps:
An initial assessment of the environment surrounding the injured person and ensuring that it is free of any dangerous factors (electricity, fire, drowning, etc.).
In the first 10 seconds from the beginning of seeing the injured person, the injured person is placed lying on his back, his degree of consciousness is assessed, and he is called in a loud voice with a shrug of the shoulders, “Are you okay??” '.
No response or abnormal breathing.
Never expose the injured person's chest.
Place the palm of one hand (the whole hand) vertically in the middle of the sternum between the nipples.
Start by doing chest compressions at a rate of 30 per minute
A period not exceeding 18 seconds, or less if there are one or two paramedics.
To perform cardiopulmonary resuscitation in a correct and effective manner, the following must be taken into account:
1- Place the injured person on a hard surface.
2- Begin compressions on the injured person's chest within 10 seconds.
3- Press hard, quickly, and to a depth of 5 cm in adults over 18 years old
4- Allow the rib cage to take its natural space after each compression
5- Reduce external influences (as long as they are less than 10 seconds)
6- Give the injured person an effective breath (by opening the airway by tilting the head back, pulling the chin forward, and opening the airway - but in the case of injuries to the cervical vertebrae, stabilize the injured person’s head).
7. Give 2 breaths if there is one or two paramedics present for the seriously injured person, within a period not exceeding three seconds.
8- Five consecutive segments of compressions and breathing are done (for two minutes) and breathing and pulse are re-evaluated.

Basic CPR
B) For a child injured in the street
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who is not breathing, speaking, or responding, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The reasons :
Total blockage of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Action Steps :
An initial assessment of the environment surrounding the injured person and ensuring that it is free of any dangerous factors (electricity, fire, drowning, etc.)
In the first 10 seconds from the beginning of seeing the injured person, the injured person is placed lying on his back, his degree of consciousness is assessed, and he is called out in a loud voice while shaking his legs, “Are you okay??” '.
There is no response or abnormal breathing.
Call for emergency medical assistance by calling the local number.
Make sure there is a clear pulse (no less than 5 seconds and no more than 10 seconds)
The pulse in the brachial artery (the inner side of the arm for easy identification of the presence of a pulse since it is the largest artery in the body) from the side opposite the paramedic.
5. When it is confirmed that there is no confirmed pulse within 10 seconds, perform cardiopulmonary resuscitation as follows:
Never expose the injured person's chest.
Place the index and middle fingers of the hand vertically in the middle of the sternum between the nipples if there is a single paramedic and the thumbs of both hands if there are two paramedics.
Start doing chest compressions at a rate of 30 compressions in a period not exceeding 18 seconds, or less if there is one paramedic, and if there are two paramedics, give 15 compressions (30 compressions, then 2 breaths) and repeat for two minutes at a rate of 100-120 compressions and 10-12 breaths.
To perform cardiopulmonary resuscitation in a correct and effective manner, the following must be taken into account:
Place the injured person on a hard surface.
Begin compressions on the injured person's chest within 10 seconds.
Press hard, quickly, and to a depth of 4 cm in children from one to eight years of age.
Allow the rib cage to take its natural space after each compression
Reduce external influences (should be less than 10 seconds)
Give the injured person an effective breath (by opening the airway by tilting the head back and pulling the chin forward and opening the airway - or in the case of injuries to the cervical vertebrae, immobilize the injured person’s head).
d. Give 2 breaths if there is one or two paramedics present
6- Five consecutive sections of compressions and breathing are performed (for two minutes) and re-evaluation of breathing and pulse.
Note: When following these steps, infection control policies for administering treatment should be taken into account
Advanced cardiopulmonary resuscitation in hospital
The Definition :
1. The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who does not breathe, does not speak, and does not respond, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
2. Total obstruction of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
3. The nursing team.
4. Tools:
5. Hands.
Action Steps :
6. Ensure that the surrounding environment is safe for the workers and the patient (within no more than 10 seconds).
7. Adjusting the patient’s position.
8. Ensure the level of consciousness of the injured person (by gently shaking the shoulders and speaking to the patient in a loud voice, “Are you okay?” for a period not exceeding 10 seconds).
9. If the patient answers, this indicates that the heart and lungs are working well. In this case, it is evaluated whether the patient needs other assistance or not.
10. If the patient does not answer, we begin by taking the following steps:
11. Opening the patient’s airway:
12. Opening the airway by installing a laryngeal tube - this is the best way to open the airway, but it is only installed in the hospital due to the lack of capabilities and human resources trained for this in the street.
13. Assessing the patient’s breathing:
14. By looking at the patient’s chest (there is movement in the patient’s chest up and down), the duration of the assessment for breathing is 10 seconds.
15. Assessing the presence of a pulse or not:
16. By checking the pulse with the carotid artery for no more than 10 seconds and no less than 5 seconds from the direction opposite the paramedic.

1. In the absence of breathing and pulse:
2. - Pressure on the sternum a distance above the xiphoid process
3. 2 fingers in the middle of the line between the nipples.
4. - Interlock the fingers of both hands and press them together.
5. The hands should be straight and perpendicular to the chest, the back should be straight, and the force of the pressure should come from the muscles of the pelvis and legs.
6. Giving breathing to the patient through a throat tube or using a tube mask (mouth-to-mouth breathing is not given).
7. The ratio of chest compressions to the rate of breathing for the patient varies depending on whether a throat tube is present or not:
8. In case of a throat tube:
9. - Perform 30 chest compressions for 2 breaths, whether it was one paramedic or two paramedics.
10. In the absence of a throat tube:
11. - Perform 100 chest compressions per minute and at the same time give 8-10 breaths per minute.
12. Perform five divisions of chest compressions and breathing, then re-evaluate breathing and pulse.
13.
14. If the heart returns to work, chest compressions are stopped and the patient is placed on a ventilator according to his condition.
Airway obstruction ( chorus)
Definition of a lump:
Bloating occurs when a solid or liquid object or the back of the tongue blocks the airway, and the victim may quickly stop breathing and lose consciousness. The blockage may be partial or complete, such as (false teeth, food debris, coins, etc.). This may affect the patient's breathing and may lead to loss of consciousness. If immediate intervention is performed, the blockage may be partial or complete.
The Reasons:-
Trying to swallow large pieces of food without chewing them well.
It may result from a muscle spasm.
Use a denture. Artificial teeth make it difficult to feel the size of the bite while chewing and swallowing.
Talking emotionally or laughing while eating.
Walking, playing, or running with objects in the mouth.
Tags:-
Partial airway obstruction:
When the patient suffers from partial airway obstruction, he coughs forcefully in an attempt to dislodge the object blocking the airway, and he may be able to speak.
A whistle may be heard when breathing.
The injured person may hold his throat with one or both hands

If the patient is conscious:
Ask the patient to cough as this helps expel the foreign body.
If the patient cannot respond, the Hemlich-Hetti method is used
The foreign body is expelled from the airway through...
Stand behind the patient and wrap your arms around his waist.
Place the thumb side of your fist in front of the injured person's abdomen, just above the navel
And hold your fist with the other hand.
Press inward and up the abdomen with quick pushes and repeat these pushes
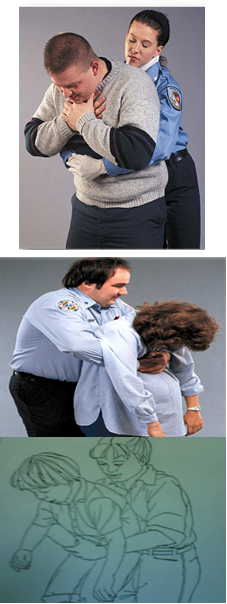
If the patient is a child from the age of puberty, we use abdominal pressures while holding the child on the foot for five pressures
If the patient is a child from one month to one year, the nurse uses compressions
Five dorsal compressions or five chest thrusts, but using the palm of the hand
An unconscious patient
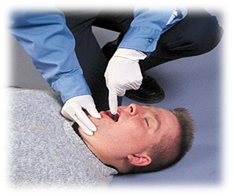
Place the patient on his back so that the airway can be opened.
Bend the patient's head backwards with a slight tilt to one side to facilitate the expulsion of the foreign body.
The fingers are inserted to wipe the patient's mouth from the inside using a hook method.
If the foreign body does not come out, the patient is given one count of exhalation and the chest is observed to rise
Follow Hemlich's steps until the foreign body exits the airway:
Sit on your knees so that they surround the patient's thighs.
Place the palm of one hand over the stomach area.
Place the other hand on the first hand and press on the abdomen with five quick successive thrusts to increase internal pressure to help push the foreign body out.
The steps are repeated until the patient expels the foreign body.
The pulse is checked and if there is no pulse, cardiopulmonary resuscitation procedures begin.
If the injured person loses consciousness, lower him to the ground, supporting his head and neck
Clean the mouth with your finger in the shape of a hook
If there is no response, apply abdominal pressure.

- Nursing evaluation
The initial examination of the patient is considered very important because its steps are the highest priority. By evaluating the patient, sources of threat to the patient’s life can be identified.
The nursing staff evaluates the patient upon admission to the hospital using the nursing staff evaluation form.
A form for evaluating the patient's condition upon admission to the hospital
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The initial information and data are recorded when the patient enters the department on the nursing staff evaluation form for the patient:
Vital signs (pressure, pulse, respiratory rate, temperature).
Weight and height.
Having an allergy.
Pain assessment
Evaluate skin condition
Assess the patient for the possibility of a fall
Nutritional assessment.
Evaluation of motor activity.
The patient's need for restraint or isolation.
Informing the patient of his rights, responsibilities, and hospital policy within 24 hours of admission.
The nursing staff evaluates the nursing staff and determines the following:
In severe cases (care)
Degree of awareness and awareness.
Vital Signs .
Complications occur.
The nursing evaluation rate is continuous, and the doctor on behalf of the department is called in the case of critical results (physiological - laboratory - x-ray) and when there is pain, and the doctor re-evaluates.
The re-evaluation of the patient is documented and a follow-up note is recorded at least once per shift (every 24 hours), and any procedures resulting from a call or emergency or important events for the patient are recorded by date and hour.
In non-acute cases:-
Are evaluated:
Vital Signs .
Patient compliance with treatment and medical instructions.
This is done every 12 hours for the internal department by nursing staff unless clinical evidence requires less than that and this is documented in the patient’s file.
Conditions that require long-term treatment (chronic diseases)
Nursing staff care for patients who need long-term or (chronic) treatment and ensure...
Vital Signs .
Complications occur
Outcomes of treatment
The nursing staff on duty also re-evaluates the patient every shift to determine the patient's needs
Cases that need to be re-evaluated
The treatment plan developed for the patient Individualized care plan
Change in patient condition
Diagnosis: Patient diagnosis
Expected outcome of care, treatment or service
The extent of the patient's response to previous treatment
The re-evaluation is documented in the patient's file
The patient should be re-evaluated immediately before anesthesia is administered
Content reassessment for nursing
Vital signs: every 6 hours in inpatient departments, every 2 hours in care and premature care, after blood transfusion, before surgical operations, during recovery, and when the patient complains that requires re-measurement, or according to the doctor’s instructions.
The Pain:
Probability of patient falling: every shift.
Skin condition: all skin color during recovery.
Nutritional assessment: when the patient needs it, according to the doctor’s orders.
Measuring blood sugar: according to the doctor’s instructions.
The patient’s need for restraint or isolation: according to the doctor’s orders.
Pain assessment:
The responsible nursing staff assesses the pain (according to the following table), determines its severity, describes the pain and its frequency by asking the patient and looking at the patient’s facial expression (in the event that he is unable to speak or in the event that he is a child). This is recorded in the pain assessment form and kept in the patient’s file when Admission of the patient to the hospital.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
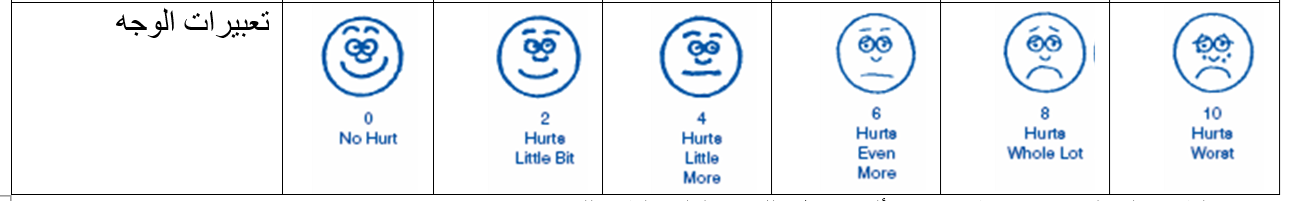
The treating physician develops a pain treatment plan and records this in the patient’s medical file.
The responsible nursing staff implements the treatment and follow-up plan in accordance with the pain model and the doctor’s instructions.
The responsible nursing staff re-evaluates the pain and records it in the previous form and completes it with each nursing shift. The evaluation can be re-evaluated more than that depending on the patient’s condition:
1. The responsible nursing staff re-evaluates the pain once before surgeries and after surgeries, once every hour for 3 hours, then every shift, or according to the doctor’s orders.
2. The responsible nursing staff re-evaluates the pain if pain is present and after administering pain medication
- Vital Signs
The Definition
These are indicators that health team members search for through a physical examination to determine the basic functions of the body, which include temperature, pulse, breathing, and blood pressure.
A) Oral temperature measurement
The Definition :
Temperature is a number that indicates the state of the body in terms of hotness and coldness.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
36.4 – 37.4 degrees Celsius.
The person in charge:
Nursing team.
Tools :
Mercury thermometer - alcohol - piece of gauze - timer.
Steps:
Identify the patient. (Patient's name and identification bracelet)
Explain the procedure to the patient.
Hand washing.
Preparing tools.
Maintain patient privacy.
Adjust the thermometer and move it vigorously until the mercury line reaches 35 degrees (the starting point).
Clean the thermometer from top to bottom with alcohol.
Place the thermometer at eye level to ensure it reaches the starting point.
Place the mercury part of the thermometer under the tongue for (three minutes) in the patient’s mouth.
Extract the thermometer from the patient's mouth.
Clean the thermometer from bottom to top with a dry piece of gauze.
Reading the measurement Recording the thermometer reading on the form for recording the temperature.
Stir the thermometer vigorously to lower the mercury level.
Clean the mercury part of the thermometer from top to bottom with soap and water, dry it, and disinfect it with alcohol.
Place the thermometer in its designated container.
Hand washing.
Reassure the patient.
Record any emergency signs.
b) Measure the temperature through the armpit
The Definition :
Temperature is a number that indicates the state of the body in terms of hotness and coldness.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
36.4 – 37.4 degrees Celsius.
The person in charge:
Nursing team.
Tools :
Mercury thermometer - alcohol - piece of gauze - timer.
Steps:
Identify the patient. (Patient's name and identification bracelet)
Explain the procedure to the patient.
Hand washing.
Preparing tools.
Maintain patient privacy.
Adjust the thermometer and move it vigorously until the mercury line reaches 35 degrees (the starting point).
Clean the thermometer from top to bottom with alcohol.
Place the thermometer at eye level to ensure it reaches the starting point.
Place the mercury part of the thermometer under the armpit, making sure that this place is dry for (five minutes).
Extract the thermometer from the patient's mouth.
Clean the thermometer from bottom to top with a dry piece of gauze.
Reading the measurement Recording the thermometer reading on the form for recording the temperature. Taking into account (half a degree increase when reading the thermometer) and signed.
Stir the thermometer vigorously to lower the mercury level.
Clean the mercury part of the thermometer from top to bottom with soap and water, dry it, and disinfect it with alcohol.
Place the thermometer in its designated container.
Hand washing.
Reassure the patient.
Record any emergency signs.
Measuring temperature through the anus
The Definition :
Temperature is a number that indicates the state of the body in terms of hotness and coldness.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
36.4 – 37.4 degrees Celsius with an increase of half a degree.
The person in charge:
Nursing team.
Tools :
Mercury thermometer - alcohol - piece of gauze - timer.
Steps:
Identify the patient.
(Patient's name and identification bracelet)
Explain the procedure to the patient.
Hand washing.
Preparing tools.
Maintain patient privacy.
Adjust the thermometer and move it vigorously until the mercury line reaches 35 degrees (the starting point).
Clean the thermometer from top to bottom with alcohol.
Place the thermometer at eye level to ensure it reaches the starting point.
Place gel on the edge of the mercury part and place the thermometer for a minute, taking into account that the patient is on his side.
Remove the thermometer and clean the mercury section from the bottom with a dry piece of gauze.
Read the measurement and record the thermometer reading on the temperature recording form. Taking into account (a decrease of half a degree when reading the thermometer).
Stir the thermometer vigorously to lower the mercury level.
Clean the mercury part of the thermometer from top to bottom with soap and water, dry it, and disinfect it with alcohol.
Place the thermometer in its designated container.
Hand washing.
Reassure the patient.
Record any emergency signs.
Note: The anal measurement method is used in children and burn cases.
Pulse measurement
The Definition :
The pulse is the wave generated in the arteries as a result of the contraction of the heart. The pulse can be felt by feeling the large arteries in the human body, such as the neck and wrist. (As in the attached picture)

The Reasons :
Monitoring the patient's vital functions.
Normal rates:
70-100 N/Q per adult and 80-130 N/Q for children.
The person in charge:
Nursing team.
Tools :
Time timer.
Steps:
1. Getting to know the patient. (Patient's name and identification bracelet)
2. Explain the procedure to the patient.
3. Washing hands.
4. Prepare tools.
5. Choose a comfortable position for the patient.
6. Place the tip of two fingers of the hand (index and middle) on the artery (radial - carotid - femoral)
7. Using the watch with the other hand.
8. Count the pulse for one full minute. The normal pulse rate is 70-100 beats/s in an adult and 80-130 beats/s in children.
9. Recording the pulse using the vital notes form and reporting if the pulse is (fast - slow - strong - weak - irregular).
10. Reassure the patient.
11. Hand washing.
Spirometry
The Definition :
12. Assessing the rate and regularity of breathing (which is the process of the body obtaining oxygen through breathing, which is necessary to carry out its activities and get rid of carbon dioxide).
The Reasons :
13. Follow up on the patient’s vital functions.
Normal rates:
12-20 N/Q per adult and 24-40 N/Q for children.
The person in charge:
Nursing team.
Tools :
Time timer.
Steps:
1. Identify the patient. (Patient's name and identification bracelet)
2. Explain the procedure to the patient.
3. Prepare tools.
4. Be careful not to measure breathing after muscular effort.
5. Place the patient in a comfortable position, preferably semi-sitting.
6. Ensure that the patient’s chest movement is clear to her.
7. Observe the rise and fall of the patient’s chest.
8. Count each inhalation and exhalation as one breath for a full minute.
9. Notice any abnormal signs in breathing.
10. Note the patient’s color, especially around the lips and fingernails.
11. Record the respiratory rate on the patient’s form.
12. Inform the doctor of any abnormal signs.
- Installing a catheter and drawing blood
The Definition :
Evaluating the movement of blood vessels by knowing the volume of blood, the blood returning to the heart, the extent of resistance of peripheral blood vessels, and the elasticity of the arteries.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
80/110 mm/Hg.
The person in charge:
Nursing team.
Tools :
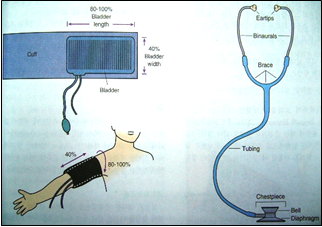
Blood pressure device and stethoscope.
Steps:
1. Getting to know the patient.
2. (Patient’s name and identification bracelet)
3. Explain the procedure to the patient.
4. Prepare tools.
5. Be careful not to measure pressure after muscular effort.
6. Place the patient in a comfortable position.
7. Maintain patient privacy.
8. Measuring blood pressure before and after giving high blood pressure medications.
9. Record your blood pressure measurement directly on the form designated for that purpose.
10. Determine the type of diet (low salt and fat).
11. Note the complications that may occur to the patient (nosebleeds).
Installation of intravenous cannula
the definition
It is a device that is connected intravenously to administer intravenous medications and solutions.
People most at risk: All patients treated with intravenous injections.
Working team:
Nursing team.
Tools :
Tray with lid - cannulas of different sizes - medical cotton - adhesive plaster strips - latex gloves - 70% alcohol.
Steps:
· Verify the patient’s identity and double-check the name.
· Explain the procedure to the patient to reduce his anxiety.
· Maintaining patient privacy.
· Wash hands and wear gloves.
· Tie the forearm with a compression bandage, preferably the forearm that is least used.
· Disinfect the catheter installation site with 70% alcohol and leave it to dry. Do not touch it after disinfection
· Inserting a cannula and monitoring the appearance of a spurt of blood in the place known as the cannula (as a sign of penetration of the vein wall) and completing the insertion slowly while pulling the metal insert out of the vein.
· Do not try to insert the same cannula again.
· Loosen the compression band from the forearm (tournament).
· Connecting the solution device to the cannula to test the efficient operation of the cannula.
· Fix the cannula with adhesive tape and write down the date of installation.
· Leave the installation site dry and visible.
· Dispose of the cannula tip immediately after use in the sharps waste safety box.
· Cleaning the used tools, putting everything back in its place, and preparing it for the next use.
Cannula removal should be considered in the following cases:
· Immediately after a blood transfusion.
· After completing the need for it, or after only 3 days have passed since installation.
When redness or inflammation appears at the cannula site
Urinary catheter installation
The Definition :
It is a procedure performed for the patient in medical conditions according to the doctor’s instructions.
The Reasons :
Bladder emptying - estimating the amount of fluid expelled - surgical operations
Working team:
Nursing team.
Exposed people:
Liver patients - kidney patients - urinary tract patients - bedridden patients
Tools :
Urinary catheter with a size suitable for the patient - urine collection bag - 10 cm syringe - salt solution - sterile gloves - gauze - Betadine for disinfection - KY gel - medical adhesive.
Steps:
1- To maintain the patient’s privacy, paraffin is placed or installed in the spare booth.
2- Tell the patient what you will do and explain the medical reasons for installing a catheter.
3- Gather the necessary tools to install a urinary catheter.
4- Surgical hand washing.
5- Wear sterile gloves.
6- Connect the urine collection bag to the catheter first.
7- Apply 3 ml of gel (or any anti-friction material).
8- He hands the sterile catheter to the doctor to install it.
After installing the catheter:
· Fixing the catheter in the thigh with plaster.
· Place the urine bag below the level of the patient’s bed and place it on a urine holder to prevent urine reflux.
· Bring the patient’s own urinal to empty the urine from the urine collection bag.
· Dispose of waste in its red bag.
· Wash hands routinely after removing gloves and dry them well.
· Recording in the nursing staff’s notes the type of catheter, the time of installation, and the doctor by whom the catheter was installed.
