
Chapters Seven and Eight
- Standard infection control procedures
Preventing the spread of infection between patients in internal wards and each other and following safe methods to prevent its spread.
Definition of infection:
It is the entry of the disease-causing agent into the human body, its multiplication, and the occurrence of signs and symptoms of the disease.
Hospital infections:
It is an infection that a person acquires while receiving health care in a hospital, and its symptoms appear after 48 hours or
More than the patient being admitted to the hospital.
The causative agent of the disease:
1) Viruses such as (all kinds of influenza, HCV, HBV, AIDS, etc.)
2) Bacteria such as (meningitis, tuberculosis)
3) Fungals (Tinia, Monilia)
4) (parasites such as (schistosomiasis, ascaris, amoeba)
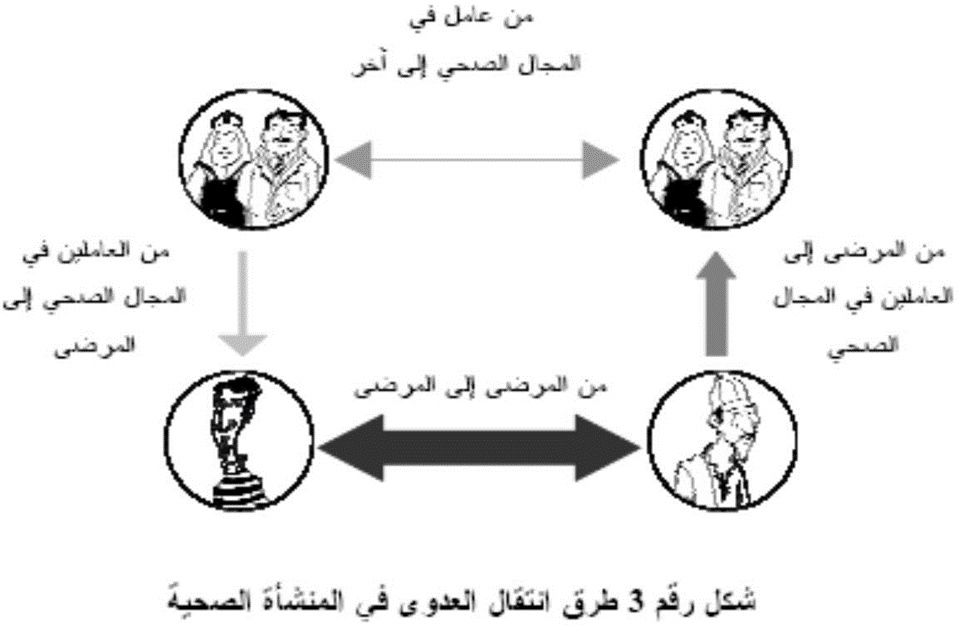
Methods of transmission of infection within the health facility:
Standard infection control precautions include the following:
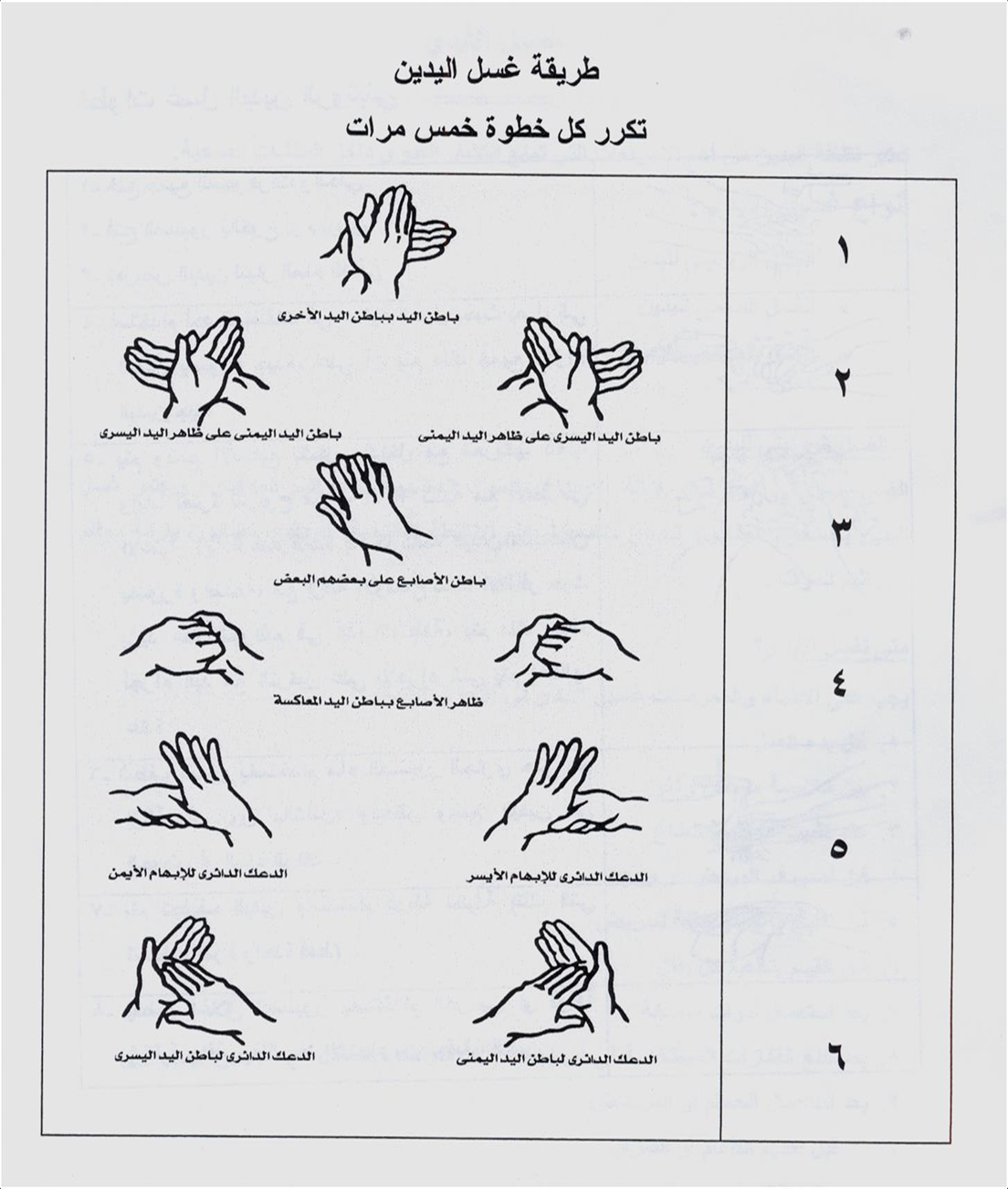
1- Hand hygiene and disinfection:
Hand hygiene is considered one of the most important measures that prevent the spread of infection within health facilities.
- The five moments (positions) for washing hands:
|
|
|
|
|
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|||
|
|
|
|
|
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
60 – 40 )WHO2009( |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
30-20 WHO2009 |
|
|
|
|
|
|
90-60 WHO2009 |
|
|
|
|
Hand cleaning methods:
Hand washing method:
2- Personal protective tools:
Gloves:
There are three main types of gloves used in health care facilities, the use of each of which varies according to the type
The task assigned to the health service provider.
A- Sterile gloves: They are used in penetrative interventions and are characterized by being sterile and can only be used once.
Its uses:
• Before surgical operations
• Before medical interventions that require a sterile method to be completed, such as: (installation of a central venous catheter, all operations
