Chapters Seven and Eight
| Site: | EHC | Egyptian Health Council |
| Course: | Developing the administrative skills of nursing leaders |
| Book: | Chapters Seven and Eight |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 1:32 PM |
-Crisis and disaster management in hospitals
What is the difference between crisis and disaster?
The Crisis :
Threat means an expected or unexpected danger to the goals, values, beliefs, and property of individuals, organizations, and nations that limits the process of
Make decision.
It is a situation resulting from environmental changes that generate crises and includes a degree of danger, threat, lack of time, and surprise, and requires
Use innovative and rapid management methods.
Disaster:
Disasters caused by human action, negligence, error, or involving system failure are called man-made disasters.
Man-made disasters are in turn classified as technological or social. Technological disasters are the results of technology failure
Such as engineering failure, transportation disasters, or environmental disasters. Social disasters have a strong human motive, like criminal acts
Stampedes, riots and war. It is an environmental disruption in the relationship between humans and their environment, largely represented by a sudden or dangerous event.
Society needs to make exceptional efforts to organize foreign aid and international aid.
Meaning of crisis management:
Crisis management means the art of controlling an emergency situation through predicting crises and sensing and monitoring internal or external variables
The external factors that generate it, mobilize available resources, raise the efficiency and capacity of the decision-making system to confront it, and reduce losses
minimum.
Symptoms of the crisis:
1. Surprise: It is an unexpected event, a quick and mysterious event, or a sudden situation in which the necessary creative events occur to surprise the decision maker.
2. The seriousness of the threat: which may lead to massive material or human losses that threaten stability and sometimes lead to the elimination of organization entity.
3. Confusing: It threatens the main assumptions on which the system is based, and creates a state of anxiety, tension, and mistrust in the available alternatives, especially in light of the lack of information, which doubles the difficulty of decision-making, and makes any a decision that involves some degree of risk.
4. The lack of time available to confront the crisis: events occur and escalate in a conflicting and perhaps severe manner, which leaves parties lost crisis, sometimes the ability to control the situation and understand it well, where efforts must be focused to make decisive decisions and quickly in a time of distress and pressure.
5. The multiplicity of parties and forces influencing the occurrence and development of the crisis, and the conflict of their interests, which creates great difficulties in controlling and managing the situation. Some of these difficulties are administrative, material, human, political, environmental, etc.
Steps to deal with the crisis:
• Forming a work team for times of crises and providing it with the best personnel, equipment, and tools.
• Planning time during crises and making use of every minute to mitigate the impact of crises.
• Raising the morale of workers in times of crises, making them feel enthusiastic, energetic, and committed to work.
• Creativity and innovation in difficult situations and igniting the spirit of creativity among employees to provide unprecedented solutions and opinions.
• Solve problems in times of crisis by identifying the problem, conducting counseling, and then choosing the most appropriate solution from the available solutions.
Disaster division:
According to location, it is divided into:
Internal disasters.
External disasters.
According to the number of victims, they are divided into:
Small disasters (the number of victims does not exceed 25)
Moderate disasters (the number of victims does not exceed 100)
Major disasters (the number of victims exceeds 100).
According to the reasons, they are divided into:
Natural disasers .
Man-made disasters.
Types of disasters:
- Natural disasters.
- Epidemics.
- Disasters resulting from transportation.
- Technological disasters.
- Terrorism disasters.
Tornadoes :
- The main health risks from tornadoes and hurricanes lie in the risk of drowning from storms over land.
Most hurricane-related deaths are caused by drowning.
- Secondary health risks include injuries resulting from flying fragments caused by strong winds.
- The nurse can provide direct care in cases of previous head injuries and drowning emergencies.
Floods:
- Floods may develop very quickly after a rapid rainstorm, or during a short period of prolonged rain
Or rapid snow melting.
- The main danger from floods is drowning.
- In the long term, health concerns from floods lie in the development of diseases from water pollution and lack of hygiene.
Earthquakes:
- A problem of great global concern
- Main health problems related to earthquakes:
- Injuries resulting from the collapse of facilities.
- Most injuries among trapped people occur at the time of the earthquake.
- One of the most well-known preventive strategies is to prevent structures from collapsing.