· Observe and record the amount of urine and any changes (blood - pus) and inform the doctor.

Drawing blood samples
The Definition :
It is a procedure done to obtain a blood sample for analysis.
Most exposed people:
Patients in departments.
Working team:
Nursing team.
Tools :
70% alcohol - sterile and dry cotton - syringes measured according to the required quantity - tourniquet
Steps:
1. Explain the procedure to the patient.
2. Washing hands.
3. Place the tourniquet above the elbow and tie it.
4. Feeling the location of the vein and cleaning and disinfecting the location of the vein and its surroundings.
5. Choose the appropriate place and tighten the skin below the area chosen to take the sample.
6. Inserting the tip of the needle into the vein at an angle of 30 degrees so that it enters the skin first and then enters the vein.
7. Raise the tourniquet and take the required amount of blood slowly.
8. Place a piece of sterile gauze over the place where the vein enters and apply pressure for 2-4 minutes until the blood stops.
9. Remove the syringe tip and place the amount of blood required for analysis into the tubes prepared for this purpose.
10. Place a sticker on each tube with the patient’s name and his file number (the department in which he is treated).
Dispose of used tools properly.
Do a sugar analysis
The Definition :
It is a procedure done to determine the blood sugar level.
Most exposed people:
Diabetics.
Working team:
Nursing team.
Tools :
Sugar analysis device - test strips with the same code as the device - sterile cotton or gauze - straws - alcohol - latex gloves.
Steps:
· Hand washing.
· Explaining the procedure to the patient.
· Wear a glove, hold the patient’s finger down and squeeze gently.
· Wiping the tip of the finger with a cotton ball containing alcohol, and the finger is suspicious.
· Place the tip of the strip or the designated place on the strip to place a drop of blood.
· Press the finger with a cotton ball until the blood stops coming out.
· Dispose of waste in the designated place.
· The nursing staff records the blood sugar level on the relevant form and gives the insulin dose according to the doctor’s orders.
Giving treatment orally
The Definition :
These are medications that are given orally (such as tablets and syrup).
The Reasons :
Treating the patient's signs and symptoms.
The person in charge:
Nursing team.
Tools :
Medications dispensed to the patient.
ten (10) It is important to follow the correct ten times before giving the medicine
Rights:-
1. The correct patient
2. The correct medication
3. The correct dose
4. The correct method
5. The correct time
6. Healthy repetition
7. Correct registration
8. Required effectiveness.
9. The right to refuse
10. The right to education
Steps:
1. Washing hands.
2. Review the doctor’s order for the medication and prepare the treatment, taking into account the time coordination, unless the time at which administration is required is specified
3. Verify the correct patient through the patient’s file and identification bracelet (full name and medical number).
4. Explain the procedure that will be performed to the patient.
5. Maintaining patient privacy.
6. Ask the patient to sit if possible so that he can take the medicine.
7. In the case of treatment with tablets, take the tablets to the patient with a glass of water, taking care not to touch the tablets with the hand.
Ensure that the patient takes the treatment dose on time in the presence of a nursing team member.
8. Notify the doctor if the patient refuses the medication to be given and write this down in the form designated for that purpose.
9. Securing the patient after giving medications that cause a change in the patient’s consciousness (narcotics, blood pressure medications, etc.) by raising the sides of the bed or warning the patient not to walk without assistance.
10. Notifying the treating physician in the event of any medication error, which is recorded in the form for reporting a medication error or the appearance of side effects of medications in the nursing registration form.
11. Recording the administration of treatment in the treatment implementation form
- Method of giving treatment
Giving the treatment via intramuscular, subcutaneous, and intravenous injections
And allergy testing
The Definition :
These are medications that are given by intramuscular, intravenous, or subcutaneous injection (such as vials, ampoules, and diabetes treatment 'insulin').
The Reasons :
Treating the patient's signs and symptoms.
The person in charge:
Nursing team.
Tools :
Medicines - syringes - cotton - alcohol - solutions - intravenous devices - cannulas of different sizes - medical adhesive - tourniquet.
It is important to follow the correct ten times before giving the medicine
(ten (10) Rights):-
1. The correct patient
2. The correct medication
3. The correct dose
4. The right way
5. The right time
6. Healthy repetition
7. Correct registration
8. Required effectiveness.
9. The right to education.
10. Right of refusal
Steps:
1. Washing hands.
2. Verifying the patient (full name and medical number)
3. Explain the procedure that will be performed to the patient.
4. Maintain patient privacy.
Preparing treatment for intramuscular injection:
1. If it is a single ampoule, withdraw the treatment using a sterile syringe and expel the air from the syringe.
2. If the treatment needs to be analyzed, the water ampoule is withdrawn using a sterile syringe, then it is injected into the ampoule containing the powder, the bottle is shaken, then the specified dose is withdrawn using the syringe, then the air is expelled.
3. The site of intramuscular injection is determined.
4. Clean the site designated for the injection with a piece of cotton moistened with 70% alcohol in a circular manner and in one direction from the inside out without going back again.
5. Insert the tip of the syringe perpendicular to the injection site, then pull the syringe plunger out to confirm the injection site (if blood is drawn, the site is considered wrong and is changed, and if nothing is drawn, the site is correct and the treatment is injected).
Preparing treatment for a patient through intravenous injection:
1. Determine the location of the intravenous injection.
2. The place to be injected is tied with a tourniquet.
3. Feel the vein with the tip of the index finger.
4. Clean the site designated for the injection with a piece of cotton moistened with 70% alcohol in a circular manner and in one direction from the inside out without going back again.
5. The tip of the syringe is inserted at an angle slightly raised along a parallel line from the surface of the skin at the site of feeling the vein.
6. The syringe plunger is pulled out to confirm the location (blood flows into the syringe).
7. Loosen the tourniquet and inject the treatment slowly.
8. Press the injection site with a piece of cotton soaked in alcohol until the blood stops at the injection site.
9. Place a small piece of gauze at the injection site and secure it with adhesive tape.
10. Dispose of injection waste in a waste disposal bag.
11. Registration in the treatment description and implementation form.
Preparing treatment for a patient by subcutaneous injection:
1. Stabilize the skin at the injection site and, with a quick pricking motion, insert the needle at an angle of 90 degrees if the skin is thick and 45 degrees if the skin is thin.
2. Injecting the treatment to be given.
3. Remove the needle and press a piece of cotton soaked in alcohol on the injection site.
4. Dispose of all waste in accordance with infection control policy.
5. Recording the administration of treatment in the treatment description and implementation form.
Drug allergy test:
1. Perform the subcutaneous injection steps at a 45 degree angle in the case of a 3 cm syringe and a flat site in the case of an insulin syringe.
2. When injecting, inject only one ml of the drug to be tested.
3. Mark the injection site.
4. Observe the injection site for 10 minutes after the injection.
5. Notify the doctor if any reaction occurs (redness of the skin, visible swelling, tendency to scratch).
6. You record this on the patient’s ticket and allergy card.
7. The syringe containing the medication to be administered is prepared and the patient is injected if no reaction occurs.
8. The remaining steps are completed as usual for subcutaneous injection.
Note: When following these steps, infection control policies for administering treatment should be taken into account.
Transfusion
The Definition :
Giving a quantity of blood or its derivatives (plasma, platelets, red blood cells) to a patient according to the doctor’s instructions.
The Reasons :
Compensating blood loss from the patient's body and treating defects in blood components.
The person performing the work: the nursing team.
Tools: A bag of blood or its derivatives (usable) - a holder for solutions - a blood transfusion device - a spongy cotton with alcohol - medical tape - a large cannula.
Steps:
1. Hand washing (routine).
2. Verifying the patient (full name and medical number)
3. Measure the patient’s vital signs to ensure that they are within normal levels.
4. Explain the procedure that will be performed to the patient.
5. Maintain patient privacy.
6. Review the patient’s full name - blood types - and match the bag number with the delivery form number.
7. Preparing medications for recovery and incompatibility next to the patient.
8. Wash your hands (sanitary) immediately before installation.
9. Open the blood transfusion device, connect it to a bottle of saline solution, and fill it (to test the efficiency of its work).
10. Connect the device to the blood bag and transfer it to the patient very slowly for the first 15 minutes.
11. Measure the patient’s vital signs every 5 minutes for the first 15 minutes.
12. Note the presence of any symptoms of blood incompatibility with the patient’s body (such as: tremors, back pain, headache, vomiting, rapid pulse, low blood pressure, rapid breathing, skin rash).
13. Increase the drip in the absence of signs indicating incompatibility according to the doctor’s instructions on the ticket.
14. Dispose of the empty blood bag after completing the administration of the required amount, connect the blood transfusion device to the salt solution, pass the solution through the device until the blood disappears from it, and dispose of it in hazardous waste.
15. Measuring vital signs after a blood transfusion.
- Oxygen therapy
The Definition :
Giving an amount of O2 gas at a specific rate according to the patient’s needs and the doctor’s recommendations.
The Reasons :
Replenishing the proportion of oxygen in the body - maintaining the vitality of tissues and cells.
The person in charge:
Nursing team.
Tools :
Oxygen catheter - oxygen connector - oxygen regulator - sterile gauze - water humidifier with distilled water - a cup of water.
Steps:
1. Hand washing (routine).
2. Verifying the patient (full name and medical number)
3. Measure the patient’s vital signs to ensure that they are within normal levels.
4. Explain the procedure to the patient.
5. Prepare the necessary tools.
6. Keep the patient in a comfortable position.
7. Connect the regulator to the oxygen tube valve.
8. Connect the humidifier to the oxygen cylinder (or if there are central connections).
9. Connect the connector to the humidifier (nasal tube - oxygen mask).
10. Test for the presence of oxygen by placing the tip of the catheter in a cup of water (bubbles appear).
11. Connect oxygen to the patient.
12. Monitor the patient’s breathing condition and implement the doctor’s instructions.
13. Register in the nursing care form to monitor the extent of the patient’s condition improvement.
14. Inform the doctor if any side effects occur.
Specialized work procedures
· Anatomy of the circulatory system
Giving the patient an electric shock (D.C. Shock).
Al-Monitor
heart drawing
Nursing care for the angina patient
Nursing care for a heart attack patient
Nursing care for a heart failure patient
Nursing care of the trauma patient
Nursing care for a patient with pulmonary edema
Nursing care of an unconscious patient
Nursing care for diabetic coma patient
Nursing care for fainting and coma patients
Anatomy of the urinary system
· Nursing care of a patient with kidney failure
· Renal dialysis
· Nursing care before, during and after a kidney transplant
· Medicines and solutions used in the kidneys
· Procedures for receiving a patient for the first time
· Receiving a hesitant patient
· Nursing procedures during placement of a clavicle catheter (Mahooker
· Nursing procedures during femoral catheter placement
· Starting the hemodialysis session
· During a hemodialysis session
· Action steps for a patient with connections for a washing session
· Nursing actions during complications
· Ending the hemodialysis session
· Caring for the hemodialysis machine
· During a peritoneal dialysis session
· Isolating the patient in the unit
· Performing monthly tests
- Giving the patient an electric shock
The Definition:
It is giving the patient an electric shock on the surface of the heart in order to suppress the irritated spot, whether it is in the atrium or the ventricle. It is very effective if it is used within 15-20 seconds of the start of the occurrence of Arrythmia (arrhythmia). Thus, the irritated spot is calmed and given an opportunity (Sponde) or The sinoatrial node produces natural charges. The joule or colors are used to measure the amount of natural charges. It begins with the first dose (200 joules), the second dose (200-300 joules), and the third dose (360 joules).
Description of the device and how to operate it:
It is a device that acts as a regular monitor in addition to giving a charge.
As for its operation: - The amount of shock is determined as previously mentioned.
Choose the type of shipment (Synchronized), meaning it comes out with ((R).
It is used in cases:
-Atrial tremor - Atrium tremor
As for the only case in which Non synchronized is used, which is VF, ventricular tremor, and there is no R, a sufficient amount of gel is placed on the Paddels and on the patient’s skin to avoid burning the skin. Also, the Paddels with the word “sternum” written on them should be placed at the sternum on the right side up, below the collarbone. .
As for the paddels labeled Appex, they are located at the apex of the heart, under the nipple of the left chest.
Purpose of using the device
It is used to correct irregular heartbeats
Complete or sudden cessation of the heart muscle
The theory of device operation
The device produces an electric shock
Through two batteries attached to the patient's chest, this shock causes the muscle cells (heart) to contract momentarily. The electric shock is obtained by storing it in a high source capacitor. The charging process continues for several seconds until
an alarm sound is heard, then the capacitor is discharged in the patient's body through the two batteries.
Security and safety measures
1-_Fees for the device:
Total isolation between the inside and outside circles
Each hoop must have an unloading key
The device should contain an audio and visual warning when the device is charging
There should be automatic emptying inside the device
2-_Safety procedures for the patient:
To protect the patient from burns, a large amount of gel is applied
Put good pressure on the two frames until they stick, because moving them allows the presence of gel between two frames and allows an electric current to pass between them, but the electric current does not reach them.
Do not connect the patient to any other device while using the device
3-_Safety measures for the user:
Clean the two frames from the gel
Do not touch the patient while giving the shock
Do not discharge the charge into the air or stick together
Electroshock device and gel
Cardiopulmonary resuscitation tools
Steps:
Show the patient's chest
Start performing CPR
Apply the gel on the pads and on the patient's skin to avoid burns
The shipment is adjusted according to the doctor’s orders
Paddles are placed on the sternum on the upper side, below the collarbone on the right side
(Apex) (pads) are placed.
Click on the shipment button
The paddles are raised after giving the load. Types of shocks, two types,,,
non synchronized or defibrillation
Synchronized or cardioversion
The differences between them
non synchronized or defibrillation
Asynchronous electric shock (1) This means that we set a time by pressing the electric charge discharge button (deliver).
We start with three successive shocks: 200 J, 300 J. 360 J 2, from least to most... and they are repeated after doing CPR for a minute until the sputum changes.
As for Synchronized or cardioversion
A shock synchronized with the start of the wave.... 1 We do not specify the discharge time. We click on discharge, but the device chooses the appropriate time.
Low joule,,, sometimes from fifty or a hundred joules 2
The patient should be given a sedative - a shock should be given. One shock should be given
· Causes of non-synchronized shock.. Non synchronized
1- Pulse ventricular tachycardia
2- Ventricular fibrillation
Causes of synchronized shock
Tachycardia refers to a group of irregular heartbeats provided that they are accompanied by a decrease in blood pressure. These are:
1-Atrial fibrillation <<<< AF
2-ventricular tachycardia
3- supra ventricular tachycardia <<< SVT
If the pressure is normal, you must start giving medications such as digoxin, adenosine, Isoptin, Cordarone... and when the pressure drops as a result of simultaneous shocks.
The fatal mistake, which is repeated daily without supervision or control, is when the ECG shows ventricular tachycardia (VT) and the doctor decides to administer a non-synchronized shock, which is non-synchronized or defibrillation.
Before he checked for a pulse, he treated it as if it was ventricular tachycardia without a pulse, but in reality it could be ventricular tachycardia with a pulse,, meaning both diagnoses are represented by one diagram.
Ventricular tachycardia registers a fatal diagnostic pulse, and ventricular tachycardia with a diagnostic pulse is not dangerous at all times, but after the wrong shock, we change the ventricular tachycardia from the presence of a pulse to the absence of a pulse and kill the patient.
Al-Monitor
The Definition:
The medical monitor device is an electronic medical tool used for medical observation, and physiological data is constantly shown on the screen of this device.
Types:
Analog note devices:
It was previously used, as the device only showed the EKG, and after special modifications were made to it, there became a monitor device that measured blood pressure and another device for measuring the pulse. These devices were widely used and helped save the lives of many people, but there were many obstacles in their way, such as Electrical interference, lack of alarms, and being expensive.
Digital note devices:
With the presence of digital signal processing technology, medical monitors have developed significantly. All models have become digital and have the advantage of miniaturization and portability. Their standards include pulse oximeter, blood oxygen meter, blood pressure, temperature, and electronic cardiogram.
Monitoring devices attached to the pacemaker:
These devices are often used in the reception and emergency units, in order to save time and effort in transferring the patient from one device to another.
Uses:
Measurement of vital signs
1. EKG
2. Measuring blood pressure using a pressure piece that is wrapped around the patient’s arms. Normal blood pressure is 12080±20
3. Measuring temperature using temperature converters
4. The normal temperature is from 36.5 to 37.5
1. Measuring the level of oxygen in the blood.
Most used individuals:
- Critical care unit patients.
- Dialysis unit patients.
- Operating room patients.
- Recovery room patients.
- Patients in reception units until they are classified.
- Patients of children in the neonatal critical care unit.
- Normal heart drawing
First, the electrocardiogram (ECG) means an electrocardiogram (electrocardiogram).
Diagnosing diseases depends mainly on taking a good look at the patient’s condition first, in addition to doing some tests. The EKG device confirms the diagnosis of many disease conditions, and in some cases it is very important for treatment.
An EKG is very important in diagnosing many conditions, including:
1. Changes in the regular rhythmic heartbeat.
2. It helps diagnose the cause of chest pain.
3. The use of thrombolytics in cases of myocardial infarction depends on the electrocardiogram.
4. It also helps in diagnosing the cause of shortness of breath (breathlessness).
So that you do not get lost from the topic, we will talk about the topic of drawing the heart in the following order:
First: We will talk about electrocardiography and how the heart beats.
Second: We will talk about the EKG device, how to make an EKG, and its pictures.
Third: We will discuss the topic of what we will read in the EKG paper.
First: electrocardiogram
The contraction of any muscle is accompanied by electrical currents called depolarization, and these currents can be recorded using electrodes. These electrodes are connected to the surface of the body. Therefore, we can record the contraction of the muscles of the entire body.
Therefore, if we want to record the contraction of only the heart muscles clearly, the person must be relaxed and all the other muscles of his body must be relaxed.
Although the heart contains 4 chambers, we will see in the electrocardiogram that there are only two chambers because the atria contract together and the ventricles as well.
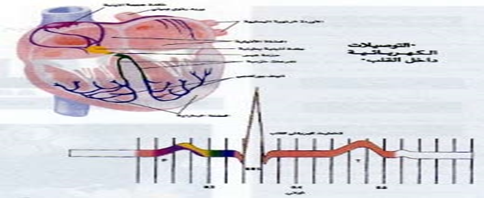
Normal pulse
• The regular rhythmic heartbeat originates from within the tissue of the heart muscle itself. It is self-moving, as the normal pulse begins with an electrical signal issued by a specialized, very small neuromuscular electrical generator and regulator located in the wall of the right atrium called the sinoatrial node, or sinoatrial node. At a rate of 60-100 pulses/electrical signal per minute, this electrical signal spreads very quickly to the atria, causing them to contract to push the blood from the atria to the ventricles. Then this electrical signal is transmitted to a receptor. In the same case, it is considered a very small backup generator located between the ventricles and the atria, and it is called the “node.” Atrioventricular (or () which allows the electrical signal to pass through electrical connections that branch from the atrioventricular node to the ventricles in a fraction of a second, which makes them contract to push blood from the ventricles out of the heart. The right ventricle pushes deoxygenated blood to the lungs to be oxidized, and the left ventricle pushes oxygenated blood to all... Parts of the body to benefit from the oxygenated blood that returns after the oxygen has been removed from it to the right part of the heart, thus completing one division of blood.
• Electrocardiogram
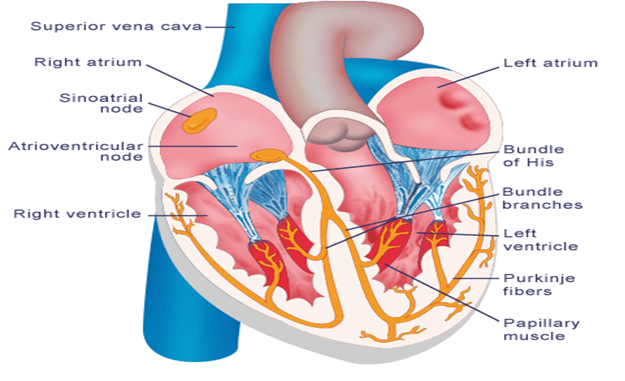
• Thus, in normal humans, the electrical signals originate from the (sinoatrial node), and at this time the system is called (cardiac rhythm) or (sinus rhythm), but in some pathological cases, the currents can arise from another source, such as (the atrioventricular node), and it is called The system at this time is called (nodal rhythm) or (nodal rhythm), or it may originate from any other source, such as the muscles of the ventricle itself, and this may be due to the failure of the sinoatrial node to issue pulses or the presence of an external source - anywhere else in the heart - that beats. At a rate higher than the primary pacemaker, it takes its place. Therefore, in a normal person, the electrical signals originate from the sinoatrial node, and at this time the system is called the “cardiac rhythm” or “sinus rhythm.” However, in some pathological cases, the currents can arise from another source, such as (Atrioventricular node) The system is called at this time (nodal rhythm) or (nodal rhythm), or it may stem from any other source, such as the muscles of the ventricle itself, and this may be due to the failure of the sinoatrial node to issue impulses or the presence of an external source - in Anywhere else in the heart - beats at a higher rate than the primary pacemaker and takes its place.
• EKG pictures (leads)
Each electrode connected to the body is considered a camera, and we place 10 electrodes on the human body, one on each arm and each leg, and at six points on the chest. Thus, we obtain 10 electrodes (cameras) from different directions. Each camera produces a different image for us from the other camera, because each One captures the view of the heart from a different angle, but it is the same view, like a football match. We find that there is more than one camera on the field, and each one captures a specific view from a specific angle, but it is.