Puncture, when dealing with large burns, preparing and mixing solutions and chemotherapy drugs for oncology patients
B- Non-sterile rubber gloves: This type of glove is characterized as non-sterile (clean) and is used only once.
Its uses:
• When giving intravenous solutions, installing a peripheral intravenous catheter, and before intravenous injection (except for patients
immunocompromised (
• When changing bandages, and when dealing with cleaning any of the devices or other equipment contaminated with blood, urine, or
Stool or any other secretions.
• When dealing with samples of patient tissues or fluids or vessels containing them
• When performing respiratory suction or when dealing with mucous membranes, such as examination or care.
With the mouth.
• Cleaning and disinfecting traces of blood or body fluids.
C- Heavy-duty gloves: These gloves are used when dealing with waste or contaminated tools and when carrying out work
Cleaning, especially in the case of sharp residues. It can be used repeatedly after cleaning and disinfecting it appropriately once
Been punctured or torn.
Its uses:
• Dealing with medical waste (waste bags and safety boxes)
• Use of detergents, disinfectants and chemicals.
• Cleaning and disinfecting the environment.
• Cleaning machines
• Dealing with blood spills in the presence of sharp waste.
Abayas:
1) Unclean, non-sterile gowns:
It is worn while performing some medical procedures that could lead to the dispersion of spray, blood, and body fluids, or during
Procedures that lead to contamination of workers’ clothes or uniforms with microbes or infectious materials.
2) Sterile gowns:
Sterile gowns must be worn during all surgical operations and some important medical interventions (such as implantation).
Central venous catheterization, mixing solutions for immunocompromised patients and newborn children (preferably
It is made of materials impermeable to liquids.