- There is recognition of the need to develop better strategies to rescue people from collapsing buildings.
Volcanoes:
- Although rare, it can be catastrophic when it occurs.
- Health outcomes associated with volcanic eruptions:
1. Respiratory diseases resulting from inhalation of ash Dr.
2. The danger for individuals near the volcano is from the presence of lava flows, or more likely from
Mudflows.
Patterns of deaths and injuries:
- Disasters involving water are the largest cause of the increase in the number of deaths.
- Floods and storm surges all cause the number of deaths to increase by a greater proportion than the number of injuries.
- As for earthquakes and disasters associated with strong winds, they cause an increase in the number of injuries by a greater percentage than the number of deaths.
Expected risks:
- Road accidents.
- Fires.
- Fires and collapses inside the hospital building.
- Radioactive contamination in the nuclear medicine building.
- Mass poisoning.
- Chemical leakage.
A plan must be designed to confront disasters and crises for each hospital, according to its expectation of disasters, its capabilities, and the number of employees in it.
And the number of sick and injured people visiting it. Therefore, it is necessary to make a solid plan, run committees in it, and determine the role of each member
Members of committees restricted to the plan.
Disaster management resources:
- Forming an emergency and disaster response committee.
- A list of emergency workers’ telephone numbers: (doctors - nurses - employees - workers).
- The structure of emergency and hospital personnel within 24 hours.
- Schematic drawing of the hospital buildings.
- Training program for the disaster management unit.
Formation of the Crises and Disasters Committee from:
- Chairman of Board of Directors . - Director of therapeutic affairs.
- Deputy Director of Crisis Management. - Head of the toxicology department.
- All hospital and hospital managers (such as the director of emergency care and surgery).
- (Director of Pharmacy, Engineering, Communications and Warehouses).
- Managing Director.
- From nursing, it includes the director of nursing, the head of the trauma nurse, the head of the reception nurse, and the head of nursing
- Surgery and Operations Departments and Head of Crisis Nurse)
The special role of nurses when disasters occur:
- Determine the size of the disaster
- Identifying the health needs of affected groups
- Setting priorities and goals
- Identify actual and potential public health problems
- Identify resources needed to respond to identified needs
- Cooperation with professional specialists and governmental and non-governmental agencies
- Unifying the chain of command communications
Communication...the key to success:
- Nursing organizations must have accurate and comprehensive records for all members of the organization
- In addition to an organized plan that includes:
- Cooperation and coordination with local authorities
- Hot line
- Inform nursing staff about where and how to report (with documentation)
- Ensure there is a coordinator to prevent any potential chaos
- Ensure that there are means of communication between patients and their families.
The need for training in disaster nursing:
- More than 11 million nurses around the world:
- It forms the backbone of the health care system
- Represents the front line of health care workers with direct contact with the public and contributes to the health of individuals
families, communities, and the world
- Nursing schools provide little or no information about disaster nursing. (World Health Organization, 2008)
- There is a shortage of trained educational personnel and colleges.
Topics to be covered in disaster nursing training:
- Organizing and planning the nurse’s work environment.
- Communication (what should the report be written about and to whom should it be sent)
- Working in destroyed facilities and damaged equipment
- Patient and worker safety
- Working with the team (being aware of each member’s responsibility and role)
- Control of disease infections
- Psychological and mental support.
When an earthquake occurs, nurses in the departments must follow some instructions:
- Complete calm, reassurance and presence with patients.
- Do not get down quickly, run away, leave the department, or create a state of terror for the patients.
- Follow up heart patients carefully.
- Quick call the emergency number via Soweto.
- If everyone feels a strong wind and there is a possibility of the building collapsing, everyone must go down under a cover such as a bed or being next to a concrete column.
- The head nurse or her representative goes over all the roles and checks on the patients.
Job duties and job cards for nursing staff members:
A- A work card for the head of the nursing staff or her representative: during disaster response:
- The presence of the head of the nursing staff immediately when the disaster is announced.
- Follow up on the attendance of nursing staff members registered in the six-call period.
- Coordinating work between the emergency department and other departments to receive victims.
- Ensure the presence of cleaners in all departments.
- Ensure the presence of employees responsible for warehouses, maintenance and entry who are registered with the Disaster Committee.