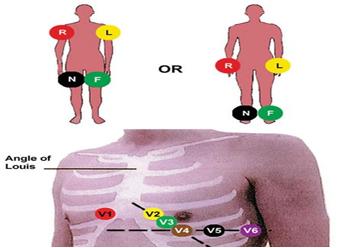
• The EKG device produces 12 images for us
• The six electrodes (cameras) on the chest produce 6 different images (leads) for us and are called
V1,V2,V3,V4,V5,V6
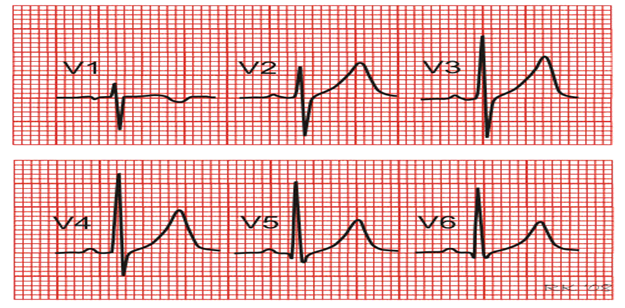
• The locations of the electrodes on the chest are as follows:
• V1: In space No. 4 between the ribs on the right
Rt. 4th intercostal space
V2: In the space number 4 between the ribs on the left
• Lt.4th intercostal space
• V3: At the point between V2 & V1
V4: At the apex of the heart APEX
V5: At the same level as the apex of the heart at the anterioer axillary line
V6: At the same level as the apex of the heart at the mid-axillary line
Link locations:
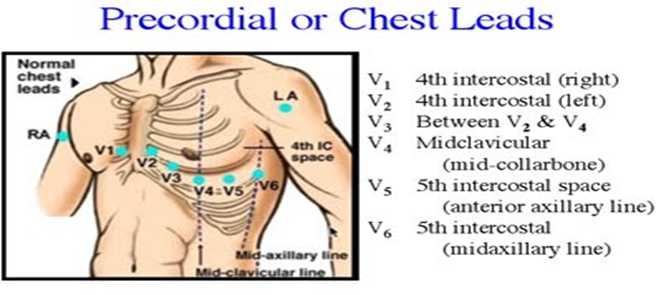
• As for the electrodes on the ends, each one produces an image for us, except for the one at the left leg, which is only for ground connection and does not interfere in the drawing.
For example: In the right hand, it is called: aVR
• The one on the left hand: aVL
• And the one at the right foot: aVF
• 3. As for the remaining three images, they are a fusion of each of the two images resulting from the poles located at the edges
For example: merging the image resulting from the camera (the electrode) located at the right hand with the other located at the left hand produces an image called:
(lead I).
• Also, the image of the right hand with the foot is called: (lead II).
• Also, the image of the left hand with the foot is called: (lead III)
• Since these images are a combination of more than one image, they are therefore magnified. In order for the resulting images to be all equal, the device enlarges the other images issued by the parties.
(aVR, aVL, aVF).
• Where the letter (V) means the word (Vector), meaning the electrode to which the camera is directed).
• The meaning of the word (a) is (augmented), meaning magnified, as we explained.
• The meaning of the word (R) is (Right arm).
• The meaning of the word (L) is (Left arm).
• And from me the word (F) is Foot).
• The pictures are arranged as follows (from left to right, of course):
• Lead I, lead II, lead III, aVR, aVL, aVF, V1,V2,V3,V4,V5,V6))-
EKG shape
• It is known that the muscles of the atria are very small when compared to the muscles of the ventricles, and therefore the electrical current accompanying the contraction of the atria will be small and is symbolized in the electrocardiogram by the symbol (P wave), while the contraction of the ventricles is symbolized by the symbol (QRS group) ( QRS complex), and then the relaxation of the ventricles is symbolized by the symbol (T wave), since the cardiac division begins with the contraction of the atria, then their relaxation, then the contraction of the ventricles, then their relaxation, and all of this is recorded as waves on the electrocardiogram paper...
In order of events:
• 1. Atrial contraction (P wave).
• 2. Then they relax (-) – and here the atria’s relaxation is not recorded because it occurs at the same time as the ventricles’ contraction, and therefore the ventricles’ contraction hinders the recording of the atria’s relaxation.
• 3. Then the ventricles contract (QRS complex).
• 4. Then they expand (T wave).
• For the QRS group, the first curvature down the straight line is called (Q wave) and the subsequent curvature upward is called (R wave) and it may be preceded by (Q wave) or not, then It is followed downward by another curvature called the S wave, which may also be preceded by a Q wave or no... That is, it is not necessary for the ventricular contraction to be represented by the entire QRS group.
• Any change in these images reveals a problem that may be in the heart rate or the result of a blocked artery or something else, but the most widely used and clearest images are (lead II) and (avR), and one of them is used to monitor the patient’s condition in care units. Concentrated, although the most widely used is (lead II
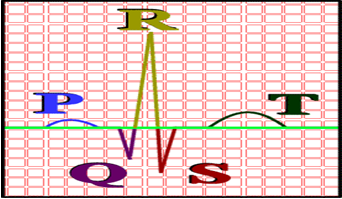
Conclusion:
• There are 10 electrodes (cameras) - they are placed on the chest, legs, and arms... They produce 12 images (leads), which are as follows:
• (Lead I, lead II, lead III, aVR, aVL, aVF, V1,V2,V3,V4,V5,V6).
• In each of these images we find some curves symbolizing the division of the heart:
• Atria contraction: (P wave).
• Their simplicity: (-).
• Ventricular contraction: (QRS complex).
• Their relaxation: (T wave)...
Important rule:
• If the direction of the electric current in the heart is in the same direction as the directing electrode (camera), then the result will be a negative (downward) curvature on the EKG paper, and vice versa, if the direction of the current is opposite the direction of the camera, then the result will be a positive (upward) curvature on the EKG paper, and that The direction of the current has nothing to do with the direction of the camera, so the signal (curvature) has any shape.
• Therefore, we find that most of the (lead II) curvatures are positive (upward) because the directed electrode (camera) is filming in the opposite direction of the current, while the (avR) curvature is downward because the directing camera is filming in the direction of the current.
• After reading the electrocardiogram, you must write a report on each of the following:
• 1. Heart rate/minute.
• 2. Heart rate rhythm (regular or not).
• 3. Cardiac axis imbalance.
• 4. Signs of ischemia.
• 5. P wave.
• 6. P-R interval(
• 7. QRS complex.
• 8. T wave().
• 9. ST segment
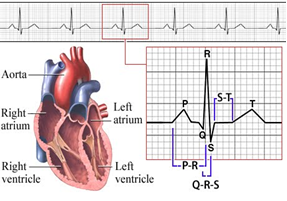
Heart rate and rhythm
• The EKG device picks up electrical currents and records them on graph paper with equal-sized squares at a regular rate. EKG paper contains large squares, and each large square contains 25 small squares (5 x 5), and each small square (1 mm) represents 0.04 seconds. Therefore, each large square (5 mm) represents 0.2 seconds, meaning that 5 large squares represent (1 second) and 300 large squares represent (1 minute).
• We can calculate the heart rate per minute. For example, if we find the complete heart division, each large square is repeated, meaning that the heart beats at a rate of 300 beats/minute, and so on...
Therefore, measuring the distance between (R waves) and each other - given that it is the highest point in the drawing - represents the heart rate. The distance between (interval R-R) represents the time it takes to conduct electrical currents through parts Different heart
• Therefore, the heart rate can be measured as follows:
• Heart rate = 300 (300 squares to calculate the number of heart beats per minute) ÷ the distance between (AR-AR), but this is if the heart rate is moving at a regular rhythm....
• Rhythm is measured by matching the distance between (R-R), which is equal in all images.
• If the rhythm is irregular, we will calculate the heart rate as follows
Heart rate and rhythm
• The EKG device picks up electrical currents and records them on graph paper with equal-sized squares at a regular rate. EKG paper contains large squares, and each large square contains 25 small squares (5 x 5), and each small square (1 mm) represents 0.04 seconds. Therefore, each large square (5 mm) represents 0.2 seconds, meaning that 5 large squares represent (1 second) and 300 large squares represent (1 minute).
• We can calculate the heart rate per minute. For example, if we find the complete heart division, each large square is repeated, meaning that the heart beats at a rate of 300 beats/minute, and so on...
Therefore, measuring the distance between (R waves) and each other - given that it is the highest point in the drawing - represents the heart rate. The distance between (interval R-R) represents the time it takes to conduct electrical currents through parts Different heart
• Therefore, the heart rate can be measured as follows:
• Heart rate = 300 (300 squares to calculate the number of heart beats per minute) ÷ the distance between (AR-AR), but this is if the heart rate is moving at a regular rhythm....
• Rhythm is measured by matching the distance between (R-R), which is equal in all images.
• If the rhythm is irregular, we will calculate the heart rate as follow
• Irregular electrocardiogram
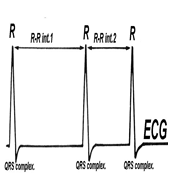
• Heart rate=
• Number of R waves
• Within 6 seconds x 10
• Of course, this calculation is done over the length of the EKG images for 6 seconds.
• P wave:
• Period: It represents the period of atria contraction.
• Duration: equal to 0.08_0.12 seconds, i.e. (2-3) small squares, and sometimes it is said to be (2.5 x 2.5) small squares, length by width.
• Shape: semicircular, symmetrical and in an upright position in the image (lead II) and upside down in (avR), as we mentioned previously.
Conditions that can be diagnosed from differences in the P wave:
• Enlargement of the right atrium, the most common cause of which is pulmonary hypertension:
• It is diagnosed by an increase in the height (length) of the (B) wave of more than 3 mm as a result of an increase in the period of contraction of the right atrium due to its large size, and because one of its most famous causes is high pulmonary pressure (Pulmonary hypertension), so it is called (P wave) by the name (P-Palmonale).
• The enlargement of the left atrium, the most common cause of which is mitral stenosis:
• It is diagnosed by an increase in the width of the B wave more than (0.11 seconds) as a result of an increase in the period of contraction of the left atrium due to its large size, and because one of its most famous causes is mitral stenosis, so it is called
• (P wave) as (P-Mitral).
· Atrial fibrillation
• and that is through:
The absence of the B wave (P wave) and its replacement by small fibrillatory waves, which are called the B wave at this time (F waves).
• Irregularity of the distance between R waves (R-R interval).
• 4- It is also possible to diagnose atrial flutter:
• By replacing (wave B) with flutter waves, which are shaped like saw teeth.
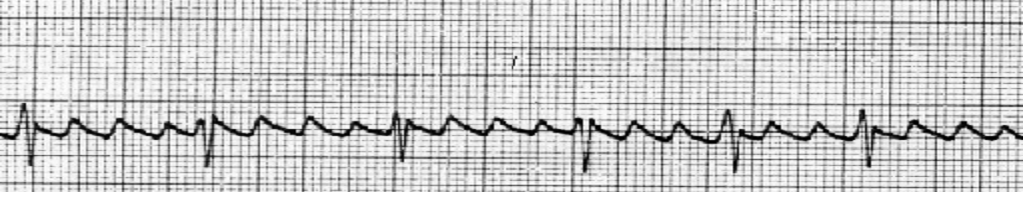
• 5- If the electrical signals originate from (the atrioventricular node)
• Nodal rhythm, not my heart rhythm, comes from (the sinoatrial node) as usual, and as we talked about previously, this may be due to the failure of the sinoatrial node (temporary or permanent failure) to issue pulses or the presence of an external source elsewhere in the heart that beats at a rate higher than The primary pacemaker (sinoatrial node) takes its place, and here it can be diagnosed through an inversion (wave B), where when (the atrioventricular node) is the source of the electrical signals, the direction of the electrical current changes and becomes in the same direction as the electrode (camera). Therefore, the B wave appears inverted (downward curvature) in (lead II) and upward in (avR)... Return to the base!!
• Third: P-R interval:
• It starts from the beginning of (wave B) to the beginning of (QRS group), that is, from beginning to beginning, and it represents the time it takes for the electrical current to travel from the sinoatrial node to the atria and from there to the ventricles.
• It is equal to = 0.12_ 0.20 seconds, which is (3-5) small squares.
Conditions that can be diagnosed from differences that occur at this distance
• : (tachycardia) palpitations (rapid heartbeat).
• The distance is shorter than the normal distance
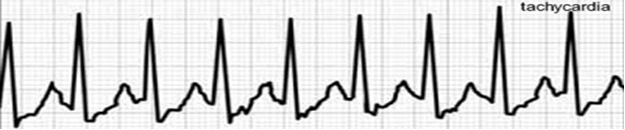
• 2- Bradycardia:
• The distance is longer than the normal distance

(Heart block): Heart block
• In the first degree of cardiac arrest:
• The usual length of distance increases.
• In the second degree:
• The length of the distance increases gradually, followed by its absence (QRS group), then it returns to normal again, and so on.
• In the third degree:
• The QRS group overlaps with (wave B), and the QRS group exists in different forms
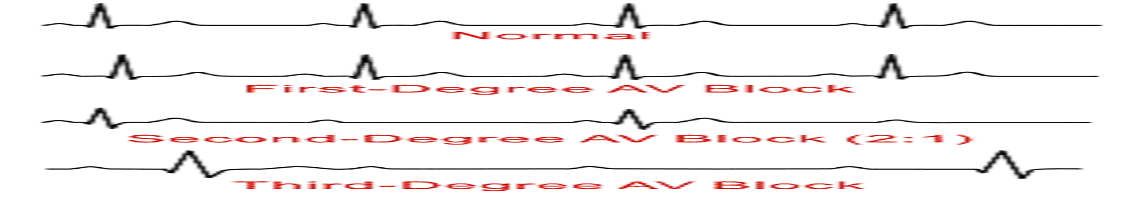
Fourth: QRS complex
• Period: represents the time it takes for the current to travel through the ventricles.
• Duration: equals = 0.12 seconds (3 small squares).
• Diagnosis: As we mentioned, it helps diagnose cases of atrial and ventricular fibrillation, atrial flutter, and other types of heart rhythm disorders.
It also helps in diagnosing angina and stroke, as we will explain, and other heart diseases.
Fifth: Cardiac Axis
• An imaginary line drawn on the heart representing the resultant electrical current, as the direction of the electrical current in the heart comes from the sinoatrial node - as we mentioned before - to the bottom, and since the left ventricle is larger than the right ventricle - because it supplies the entire body with blood - so if we imagine the path of the current The electrical current in the heart will be from top to bottom and directed slightly to the left. This is what is called the heart axis.
• Any changes in this axis are called misalignment of the heart’s axis to the right or left
• ( Rt or Lt axial deviation)
• In the event of an infarction in the left ventricle... the electrical current directed towards the left decreases, and thus a misalignment of the heart's axis towards the right occurs.
• If there is hypertrophy in the left ventricle... the electrical current increases towards the left and thus an imbalance occurs in the heart’s axis towards the left.
• Cardiac axis imbalance can be measured through (QRS group) through only 3 images, namely (lead I, lead II, lead III), as (lead II) is located directly opposite the direction of the electrical current (opposite the direction of the heart axis). Directly, (lead I) is located to the left of (lead II), while (lead III) is to the right of (lead II).
• And based on the rule... we will find that the QRS group in (lead II) is represented by a large upward curvature because it is directly facing the electric current, while in (lead I, III) the curvature will also be upward, but less than (lead II), as they are not directly facing the electrical current.
• Thus, in the event of an imbalance in the heart’s axis to the right, the QRS group in (lead I) will be represented by a downward curvature, while in (lead III) its rate of curvature will increase upward... and vice versa!
Sixth: QT interval
• It starts from the beginning of (group QRS) until the end of (wave T), and it represents the time it takes for the ventricles to contract and relax.
It is equal to = 0.30 - 0.44 seconds, which is less than two large squares and one small square.
This distance increases due to antiarrhythmic drugs that block potassium channels.
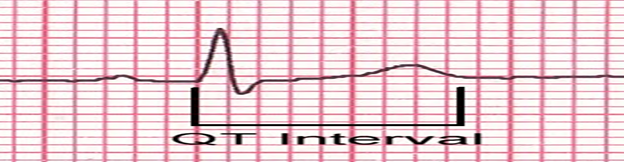
Seventh: T wave
• Period: represents the period of diastole of the ventricles.
• Duration: 4 small squares represent height.
• Shape: It is very similar to wave B, but wave T is asymmetric and takes the shape of the letter T and is in an upright position in the image (lead II) and inverted in (aVR).
Diagnosing some differences due to changes in the T wave:
• The T wave is low or flat in cases of:
• Hypokalemia and pericardial effusion.
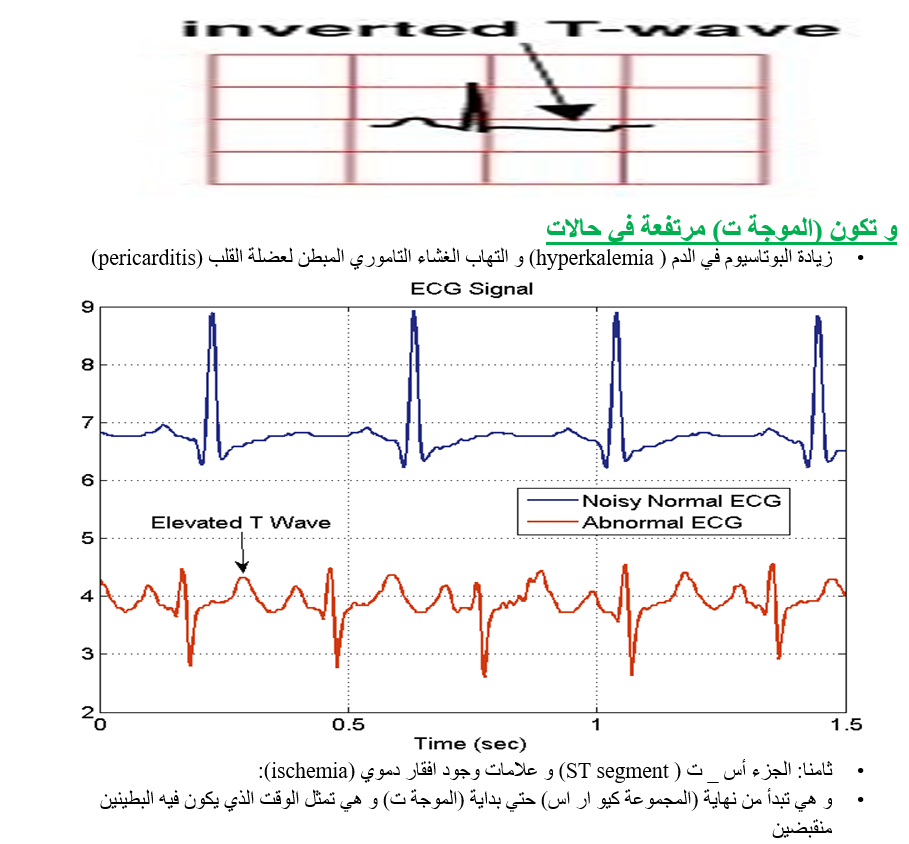
• It is equal to = 0.08 _ 0.12, i.e. (2-3) small squares.
Angina:
It is one of the most important distances that diagnose many cases, the most important of which are:
• The distance (AS_T) is lower than its normal level by 1 mm, and the (T wave) is also lower than its level... This is in addition to the presence of some types of heart rhythm disturbances
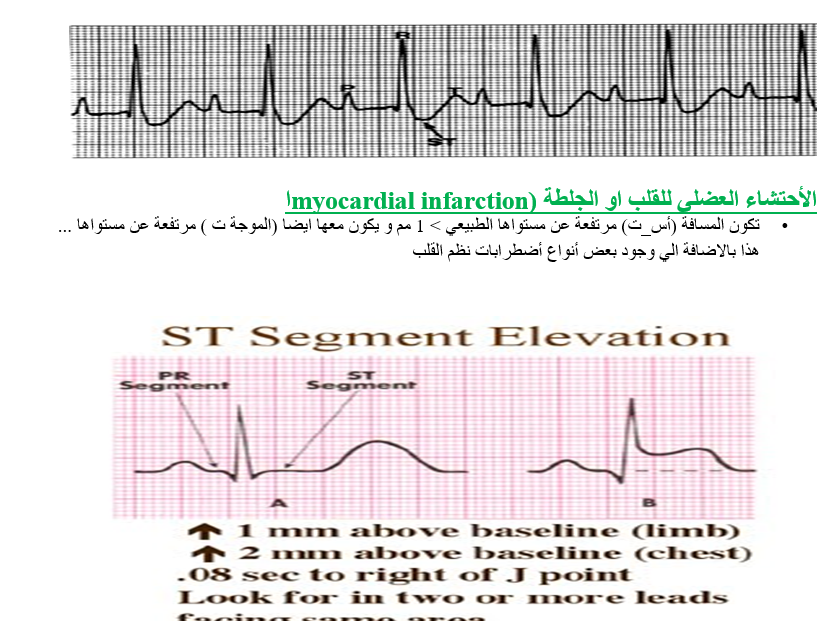
• If it is present in:
• 1. lead I, aVL) so this is a lateral infarction.
• 2. II,III, aVF) This is an inferior infarction.
• 3. V1-6) This is an anterior infarction.
• If the clot is old, it is characterized by the Q wave being 4 mm deeper than its level and 0.04 seconds wider. This is important for diagnosing an old clot.
• The EKG is one of the very important tests that medicine cannot do without or replace with another test... As we explained, it is very important in diagnosing many cases. It is important in diagnosing heart diseases resulting from high blood pressure, rheumatic fever, and birth defects. An ECG is often taken while the patient is lying in bed, as we talked about, and this method is called a resting ECG. This picture may be taken while the patient is exerting himself, and this test is called a stress electrocardiogram. It shows whether the heart is receiving enough oxygen during vigorous activity. Doctors use a stress EKG to diagnose coronary artery disease, in which the arteries supplying the heart muscle have narrowed to a dangerous extent, restricting blood flow.
- Anatomy of the circulatory system
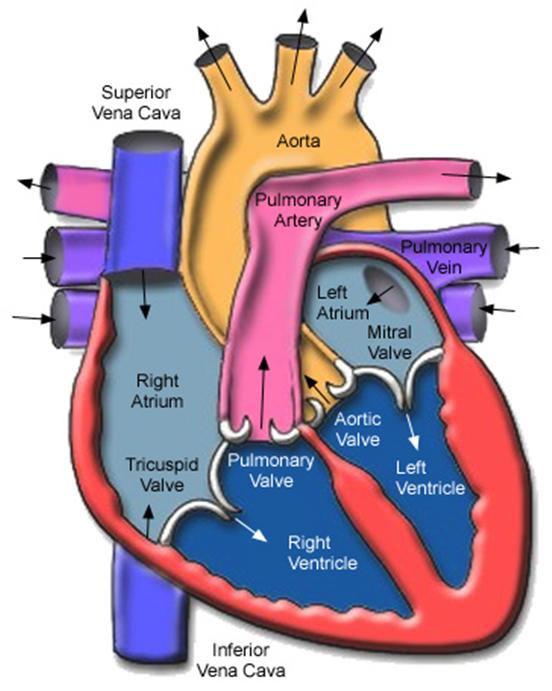
It is a device that performs the following functions:
- Distributing oxygen, nutrients and hormones to all parts of the body through the blood.
- Returning blood carrying carbon dioxide and metabolic waste from various parts of the body to the heart
- Transferring impure blood to the lungs to get rid of carbon dioxide and absorb oxygen, as well as transferring blood to the kidneys and excretory organs to get rid of metabolic waste.
The circulatory system consists of:
The heart
The blood
Blood vessels
The heart :
A hollow muscular organ the size of a master's fist. It is located in the middle of the chest cavity between the lungs, slanted to the left. It is surrounded by a pericardial membrane that protects it from friction and facilitates its movement. It consists of a special muscle tissue that has the ability to contract and relax throughout life. The heart works as a pump to push blood into the blood vessels until the system The department has the function of distributing blood to all parts of the body.