- The abaya (whether clean or sterile) must be used once and then disposed of in the hazardous waste bin.
If it is single-use or in the laundry basket if it is frequently used.
- It is prohibited to use the same gown to care for more than one patient.
Medical gowns, like all personal protective equipment, are used for one provider to care for one patient and for one procedure
One.
Plastic bibs:
Single-use aprons are worn when performing some medical procedures that could lead to the dispersion of spray and blood.
And bodily fluids or while performing some procedures that lead to contamination of clothes or uniforms of workers with microbes
Or infectious materials.
Headwear:
It is recommended to wear single-use head coverings, which contain the hair to prevent hair loss or spreading
Microbes.
Examples of uses:
• Surgical procedures in the operating room.
• Mixing intravenous solutions.
• Sterilization department (packaging area)
• Kitchen (during cooking/preparing meals)
The traditional head covering (scarf or hijab) is not a substitute for the head covering intended for patient care.
Providing protection for the face (eyes, nose and mouth):
The health care provider should be careful to wear a face mask (face shield) or eye protection (goggles).
And the surgical mask together when the possibility of his face being exposed to blood spray or body fluids flying from the patient increases.
Respiratory masks:
1) Surgical mask: A mask that tightly covers the nose and mouth should be used when exposed to respiratory secretions.
of the patient or splashes of blood and other body fluids as part of standard precautions.
Indications :
• surgeries.
• Some invasive medical interventions (such as installation of a central venous catheter, spinal fluid aspiration, injections into
spinal fluid )
• With immunocompromised patients.
• When there is a possibility of exposure to any contaminated spray (such as exposure to surgical instrument washing spray or suctioning device secretions).
respiratory
In addition, patients and workers infected with droplet-borne diseases wear respiratory masks to prevent
Infection.
2) High-efficiency respiratory mask: used when exposed to airborne diseases
Indications for use:
• Preventing some diseases such as: (active tuberculosis, measles, chicken pox, infectious diseases)
The emerging coronavirus (SARS/Coronavirus/....) due to its seriousness.
Foot protectors:
Sabo: A protector that covers the foot, provided that it is not permeable to fluids.
Boot: A protective shoe that covers the foot and leg.
Indications for use:
• In operating rooms
• When cleaning surgical instruments
• Cleaning and disinfecting the environment
• Cooking, collecting and transporting waste.
Respiratory health precautions and cough etiquette.
1. Identifying the patient who may have a respiratory infection:
Health facility workers must pay attention to the need to quickly detect patients with an existing respiratory infection
Their arrival to the health facility.
Provide instructional panels explaining respiratory health precautions and cough etiquette, which include:
- Cover the mouth and nose when sneezing and coughing.
Use paper tissues only once and dispose of them in the trash.
Wash hands after contact with respiratory secretions.
The patient must provide information about his medical condition when logging in.
2. Providing the following supplies and supplies at the reception point and outpatient clinics: surgical masks, paper tissues, and a basket.
Trash, equipment and supplies for washing and disinfecting hands.
3. Apply the respiratory health precautions and cough etiquette mentioned above to all patients who show symptoms
Respiratory infection, including facility workers.
4. Isolating patients likely to have a respiratory infection from the rest of the patients.
5. Establish rules for visiting these patients, including:
Postpone the visit as much as possible if there is no urgent need.
Prevent visitors with symptoms of respiratory infection from entering the patient care area.
6. Responsibilities of health service providers:
- Monitor the application of respiratory health precautions in addition to precautions when dealing with patients who suffer from
Respiratory infection, and when there is suspicion that it may be an airborne infection, isolation precautions are applied
Airborne diseases.
- Prevent workers with respiratory infections from direct contact with patients. When necessary, they are obligated
By wearing a respiratory mask and washing hands frequently.
- Ensure the implementation of the policy of vaccinating health facility workers with the necessary vaccines, including influenza vaccination
Seasonal annually.
7. Communicate with the relevant departments in the Ministry to learn about the latest developments regarding influenza and systemic infections
Respiratory infection, and monitoring and follow-up activities are intensified to quickly discover new cases.
8. In the event of increasing rates of respiratory infections and a high rate of influx of cases into the facility, an allocation is made
A triage and classification area to isolate potentially infected patients from the rest of the patients and direct them to designated care areas
for them .
3- Safe injection:
A safe injection is one that does not cause harm to the recipient, nor does it expose the service provider to any risks that can be avoided.
It does not produce any waste that may harm others or the environment.