- Ensure the availability of all medical supplies, tools and devices necessary to prepare to receive victims in the reception department intensive care, operations and all internal departments.
- Continuous supervision of the performance of the nursing staff in all departments.
- Ensure that victims’ data is recorded in disaster records and that supplies used are recorded in victim forms.
- Writing reports for the hospital director to monitor performance and improve performance.
B- A work card for the reception department supervisor during disaster response:
- Attending the hospital immediately when called when a disaster occurs.
- Participate in sorting and classifying victims in the reception department.
- Preparing the necessary medical supplies, tools and devices in all reception rooms.
- Participate in helping victims and providing them with the necessary care.
- General supervision of the performance of the reception nursing staff in providing assistance to victims.
- Giving orders not to use phones for personal calls.
- Supervising the implementation of doctors’ orders (including treatment, x-rays, and tests).
- Supervising the immediate bringing of test results and rumors.
- Inform the Emergency and Operations Department of preparations to receive victims who need operations.
- Supervising the recording of victims’ data in disaster records.
- Supervising the cleanliness of the reception rooms immediately after treating the victims and transporting them to the internal departments, while placing the waste in bags red and sent to the incinerator.
- Delegating reception nurses to work rules according to the color of the card that distinguishes their performance:
▪ A- Red color // Cardiopulmonary recovery nurse.
▪ B- Yellow color// General surgery case nurse.
▪ C- Green color // Nurse for mild cases.
▪ D- Blue color // Medicines and supplies nurse.
▪ D- Blue color // Victim triage and classification nurse.
▪ T- Yellow color // Coordination Nurse) handles the nurses’ needs during their work.
- Writing a report to the Chairman of the Disaster Committee on the nurses’ performance while treating victims.
C- Work card for the operations department supervisor during disaster response:
- The presence of the surgical and emergency nursing supervisor when called when a disaster occurs.
- Ensure the presence of all nurses in the operating rooms.
- Ensure the presence of all anesthesia nurses in the operating and recovery rooms.
- Ensure the presence of all nurses responsible for machines and sterilization of operations.
- Ensure the presence of a nurse responsible for supplies in the operating department.
- Ensure the presence of a pharmaceutical nurse in the operations department.
- Ensure the presence of cleaning workers in the operations department
- Ensure that all medical devices in the operations department are working, exclude broken devices and send them to the maintenance department immediately.
- Ensure that a large number of brushes, clothing, and sterile instruments are available in the operating rooms.
- Supervising the dispensing of supplies and medications in operating rooms
- Supervising the performance of nurses while performing operations on victims.
- Supervising the cleanliness of operating rooms after each operation.
- Increasing the number of operating trolleys to transport injured people using the trolleys of some departments.
- Supervising the disposal of waste by placing it in red bags. The section, date, and time are written and placed in the bag
Garbage to be burned in the engine.
- Supervising the placement of the laundry used during operations with the used laundry holder and placing it in the special room with used laundry.
- Supervising the transfer of victims from the operating room to the recovery room and then to other departments.
- Ensure that victims’ data is recorded in notebooks for disaster cases and ensure that the supplies used in the disaster are recorded victims' form.
- Writing a report to the Chairman of the Disaster Committee regarding the incapacity that occurred, if any, and the nurses’ performance while performing operations on the victims.
Note: In the event of disasters, surgical operations are canceled and the operating rooms become hospital rooms for performing operations on victims’ cases.
D- Work card for the supervisor of the intensive care department during disaster response:
- Attending the hospital immediately when called when a disaster occurs.
- Ensure the presence of a cardiopulmonary recovery nurse.
- Ensure the presence of a general surgery nurse.
- Ensure the availability of a nurse for medications and supplies.
- Ensure the presence of a coordination nurse (who handles the nurses’ needs during their work).
- Distributing nurses to intensive care beds, 2 nurses per bed, to give them the necessary care.
- Assisting department nurses to assist if there is a shortage, and these nurses are distributed for handling, coordination, and coordination he relies on her to take care of a sick person.
- Preparing the medical supplies, tools and devices necessary to receive victims in the intensive care department.
- Participate in providing first aid to victims and providing them with the necessary care.
- General supervision of the performance of nurses in the intensive care department while receiving victims.