Heart shape:
The heart is roughly pyramid-shaped, with an apex, a base, and three surfaces.
Top of the heart:
It heads to the left and below the heart and is located in the normal state directly under the nipple of the left breast in the distance between the fifth and sixth ribs, about 9 cm from the anterior half line, and it consists of the tip of the left ventricle.
Heart base:
It projects upward and consists of the right atrium and the left atrium
Heart surface:
1- The front surface
It is located behind the sternum and the cartilages of the second to sixth ribs, and its composition is shared by the right atrium, the right ventricle, and a small part of the left ventricle.
2- The lower surface
It rests on the diaphragm and consists of the left ventricle and part of the right ventricle.
3- The left surface
It consists mostly of the left ventricle and part of the left atrium.
Departments of the heart:
The heart consists of four chambers, two atria and two ventricles. The right and left atrium are separated by a barrier called the interatrial septum. The right and left ventricles are also separated by the interventricular septum.
There is an opening between each atrium and its ventricle, called the aperture between the atrium and the ventricle. It is guarded by a valve that allows blood to pass from the atrium to the ventricle and does not allow it to return in the opposite direction. It can be divided into right and left halves.
1- Right half:
It consists of the right atrium and the right ventricle and pumps impure blood carrying carbon dioxide.
2- Left half:
It consists of the left atrium and the left ventricle and pumps pure blood and carries oxygen.
Heart chambers:
1- Right atrium:
Impure blood reaches it from all parts of the body through:
A- The superior vena cava from the upper part of the body.
B- The inferior vena cava of the lower part of the body.
C- Coronary venous sinus: from the heart.
The atrium pushes the impure blood into the right ventricle through an opening guarded by what is called a ventricle
Three-cuspid valve.
2- Right ventricle:
It receives impure blood from the right atrium and then pushes it to the lungs through the artery
The lung, whose beginning is guarded by a valve called the 'pulmonary valve'
3- Left atrium:
It receives fresh blood from the lungs through four pulmonary veins and then pushes it to...
The left ventricle through an opening guarded by a bicuspid valve called the mitral valve.
4- Left ventricle:
Pure blood reaches it from the left atrium and then pumps it to all parts of the body through
The aorta, whose beginning is guarded by a valve called the 'aortic valve'. It is noted that the walls of the atrium are less thick than the walls of the ventricle, which pushes blood to all parts of the body.
5-Blood vessels:
The heart is supplied with blood by two small arteries called the coronary arteries
The coronary blood flows from the beginning of the aorta, while the impure blood returns to the heart either directly or through the coronary venous sinus.
6- Heart nerves:
The heart feeds the involuntary nervous system with sympathetic nerves, which specialize in increasing the speed and strength of the heartbeat, and parasympathetic nerves, which reduce the speed and strength of the heartbeat. However, it must be noted that the heartbeat itself is due specifically to the properties of the heart muscle and does not require any nerves to perform it.
7- Pericardial membrane:
The heart and the large blood vessels connected to it are surrounded by a membrane called the pericardium.
This membrane consists of two parts:
1- A fibrous membrane on the outside protects the heart and connects it to the sternum.
2- A thin membrane with two layers
A- The parietal layer lines the fibrous membrane from the inside.
B- The visceral layer covers the outer surface of the heart and is located between the two layers
A narrow capillary space containing a viscous fluid that facilitates the movement of the heart and reduces its friction
The blood circulation is divided into:
1- Minor (pulmonary) circulation, in which the blood is purified in the lungs and then returns to the heart.
2- Greater (general) circulation, in which pure blood is distributed to all parts of the body
Then the pure blood returns to the heart.
3- The portal cycle, in which blood loaded with nutrients passes from the digestive canal to the liver
From there to the inferior vena cava.
1- Microcirculation:
Impure blood from all parts of the body reaches the right atrium, which contracts and pushes the blood through the opening of the three-cuspid valve into the right ventricle. The three-cuspid valve closes and the blood rushes through the pulmonary valve to the pulmonary artery, which divides into two branches, each of which passes to one of the lungs.
The blood is purified in the lungs, getting rid of carbon dioxide and gaining oxygen. Then the purified blood returns to the left atrium through four pulmonary veins.
2- Greater circulation:
The left atrium contracts, pushing blood through the mitral valve into the left ventricle. The left ventricle contracts, closing the mitral valve, and blood rushes through the aortic valve to the aorta, which distributes pure blood to the heart and all parts of the body.
Impure blood collects and then returns to the right atrium via the superior vena cava, inferior vena cava, and coronary venous sinus.
3- The papal session:
Impure blood collects from the digestive tract, loaded with nutrients after they are digested and absorbed, and then passes into the portal vein, which carries it to the liver.
The portal vein in the liver divides into capillaries, and thus the blood passes through the liver cells, where some metabolic processes take place.
The capillaries gather again to form small veins that end in the two hepatic veins that drain into the inferior vena cava, and thus the blood returns to the greater circulation.
4- Blood vessels:
Blood vessels are the tubes that transport blood from the heart to the body's organs and then return blood from the body's organs to the heart. Blood vessels are divided into arteries and veins.
The blood vessel consists of three layers:
1- A smooth inner layer that is in direct contact with the blood.
2- An intermediate layer composed of involuntary muscles that control the expansion and constriction of vessels
Blood flow as needed, and it is thicker in an artery than in a vein.
3- Fibrous outer layer.
Arteries:
The artery is the blood vessel that carries blood from the heart to the organs of the body. All arteries carry pure blood, except for the pulmonary artery and its branches, which carry impure blood. All the arteries of the body except the pulmonary artery arise from a common trunk, which is the aorta, which starts from the left ventricle and then gives branches that divide into smaller arteries. It gets smaller until it ends in the various organs with tiny blood vessels called adjacent capillaries to form braids of capillaries that nourish the tissues with different cells. From these braids begin the tributaries of the veins that come together to form larger and larger veins, and in the end the superior vena cava and the inferior vena cava are formed, which open into the right atrium.
Veins:
The vein is the blood vessel that carries blood from the body's organs to the heart. All veins carry impure blood except for the four pulmonary veins, which carry pure blood from the lungs to the left atrium.
Blood circulation :
This cycle lasts 8 of a second and includes three turns.
1- Contraction cycle:
It begins with the contraction of the right and left atria, and the blood passes from each atrium to the corresponding ventricle through the valves between the atria and the ventricles. Then the ventricles contract and these valves close, and the blood passes from the right ventricle to the pulmonary artery and from the left ventricle to the aorta, thus ending the cycle of contraction.
2- Relaxation cycle:
The contraction cycle follows, during which the heart muscles relax, the pressure inside its chambers decreases, and the pulmonary and aortic semilunar valves close to prevent blood from returning to the ventricles.
3- Rest cycle:
The relaxation cycle follows, in which impure blood flows from the hollow veins to the right atrium, and pure blood flows from the pulmonary veins to the left atrium until the atrium is filled with blood.
Heartbeat :
In the normal state in adults, the heart contracts 72 times per minute and in a newborn child about 120 times per minute. The heart’s contractions are reflected in the arteries because they are rubber tubes, causing waves that determine the pulse. Feeling the pulse can determine the state of the heartbeat in terms of speed, strength, and regularity. The best place to feel the pulse is The radial artery is located directly under the skin in front of the lower end of the radius.
Heart sounds:
The heart has two basic sounds in each beat or beat, known as the first sound and the second sound.
First voice:
It is longer and lower in intensity than the second sound and is heard in the form of a 'pulp' and is caused by the contraction of the heart muscle and the closing of the valves between the atrium and the ventricle forcefully at the apex of the heart, about 9 cm from the front half line in the distance between the left fifth and sixth ribs.
Second voice:
Farther and more intense than the first sound and it is heard in the form of a 'bear' caused by the closing of the pulmonary artery and aortic valves. This sound is heard on both sides of the sternum in the space between the first and second ribs. In some pathological conditions that affect the heart valves and distort them, these valves narrow or recoil and the heart sounds become It is abnormal and is caused by what is called heart murmur.
- Nursing care for angina patients
The Definition:
• It is when the heart muscle suffers from a sudden, severe decrease in the oxygen necessary for its functioning due to insufficient myocardial perfusion. Men are more susceptible than women, especially between the ages of fifty and fifty-eight.
Types of angina:
There are many different types:
1- Organic angina attacks (alarming syndrome):
The pain suddenly strikes the patient while resting, without any significant effort, and in the form of multiple and increasing attacks. This type is dangerous, as the pain may sometimes last for twenty minutes or more, and a nitroglycerin tablet may have no effect sometimes.
2- Constant stable angina pectoris:
This type can move, over a period of time, to a stage in which the patient adapts to his illness, and the time factor has played a role in the division and allowed the two compensating lateral divisions to grow. Thus, attacks of pain occur only rarely, and if they do occur, they are mild, and medical treatment often protects the patient and helps to provide complete comfort for the patient.
3- Cases of recurrent angina:
In this type, the patient suffers from more than one seizure per day, and his intake of nitoglycerin tablets increases, one after the other, until it sometimes reaches ten or twenty pills per day. This condition can last for several weeks, but one of two things is assumed to occur. Either it is an expression of multiple infections. It is important for the trunks of the three arteries, or the injury is normal, but the patient presents to it with an anxious disposition and a distinctive nervous state.
4- Convoluted or 'camouflaged' seizures:
These cases are of special importance, and we mean seizures that occur in patients suffering from problems and medical conditions other than coronary insufficiency. Pain in such cases often indicates, in its extension, times of occurrence, and changes, the location and causes of the injury or disease in question, as is the case, for example, in cases of rheumatism of the cervical spine (disc) or disorders of the digestive system, such as in stomach ulcers, and it must be investigated whether these conditions alone are responsible for what is happening. Is it a symptom or does it actually correspond to real coronary insufficiency, which increases its severity and importance?
Signs and symptoms of angina:
Angina pectoris attacks its owner in the form of painful attacks, and the pain appears in the front of the chest and behind the sternum. It grows and develops, but remains in the middle between the breasts, or spreads upwards towards the top of the sternum and neck, or towards the lower jaw on its side. The left arm often gets its share on the inner side opposite the torso, or in a Ring around the other two fingers of the left hand.
Most of the time, the pain is squeezing, and sometimes it is crushing, or it forms pressure or a pincer applied to the chest with force, or tightness, stretching, or heaviness on the chest, sometimes leading to a fire inside it.
The person is pale in color - increased sweating, an increase in the number of heartbeats, and heart disturbances.
Diagnostic methods for angina pectoris:
1- Medical history:
In it, the patient is given a complete history of his illness, in which the patient is described about the seizure and whether it accompanies effort/nervousness or after eating a fatty meal, in which the characteristics of the pain, its location, duration, and the areas in which it is tolerated and removed are described.
2- Chest X-ray:
It appears if there is an enlarged heart or congestion in the lungs.
3- Arteriography:
The patient is examined to diagnose him and select the patients for whom the by-pass (aortic-coronary) junction procedure is performed.
4- Stress EKG:
In it, the patient makes an effort while riding a certain bicycle or while walking in place on a moving electric carpet and in the opposite direction to his walking or climbing the stairs. As a result, there is an increase in the heart rate, blood pressure, and heart function, and then angina pectoris pain or changes in the electrocardiogram appear.
5- Normal EKG:
There is a decrease in the St Segment, and this occurs with T wave invsesion
Medical treatment for angina
1- Aspirin:
It works to prevent platelet aggregation and thus reduces the incidence of stroke and reduces the incidence of death in patients with angina.
2- Heparin:
It is given to prevent the occurrence of a clot, and 5,000 units are given intravenously every 4 to 6 hours, while an EKG is continued to determine the effectiveness of the action of heparin. PTT or PT is done two hours after heparin is given if it is given intravenously, every 4 hours and then daily.
3- Medications treating angina pain (Nitroglycerin) Nitroglycerin:
These medications appear to:
1- They increase the expansion of the arteries and thus their ability to carry a larger amount of blood. These medicines and many other medicines, on the other hand, are considered by dilating the small arteries of the heart to help in the emergence and growth of the network of collateral arteries that carry blood to the places that lack perfusion and are called (the two collateral divisions). They also By expanding the surrounding body vessels, which reduces the pressure within them and thus the burden placed on the heart. These drugs enter into the work of the second category of drugs whose work is limited to reducing the work of the heart muscle and reducing its consumption of oxygen.
2- Beta adrenergic blocking:
These medications are considered of great importance as they have the ability to reduce the number of heartbeats, blood pressure, and contractions (cardiac muscle). They also reduce the heart muscle’s need for oxygen. They also have the ability to prevent the occurrence of heart rhythm disturbances (arrhythmias) and reduce the incidence of heart attack and death. The sudden. Example tenormin.
5- Calcium channel blocking:
This group is considered one of the most important medications that have the ability to reduce the contraction of the heart muscle and relax the fine muscles present in the coronary and peripheral vascular smooth muscle. They also have the ability to control chest pain in unstable angina. Example: Thiazem.
6- Surgical treatment (aortic-coronary “bridging” operation):
It was given this name because it requires removing a vein from the patient’s own thigh, the “rotten vein,” and placing it as a bridge between a place in the aorta and another in the atherosclerotic coronary artery after the site of the narrowing in it.
After the transplantation process, blood flows through this venous 'air' bridge from the aorta, where the blood rushes forcefully towards the concerned cardiac muscle through the rest of the affected artery itself, leaving the narrowing itself alone and compensating for it by increasing the perfusion of this muscle and supplying it with oxygen.
- Nursing care for a heart attack patient
Heart attack
The Definition:
Sudden, severe chest pain resulting from the blockage of one of the coronary arteries, most often by a blood clot, which deprives part of the heart muscle of blood supply, leading to its necrosis and death. The dead tissue may dissolve after a few weeks due to an adherent relationship.
1. A heart attack is the result of a complete, acute and sudden deprivation of the myocardium, or part of it, of blood and oxygen due to the blockage of one of the coronary arteries by a blood clot in most cases. This leads to infarction, necrosis, and death in some of them, to varying degrees in depth and breadth.
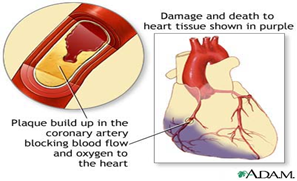
The Reasons:
1. The most important cause is the occurrence of a clot in the coronary artery supplying the heart muscle, which reduces the amount of blood reaching the heart muscle.
2. As a result of fatty accumulations that continue to deposit over time on the walls of the coronary arteries.
3. A blood clot dislodges and travels with the bloodstream until it reaches a point in the artery that is too narrow to allow its middle to pass, so it stops there and blocks it.
4. The presence of risk factors that lead to coronary artery disease (age - gender - high blood pressure - cholesterol - sugar).
Signs and symptoms :
Chest pain is not related to effort except rarely (in only about 10% of all cases). It occurs behind the sternum in the middle of the chest, and constitutes severe pressure or crushing, but in terms of its wide spread and extension, it may include the jaws, shoulders, arms, and even the middle of the back, and sometimes the area Stomach.
Duration: It may last hours and sometimes a day or more:
1. Nitroglycerin tablets have no effectiveness or significant effect on the pain of a heart attack, and this is what distinguishes it from the pain of angina pectoris.
2. Stomach upset or indigestion, especially if accompanied by nausea or vomiting.
3. A deep and intense feeling of anxiety, confusion, and fear of the inevitable death of a relative.
4. Changes in the number and regularity of heartbeats.
5. Mild headache - difficulty breathing - low blood pressure accompanied by pain, severe sweating and a feeling of weakness.
6. An increase in temperature between 37.7 and 39. It rises about 24 to 48 hours after the stroke occurs and returns to normal within 6-7 days.
7. Skin color is grey, cool and moist.
Diagnostic methods for myocardial infarction:
1. An increase in cardiac enzymes (cpk), especially MB - cpk, reaching a maximum increase in about 24 hours, LDH.
2. Signs and symptoms.
3. Arteriography and cardiac catheterization are performed, but this is postponed until the patient's condition stabilizes.
4. An increase in the number of white blood cells within a few hours of the onset of pain, reaching 12,000 - 15,000 for a period of 3-7 days.
5. An increase in the erythrocyte sedimentation rate in the first week after the clot occurs, and it remains high for about 7 weeks.
6. Changes in the electrocardiogram: An increase in the ST segment occurs and may last about two weeks, T wave inversion and Q wave.
Analysis of cardiac enzymes:
1. Creatine phosphokinase is specific to the heart only. It begins to rise 2-4 hours after the stroke occurs, reaches its peak after 14-36 hours, and returns to normal after 3 days.
2. Serum glutamic oxalocatic transominase SGOT begins to rise after 8-12 hours, reaches its peak after 18-36 hours, and returns to normal level after 3-5 days.
3. LDH Lastic dehydragenase starts to rise after 8 – 48 hours, reaches its peak after 3 – 6 days, then returns to normal after 4 – 8 days.
Complications of heart attack:
1. High blood pressure as a result of pain or the first signs of heart failure and usually responds to treatment.
2. Complete heart block: Complete blockage of the heart's electricity occurs in about 6% of cases of heart attack. It may occur within a few hours of the stroke occurring in about a third of these patients. This happens to most patients within 48 hours and rarely after 4 days.
3. Cardiogenic shock: occurs in about 5% of cases. Dopamine is usually given in such cases (cardiogenic shock).
4. Heart failure, which is defined as the amount of blood pumped by the heart is insufficient to meet the needs of the heart. It is characterized by fluid retention in the body and swelling in the legs (Oedema).
5. Ventricular dysfunction, which can lead to cardiogenic shock, which is the main cause of death during hospitalization.
6. Some patients may develop a group of symptoms approximately 1-6 weeks after the stroke, which are characterized by pain in the pleural lining, joint pain, and high temperature, as a result of an autoimmune reaction. Aspirin may be effective in this case, and in some cases you need Cortisone.
7. Mitral valve regurgitation.
8. Pericaditis, an inflammation of the lining of the heart that may occur within 24 hours. The pain increases with breathing and may go away when sleeping on the right side.
9. Dysrhythmias are found in about 50% of cases and occur as a result of ischemia or a difference in treatment.
Medical treatment for heart attack:
1. The patient must be admitted to cardiac intensive care, and the following must be done:
A- Connect the patient to the monitor and perform an EKG
B- Delivering oxygen to the patient
C- Installing a cannula and taking blood samples to perform heart enzymes.
D- Giving medications that are used to reduce the size of myocardial infarction resulting from coronary artery thrombosis.
2. Treating pain and providing psychological and nervous balance:
Effective and rapid action to relieve the patient of his pain is considered the first and most important thing, on the one hand, because of the pain itself, and on the other hand, because of the anxiety and disturbance that the patient experiences, which may even lead to the fear of inevitable death. Among the analgesic drugs, we resort to the fastest-acting or most effective drugs, such as morphine and its derivatives, as well as nervous and psychological tranquilizers.
3. Treatment of emergency deficiency in cardiac perfusion:
1. Myocardial infarction is only the result of a severe and complete deficiency in its perfusion and in supplying it with the necessary oxygen for its functioning. Therefore, it is necessary to give the patient oxygen and arterial dilators (nitroglycerin) at regular and close times to dissolve under the tongue, and later, or even at the same time, and permanently, the patient takes moderate arterial dilators. The long-term effect lasts the longest, up to approximately 12 hours.
Tridil is prepared in a 5% glucose bottle, not a plastic packet, because it is deposited on the plastic wall. Tridil is calculated according to the pressure and pulse of the patient’s sense of pain, and Tridil is stopped gradually.
4. Rest in the acute phase of a heart attack:
As soon as the patient arrives in intensive care, the first thing that is done quickly, completely and effectively is in the form of intravenous or subcutaneous injections at regular times and under careful laboratory and laboratory monitoring, such as PTT, which we order and ask of him, is to immediately lie down in bed and have complete and absolute rest, especially in the first days.
5. Thinning or preventing blood clotting:
1. Streptokinase:
It is a medication that is given within the first 6 hours for chest pain resulting from a coronary artery clot. It works to dissolve the clot and thus reduce its effect.
Medications that should be given with and after streptokinase:
1- Hydrocortisone - Slocutive
Because streptokinase is made from some bacteria, it causes an allergic reaction in the body after it is given, and hydrocortisone works to reduce the allergy associated with it.
2- Heparin:
Nursing note when administering streptokinase:
1. Observing the patient’s pressure and pulse, as well as noting the patient’s complaint of shortness of breath - vomiting - profuse sweating - scratching. This occurs as a result of an allergy to it, and in this case, an overdose of salt solution - hydrocortisone is given.
2. The anti-streptokinase drug is cilokapron and is given in case of allergy to streptokinase.
Contraindications:
1. The presence of any recent bleeding, for example (varicose veins - stomach ulcers - bleeding hemorrhoids).
2. There is a history of brain hemorrhage.
3. Patients older than 70 years of age so that brain bleeding does not occur.
4. During pregnancy.
Caring for patients with death of part of the heart muscle
The whole world suffers from this disease, and the death rate due to this disease is high all over the world, and deaths are common among men aged (40-70 years).
Deaths are rare among women before menopause, and of course when we talk about the causes of heart muscle death, we attribute this to the same causes as atherosclerosis.
The meaning of the death of the heart muscle is that it loses its function and function and becomes useless because of something simple (a clot) that closes an artery that feeds the heart muscle, preventing the blood from reaching it, so the muscle in this part dies, and this part of the heart becomes fibrotic, its cells change, and the life of this part changes, and it is usually in the left ventricle. The septum between the ventricles has a thick wall and high blood pressure. Of course, the location of this injury and the extent of its extension depends on the affected artery, and on the efficiency of the side arteries to divide blood into the heart (usually the left coronary artery).
Symptoms:
- Acute pain occurs suddenly and is not preceded by stress or tension (or what precedes angina). The pain intensifies and its peak intensity is behind the sternum and spreads to reach the middle of the chest, neck, jaws, the area of the so-called (stomach mouth), and both shoulders, especially the left shoulder and left arm. .
- The pain is similar to angina pain in its characteristics, location, and spread, except that it is more severe and longer.
- The pain exceeds hours and sometimes extends for a day or two, and does not improve or disappear with rest or with that pill under the tongue.3
- The pain may precede angina, or the pain may be severe from the first moment.
- The pain is accompanied by profuse sweating, and sometimes this is accompanied by nausea or vomiting.
- Our final evidence that part of the heart muscle has become fibrous (death) is the characteristic electrocardiogram of this condition.
Complications:
- The patient suffers from some complications, the most important of which is heart disease, irregular heartbeat, and an increase in heart rate (70-80% per minute).