Examples of infections reported to occur through injections:
|
|
|
|
|
|
, |
|
The basic components of the injection:
1. Use sterile injection tools
2. Preventing contamination of injection tools and fluids.
3. Protecting the health service provider from acupuncture or sharp tools.
4. Protecting the environment and society by preventing access to waste from the injection process.
5. Some practical methods to be followed:
- Hand hygiene
- Use gloves
- Follow the necessary precautions when using multi-dose medication containers.
- Preparing the skin before injection: The skin must be cleaned before injection and then disinfected with a suitable antiseptic such as alcohol.
- Follow the closed system for intravenous injection.
- Follow the non-touch method: If any part of the syringe is touched, it is considered contaminated.
4 - Precautions for storing, preparing and handling medications:
The safe storage, preparation and handling of medical treatment that is injected, whether intravenously or otherwise, is considered one of the most important components.
Anti-contamination methods to reduce infection rates within health facilities.
Obligatory requirements:
1. Medications should not be prepared in syringes in advance and stored until treatment is carried out.
2. The new syringe should not be opened except for actual use.
3. One syringe should not be used for more than one patient, even if the tooth is changed.
4. The syringe must not be reused when withdrawing any treatment or solution from its designated container.
One syringe tooth - one syringe body - one procedure
5. It is prohibited to use solutions prepared for intravenous drip to dissolve medications (single ampoules of sterile water must be used
the use (
6. The rubber cover of treatment containers must be disinfected with a suitable disinfectant such as alcohol and left to dry before inserting the syringe tip.
7. Multi-dose containers should be allocated to one patient whenever possible, and if necessary, this should be done in one place
Designed for treatment preparation.
8. When mixing and compounding solutions and treatments, it is preferable to do so in the clinical pharmacy, in a central location in the medical facility.
If they are not available, a separate room must be prepared for mixing and installing solutions and treatments.
5 - Reprocessing medical machines and tools:
A. Cleaning: is the removal of suspended materials (such as organic and inorganic materials) present on the surface of the tools that should be
Reprocessed. It can be done either manually or automatically using washing machines, usually using running water and detergents.
B. Disinfection: Disinfection is done in one of two ways: either using heat or using chemicals. An operation must be performed
Careful cleaning before the disinfection process, as organic materials (such as blood and body fluids) hinder the efficiency of disinfection in the elimination
On microbes.
C. Sterilization: Eliminate all forms of microbial life, including bacterial sacs. Sterilization methods can be divided
Basically for the following:
First: thermal sterilization:
Wet heat sterilization: using steam under pressure from an autoclave.
Dry heat sterilization: Sterilization using dry heat using dry heat in an electric sterilization oven.
Second: Sterilization under low temperatures
Third: Other means of sterilization: such as sterilization with gamma rays and sterilization by filtration.
6 - Cleaning and disinfecting the environment:
Environmental cleanliness is the process of removing organic materials, dust, and dirt, which leads to the elimination of a large percentage of
Microbes.
Common cleaning methods:
1. Dry cleaning method (sweeping): Dry brooms, dry cloths, and dusters should not be used in places
Treating patients as it leads to the spread of bacteria-carrying particles.
2. Wet cleaning method: Wet cleaning is done using a damp cloth to clean surfaces with an additive
Detergents or disinfectants
7- Textile reprocessing:
Basic principles of infection control when dealing with sheets, covers and furnishings:
- Individuals who collect, transport, sort and wash sheets and blankets should receive the necessary training.
They should also wear the necessary protective clothing, in addition to facilitating their access to hand-washing areas.
Dirty sheets and blankets should be removed very carefully and quietly, while reducing the movements necessary for this as much as possible.
So that this does not cause the spread of microbes in the air.
- All used sheets and covers are considered contaminated and there is no need to distinguish the colors of collection bags.
- Moving dirty sheets and blankets. Bags containing dirty sheets and blankets are not allowed to be transported via
Carrying it by hand, it is preferable to use carts or containers with a lid.
- You should avoid touching dirty or contaminated sheets and covers.
8 - Health care waste management:
First: Ordinary (semi-domestic) waste: These wastes are similar in composition to household waste.
Second: Health care waste: It can be divided into two types:
1. Non-hazardous waste: examples include packaging papers for medical equipment and supplies.
2. Hazardous waste: includes: infectious waste, autopsy and surgical waste, sharp instrument waste, waste
Chemicals, pharmaceutical waste, radioactive materials, heavy metals, etc.