- Giving orders not to use phones for personal calls.
- Supervising the implementation of doctors’ orders (such as treatment, scans, and tests), and supervising the bringing of the results of the tests and scans immediately.
- Inform the Emergency and Sixth Operations Department of preparations to receive victims who require operations.
- Supervising the recording of victims’ data in disaster records.
- Supervising the cleanliness of intensive care rooms immediately after treating victims, while placing waste in red bags and sending it away to the Holocaust.
- Writing a report to the Chairman of the Disaster Committee on the nurses’ performance while treating victims.
It is a business card for supervisors during disaster response:
- Attend the hospital immediately when called and announce when a disaster occurs.
- Evacuate beds occupied by stable cases by informing the doctors and the head of the department.
- Preparing new mattresses for all beds to prepare for the entry of infected people.
- Ensure the presence of all department nurses.
- Ensure the availability of a nurse for medications and medical supplies.
- Ensure the presence of cleaners in the department.
- Supervising the dispensing of medications for each case of the victims.
- Supervising the taking of laboratories and x-rays for all infected people, and bringing the results of the tests and reports to each the injured.
- Supervise the implementation of treatment, take vital notes for all victims and ensure that nurses do nursing care for every injured person.
- Supervising the cleanliness of all department rooms immediately after treating victims, and placing waste in red bags and send it to the incinerator.
- Writing a report to the Chairman of the Disaster Committee on the nurses’ performance during aiding, receiving, and providing nursing care for the victims.
Action in the event of a fire:
- Press the alarm button located next to the counter on the floor.
- Pull the patient’s bed out of the room and evacuate the patients from the department under the supervision of the head nurse or her representative during shifts and staying up late.
- Evacuating patients from the hospital by transporting them to the bed via elevator, in the event that the electricity supply to the hospital is cut off unable patients are carried.
- Take down the room's curtains.
- Evacuate the floor of visitors.
- Close doors and bathrooms to prevent the spread of fire.
- Trying to put out the fire using firefighting equipment in the building.
- The maintenance department disconnects the electrical current according to the situation.
- The civil defense team acts quickly to extinguish the fire.
- If a fire occurs in the care or operations department, the maintenance department separates the gases from the critical departments and monitors ventilator patients are given care or operations using cylinders or manually until they are transferred according to the situation.
- Containing the fire and trying not to spread it anywhere else.
Extinguishing means or tools:
Providing these tools in all hospital areas:
- Fire extinguishers in front of elevators filled with carbon dioxide gas.
- Dry powder device on each floor. - Fire hydrants and hoses on the roads.
- A container containing sand to be used in some fires that cannot be extinguished with water.
- Blankets next to exits for use during a fire.
- Risk Management
introduction :
Traditional risk management focuses on risks resulting from physical or legal causes (for example: natural disasters, fires,
accidents, death and lawsuits). On the other hand, financial risk management focuses on those risks that can...
Manage them using financial swap instruments.
Risk management is not limited to public institutions and organizations only, but also to all activities, long and short
Long term. The benefits and opportunities of risk management must be considered in relation to the various affected stakeholders and not only in...
Its relationship to the organization’s activity.
Regardless of the type of risk management, all major organizations as well as smaller groups and organizations have a team
Risk management specialist.
Danger:
• It is the possibility of something undesirable to happen.
• Measuring the probability of a specific undesirable event that results in undesirable consequences, including losses or injuries.
Risks :
• Risk can be defined as a complex combination of the probability of an event occurring and its consequences.
• Risk is also a link between the probability of an event occurring and the consequences of its occurrence.
• The risks facing any organization and its activities can result from external and internal factors. It can be further divided into
Types of risks such as strategic, financial, operational, environmental, security, safety...etc.
• Risk management is increasingly referred to on the basis of its association with the positive and negative aspects of risk, and therefore takes
The standard takes into account risks in terms of both negative and positive aspects.
• In the area of safety, it is generally observed that only negative results are considered, which has led to focused risk management
Safety prevents and reduces damage.
Classification of the organization's activities:
• Strategy: It is concerned with the long-term strategic goals of the organization, and can be affected by several factors, including (extent
Availability of capital, political and sovereign risks, legal and legislative changes, reputation, and environmental changes.