- Heart failure, and a defect in the heart valves (mitral valve) in particular, and the formation of small clots, the effect of which we see in those who rest for a long period of time during illness, so clots appear in the legs and thighs.
- Sometimes swelling occurs in some parts of the heart, which leads to heart failure, the formation of small clots, and irregular heartbeats.
- Submembranous hemorrhage may occur, leading to sudden death.
- The fate of patients with myocardial fibrosis or death is divided between death (sudden death in a fifth of the cases) and before they go to the doctor or the doctor goes to them.
- Another five occur within a month after the crisis (as a result of complications of the condition).
- Others (about 60%) do not show symptoms, or they may be attacked by angina attacks.
Treatment:
· To deal with the patient, we must know that if the patient is given complete physical and psychological rest, he will automatically improve, and it is known that the purpose of giving drugs is to relieve symptoms and prevent or deal with complications.
· He must deal with the pain and he must deal with it immediately and deal seriously and carefully (morphine at that time is the solution) or its alternatives with the knowledge of the doctor (10 milligrams intramuscularly or intravenously), and repeat if necessary. The doctor must note that the doses given in the first twelve hours do not exceed (60 milligrams) so that the patient’s respiratory system does not collapse or bouts of vomiting occur.
· Rest is very necessary for improvement to occur, and this rest may take a long time, so side effects of prolonged sleep in bed must be taken into account, such as: (bed sores - clots in the legs - pneumonia - urinary retention - constipation... etc.).
· The period of rest in cases that are not accompanied by complications (rest from work after this period) is about 3 weeks, and in the event of complications it is 6 weeks, and the patient is given a mild sedative to reduce his anxiety or a sedative.
· The patient’s food should be taken into account, especially in the first weeks. It contains fewer calories, less salt, is light and easy to digest, and small quantities (frequent meals).
· Complete abstinence from tea, coffee, and smoking, especially in the early stages.
· It is recommended to place the patient in the hospital’s intensive care room to deal with the condition in a timely manner, and to follow up on complications and medical treatment of them.
Care of coronary artery disease patients
Continuing nursing care in the intensive care unit is considered vital until the patient's condition stabilizes. Nursing staff members should note the following:
1. Observing vital signs such as pulse, breathing, temperature and blood pressure.
2. Complete bed rest.
3. Moving the legs to avoid leg stroke.
4. Execute the treatment exactly as the doctor ordered and note the side effects of the medication.
5. Assess and observe incoming and outgoing fluids.
6. Good observation – Difficulty breathing – Discomfort – Chest pain – Food – Medications given.
The nursing staff must make some observations on the patient so that they can evaluate his condition and detect early complications. The observation must be either direct, such as looking, hearing, and touching the patient, or indirect, such as measuring blood pressure and using a monitor. The observation of the patient must be complete, from head to foot, as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Duties of nursing staff:
1. Nursing staff must direct their efforts towards early detection of complications, preventing other injuries to the heart muscle, and giving the patient a sense of comfort.
2. Continuous observation of the monitor while the patient is in the intensive care unit in intermediate care and the ability to interpret and read the ECG to investigate complications and heart rhythm disturbances.
3. Regarding the occurrence of an obstruction in the process of gas exchange: Nursing staff must be aware of the signs of lack of oxygen in the brain, hypoxia, which are considered to be: blood pressure - heart rhythm disturbances - difficulty breathing - dizziness - headache - lack of balance - nausea - anxiety - A feeling of discomfort, so she must inform the doctor.
4. Giving the patient oxygen according to his condition: The nursing staff must take care of the mouth, teeth and lips, which may cause cracks as a result of the use of oxygen (cream).
· Nursing staff must: Listen to the sound of breathing - and count the number of times, depth, and rhythm of breathing every 1 hour.
· Giving the patient diuretics: while monitoring body salts.
· To relieve chest pain: Nursing staff must evaluate and record a complete description of the pain and the activity performed to determine the cause of the pain.
· Complete rest for the patient to reduce oxygen consumption.
· Do an EKG during pain.
· Giving pain relievers and arterial dilators.
· Nursing staff must encourage the patient to stop smoking because it is a major cause of the disease.
· Giving nursing care to a patient who suffers from vomiting and nausea, including:
· Place the patient in a comfortable position (half-sitting). Place a renal pelvis next to the patient.
· Recording and reporting the contents, colour, quantity and smell of vomit.
· Give small, frequent meals and fluids.
· Administer antiemetic medications as ordered by the doctor.
· Oral nursing care.
5. Regarding food: The patient may be placed on a special diet according to his condition, such as reducing salt to different degrees, such as in high blood pressure and edema, as well as reducing fat and cholesterol, as in the case of patients with high cholesterol, as well as reducing calories, and that food should consist of 5 to 6 small meals. Fat-free, and also avoid foods that lead to the formation of gases and abdominal bloating. You should also avoid very hot or very cold food.
6. The nursing staff must help the patient reduce the level of anxiety and disturbance by reassuring him, making him feel comfortable, encouraging him to express the fear inside him regarding his illness, and helping him to adapt to his medical condition. Nursing staff must encourage the patient to do some activities in order to reduce his fear, such as reading newspapers or books.
7. Regarding sexual activity: There are some tips that nursing staff must give to the patient in order to help him and his wife feel pleasure and satisfaction in the sexual relationship while reducing the effort on the heart:
· Adequate rest before sexual intercourse.
· Find a comfortable position for him and his wife.
· Take some drugs, such as nitroglycerin, before sexual intercourse to prevent chest pain.
· Postpone sexual intercourse for 1 - 1 ½ hours after eating a heavy meal.
· Inform the doctor of some symptoms if they occur during sexual intercourse, such as:
- Increased heart rate and continues for more than 15 minutes.
- Chest pain that did not respond to nitroglycerin.
8. The nursing staff must advise the patient to avoid violent muscle and mental exercises and to perform some moderate exercises that do not cause chest pain, such as walking, which begins in a short distance through the room and then begins to increase gradually over a period of a week, with continuous observation from the doctor.
9. Helping the patient with excretion: The vast majority of patients may suffer from constipation:
◾ Nursing staff must give them fiber in the food provided to them and sufficient fluids.
◾ Preventing spicy foods and giving laxatives.
◾ Giving the potty to patients who are not allowed to move, taking into account individuality and confidentiality.
◾ Make a plan for the activity according to the situation and what is permitted.
10. With regard to the lack of information about the patient about the nature of the medication, the time, the dose, the number of times it is taken, the side effects, and its expected drug effect, the nursing staff must explain to the patient the action, dose, time, and side effects of the medications he is taking, and urge the patient to repeat this information:
◾ Encourage the patient to take a break if he feels dizzy after taking medications.
◾ The patient must record the number of times chest pain occurred and the medications he took, the dosage and number (Isordil).
◾ Avoid alcohol derivatives while taking the medication.
E Note the side effects of the medication and inform the doctor.
11. The nursing staff must develop or plan an educational program for each patient individually when he is discharged home (for the patient and his family), which includes:
◾ Controlling various risk factors and the extent of benefit from that.
◾ Sexual activity.
◾ Medications given (name - dosage - effectiveness of the medication - side effects).
◾ Develop an exercise program to do at home.
◾ The importance of follow-up and departmental medical examination. Signs and side effects that require consulting a doctor (chest pain that does not go away with the use of nitroglycerin - palpitations - irregular heartbeat - dizziness).
◾ Teaching family members the steps for cardiothoracic resuscitation.
◾ The importance of taking nitroglycerin before engaging in any activity or effort.
◾ Pulse counting methods.
◾ Eat foods low in salt, cholesterol, and fat and control calories.
◾ Health education for Pacemaker patients.
◾ Guiding the patient’s family on the importance of providing a nice, calm atmosphere filled with love and respect. Respect the person and do not use negativity with him, but rather use means of reason and understanding, provided that this is within the scope of the doctor’s recommendations and instructions.
◾ With regard to work, one must avoid putting in any effort, whether physical or psychological, and try to replace stressful tasks with others that are less strenuous if possible.
◾ His daily life must be far from noise, disturbance, and stress, and this does not mean isolation and staying away from people.
◾ The patient must take adequate daily rest.
◾ The residence must have all the characteristics in terms of its atmosphere being calm and well ventilated, allowing air and sun to enter.
◾ The water when bathing should be lukewarm, neither cold nor hot, and for a short period of time, while long standing and tiring positions must be avoided during it.
◾ As for the visit, it must be a source of comfort, reassurance, and joy for the patient during his home recovery. The number of visitors should be small, the duration of the visit should be as short as possible, and it should not be subject to boring discussions and conversations or arousing sensitivity and enthusiasm.
- Nursing care for a heart failure patient
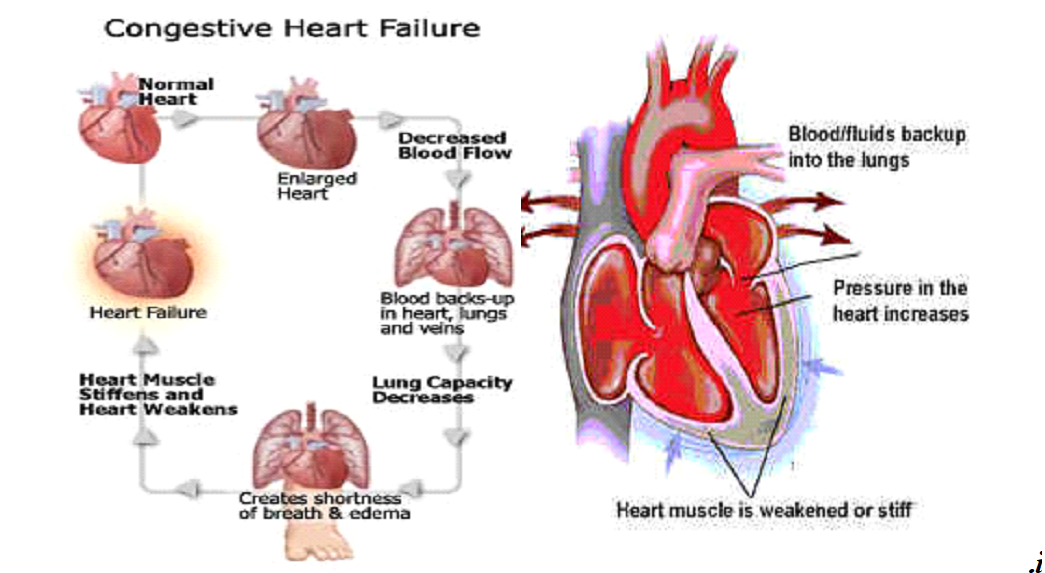
The Definition
It is a failure of the heart muscle to pump an appropriate amount of blood to meet the body’s need. This decline can either be an acute decline that leads to a sudden stop of the heart muscle pumping blood, which results in blood. Or it can be a chronic decline that occurs gradually and its symptoms are mild. Heart failure is characterized by the occurrence of compensating factors to compensate for the heart failure. like
· Rapid heart rate
· Heart enlargement, especially ventricular hypertrophy
· Ventricular dilatation
· Abnormal amounts of blood accumulate in the respiratory system. Pulmonary congestion
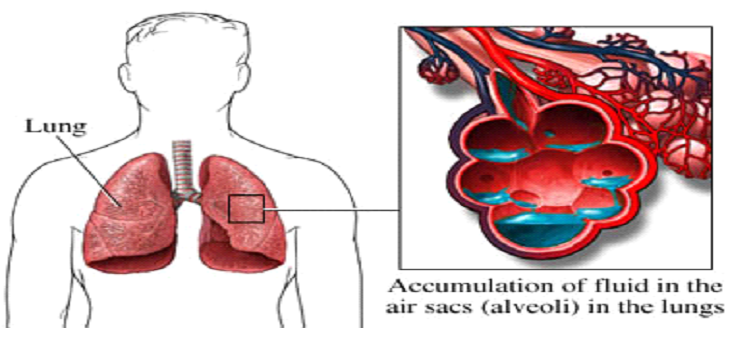
Its causes
Heart failure occurs if one or more mechanical causes combine
1 - The amount of blood supplied to the heart is small as a result of bleeding and dehydration
2 - The amount of blood supplied to the heart exceeds what is necessary due to the large number of solutions
3 - The amount of blood entering the heart is small as a result of narrowing in one of the valves or arteries
4- Injury of any kind to the heart muscle itself
5- Increased nutritional needs of the body as a result of high fever or pregnancy
The goal of heart failure care
The main goal is to eliminate or reduce the causes that lead to the disease
1- Complete physical and muscular rest
2 - DIGITALIS Digoxin
3 - Suitable for a fatty meal, Sodium, Potassium
4- A dilator for arteries and veins
5- Reducing the accumulation of water and sodium inside the body by following the following methods
· a - Sodium in meals
· b - Diuretic
· c - Reducing the amount of fluids entering the body
· d - Reducing stress for the patient
6- Giving the patient oxygen
7- Removal of pleural effusion and peritoneal effusion
8- Tell the patient everything about his illness and how to deal with it
Section Nursing personnel towards illness
1- Place the patient in a quiet, cool room to help him sleep
2- Place all things within the patient’s reach
3- Keep the patient in a comfortable position constantly
4- Trying to reassure the patient about his health
5 - The patient talked about the importance of rest when he returns home
6 - Defining the patient's symptoms of digitalis poisoning
- Nausea - vomiting - diarrhea - headache - depression - tension - dizziness - spasms - hallucinations - memory loss - increased or decreased heart rate - urticaria.
- If any of the above symptoms occur, treatment must be discontinued
- Giving the patient potassium chloride
Must before giving digitalis
1- Taking the patient’s pulse for a full minute with the stethoscope on the patient’s chest
2 - We carefully observe the heart rate if it is regular or irregular and record it
3 - If the patient’s pulse is fast, less than 60 beats per minute, the dose should be stopped and the doctor should be informed.
4 - The patient must be carefully observed for any symptoms of Vitalis poisoning
5-The patient should be given meals rich in potassium
Avoid giving the patient any food that contains sodium salts, such as peanuts or chips
Avoid salt at all
6- Weigh the patient every day at the same time and on the same scale, usually before breakfast
7- Take care of the patient’s skin because swollen skin is more susceptible to cracking
8- Oxygen therapy in case of difficulty breathing
9- An internal and external fluid map must be done
Shock
introduction
The main reason for shock is the lack of sufficient oxygen reaching the tissues, as well as the failure of them to get rid of harmful substances resulting from the metabolic process. Shock also occurs after accidents or injuries as a result of a decrease in blood volume or fluids in the body as a result of bleeding or severe diarrhea, which also leads to a decrease in body volume or As a result of a sudden injury accompanied by severe pain, the shock is divided according to its types into surgical shock and nervous shock. The shock is also divided according to the time of its occurrence into primary shock and bilateral shock.
Shock :
A decrease in the amount of blood that reaches the vital organs in the body, such as (the brain, heart, and kidneys), which leads to depriving the tissues of these organs of a sufficient amount of oxygen and nutrients carried by the blood.
Causes of shock
o The body loses a large amount of blood, as in cases of bleeding
o Acute heart failure
o The body loses a large amount of fluids, as in cases of severe diarrhea
o Severe pain
o Electric shock
o Poisoning and severe allergic reactions
Signs and symptoms of shock
o The affected person has a pale face
o The skin is pale or bluish in color and cool and clammy to the touch
o Increase in respiratory rate and breathing becomes shallow and irregular
o The pulse is fast, weak, or irregular
o Breathing is fast and shallow (the patient tries to take in the largest amount of oxygen from the air, which increases its speed and may be deep but irregular.
o Low blood pressure.
o A drop in temperature below 35 degrees Celsius.
o If you look at the injured person, you will find that he appears anxious and disturbed
o The victim complains of extreme thirst and may become nauseous and vomit
o In the final stages, the injured person loses consciousness
o Dilated pupils
Types of shock:
1- Surgical trauma:
It is a result of the loss of a large amount of blood, as in cases of severe bleeding, whether external, internal, or after operations, or as a result of the loss of a large amount of fluids in the body, which leads to a decrease in blood volume in the blood fraction, such as in cases of severe diarrhea?
2- Nervous shock:
It occurs in cases of severe pain, such as in first-degree burns, or as a result of emotional disturbance such as fear, or severe psychological emotions such as hearing bad news or being exposed to an accident even though there is no physical injury.
3- Initial shock:
It occurs at the time of an accident or sudden illness that is accompanied by severe pain.
4- Secondary trauma:
It may not occur until several hours after the accident or sudden illness, and usually
be dangerous.
Trauma first aid:
The injured person is treated immediately where he is located until he is transferred to the hospital or summoned
Ambulance for him.
1- Calm the patient down, do not move him, and treat any other injuries, such as fractures or wounds.
2- The injured person is placed lying on his back at the scene of the accident with his head on one side to avoid inhaling any secretions coming out of the mouth.
3- If he is in the house, raise the legs of the bed or lift the lower part of the body up so that the blood reaches the brain.
4- Loosen the ties and compressive clothing around the neck, chest and waist of the injured person and prevent crowding around him.
5- If the injured person suffers from injuries in different parts of the body, such as neck or spinal injuries, he must not be moved until he is transferred to prevent complications.
6- Warm the injured person naturally with additional blankets so that sweat secretion and loss of fluids from the body do not increase.
7- Do not give the injured person anything by mouth.
8- Alleviate the injured person’s pain by making him comfortable until he is transferred.
9- Observing the condition of the injured person and taking vital signs regularly until he is transferred to the hospital.
To treat shock, the doctor gives the injured person:
- In case of bleeding blood transfusion
- In case of burns, plasma
- In case of vomiting and diarrhea, Glucose and salt solution
Nursing care for circulatory system patients
The most important general symptoms and signs:
1- Pulse:
There may be a difference in rate, regularity, and strength. The pulse may be faster or slower than the normal rate, irregular, or its strength varies, depending on the case.
2- Breathing:
There may be a change in the rate, regularity, and depth, as well as the occurrence of abnormal sounds accompanying the breathing process. It is common in heart disease to have shortness of breath, especially when moving, or when chest pain occurs.
3- Pressure:
Arterial pressure is one of the important factors that shows the state of blood circulation. It is observed in heart patients a decrease in systolic pressure and an increase in diastolic pressure above the normal rate.
4- Patient’s colour:
There is a change in the color of the patient’s skin. Blueness or dullness may occur in the color, as well as blueness in the lips and nails. This condition appears as a result of a lack of oxygen in the bloodstream, which leads to a change in the color of the skin, lips and nails. The lack of oxygen may also affect mental and physical efficiency, causing dullness or dullness. Loss of feeling.
5- Chest pain:
It is noted that the occurrence of chest pain varies in type, severity, location, and cause of its occurrence from one case to another. The pain may occur when the patient exerts any effort or while resting. In some cases, the pain appears in the abdomen or stomach, and the pain may spread to the shoulder, arm, left or right hand.
6- Tumor:
It usually appears in the lower extremities, especially the feet, as a result of fluid accumulation. In some severe cases, it appears in the abdomen (ascites), which is a distinctive sign that there is pressure in the work of the heart.
7- Feeling the heartbeat:
The patient may feel and be alert to his heartbeat as a result of the change in heart function caused by the disease.
8- Cough:
The patient may develop a cough that may be wet and accompanied by a mucus secretion interspersed with air bubbles, or accompanied by blood in late cases of the disease.
The role of nurses in preventing heart disease:
1- Discovering cases among individuals who frequent it by noticing symptoms and signs of heart disease such as shortness of breath, cyanosis, swelling or swollen veins, and chest pain upon exertion.
2- Educating individuals to prevent disease by helping them form healthy habits, whether children or adults, through:
- Encouraging sports and physical activity, especially walking.
- Annual medical examination.
- Reducing the percentage of fats in food.
- Not smoking due to the high incidence of heart disease among smokers.
1- Providing the necessary care for patients, especially conditions that affect the heart, such as rheumatic fever, high blood pressure, and obesity.
2- Helping heart patients live with their disease by advising them on how to prevent the occurrence of problems or complications that may lead to heart failure, and how to organize their lives, activity, and diet, and advising them to observe moderation in work, exercise, rest, and entertainment, and to avoid mixing with infectious disease patients due to their weak resistance to disease.
3- Activate blood circulation to prevent clots by moving the lower extremities and encouraging the patient to do gradual exercises as soon as the patient’s condition allows for this.
Pulmonary infiltration:
The Definition:
Pulmonary infiltration is lung congestion as a result of an increase in the amount of blood in the blood vessels in the respiratory system, which leads to great difficulty in breathing. This infiltration often occurs as a result of failure of the left part of the heart, which results in difficulty in the return of blood from the respiratory system to the heart, leading to blood accumulation in the lung. It leads to pulmonary infiltration, which leads to the end of the patient's life due to suffocation
Symptoms
◾ Severe difficulty breathing, especially in the horizontal position
◾ Paleness in the face
◾ Increased heart rate
◾ Secretion of large amounts of phlegm mixed with blood
◾ Blueness
The primary goal of our care for this patient is to help the patient take the amount of oxygen he needs
This is done with my machines
1 - The patient sleeps at an angle of 90 or 45 degrees or sits in a chair because this position facilitates the patient’s breathing process
2- Providing the patient with 8 liters of humidified oxygen
3- Giving the patient digoxin
4- Giving the patient a diuretic such as Lasix 40 gm to 120 ml intravenously slowly
5- Giving aminophylline 250 to 500 volume to dilate the bronchi
6- Sometimes the patient needs a respirator to save his life
- Nursing care for an unconscious patient
Loss of consciousness
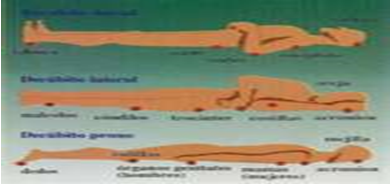
It occurs suddenly, spontaneously and for a short period
Its causes:
· Decrease in the amount of oxygen reaching the brain
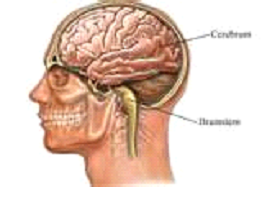
· The amount of sugar in the blood decreases below (60 mg/100 ml of blood)
· Poisoning by drugs – alcohol
· Lung clots
· Seizures Epilepsy
· Severe infection
· Cerebrovascular diseases
· Severe decrease in blood pressure (less than 60 mm Hg)
· Lack of response in the case of mental illness
Symptoms:-
· Pale color
· Pulse rate falling below the lowest normal rate (60)
· Hypotension
· The person returns to his normal state after a short period. Meanwhile, the person sleeps in a shock position, and if he does not wake up, he must be examined.