Definition of procedure:
• Obligating workers in internal departments to use safe methods to prevent hospital infections.
procedures :
First: Special procedures for the health service provider:
Medical service providers (doctors and nurses) do the following:
1. Wash hands hygienically before dealing with the patient.
2. Change gloves between one patient and another and between one procedure and another.
3. Wash hands hygienically when performing the following procedures: -
4. Before installing a peripheral cannula and urinary catheter.
5. Before giving non-oral solutions and medications
6. Wear a plastic apron when exposed to the patient's blood, fluids, and secretions
7. Change personal condoms if they are contaminated at any time, even if for the same patient.
8. Washing hands between one procedure and another, even if it is for the same patient.
9. Disposing of urine and feces in the patients’ bathroom and throwing in water and chlorine afterward.
Second: When preparing intravenous solutions:
1. The nurse prepares all tools before starting work (sterile gloves, dressing gown, and belts for mixing solutions).
2. The department supervisor allocates a clean place for preparing medications and solutions in the unit and is not used for any other purpose
3. The department supervisor assigns a nurse responsible for mixing solutions in case there is a need to mix solutions to prevent
The spread of hospital infections, and alternatives are also allocated in the event that the responsible nurse is not available.
4. The nurse washes hands hygienically before starting work on mixing solutions, and uses a new sterile syringe.
With each type of solution. (Every time you use a new sterile syringe.)
Third: When giving medications by injection:
1. The nurse washes hands hygienically, wears gloves, and disinfects the site of intervention with alcohol.
2. The nurse uses the ampoule with distilled water only, not salt solution, and the remainder is disposed of immediately
Fourth: Special procedures for patient care:
1. Every nurse responsible for a patient takes care of the patient’s general hygiene.
2. Doctors and nurses should avoid touching wounds with their hands, and non-contaminated methods should be followed when caring for wounds.
Use a sterile dressing bottle every time you change the patient's wound.
3. The doctor and nurse use sterile spare gloves on the wound and use the non-touch method
4. The doctor cleans the wound using a surgical mask and a piece of cotton or gauze moistened with an antiseptic solution, such as
Surgical alcohol or betadine. It is not allowed to touch the wound with the hands.
5. The doctor isolates patients with infectious diseases in an isolation room in a unit in the internal department.
6. The department supervisor and the responsible nurse follow isolation precautions with isolation patients as per policy
For insulation.
Fifth: Special procedures for employees within departments:
1. The infection control team vaccinates all employees in the unit against hepatitis B.
2. The occupational safety and health officer ensures that all employees in the department are free of infectious diseases.
3. All medical service providers wash hands before and after dealing with the patient.
4. All medical service providers wash hands between one procedure and another, even if it is for the same patient.
5. All medical service providers wear protective clothing while dealing with the patient.
6. All medical service providers are committed to not smoking, eating or drinking inside the burn unit.
Sixth: Special procedures for visitors:
1. The visiting officer limits the number of visitors to only two per patient, and then they do so in succession, as permitted
The patient's condition .
2. The doctor evaluates each patient individually and determines the duration of the visit so that it does not affect the patient’s general condition
3. The security officer warns visitors not to smoke, eat, or drink inside the department.
4. The nurse warns visitors not to touch any of the tools or devices around the patient.
Seventh: Department environment:
1. Sufficient space must be left around each patient's bed for the medical equipment used and for the service provider to pass through
Health care is easy to reduce the risk of transmitting infection between individuals.
2. There must be a safety box next to each bed to dispose of sharp waste.
3. There must be a physical separation between the patient and the other that is easy to clean weekly or when it becomes contaminated at any time or between
The patient leaves and before another patient enters.
Eighth: Cleanliness of the department environment:
1. The worker wet-cleans the unit and surfaces daily from top to bottom and at the beginning of each shift
Getting dirty at any time with soap and water, then with chlorine 1000 parts per million. Ask about dilution. Control unit.
The infection must be reduced according to the concentration of chlorine present in the institute.
2. The worker cleans the unit, surfaces, and all work areas (inventory) at least once every week or two
It starts from top to bottom in the previous manner.
3. The worker cleans the patient's area and changes the bedding daily between the patient and the other if they become dirty.
4. The worker removes a large blood spill immediately by first placing a single-use cloth on the area
Spillage, then concentrated chlorine is placed as it is from the bottle, then it is lifted from the ground, then cleaned a second time with a cloth with a soft cloth.
Single use in the same way if there are traces of it, then clean with soap and water and then dry.
5. The worker removes the small bloody spill immediately. First: Wipe the spill with a reusable cloth
One moistened with 5000 parts per million chlorine. The Infection Control Unit asks about dilution so that the dilution is done accordingly
The concentration of chlorine present in the institute, then the piece of cloth is disposed of in the red basket, and this process is repeated in its case
If there is a trace, then the place is cleaned with soap and water, then dried well.
6. All health service providers are committed to separating waste so that contaminated waste is disposed of in the red bin
Regular waste is in the black bin, and sharp waste is in the safety box.