Natural (.
• Operational: It is concerned with the aspects of daily activity that the organization faces during its pursuit of achieving strategic goals.
• Financial: It is concerned with the effective management and control of the financial aspects of the organization and the impact of external factors such as availability
Credit, exchange rates, interest rate movements and various other market exposures.
• Knowledge management: concerned with the effective management and control of knowledge sources, production, and other protection factors
and communications. External factors may include unauthorized use or misuse of intellectual property,
Power outages, and technological competition. Internal factors may include the failure of administrative systems or the loss of important elements
Manpower.
• Compliance with laws: concerned with aspects such as health and safety, environment, commercial specifications, consumer protection,
Information systems protection, employment and legal aspects.
Risk Management
• It is an essential part of the strategic management of any organization.
• They are the procedures that organizations follow in an organized manner to confront the risks associated with their activities, with the aim of achieving benefits
Sustainable outcomes from each activity and portfolio of all activities.
• The primary focus of good risk management is to recognize and address these risks.
• Risk management helps to understand the potential positive and negative aspects of all factors that may affect the organization,
It increases the probability of success and reduces both the probability of failure and the uncertainty of achieving the overall goals of the organization.
• Risk management activities must be continuous and constantly evolving and linked to the organization’s strategy and how to implement it
The strategy. It must deal in a systematic manner with all the risks surrounding the organization's activities in the past
The present and the future in particular.
Risk management protects and adds value to the organization and various stakeholders by supporting the organization’s objectives
road :
• Provide a framework for the organization to support the implementation of future activities in a consistent and controlled manner.
• Developing decision-making, planning and prioritization methods through a comprehensive and organized understanding of the organization’s activities,
And the negative and positive changes and opportunities available.
• Contributing to the effective use (allocation) of the capital and resources available to the organization.
Reducing fluctuations in non-core areas of activity.
• Protecting and developing the organization’s assets and reputation.
• Develop and support human resources and the organization’s information base.
• Maximize operating efficiency.
Steps in the risk management process:
• Planning the risk management process and mapping the scope of work and the basis and standards that will be relied upon as well
Defining a framework for the process and an agenda for analysis.
• Identify and identify risks.
• Risk analysis .
• Description of risks.
• Risk assessment.
• risk assessment.
• Preparing risk reports and communications.
• Addressing risks.
• Monitor and review risk management processes
Steps for qualitative risk assessment:
Determine the work task:
• The first step
- Hazard identification
- This step is the most important in determining risks (natural, chemical, biological, ergonomic, etc.)
- Physiological (use the attached checklists
• The second step
- Identify potential consequences
The likely outcome of accidents is that they may cause the following:
- Disruption in production processes
- People getting injured
- Losses in machinery and equipment
- Falling under the responsibility of the law
• The third step
What are the possibilities that, if they existed, would lead to an accident or this defect?
There will be several possibilities for each risk, such as personal error, mechanical failure, unusual circumstances, etc. and use
- Matrix table to determine the level of risk.
• Fourth step
- Apply risk control measures
- Which is summarized in (ERICPD)
- Remove Eliminate
- Reduce
- Isolate
- Control control
- Personal protective equipment (PPE).
- Discipline i Discipline
• Fifth step
- Re-appraising the Residual Risk
- Has the risk been reduced to an acceptable level? ALA RP
- Can other means be added to reduce the probability of the risk occurring or its consequences if they occur?
- Who is responsible for making these changes?
- It must be known that detecting dangers is the work of every individual in the facility and is not limited to specific individuals
- Controlling dangers must be done through two methods, the first is local control and the other is administrative control management control.
Example:
- Process: Inhaling iron rust dust in the air in the oven area
- Evaluation: Pulmonary ossification
- Local control: done by
1 - Good ventilation above the oven and dust removal
2- Use personal protective equipment (air filter)
Types of danger:
- Risks associated with machinery and equipment.
- Risks associated with materials and raw materials.
- Risks associated with the workplace.
- Risks associated with work methods.
- Risks associated with the work environment.
- Risks resulting from the structure of the work.
- The risk may affect individuals or affect the environment.
- Danger exposes individuals.
- It affects the health of workers.
- Injuries happen.
- Lives lost.