· During shock or coma
· Observes the pupils, breathing, movement and level of consciousness
· He hears breathing, counts the heartbeats, and notes their regularity
Paramedic section
· Ensure safe breathing
· Note vital signs
· Shock mode
· Start giving solutions with Regers lactate or plasma, if available
· The patient is connected to a heart monitor
· Make an EKG
· Giving prescribed medications
· Trying to make the patient aware of what is around him, the place and the people around him
· Most cases of accidental fainting only require observation for an appropriate period and then the patient is discharged from the hospital in this case (the patient is accompanied by one of his family or relatives
In cases that threaten the patient’s life, such as:
· Acute coronary artery thrombosis
· Decreased and irregular heartbeat
· Severe bleeding from the gastrointestinal tract
· Lung clot
· Kidney failure
· Drug poisoning that causes severe collapse of the heart and lungs
· Pollution
Nursing care for diabetics
Diabetic coma:
Blood glucose level is higher than 300 mg/100 milliliters of blood.
Its causes:
Failure to follow diet and medication, lack of physical exercise, exposure to infection, and exposure to a severe psychological crisis.
How to avoid it:
Following a diet and treatment regimen, exercising daily (walking for an hour a day), continuous follow-up with urine and blood tests, training the patient to inject himself with insulin, and ensuring personal hygiene.
Its symptoms:
Increased urination, extreme hunger and thirst, blood pressure disturbances, constipation, difficulty breathing, tendency to vomit, abdominal pain, anxiety, dryness and redness of the skin, dizziness, and an apple-like odor emanating from the mouth.
Treatment: Water-based insulin: 1/3 of the daily dose, and the remaining 2/3 of the dose is given subcutaneously. A urine and blood sample for analysis.
Nursing care:
Taking a urine and blood sample for the following tests: blood glucose - blood salts - blood alkalinity - acetone - urea - hematocrit. Giving a dose of insulin and solutions and performing an EKG according to the instructions of the treating physician.
Observing and recording vital signs every 15 minutes and a fluid chart (according to the instructions of the treating physician) if he is in the hospital.
Educating the patient about (diet - exercise - following treatment - the importance of follow-up - the importance of personal hygiene and avoiding infection - how to analyze urine for sugar and acetone and give himself an insulin injection if he is able to do so).
2- Infection, cataracts, and complications of the retina, blood vessels, kidneys, and nervous system:
Purulent infections occur in diabetics due to the body's lack of resistance and the effect of all these previous complications on the patient's general condition, and may lead to gangrene or amputation of one of the limbs, especially the lower limbs.
Section: Nursing personnel in patient health education:
· Emphasize the importance of following the diet and treatment regimen and physical exercise appropriate to his age and health condition.
· How to conduct urine and blood tests and fill and inject insulin for himself if he is able to do so.
· Emphasize the importance of regular follow-up, personal hygiene, and staying away from sources of infection
Daily foot care:
· Washing using a good type of soap and lukewarm water, then drying well, especially between the fingers, using pressure and avoiding violent massage to maintain the integrity of the skin.
· Apply cream or edible oil to maintain the softness of the feet and reduce friction, and massage with alcohol once a week. The massage is from the toes to the top of the feet. If there are varicose veins, massage the feet very gently and do not massage the legs.
When taking care of nails:
· Immerse it for half an hour daily in lukewarm water with a teaspoon of Borax dissolved in it, then dry it with pressure and massage it around with nourishing oil or cream in order to strengthen the nails and prevent them from cracking.
· Nails are cut straight and not so short that they reach the soft tissues and do not cut the sides.
When choosing a shoe, make sure that it has a short, comfortable heel that does not put pressure on the toes. When using new shoes, make sure that they are worn for only half an hour on the first day, then for an hour on the second day.
To get rid of calluses:
Immerse the foot in lukewarm water and good-quality soap for ten minutes, then rub the excess tissue with a towel, avoiding causing skin inflammation and not cutting the callus.
To avoid blood division disorders:
· The patient is advised to abstain from smoking to prevent blood vessel constriction.
· Keeping feet warm.
· Do some exercises for the legs and avoid wearing anything that puts pressure on them to improve blood flow.
· Avoid taking any medication or placing it near hot water without consulting your physician.
· Make sure to change socks at least daily.
· If any wound occurs, it must be covered immediately with sterile or clean gauze and consult a doctor immediately.
· Do not use shoes if there is any wound on the feet.
· Inform the doctor when redness, blisters, pain, or swelling appear to avoid contamination that may lead to gangrene.
For the pubic area:
· It should be washed well after urinating or defecating and dried well with a soft cotton towel.
· Underwear should be changed daily and when needed, making sure it is cotton so that it can be washed in hot water and dried in the sun.
Take care to notice the presence of blisters or bumps and report them immediately to the treating physician.
Care steps that reduce eye risks:
· The entire eye should be examined every year.
· Tell your doctor if there is blurring or a dark spot, not seeing things clearly, a feeling of pressure or pain in the eye, difficulty seeing in dark light.
· Make a sectional measurement of intraocular pressure.
Dental Care:
· High blood sugar increases the risk of dental and gum problems. Good daily care at home and regular visits to the dentist will prevent these problems.
· Teeth should be brushed daily, and this is the best way to keep teeth and gums healthy.
· Visit the dentist every 6 months.
· The doctor must be informed that he is diabetic.
Ramadan fasting and diabetics:
· In the case of diabetes, it is undoubtedly useful in treating the second type, as it is an opportunity to apply the diet prescribed by the treating physician and thus reduce the patient’s weight, which may lead to recovery from the disease in simple cases in which the diet is used as the only treatment for the disease.
· In cases where blood sugar-lowering tablets are used, blood sugar decreases and the patient’s weight decreases, and thus the body responds more efficiently to blood sugar-lowering medications.
Unwell days:
He must analyze his urine daily, regardless of the amount of food, and he must continue taking diabetes medication and not change it except after the supervision of a doctor.
When any infection appears, regardless of its severity, the patient must quickly consult his doctor instead of neglecting it in the hope that it will improve automatically or treating it himself.
It must be treated according to the doctor's instructions, as he is able to judge and estimate the optimal treatment and the need for medical tests.
Therefore, a diabetic patient should avoid any wrong treatment that could have serious consequences.
Some daily guidelines that a diabetic patient must follow:
· Sugar pills should be taken in the prescribed dose.
· Tell your doctor when you feel tired or when you think there is some kind of infection.
· Do a blood sugar test approximately every 4 hours.
· Do a urine acetone test if the blood sugar level is higher than 240 milligrams.
· If the patient feels stomach fatigue, he should take fluids in small doses to avoid vomiting.
· Make sure to keep chocolate, candy, or a piece of sugar to use when needed.
· Keep a card on which is written that he is a diabetic patient, the type of treatment and dosage he is taking and the times of taking it, the doctor supervising his treatment or the hospital he visits.
Fainting and coma
Definition of fainting:-
It is when a person completely loses consciousness as a result of a lack of continuous supply of blood to brain cells
Types of fainting
1. In most cases, the person loses consciousness for a short period, and the person regains consciousness as soon as he falls to the ground, as a result of blood rushing to the brain from the extremities.
2. In other cases, the person loses consciousness and is like a deep sleeper (sleep), and you cannot wake him up by stabbing. In this case, the person either regains consciousness or enters a complete coma
3. The person completely loses consciousness and enters a coma
Signs and symptoms of fainting
· Paleness of the face
· Profuse and cold sweat with coldness in the extremities
· Dizziness or lightheadedness with difficulty concentrating, nausea
· Feeling numbness in the extremities and inability to hold anything
· Confusion of sight and confusion of thoughts
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
First aid:
◾ A] If the person feels that he will faint, do the following:
1. Help the injured person to sit, lean forward, and place his head between his knees
2. Ask the injured person to take a deep breath
3. Make sure there is fresh air
◾ B] If the person loses consciousness:
1. Place the patient on the floor lying on his back with the legs raised
2. Loosen the injured person’s tight clothing, especially around the neck
3. Break up any gathering around it to allow air to be renewed for the injured person
4. When the person begins to regain consciousness, explain what happened to him and look for other injuries
◾ C] First aid for a person in a coma:
1. Try to wake up the person in a coma by stimulating the sensory center by tugging on the ear to see if he reacts to the tugging or not.
2. If he does not react to pulling the ear, open the victim’s mouth and make sure that there is nothing blocking the airways
3. If you find an obstruction in the airways (the tongue or a piece of meat), push the injured person’s head back, insert two fingers into the injured person’s mouth, and remove the material causing the obstruction.
4. To open the airways, push the head back and the lower jaw forward, which helps the injured person breathe
5. Make sure that the injured person is breathing by:
¨ Look at the injured person’s chest
¨ And listen to the same afflicted person
¨ Place your hand above the chest to feel the air entering the chest
6. If the injured person is not breathing, begin artificial respiration immediately
If the injured person is breathing, place the injured person in the side-lying position. This position will help the injured person to breathe by placing the tongue and jaw in a forward position and helps fluids and vomit exit from the mouth so that there is no obstruction in the air passages.
- Physiological anatomy of the urinary system
Components of the urinary system:-
· The kidneys are the excretory organs
· The ureters are the ducts that carry secretions from the kidneys to the bladder
· The bladder is the place where urine is collected
· The urethra is the place through which urine exits the body
Urinary system function:-
Formation and secretion of urine and removal of waste and water in excess of the body’s need
Description of the parts of the urinary system:-
1- The kidneys:
· There are two kidneys in the human body, each of which is 10-12 cm long, about 6 cm wide, and 2 cm thick. Each kidney weighs about 150 grams in men and 130 grams in women. They are located near the midline in the body, behind the peritoneal cavity of the posterior abdominal wall. The kidney The right kidney is lower than the left kidney by about 1.25 cm. In general shape, the kidney resembles a bean and is dark red in color. In the upper part of each kidney is the suprarenal gland. Each kidney consists of several units called nephrons, and each kidney contains from one million to 2 million nephrons, and it decreases. Their number depends on age or illness
College installation:-
The kidney is composed from the outside to the inside by:
1) College portfolio
2) The crust layer
3) Medullary layer
· Each kidney consists of a large number (one million - one and a half million) of tiny channels (nephrons or filters) connected by connective tissue. Each channel in the cortical layer begins with a crescent-shaped indentation called Bowman’s capsule, inside which there is a plexus of blood vessels starting from the incoming artery and ending with the outgoing artery.
· Bowman's capsule and the blood plexus are located inside tiny balls called Malpighian cells, and there are many thousands of these cells in the cortex.
· From Bowman’s capsule emerges a tortuous canal called the tortuous duct. The first goes towards the medulla layer, forming the descending duct. Then it returns to the cortex again, forming the ascending duct. In the cortex, it winds upon itself to form the second tortuous duct. Finally, it returns to the medulla, where they gather to form urinary collecting ducts, each of which ends by opening. On the tops of the Pyramids of Malpighi in the Ureter Basin.
Kidney function in the body:
· Normal kidneys perform four basic functions in the human body:-
- Excretion of excess water from the human body
- Ridding the body of toxins and secretions resulting from the food combustion process, such as:
· Excretion of waste resulting from protein digestion in the body (such as urea and creatine)
· Secretion of some ions and regulation of acid balance (PH) in the blood, such as (sodium - potassium - calcium - phosphorus - chloride - phosphate - and hydrogen)
· Excretion of medications, toxins and chemicals that may harm the body
Hormonal function:-
The kidneys secrete three hormones:
· Hormone (renin), which helps conserve the amount of fluids and sodium by regulating the hormone
· Aldosterone is from the suprarenal gland, so the secretion of renin increases in the event of a lack of sodium in the blood or in a state of dehydration, so renin works to raise blood pressure, and thus the kidneys regulate the blood pressure of the human body.
· The hormone erythropoietin stimulates the bone marrow to secrete red blood cells.
· Activating vitamin D, which is necessary for the health of the mouth, teeth and bones.
· A regulatory function to regulate the amount of fluids in the body.
· Concentration of salts such as sodium and potassium, which regulate blood yellowness.
2- The Ureter
· It is a muscular canal that delivers urine from the kidney to the bladder. It is 25 cm long and performs regular contractions from top to bottom to push urine into the bladder.
3- The Urinary Bladder:-
. It is a muscular sac whose primary function is to store urine until it is time to expel it from the body through the urethra
4- The urethra:-
· It is the canal that carries urine from the bladder to the outside of the body. It is different in men than in women, as it is 20 cm in men and only 4 cm in women.
Urine formation in the kidneys:
Urine is formed through three stages:
· Filtration:- where water, salts and some other substances are filtered from the blood
· Absorption: - Some of the water and salts that the body needs are reabsorbed into the blood
So that the blood components are not affected by losing all the water and salts dissolved in them
· Excretion: It is carried out by the cells of the kidney tubules, which have the ability to test substances that exceed their quantity
The normal limit allowed in the body or when it is not needed and it is disposed of
Formation of urine. This occurs in healthy, unaffected kidneys
Characteristics of urine:-
Color : yellow
Specific density: from (1005) to (1025)
Concentration: Acid about (PH = 6)
Smell: (Aromatic)
Content: Water + urea + creatine + ureate (protein product) and ions
ammonium
Inorganic substances: sodium - potassium - calcium - chloride - phosphate - sulfate
Exalates + about 100 gm protein (albumin) / 24 hours
The amount of urine in twenty-four hours (from half a liter to one and a half liters). This depends on the fluids entering and leaving the human body during the day, as well as the weather condition, the general health condition of the individual, and the condition of the kidneys in particular.
- Nursing care for patients with kidney failure
It is the kidney losing all of its function, or this loss is gradual, and it is called chronic kidney failure, and the kidney is able to perform part of its functions. Or it is acute kidney failure, in which the kidneys suddenly fail to perform their functions, which causes death.
Kidney functions
1- Excretion of substances in excess of the body’s needs, such as salts and fluids
2-Reabsorption of salts that the body needs, such as sodium
3- Maintaining blood pH balance
4-Stimulates the spinal cord to form red blood cells
5- It secretes renin, which regulates blood pressure
Causes of kidney failure
Ø Reasons related to blood division, which are the lack of blood supply to the kidneys, which causes the kidneys to stop working
Ø Causes related to the kidneys, such as kidney inflammation
Ø Causes specific to the post-renal parts, such as the ureters and the bladder, as a result of obstruction of the bladder or the right or left ureter, or both, with a stone, which prevents the passage of urine and collects in the ureter and returns to the kidneys again and destroys the kidney cells. Kidney failure causes death by 50%, but if it is discovered early, the patient can be saved or treated.
Symptoms of acute kidney failure
1 - Nausea and vomiting
2 - Scratching
3 - Spasms
4 - Swelling in the extremities
5 - Pleural exudation
6 - The amount of urine is less than 400 cc/day (normal is 1500 cc/day)
Symptoms of chronic kidney failure
1 - Anemia
2 - Fatigue easily
3 - Increased creatinine in the blood
4 - Low specific density in urine
5 - Swelling in the limbs
6 - Rapid bleeding
7 - The patient needs dialysis in the following cases: urea 35 ml/liter
Cretinine 800 μmol/L Bicarbonate 12 mmol/L
The purpose of washing
1- Removing urea and creatine from the blood
2- Maintaining the appropriate proportion of salts in the body
3- Removing excess fluids from the blood
Types of washing
Peritoneal dialysis is done through the peritoneal membrane. Hemodialysis is done through the blood
Disadvantages of peritoneal dialysis
1- Penetration of the bladder, intestines, or blood vessels during cannulation through the peritoneal membrane
2- A clot in the cannula, but it can be removed with heparin
3- Ascites
Nursing responsibility towards the peritoneal dialysis patient
1- Observing the patient’s temperature, pulse, breathing, pressure, weight, inside and outside, and informing the doctor if there is a collection of fluid inside the patient’s abdomen of more than 300 cm.
2- Change the location of the cannula at least once a day
3- Keep spare parts dry and clean
4- Relieve the patient’s pain by reducing the rate of entry of peritoneal dialysis fluid
Disadvantages of hemodialysis
1- Infection with blood diseases such as AIDS and hepatitis
2- Blood clotting
3- Low blood pressure
4- Limiting the patient’s movement for more than 4 hours
5- Bleeding due to heparin
Nursing department towards the hemodialysis patient
1- Observe vital relationships constantly
2- Test the clotting time constantly
3- Clean the cannula connection site daily and apply an antibiotic
4- The cannula site must be protected from destruction
5- Providing the patient with food during washing
To prevent kidney failure
o The patient should be turned every two hours to prevent stones
o Monitor the urine, its quantity and color, and inform the doctor of any change in the color, quantity or turbidity of the urine
o Conducting urea tests
o Monitor the bladder to prevent urine accumulation in it, because accumulation in the bladder leads to the formation of stones
o Blood pressure monitoring and treatment because chronic high blood pressure is considered a cause of kidney failure
o Giving the patient an amount of fluids of no less than 2500 cc/day
o Speedy treatment of hypoglycemia
Treating any kidney infections
o Detecting and breaking up stones
o We must prevent medications that are excreted through the kidneys because this leads to more destruction of the kidney cells - observing the inside and outside and informing the patient.
- The patient’s meal should be rich in carbohydrates and reduce the amount of protein in meals. A normal person needs 1 gm of protein per kg of body, but in the case of a patient with kidney failure, he needs 6. g/kg - Reducing table salt in meals
As for patients with kidney failure, the following must be taken into account:
If the amount of fluid coming out is small, we must do the following
◾ Reduce fluids for the patient
◾ As for the patient’s food, it must contain large amounts of carbohydrates, while reducing protein and completely eliminating table salt from the patient’s meals.
◾ The patient’s weight must be monitored daily, and if any increase is noticed, tests must be performed on the patient to determine the levels of creatinine, sodium, and potassium in the blood.
◾ For the dialysis patient, blood tests must be performed before dialysis to discover whether he is suffering from hepatitis or AIDS.
◾ We must allocate a special artificial kidney device for hepatitis C patients to prevent the spread of the disease. The artificial kidney unit must be sterilized after each patient.
◾ Heparin should be given to prevent blood clots
◾ Giving the patient advice about meals
Medications and treatment for patients with kidney failure
◾ The ideal solution is to transplant a kidney. One is sufficient and it is implanted in the lower part of the abdomen, for example. It does not require removing the diseased kidney, but rather leaving it to reduce inflammation. However, when the kidney is not available, it is necessary to perform dialysis with medications and pay attention to food.
◾ Someone might say, why do you publish the names of medicines in a daily newspaper? The answer is that these medicines are not a secret and must be made clear to patients with kidney failure, just like all chronic diseases, all aspects of which must be clear to everyone.
◾ We do not imagine a healthy person who would buy medications for kidney patients as preventative measures because they treat the condition but do not protect against the disease.
◾ A patient with kidney failure must follow the advice of the doctor and nutritionist in choosing the correct times when taking medications in order to ensure the effectiveness of medications that may conflict with other medications or with diets.
◾ We will talk about some medications that are prescribed to some patients with kidney failure.
1- Medications that reduce phosphorus absorption:
Such as Caltrate, Ulsaheal, or Amphojel, these medications should be taken with meals due to their effectiveness when taken with a meal, as they work to prevent the absorption of phosphorus in the meal. Calcium carbonate may be prescribed to increase
calcium, so it is recommended to take it between meals in these cases.
2- Iron:
Iron medications are prescribed for patients who suffer from anemia that accompanies some patients with kidney failure. These medications should be taken between meals or at night when the stomach is empty. These medications should not be taken with
medications that reduce phosphorus absorption, as food and medications that reduce phosphorus absorption reduce iron absorption.
3- Ascoplex:
These tablets contain vitamin C, which helps absorb iron. Therefore, they should be taken with iron tablets, and the best time to take them is three hours after eating dinner.
4- Potassium medications: such as Kayexalate
It is used when the level of potassium in the blood is high, and it should not be taken with orange juice, milk and its derivatives, or foods that contain high amounts of potassium.
These medications may cause constipation, so it is recommended to eat foods rich in fiber, such as salads and fruits with their peels.
5- Blood pressure medications:
If the patient is taking medications to treat blood, he should ask the doctor about the possibility of taking these medications before performing dialysis. The doctor will tell him whether he should take these medications before the dialysis process or not.
6- Diabetes medications:
A diabetic patient who uses insulin or tablets should take them with a meal at home before he comes for dialysis.
The most important tests performed for patients in dialysis units:
◾ Hemoglobin analysis every 1 month
◾ Kidney function tests (urea - creatinine) every 1 month
◾ Complete blood count analysis every 1 month
◾ Liver function analysis, virus tests every 3 months
Renal resection
The unit's nursing supervisor reviews the patient's data to ensure that the specified treatment session will be conducted on the specified date according to the daily schedule in the case of old patients.
Coordination is made between the unit supervisor and the secretariat to create a new file to store the patient’s papers. He is given a list of the instructions he follows before and during each session, the follow-up system, food, and the financial system he follows. The patient is added to the daily washing schedule in line with the system followed in the unit, taking into account the appointments that suit the patient according to Instructions of the treating physician in the case of new patients.
The nurse ensures that the patient follows the instructions related to keeping his tools or personal belongings in the designated place outside the unit in the locker room.
Preparing the patient to enter the unit by ensuring that the patient takes off the clothes he is coming in and wears his dressing gown or wears his own robe or pajamas if this will make him feel more comfortable, provided that the clothes are clean and in good condition. Then the patient washes his hands and dries them well before entering the unit.
The patient obtains his own identification card
Follow up on the procedures for the patient’s exit from the unit after the end of the session by giving the patient his card from the unit’s secretariat to hand it over to the place designated for dialysis patients in the outpatient clinic. Then he receives his belongings that he left when he entered the unit. The unit’s nursing supervisor also explains the follow-up system and attendance times for the sessions to the patient. His family or those with him how to act in emergency situations. They must also be given the direct phone number of the unit to ensure rapid action in case of emergency.
The head of the unit in the morning, or whoever performs her work at noon and night, writes down the names and numbers of patients for whom sessions were conducted during her presence, and signs the statement, along with writing the name of the doctor who followed up with him during the sessions, and sends it to the accounts.
Reports on the patient's daily sessions are summarized each month in one report and then at the end of each year in one report. This includes monthly research for each patient.
- Kidney transplantation
introduction:
Kidney transplantation is considered the best treatment for chronic kidney failure, as the transplanted kidney performs the functions of the original kidneys, while dialysis performs a limited function by ridding the body of metabolic waste and excess fluids than the body needs. The operation is performed by a specialized surgical team, and the kidney is obtained from a living or deceased donor. The kidney is usually implanted in the right side of the lower abdominal cavity, where it is connected to the right pelvic artery and vein. The ureter is also connected to the urinary bladder in a process that usually takes about three hours. It is expected that urine production will begin immediately after the kidney taken from a living donor is connected, while the kidney taken from a deceased person may need some time to begin working fully efficiently. The patient undergoes intensive medical and surgical supervision after the operation to control the levels of fluids, salts, and immune medications in the blood. He remains in the hospital from one to two weeks, and after his discharge, he remains under the ongoing supervision of kidney transplant doctors.
Obtaining a new college:
A patient with chronic kidney failure can obtain a new kidney for transplantation from one of the following sources:
First: Living relative donors. In order for a relative to be considered a suitable donor, he must meet the following conditions:
He must be of legal age (21 years) according to the law.
He must have full mental faculties, be responsible for his actions, and be well-versed in the procedures, results, and even complications that accompany the kidney donation process.
The necessary medical examinations and tests must prove that he is medically fit. It is also important that he does not suffer from any chronic diseases, such as diabetes, high blood pressure, or hepatitis.
He must be immunologically suitable according to the results of blood type and tissue analyses.
Second: Living donors who are not relatives:
A large number of people apply to the Organ Transplant Center with their desire to donate one of their kidneys to patients with chronic renal failure. In order for their desire to donate to be approved, it must be ensured that The following is available:
All conditions mentioned for related donors must be met.
There is no suspicion of trafficking or taking money for money.
The donation must not be made under the influence of threats or blackmail.
The donation must be approved by the special committee to interview these donors, which was formed by a ministerial decision.
It is worth noting that some people travel to some Asian countries to buy a kidney, but as a result of performing the operation in unqualified centers whose primary goal is financial gain, the resulting rate of complications is unacceptable and sometimes dangerous for patients.
Third: Obtaining a kidney from deceased people:
◾ Chronic kidney failure patients are registered in special lists according to blood type. When a kidney from a deceased donor is available, a number of these patients are summoned in order of priority to the organ transplantation department, where they are medically examined, in addition to some analyzes and examinations, as well as immunological tests. Patients are selected according to a points system given to patients registered on the waiting list, and it takes into account the patient’s age, the period of dialysis treatment, medical fitness, and histological compatibility.
Preparing for a kidney transplant:
Kidney transplantation is considered the ideal treatment for patients with chronic kidney failure because kidney transplantation:
◾ It gives the patient a longer life span and a better quality of life.
◾ Lowest cost treatment method.
◾ For children, it is the only means that:
◾ It gives them the opportunity for normal physical and mental development.
◾ It gives them a better opportunity for school attendance and academic achievement.
◾ Avoid the frequent (psychological and health) suffering associated with dialysis.
Procedures to be completed before kidney transplantation:
Obtain a detailed medical report from the treating physician in the patient’s kidney disease unit. This report includes the following:
◾ Medical history of the patient referred for a kidney transplant.
◾ Results of the clinical medical examination.
◾ Results of laboratory tests, especially hepatitis viral tests.
◾ Results of endoscopic examinations of the esophagus, stomach and duodenum.
◾ Examination of the bladder and urethra using color x-rays, and sometimes, if necessary, or conducting special tests for the function of the urinary bladder and examining the bladder endoscopically.
◾ The absence of chronic inflammatory sites such as tooth decay and tuberculosis (which require a chest x-ray and skin tuberculosis examination).
◾ Results of tests that indicate the fitness of the heart to perform a kidney transplant (planning, ultrasound, and nuclear rays).
◾ The patient is free of any non-benign tumors
◾ Mammogram for women over forty
◾ The patient’s medical report is reviewed by the organ transplant surgeon and nephrology consultant at the organ transplant center, a medical examination is signed on it, and any missing tests and analyzes are completed.
◾ Conducting immunological tests between the patient and his accompanying donor.
Determine the date of admission to the hospital and performing the kidney transplant operation well before the operation.
Kidney transplant process:
The kidney transplant operation is performed under general anesthesia and usually takes (3-4) hours. The kidney is placed on the right or left side of the pelvis, outside the peritoneal cavity. The blood vessels of the kidney are connected to those in the pelvis, and the ureter of the new kidney is transplanted into the esophageal bladder. Z.
The patient stays in the hospital after the kidney transplant for one to two weeks, during which he:
o Close monitoring of the patient’s health condition.
o Giving intravenous solutions of appropriate types and sizes.
o Giving immunosuppressive medications and regulating the doses according to the patient’s need.
◾ Monitoring the function of the transplanted kidney.
o Teaching the patient about the different types of medications that he must take, especially the dosage and time to take the medication before leaving the hospital.
◾ After leaving the hospital, the patient must strictly adhere to the outpatient clinic appointment times that are given to him.
o The patient must visit the Organ Transplant Center
o When exposed to any disease symptom.
After the operation:
The patient stays in the hospital after the kidney transplant operation for one to two weeks, as he needs intensive care. He is given the required solutions and medications on a daily basis until his condition stabilizes. During this period, the patient’s family is requested to reduce visits to him, while following the instructions from the treating doctors and the nursing staff responsible for his care. The patient is so that he is not exposed to infections and infectious diseases from others, due to his extensive use of immunosuppressive drugs, which weaken the body’s resistance to these diseases.
The patient may need to stay in the hospital for a longer period than that, depending on the case. For some patients, their condition requires taking a sample from the transplanted kidney when temporary impairment of kidney function occurs, so that rejection or other cases can be diagnosed early and appropriate treatment given.
When the patient is discharged from the hospital, he gives detailed instructions about medications, diet, and appointments for review at the outpatient clinic, and is given the prescribed sick leave.
Medications to prevent kidney transplant rejection:
The human body has lines of defense that protect it from harmful influences, including the external line, such as the skin and mucous membranes lining many of the body’s systems, and the internal line of defense, which is what is known as the body’s immune system, which consists of white cells and antibodies secreted by some of these cells. We know that a kidney transplant patient needs to do many tissue compatibility tests before performing the operation, and despite these tests, the transplanted kidney is still considered a foreign organ to the body that the immune system must attack (i.e. reject). For the operation to be successful, the immune system must be suppressed, which is known as reducing immunity, so that it does not attack the transplanted kidney. Here, the section includes anti-rejection medications.
Immunosuppression requires two stages:
Qualification:
In which strong doses of these medications are given, usually intravenously, before the operation and sometimes during the first few days after the operation.
Continuity:
In it, oral medications are given daily to maintain a low performance rate of the immune system that allows the transplanted kidney to be accepted without exposing it to rejection, while maintaining a degree of the body’s immunity that works against many microbes to which it may be exposed.
Thanks to scientific development, many of these medications have been discovered, making it possible to give them according to the condition of each patient, after it was limited in the past to two or three medications given to all patients, which may negatively affect their health if side effects of these medications appear.
Among these medicines:
- Cortisone. Prednisolone
- Amuran. Imuran
- Alsalbet. Cellcept
- Neoral. Neoral
- Prograph. Prograf
- The Rapamites. Rapamune
The doses of these medications are gradually reduced to reach the lowest amount by the end of the first year after transplantation.
Preventing infectious infections in kidney transplants:
Anti-rejection medications suppress or reduce the body's immunity, which is necessary to prevent kidney rejection. At the same time, a degree of this immunity must be maintained to fight various microbes. Therefore, the treating physician performs departmental examinations to ensure the percentage of these medications in the blood and their effectiveness, and therefore tries to weigh the difficult equation to preserve the kidney and prevent infection. However, the patient may go through periods where his immunity decreases to a degree that may allow the infection to occur, for reasons that may be general, like any other person, such as cold attacks, changing seasons, and malnutrition, or for special reasons, such as raising the doses of medications due to suspicion or treatment of kidney rejection, or the necessity of using some medications. Which will increase the effect of anti-rejection medications on the immune system, and do not forget that some infections, especially viral ones, may significantly reduce the body’s immunity.
The body's immunity is at its lowest possible during the first six months after transplantation, so the patient is prescribed antiviral, antibacterial, and antifungal medications during this period that help reduce the possibility of infection. Patients are also generally advised to avoid mixing with people with contagious diseases, especially children, and to stay away from crowded, poor places. Ventilation, and eating fresh food prepared at home while staying away from ready-made meals available in the market, and taking care to consult a doctor immediately when epidemic diseases spread in the environment surrounding the patient.
It is not recommended to wear a mask on the face, and wearing it is limited only when there is a possibility of exposure to cases of infectious respiratory diseases through the breath or mouth spray, which requires staying away from these patients.
Vaccination and kidney transplantation:
Following vaccination schedules according to the advice of the treating physician is an essential element in preventing bacterial and viral diseases to which a kidney failure patient is exposed before and after the transplant. This is done in consultation with the treating physician and the preventive health department in hospitals. As a basic rule, vaccinations taken from a live, weakened (i.e. inactive) microbe cannot be given. Known in various vaccination centers.
Food after kidney transplant:
There is no doubt that a patient with kidney failure faces a lot of suffering in what he eats or drinks, and therefore he feels that a kidney transplant will relieve him of this suffering. This is true to a large extent, as he will not need to be careful about drinking water, nor be afraid of drinking too much. Who eats fruits and vegetables because of the potassium, and he can eat whatever meat he wants, and that is in the best assumptions, that is, when there are no other obstacles to these types of foods and drinks.
But the following must be taken into consideration:
◾ Kidney patients often also suffer from high blood pressure, and this requires reducing the amount of salt they eat, especially found in canned cheeses, processed meats, and ready-made meals.
◾ He may also suffer from high blood cholesterol or triglycerides, which requires reducing the amount of fat he eats, which is often found in full-fat dairy products, meat, fried foods, chocolate, and nuts.
◾ Given the high rates of diabetes in our country, especially since it is one of the main causes of kidney failure, a significant percentage of kidney transplants suffer from this disease. Therefore, a special diet must be adhered to that prevents high blood sugar and, more importantly, prevents the emergence of new cases from those who are predisposed to this disease. Due to genetic factors or other health reasons.
◾ We must keep in mind that kidney transplant medications may be responsible for some nutritional problems, such as increased appetite, increased obesity, high blood pressure, and diabetes, and this can be controlled with the necessary diet for various types of these health problems. They may also cause Digestive system disorders resulting in dehydration or malnutrition.
Fasting after kidney transplant:
◾ Ramadan fasting is one of the beloved obligations of all Muslims, and the obligation of fasting is lifted from the sick until he recovers, the pregnant woman until she gives birth, and the traveler until he returns, and kidney transplants are the same as patients, they have a permit to break the fast (and God knows best), as they are in need of continuous medical follow-up and a special system in Eating, drinking, and taking medications. If this regime is compatible with fasting and his kidney functions are normal, he is permitted to fast after consulting his treating physician.
◾ The effect of fasting on the functions of the transplanted kidney was monitored in a number of patients who wished to fast - after reviewing their health condition - and compared to their counterparts who did not fast, and we did not find any differences between them. This allowed us to identify the conditions that enable kidney transplants Of fasting - God willing - without any problems, which are:
◾ Kidney functions must be stable for a period of no less than six months before fasting.
◾ The creatinine level should not exceed 200 micromol/L.
◾ The number of times you should take any of the essential medications should not exceed twice a day (that is, every 15 hours at least).
◾ He must not be suffering from kidney stones or acute or chronic stomach ulcers.
The following must be taken into account:
o Eat the suhoor meal and then take the morning medications 15 minutes before the dawn call to prayer with two cups of water.
o Drink water and dates or a little soup at the Maghrib call to prayer, then take evening medications and perform the Maghrib prayer (to give the opportunity for the medications to settle inside the stomach), and then eat breakfast.
o Make sure to drink plenty of water during breakfast.
o It is recommended to eat a light suhoor meal while reducing the amount of salt and proteins to avoid diuresis during fasting.
o It is recommended not to eat a lot of sugars, starches and fats, especially for diabetics, and to eat moderate meals in order to avoid stomach and digestive system problems.
o The basis is regularity in taking medications. If dawn calls and the patient has not taken his medication, he must break his fast to take the medication.
Sports after kidney transplant:
o A kidney transplant is performed to rehabilitate a chronic kidney failure patient so that he can perform his duties normally and participate effectively in public life. The patient begins to move out of bed on the second day of the operation, and when he leaves the hospital, he walks normally. After three months, he begins to exercise, which increases in strength, until he reaches full athletic activity six months after the operation.
Contraceptive medications:
◾ There are side effects of contraceptive medications that are not suitable for the kidney transplant patient and may cause her health problems, so she should refrain from using them except in limited cases with the approval of the treating nephrologist and it is recommended to use condoms.
Pregnancy after implantation:
◾ Kidney failure often leads to a decrease in fertility, and fertility does not recover completely after the transplant. However, the kidney transplant patient can get pregnant and give birth naturally after the transplant, and a period of stabilization of the medical condition lasts for one to two years after the operation, knowing that there is an increased possibility of kidney rejection with Pregnancy and childbirth, and preparation for this is done through regular follow-up in the women’s clinic and the transplant clinic, adjusting medications according to the development of the condition, and taking the required precautions before, during and after childbirth in arrangement with the obstetrician and gynecologist.
Protection of the transplanted kidney:
- A kidney transplant patient must protect his kidney from cases of rejection, starting from choosing the most suitable donor whose tissues are compatible with him, to completely regularly taking kidney transplant medications and others, especially immune-reducing medications and diabetes and blood pressure medications, and medical follow-up in the outpatient clinic according to the scheduled appointments, and performing departmental examinations for detection. On kidney function according to the advice of the treating physician, following his instructions and advice, not measuring his condition against the condition of other patients because the nature of the disease and his condition differs from one patient to another, and not taking any medication or performing large or small surgeries without consulting him.
- Conducting patient reception and catheterization
Steps:
◾ . Patients are received at the kidney clinic, examined, tests are performed, and their condition is determined if it requires dialysis or not.
◾ The patient was received in the space designated for patients in the Artificial Kidney Unit in the outpatient clinic
◾ The card is extracted.
◾ A specific allocation form that includes the patient’s name, date of birth, and code number assigned to him, as well as his financial treatment system.
◾ The patient goes to the unit and presents his card to the unit’s secretariat, who extracts the treatment file and gives it to him.
◾ This file contains his monthly records, his patient history, and the forms designated for monitoring his condition during the washing session.
Procedures for receiving a hesitant patient
Steps:
· The unit’s administrator follows up by confirming appointments through the appointment card and recording the patient in the unit’s accounting records.
· To weigh the patient before entering the session.
· Recording the patient in the unit’s visitor book.
· The weight in excess of the normal weight is calculated to be withdrawn.
· Take complete vital signs.
· Preparing the patient for a hemodialysis session.
· Testing of electricity and water connections.
· Prepare a jar of washing solution and place it next to the machine. Place the stick inside the jar according to the type of washing solution.
· Open the machine and test the machine.
· Place the filter in place on the machine.
· Placing the artery connection and the vein connection in their correct place.
· Connect the artery connection to the saline solution bottle to remove air from the filter lines.
· Make sure the air comes out and put (a) heparin in the intravenous connection and make a closed circuit.
· Pass the solution through the machine for 30 minutes..
· Connecting the patient to the machine designated for him.
Nursing procedures for inserting a clavicle catheter (Mahooker)
Steps:
◾ Routine hand washing
◾ Preparing the necessary supplies and medications (catheter set - plaster - surgical betadine - xylocaine - sterile gloves - surgical thread - sterilization packet - sterile gauze).
◾ Explaining the procedure in a simple way, which helps provide psychological stimulation to the patient
◾ Hand washing is surgical
◾ Assist the doctor in sterilizing the installation site
◾ Help the doctor to administer Xylocaine to the site of application
◾ Follow up on the patient’s transfer to the radiology department for chest x-rays to be performed by the worker after installation
◾ Show the doctor the x-rays to monitor the location of the catheter
◾ Helping the doctor install the catheter
◾ Giving a Hepa Ren ampoule to analyze a centimeter in the arterial and venous connection after the end of the session.
◾ Change the place of the mohawk and put it on without a silk cover
◾ Routine hand washing
Nursing procedures during femoral catheter placement
Steps:
◾ Routine hand washing
◾ A spare bag containing a sterilizing bowl, sterilizing towels, and silk thread. Prepare the required supplies (sterile gloves, surgical betadine, sterile gauze).
◾ Explaining the procedure in a simple way, which helps provide psychological stimulation to the patient
◾ Hand washing is surgical
◾ Sterilize the catheter site (groin) with Betadine, taking into account the contact time.
◾ Help the doctor to administer Xylocaine at the site of installation
◾ Help the doctor install the catheter
◾ Routine hand washing after installation. Wash your hands and wear personal protection
◾ Remove the femoral catheter after the session ends and apply pressure on the catheter site for a few minutes while doing leg exercises.
◾ Put a sterile pad on the catheter site and put it on without a cover after the bleeding stops.
- Procedures for starting a hemodialysis session
Steps:
· Routine hand washing.
· Preparing supplies
· Wash your hands (hygiene) before starting work
· Wear protective clothing (gloves, mask, glasses).
· Vital signs are measured before the session, and blood pressure is measured every hour during the session and whenever the patient’s condition requires
· Disinfect the site of the venous and arterial connection in the patient’s hand with Betadine, taking into account the time the Betadine comes into contact with the Vistula catheter in the patient’s arm, after ensuring that the catheter is fixed in the patient’s arm and connecting the patient to the device.
· Connecting the closed artery connection to the closed artery needle
· Open the valve after ensuring that there is no air in the connections.
· Open the blood pump slowly and give the amount of heparin agreed upon with the treating physician
· Close the intravenous connection valve when blood reaches it and close the blood pump
· Connect the end of the closed stopcock patient connector to the end of the closed intravenous needle 5
· Open the blood pump slowly while opening all closed valves
· Ensure that the blood level in the air barrier rises and gradually speed up the blood pump
· Wrap the extensions around the patient’s hand in a safe manner and secure them
· Routine hand washing Hemodialysis supplies
Work procedures during a hemodialysis session
Steps:
· Fill out the follow-up paper data during the session for each patient, including weight, vital signs, medications, and solutions during the session. Record excess weight, pump speed.
· Notice any signs of low blood pressure (dizziness, sweating, depression, lack of concentration).
· Give the dose of heparin at the specified times.
· Monitor blood pressure every hour during the session.
· Observing any changes that occur in the patient during the hemodialysis session (bleeding from the site of the blood connection - continuous monitoring of the patient’s hemodialysis machine - vomiting...etc.
Action steps for a patient with laundry hooks
Steps:
◾ Inspect the vest or graphite daily to ensure its efficiency.
◾ Ensure that there are no signs of infection (redness and swelling).
◾ Wash the session from the arm that has the vestula or graphite daily with water and soap daily and before starting.
◾ Warning to change the location and take the needles with the vestula so as not to expand their size
◾ Light pressure on the location of the needles after removing them and putting spare ones on them for a few minutes until ensuring that the blood has stopped and that there is no bleeding before leaving the unit.
◾ Warning to remove the spare parts from the Vistula the next morning
Catheter handling:
◾ Hygienic hand washing.
◾ Wear personal protection.
◾ Place the sterile spare parts on the catheter site after completing the session.
◾ Giving treatment to help thin the blood according to the doctor’s instructions.
◾ After completing routine hand washing.
◾ Warning the patient to keep the dressing dry, especially (when showering) and between sessions.
◾ Inform the doctor when the temperature rises to prescribe appropriate treatment 7
◾ Warn the patient to be careful and be gentle when putting on and taking off clothes, when putting on and uncovering the blanket, and when sleeping.
Nursing actions during hemodialysis complications
A) Low blood pressure
Steps:
◾ Withdrawal is stopped after reviewing the doctor.
◾ Reduce the withdrawal rate after consulting a doctor
◾ Increase the sodium and calcium solution with the dilazit converter after consulting the doctor
◾ Reduce the dilazite temperature after consulting a doctor
◾ Stop treating high blood pressure about 4 hours before the session after consulting the doctor
◾ Giving medications to raise blood pressure as directed by the doctor, such as midodrine 6 mg, half an hour to an hour before the session.
◾ All previous procedures are performed in the presence of the doctor and according to his instructions.
B- Muscle tension
Steps:
◾ Reduce the withdrawal rate after consulting a doctor
◾ Give a salt solution after consulting a doctor
◾ Follow up on reaching the ideal weight rate
C- Imbalance
◾ Steps:
◾ Use small-sized filters after consulting a doctor.
◾ Reducing blood flow rate (PMP) and dilazit after consulting a doctor
Taking an intravenous diazepam injection as directed by the doctor and the HIV virus
Ending the hemodialysis session
Steps:
· Routine hand washing
· Prepare the necessary supplies (no coverall + sterile gauze).
· Wear protective clothing (apron, gloves, mask, glasses).
· Measure blood pressure before ending the session to determine the type of solution used: salt or glucose
· Hand washing is hygienic
· Close the blood pump and close the artery stopcock and the artery needle
· Place the artery connection in the solution bottle and open the blood pump
· Activate the connections and filter to ensure that blood does not clot in the filter
· Raise the vestula and apply gentle pressure on it
. Disinfecting the site of the vestula with betadine and sterile gauze and no cover after ensuring that there is no blood in the site of the vestula.
. Dispose of the connections, filters, and all consumables belonging to the patient and change the furnishings.
· Disinfect the machine from the outside with chlorine and alcohol
· Weigh the patient and record this in the medical file
· Measure blood pressure before allowing the patient to leave the unit
· Recording all supplies and medications and signing the responsible nursing staff
· Follow up on the patient’s signature on the session and confirm the date of the next session.
· Follow up on the patient’s discharge when he leaves the unit by the worker.
- Taking care of the hemodialysis machine
Steps:
◾ Wear personal protection.
◾ Remove the solution stick from the jerry can and place it in the machine
◾ Connecting the dialysis tubes to the machine
◾ Ensure that all doors (pump, blood tank) are closed to create a closed circuit (Rinse).
◾ Enter a program first.
◾ Enter the machine into the Dis infection program.
◾ Apply the necessary solution to the machine: chlorine solution in cases of acetate washing and citric solution in cases of bicarb washing
◾ Shut down the machine after the machine finishes the program
◾ Wipe the machine from the outside with chlorine diluted at a rate of 100 cm chlorine / liter of water for the body of the machine.
◾ Wipe the parts of all operating switches with 95% alcohol
Sterilization protocol for the Fresenus dialysis machine, model 8004
First: In the case of washing using Acetate solution.
◾ Rinse is done between each session.
◾ At the end of the day (and every day), one of two methods is followed
The first method:
◾ Performing PGM5 cold chemical disinfection using sodium hypochlorite diluted by 10%.
◾ Trade name (Javel or Clorox)
◾ Conducting a thermal disinfection program. Hot Rinse Pgm
The second method:
Perform hot chemical disinfection on PGM2 (from the back, yellow link) using one of the following media:
◾ Fresenius Diasteril
◾ Fresenius Citrosteril
NB :
Devices equipped with Diasafe Filter are chemically disinfected using PGM2 – (rear yellow link Fresenius Diateril only)
Second: In the case of washing using a solution (using: Bicarbonate
One of the following two methods is followed:
First method:
Immediately after each bicarbonate washing session, calcifications (calcium salt deposits) are removed and the machine is chemically disinfected from the back of PGM2 using one of the following media:
Fresenius Diasteril
Fresenius Citrosteril
The second method:
Immediately after each bicarbonate washing session, calcifications (calcium salt deposits) are removed using
PGM2 from the back (yellow link) is diluted using Citric Acid Concentrate
100% 10g citric per liter of water from the water treatment unit.
. At the end of the day and every day, a cold chemical disinfection (PGM5) is performed using the chemical agent sodium hypochlorite diluted by 10% (trade name: Javel or Clorox).
NB :
Devices equipped with Diasafe Filter are chemically disinfected with PGM2 on the back
Yellow link using the agent Diasteril. Fresenius only
Procedures during a peritoneal dialysis session
Steps:
◾ Explaining the procedure in a simple way, which helps with psychological stimulation.
◾ Routine hand washing.
◾ Wear protective clothing.
◾ Preparing medical supplies
◾ Hand washing is surgical
◾ Sterilize the abdominal skin with Betadine, taking into account the contact time
◾ Assistance in injecting a local anesthetic (Xylocaine) into the selected area in the lower abdomen
◾ Assist in installing the peritoneal catheter and ensuring its placement by the doctor
◾ Nursing staff should handle the patient and the connections in a sterile manner
◾ Place a bottle of washing solution, whether concentrated or diluted, depending on the patient’s condition, inside the peritoneal cavity over a quarter of an hour.
◾ Continue leaving the solution for 55 minutes, then empty it over the course of a quarter of an hour
◾ Put heparin and the antibiotic in the lubricants or solution used according to the doctor’s instructions
◾ Safe disposal of waste
◾ Routine hand washing
Isolating the patient in the unit
Steps:
. The unit supervisor isolates each of the hepatitis B5 patients individually in an isolation room. HCV/HBV patients
. Isolating patients physically (in a separate room from the rest of the patients)
. Allocating their own machines, special supplies and tools, and their own nursing staff who do not deal with the rest of the patients during the dialysis session.
. Follow all infection control procedures during each procedure.
Doing monthly tests
Steps:
. Visit the patient with the doctor and determine the type of tests required.
. Continue writing analyses
. Explain the procedure in a simple way to the patient
. Prepare special tubes for the sample type.
. Collect samples while following infection control instructions
. Send the sample to the laboratory
. The results of the tests are brought from the laboratory by the medical secretariat
. Informing the doctor of the results and recording them in his patient file and the analysis notebook
. Giving a copy of the test permit to the accounting employee to place in the patient’s file
. Presenting monthly analyzes to the unit manager
- Medical terminology
|
|
|
|
|
|
مريض |
Patient |
العلامات الحيوية |
Vital signs |
|
اسم المريض |
Patient name |
الضغط |
Blood Pressure |
|
السن |
Age |
النبض |
Pulse |
|
النوع |
Gender |
الحرارة |
Temperature |
|
ذكر |
Male |
التنفس |
Respiration |
|
انثى |
Female |
الالم |
Pain |
|
الوظيفة |
Occupation |
غرفة |
Room |
|
الحالة الاجتماعية |
Marital History |
قسم |
Department |
|
متزوج |
Married |
العمليات |
Operation |
|
اعزب |
Single |
الطوارئ |
Emergency |
|
متزوج ويعول |
Married with |
اقسام الداخلى |
In patient |
|
مطلق |
Divorced |
العيادات |
Clinics |
|
نعم |
Yes |
دخول جديد |
New admission |
|
لا |
No |
خروج |
Discharge |
|
عادات خاصة |
Special Habits |
وقت |
Time |
|
تدخين |
Smoking |
تاريخ |
Date |
|
كحوليات |
Alcohol |
دبلوم تمريض |
Diploma nurse |
|
مرض |
Diseases |
افراد هيئة التمريض |
Nurse |
|
حساسية |
Allergy |
طبيب |
Doctor |
|
شكوى |
Complaints |
قبل الدخول |
Before admission |
|
تعليق |
Comment |
دخول |
Admission |
|
اجهزة الجسم |
Body Systems |
بعد الدخول |
After admission |
|
طبيعى |
Normal |
ادوية |
Medications |
|
غير طبيعى |
Abnormal |
حالى |
Present |
|
عام |
General |
العلاج الحالى |
Present medications |
|
ارتفاع |
Height |
الدواء |
Drug |
|
الوزن |
Weight |
الجرعة |
Dosage |
|
عينة |
Specimen |
عدد مرات |
Frequency |
|
وريد |
Vein |
الوقت- الفترة |
Duration |
|
شريان |
Artery |
المظهر العام |
General Appearance |
|
دم |
Blood |
الجلد |
Skin |
|
تاريخ المرض |
Past History |
الراس |
Head |
|
محطة تمريضية |
Nursing station |
توقيع |
Signature |
|
المرض عندالعائلة |
Family History |
العين |
Eyes |
|
فحوصات الجسد |
Physical Examination |
الاذن |
Ears |
|
فحص الصدر |
Breast examination |
الانف |
Nose |
|
تنميل الاطراف |
Numbness |
الفم |
Mouth |
|
ولادة طبيعية |
Normal labor |
اسنان |
Teeth |
|
ولادة قيصرية |
Cesarean section |
رقبة |
Neck |
|
عنق رحم |
Cervix |
الصدر |
Chest |
|
المخ |
Brain |
بطن |
Abdomen |
|
تورم |
Edema |
العظام |
Bone |
|
ازرقاق |
Cyanosis |
الحالةالنفسية |
Psychological Status |
|
صفرة |
Jaundice |
التشخيص |
Diagnosis |
|
مرض السكر |
Diabetes mellitus |
العوامل الخطرة |
Risk Factors |
|
الخطةالتمريضية |
Nursing care plan |
خطة رعاية |
Care plan |
|
اختناق |
Dyspnea |
ملحوظة |
Notes |
|
عسر هضم |
Dyspepsia |
وتر |
Tendon |
|
صعوبة بالبلع |
Dysphagia |
متابعة |
follow-up |
|
صعوبة فى النطق |
Dysphonia |
اسباب |
Reason |
|
السابق |
Previous |
تحاليل المعمل |
Laboratory Investigations |
|
اضطراب فى النوم |
Dyssomnia |
تخدير |
Anesthesia |
|
صعوبة فى التبول |
Dysuria |
بدايةالتخدير |
Start of anesthesia |
|
تقييم مجرى الهواء |
Airway Assessment |
نهاية التخدير |
End of anesthesia |
|
مجرى الهواء |
Airway |
مساعدة |
Assistant |
|
فصيلةالدم |
Blood Group |
نوع التخدير |
Type of anesthesia |
|
شمع الاذن |
Ear wax |
موضعى |
Local |
|
وجع الاذن |
Earache |
كلى |
General |
|
منظار بطن |
Laparoscope |
اجراءات |
Procedures |
|
استكشاف بطن |
Laparotomy |
قبل العملية |
Pre-operative |
|
التهاب الحنجرة |
Laryngitis |
بعد العملية |
Post-operative |
|
ورم ليمفاوى |
Lymphoma |
اثناء العملية |
Intra-operative |
|
دم النفس |
Lochia |
تقييم |
Sheet |
|
وجع فى الظهر |
Back pain |
تحويل المريض |
Referral |
|
صداع |
Headache |
حساسية |
Sensitivity |
|
جرح |
Wound |
الزهرى |
Syphilis |
|
جرح نافذ |
Stab wound |
الحنجرة |
Larynx |
|
وريد |
Vein |
بولينا |
Uremia |
|
شريان |
Artery |
حصوة المثانة |
Bladder Stone |
|
التهاب الفم |
Stomatites |
كلي |
Kidney |
|
يعانى من |
Suffer from |
ارتفاع الضغط |
Hypertension |
|
مضاد حيوى |
Antibiotic |
انخفاض الضغط |
Hypotension |
|
مضاد الحساسية |
Anti-allergic |
غيبوبة |
Coma |
|
مضاد للفطريات |
Anti-fungal |
شبه غيبوبة |
Semi coma |
|
مضاد للفطريات |
Anti-parasitic |
نزيف من الانف |
Epistaxis |
|
مانع الالتهاب |
Ant-inflammatory |
نبض سريع |
Tachycardia |
|
مضاد التسمم |
Anti-toxic |
نبض بطئ |
Bradycardia |
|
مطهر |
Antiseptic |
منتظم |
Regular |
|
مضاد الحساسية |
Antihistaminic |
غير منتظم |
Irregular |
|
غيرواعى |
Unconscious |
شحوب |
Pallor |
|
واعى |
Conscious |
المعدة |
Stomach |
|
مانع لافراز البول |
Anti-diuretic |
امعاء |
Intestine |
|
مضاد للتسمم |
Antitoxic |
بول |
Urine |
|
مانع تكون الجلطة |
Anti-thrombosis |
براز |
Stool |
|
تطبيق عملى |
Application |
جراحة |
Surgery |
|
التهاب مفاصل |
Arthritis |
شهية |
Appetite |
|
رحمى |
Uterine |
شريان ابطى |
Axillary artery |
|
مهبلى |
Vaginal |
شريان عضد |
Brachial artery |
|
الربو |
Asthma |
شريان سباتى |
Carotid artery |
|
سماعةالجنين |
Fetoscope |
شريان فخذى |
Femoral artery |
|
حمى |
Fever |
سائل |
Fluid |
|
مصاب بالحمى |
Feverish |
خريطة السوائل |
Fluid chart |
|
غرغرينا |
Gangrene |
توازن السوائل |
Fluid balance |
|
العقد العصبية |
Ganglion |
افرازات |
Secretion |
|
جهاز التنفس |
Respiratory System |
بلغم |
Sputum |
|
الجهاز القسمى |
Cardiovascular System |
يعصر |
Squeeze |
|
الامعاء والمعدة |
Gastrointestinal System |
يلاحظ |
Observe |
|
الجهاز التناسلى |
Genitourinary System |
حمام سرير |
Bed bath |
|
جهازالغدد الصماء |
Endocrine System |
معايير الجودة |
Quality standard |
|
الجهاز العصبى |
Neurological System |
التحكم بالعدوى |
Infection control |
|
إستغاثة إنعاش قلب رئوي |
Code Blue |
تصنيف المرضى |
Triage |
|
|
|
|
|
|
أوضاع الجسم |
Body Position |
تجاویف الجسم |
Body Cavities |
|
الوضعیة التشریحیة |
anatomical position |
التجویف الباطني |
Abdominal cavity |
|
وضعیة الإستلقاء |
decubitus position |
التجویف القحفي |
Cranial cavity |
|
وضعیة الإستلقاء الظھري |
dorsal recumbent |
التجویف الحوضي |
Pelvic cavity |
|
وضعیة فاولر |
Fowler position |
التجویف النخاعي |
Spinal cavity |
|
وضعیة ترندلبورج |
trendelenburg position |
التجویف الصدري |
Thoracic cavity |
|
أصناف الامراض |
Disease Categories |
وصف المرض |
Description of Disease |
|
الأمراض الإنحلالیة |
Degenerative Diseases |
حاد |
Acute |
|
الاِضطرابات الھورمونی |
Hormonal disorders |
حمید |
Benign |
|
الاِضطرابات المناعیة |
Immune disorders |
سرطانى |
Carcinoma |
|
الأمراض المُعدیة |
Infectious Diseases |
مزمن |
Chronic |
|
الاِضطرابات العقلیة والعاطفیة |
Mental and emotional disorders |
السبب |
Etiology |
|
الاِضطرابات الأیضیة |
Metabolic disorders |
تورم |
lesion |
|
السرطانية الامراض |
Neoplastic Diseases |
متكيس |
Cyst |
|
احتشاء عضلة القلب |
myocardial infarction |
ورم |
Parasite |
|
انسداد |
occlusion |
صبغه ملونه |
Gram stain |
|
القنوات الشریانیة السالكة |
Patent ductus arteriosus |
التهاب |
Inflammation |
|
التھاب الورید |
phlebitis |
فتق |
Hernia |
|
السدة القلبية |
plaque |
امراض الروماتيزم |
rheumatic heart disease |
|
الصمام الأبهرى |
aortic valve |
الأبهر |
aorta |
|
صدمة |
Shock |
جلطه |
Thrombosis |
|
تسارع القلب |
tachycardia |
تضییق |
Stenosis |
|
قمة |
apex |
سكتة |
Stroke |
|
شريان |
artery |
اغماء |
Syncope |
|
الشراين الصغيرة |
arteriole |
التھاب الورید الخثاري |
Thrombophlebit |
|
العقدة الجيبة الأذينية |
atrioventricular (AV) node |
الحزمة الأذينية البطينية |
AV bundle |
|
شعيرات دموية |
bundle branches |
الأذين |
atrium |
|
جهاز القلب والأوعية الدموية |
cardiovascular system |
الصمام الثنائى |
bicuspid valve |
|
أصوات القلب |
Heart sound |
الوريد الأجوف السفلى |
Inferior vena cava |
|
الشريان الرئوى |
Pulmonary artery |
الصمام المترالى |
Mitral valve |
|
الوريد الرئوى |
Pulmonary vein |
||
|
|
|||
|
|
|
|
|
|
|
|
مريض |
Patient |
العلامات الحيوية |
Vital signs |
|
اسم المريض |
Patient name |
الضغط |
Blood Pressure |
|
السن |
Age |
النبض |
Pulse |
|
النوع |
Gender |
الحرارة |
Temperature |
|
ذكر |
Male |
التنفس |
Respiration |
|
انثى |
Female |
الالم |
Pain |
|
الوظيفة |
Occupation |
غرفة |
Room |
|
الحالة الاجتماعية |
Marital History |
قسم |
Department |
|
متزوج |
Married |
العمليات |
Operation |
|
اعزب |
Single |
الطوارئ |
Emergency |
|
متزوج ويعول |
Married with |
اقسام الداخلى |
In patient |
|
مطلق |
Divorced |
العيادات |
Clinics |
|
نعم |
Yes |
دخول جديد |
New admission |
|
لا |
No |
خروج |
Discharge |
|
عادات خاصة |
Special Habits |
وقت |
Time |
|
تدخين |
Smoking |
تاريخ |
Date |
|
كحوليات |
Alcohol |
دبلوم تمريض |
Diploma nurse |
|
مرض |
Diseases |
افراد هيئة التمريض |
Nurse |
|
حساسية |
Allergy |
طبيب |
Doctor |
|
شكوى |
Complaints |
قبل الدخول |
Before admission |
|
تعليق |
Comment |
دخول |
Admission |
|
اجهزة الجسم |
Body Systems |
بعد الدخول |
After admission |
|
طبيعى |
Normal |
ادوية |
Medications |
|
غير طبيعى |
Abnormal |
حالى |
Present |
|
عام |
General |
العلاج الحالى |
Present medications |
|
ارتفاع |
Height |
الدواء |
Drug |
|
الوزن |
Weight |
الجرعة |
Dosage |
|
عينة |
Specimen |
عدد مرات |
Frequency |
|
وريد |
Vein |
الوقت- الفترة |
Duration |
|
شريان |
Artery |
المظهر العام |
General Appearance |
|
دم |
Blood |
الجلد |
Skin |
|
تاريخ المرض |
Past History |
الراس |
Head |
|
محطة تمريضية |
Nursing station |
توقيع |
Signature |
|
المرض عندالعائلة |
Family History |
العين |
Eyes |
|
فحوصات الجسد |
Physical Examination |
الاذن |
Ears |
|
فحص الصدر |
Breast examination |
الانف |
Nose |
|
تنميل الاطراف |
Numbness |
الفم |
Mouth |
|
ولادة طبيعية |
Normal labor |
اسنان |
Teeth |
|
ولادة قيصرية |
Cesarean section |
رقبة |
Neck |
|
عنق رحم |
Cervix |
الصدر |
Chest |
|
المخ |
Brain |
بطن |
Abdomen |
|
تورم |
Edema |
العظام |
Bone |
|
ازرقاق |
Cyanosis |
الحالةالنفسية |
Psychological Status |
|
صفرة |
Jaundice |
التشخيص |
Diagnosis |
|
مرض السكر |
Diabetes mellitus |
العوامل الخطرة |
Risk Factors |
|
الخطةالتمريضية |
Nursing care plan |
خطة رعاية |
Care plan |
|
اختناق |
Dyspnea |
ملحوظة |
Notes |
|
عسر هضم |
Dyspepsia |
وتر |
Tendon |
|
صعوبة بالبلع |
Dysphagia |
متابعة |
follow-up |
|
صعوبة فى النطق |
Dysphonia |
اسباب |
Reason |
|
السابق |
Previous |
تحاليل المعمل |
Laboratory Investigations |
|
اضطراب فى النوم |
Dyssomnia |
تخدير |
Anesthesia |
|
صعوبة فى التبول |
Dysuria |
بدايةالتخدير |
Start of anesthesia |
|
تقييم مجرى الهواء |
Airway Assessment |
نهاية التخدير |
End of anesthesia |
|
مجرى الهواء |
Airway |
مساعدة |
Assistant |
|
فصيلةالدم |
Blood Group |
نوع التخدير |
Type of anesthesia |
|
شمع الاذن |
Ear wax |
موضعى |
Local |
|
وجع الاذن |
Earache |
كلى |
General |
|
منظار بطن |
Laparoscope |
اجراءات |
Procedures |
|
استكشاف بطن |
Laparotomy |
قبل العملية |
Pre-operative |
|
التهاب الحنجرة |
Laryngitis |
بعد العملية |
Post-operative |
|
ورم ليمفاوى |
Lymphoma |
اثناء العملية |
Intra-operative |
|
دم النفس |
Lochia |
تقييم |
Sheet |
|
وجع فى الظهر |
Back pain |
تحويل المريض |
Referral |
|
صداع |
headache |
حساسية |
Sensitivity |
|
جرح |
wound |
الزهرى |
Syphilis |
|
جرح نافذ |
Stab wound |
الحنجرة |
Larynx |
|
وريد |
Vein |
بولينا |
Uremia |
|
شريان |
Artery |
حصوة المثانة |
Bladder Stone |
|
التهاب الفم |
Stomatites |
كلي |
Kidney |
|
يعانى من |
Suffer from |
ارتفاع الضغط |
Hypertension |
|
مضاد حيوى |
Antibiotic |
انخفاض الضغط |
Hypotension |
|
مضاد الحساسية |
Anti-allergic |
غيبوبة |
Coma |
|
مضاد للفطريات |
Anti-fungal |
شبه غيبوبة |
Semi coma |
|
مضاد للفطريات |
Anti-parasitic |
نزيف من الانف |
Epistaxis |
|
مانع الالتهاب |
Ant-inflammatory |
نبض سريع |
Tachycardia |
|
مضاد التسمم |
Anti-toxic |
نبض بطئ |
Bradycardia |
|
مطهر |
Antiseptic |
منتظم |
Regular |
|
مضاد الحساسية |
Antihistaminic |
غير منتظم |
Irregular |
|
غيرواعى |
Unconscious |
شحوب |
Pallor |
|
واعى |
conscious |
المعدة |
Stomach |
|
مانع لافراز البول |
Anti-diuretic |
امعاء |
Intestine |
|
مضاد للتسمم |
Antitoxic |
بول |
Urine |
|
مانع تكون الجلطة |
Anti-thrombosis |
براز |
Stool |
|
تطبيق عملى |
application |
جراحة |
Surgery |
|
التهاب مفاصل |
Arthritis |
شهية |
Appetite |
|
رحمى |
uterine |
شريان ابطى |
Axillary artery |
|
مهبلى |
vaginal |
شريان عضد |
Brachial artery |
|
الربو |
Asthma |
شريان سباتى |
Carotid artery |
|
سماعةالجنين |
Fetoscope |
شريان فخذى |
Femoral artery |
|
حمى |
Fever |
سائل |
Fluid |
|
مصاب بالحمى |
Feverish |
خريطة السوائل |
Fluid chart |
|
غرغرينا |
Gangrene |
توازن السوائل |
Fluid balance |
|
العقد العصبية |
Ganglion |
افرازات |
Secretion |
|
جهاز التنفس |
Respiratory System |
بلغم |
Sputum |
|
الجهاز القسمى |
Cardiovascular System |
يعصر |
Squeeze |
|
الامعاء والمعدة |
Gastrointestinal System |
يلاحظ |
Observe |
|
الجهاز التناسلى |
Genitourinary System |
حمام سرير |
Bed bath |
|
جهازالغدد الصماء |
Endocrine System |
معايير الجودة |
Quality standard |
|
الجهاز العصبى |
Neurological System |
التحكم بالعدوى |
Infection control |
|
إستغاثة إنعاش قلب رئوي |
Code Blue |
تصنيف المرضى |
Triage |
- Abbreviations
|
AF |
Atrial fibrillation |
|
APB |
Atrial premature beats |
|
APC |
Atrial premature contraction |
|
AV block |
Atrio ventricular block |
|
AV Junction |
Atrioventricular |
|
A-V valve |
A trio ventricular valve |
|
AVF |
Augmented vector foot |
|
AVR |
Augmented vector right |
|
AVR |
Augmented vector left |
|
CBS |
Catheter By bass surgery |
|
ECD |
Electro cardio Defibrillator |
|
ECG |
Electrocardiography |
|
ICD |
Implantable Defibrillator |
|
IVC |
inferior vena cava |
|
LA |
Left atrium |
|
LOC |
Level of Consciousness |
|
NCP |
Nursing Care Plan |
|
PACS |
Premature atrial contraction |
|
PVCS |
Premature ventricular contraction |
|
RA |
Right atrium |
|
SCA |
Sudden Cardiac Arrest |
|
SN node |
Sino atrial node |
|
SND |
Sins node dysfunction |
|
SVC |
superior vena cave |
|
SVT |
Supra ventricular tachycardia |
|
VF |
Ventricular fibrillation |
|
VT |
Ventricular tachycardia |
|
MI |
Myocardial infaraction |
|
ECG |
Elecrtocardial gram |
|
CPR |
Cardiopulmonary resuscitation |
|
DC |
Defibrillator shock |
|
CPR |
Cardiopulmonary resussitaion |




The Reviewer
Nursing procedures manuals were prepared for 2012 and updated for 2017
Procedural work guide for the Reception and Emergency Department (Central Nursing Administration)
Procedural work guide for the intensive care department (Central Administration of Nursing)
Procedural work guide in the Artificial Kidney Department (Central Administration of Nursing)
Emergency nurses training manual
First aid guide
(The American Hope Project in cooperation with the Egyptian Red Crescent)
Nursing Procedures Quality Handbook
Your guide to the basics and skills of nursing (Egyptian-Korean side)