- Hazard affecting the environment.
- Risk of contamination.
Types of danger can be divided into:
Natural hazards:
• Falling from heights. Collision with falling objects
• Skating. Stumbling
• Things falling. Failures in the scaffold
• Defects in a machine or tool. the noise
• Manual transfer. Storage and p
• Transport . Radiations
• Cleanliness and arrangement. Lighting
• Temperature
Electrical hazards:
- Shock
- Burn
- Mechanical burns
Chemical risks:
- Gases
- Fumes
- Smoking
- Biological risks:
- Bacteria
- Viruses
- Standard infection control procedures
Preventing the spread of infection between patients in internal wards and each other and following safe methods to prevent its spread.
Definition of infection:
It is the entry of the disease-causing agent into the human body, its multiplication, and the occurrence of signs and symptoms of the disease.
Hospital infections:
It is an infection that a person acquires while receiving health care in a hospital, and its symptoms appear after 48 hours or
More than the patient being admitted to the hospital.
The causative agent of the disease:
1) Viruses such as (all kinds of influenza, HCV, HBV, AIDS, etc.)
2) Bacteria such as (meningitis, tuberculosis)
3) Fungals (Tinia, Monilia)
4) (parasites such as (schistosomiasis, ascaris, amoeba)
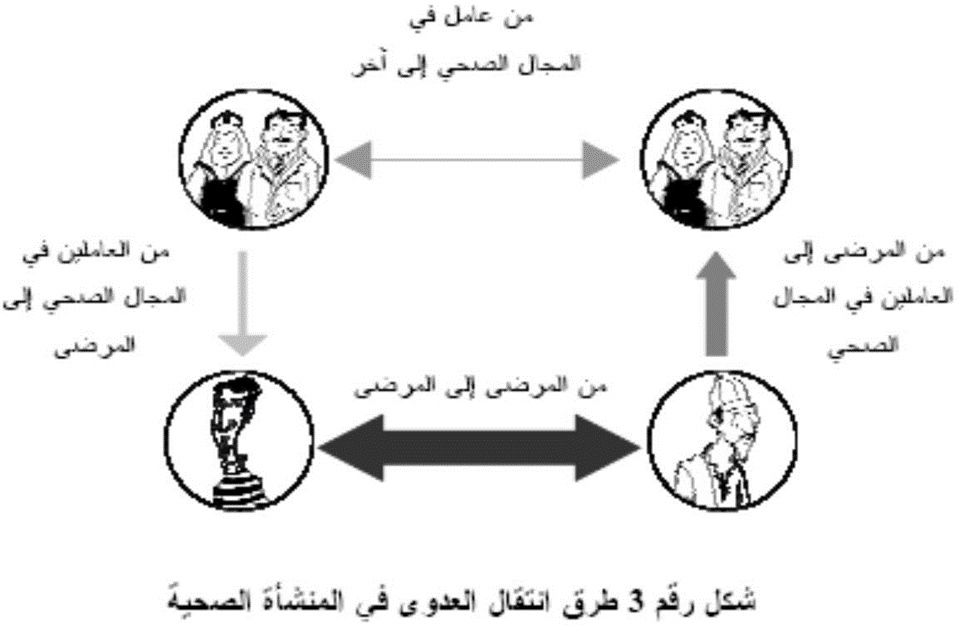
Methods of transmission of infection within the health facility:
Standard infection control precautions include the following:
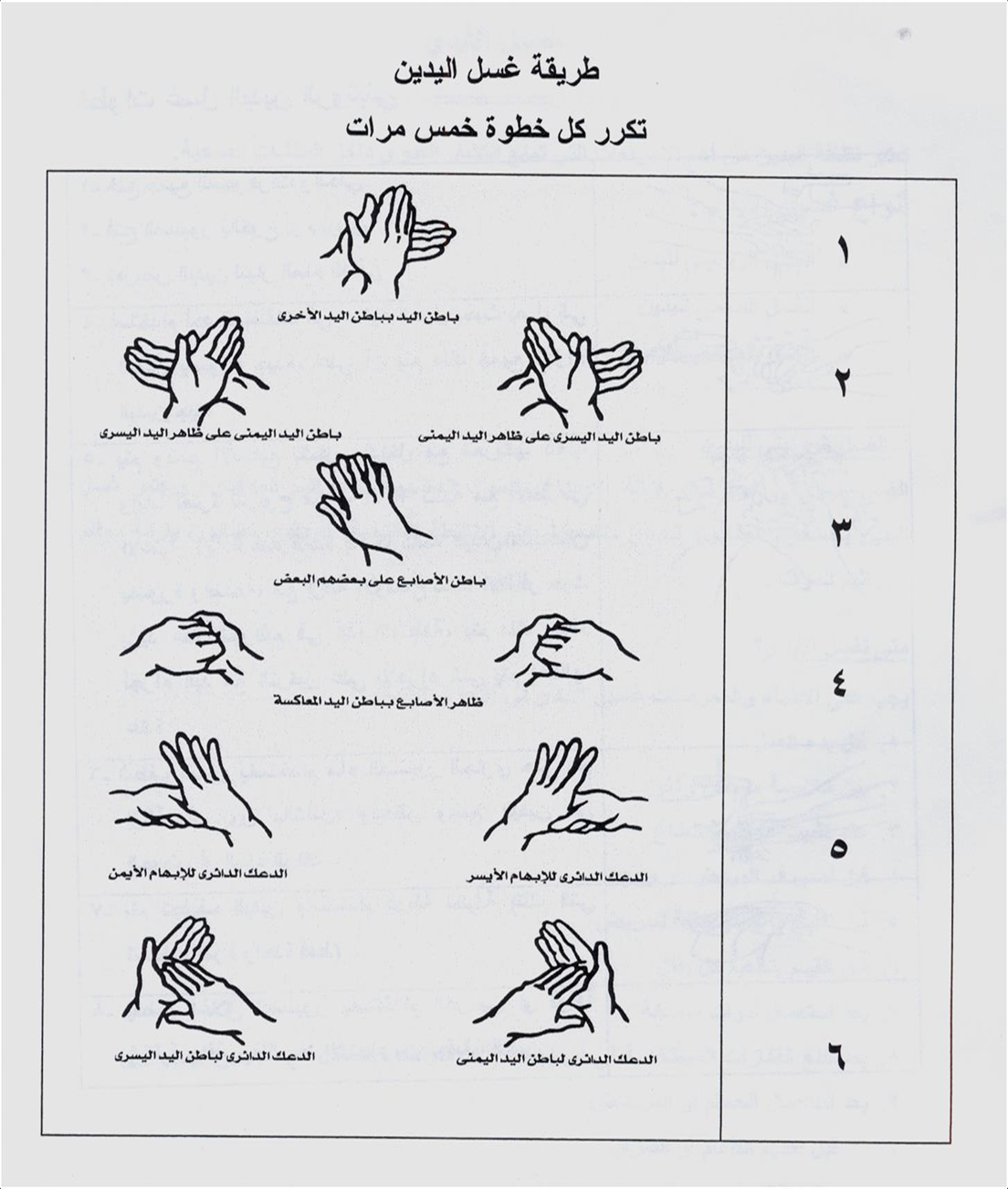
1- Hand hygiene and disinfection:
Hand hygiene is considered one of the most important measures that prevent the spread of infection within health facilities.
- The five moments (positions) for washing hands:
|
|
|
|
|
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|||
|
|
|
|
|
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
60 – 40 )WHO2009( |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
30-20 WHO2009 |
|
|
|
|
|
|
90-60 WHO2009 |
|
|
|
|
Hand cleaning methods:
Hand washing method:
2- Personal protective tools:
Gloves:
There are three main types of gloves used in health care facilities, the use of each of which varies according to the type
The task assigned to the health service provider.
A- Sterile gloves: They are used in penetrative interventions and are characterized by being sterile and can only be used once.
Its uses:
• Before surgical operations
• Before medical interventions that require a sterile method to be completed, such as: (installation of a central venous catheter, all operations
Puncture, when dealing with large burns, preparing and mixing solutions and chemotherapy drugs for oncology patients
B- Non-sterile rubber gloves: This type of glove is characterized as non-sterile (clean) and is used only once.
Its uses:
• When giving intravenous solutions, installing a peripheral intravenous catheter, and before intravenous injection (except for patients
immunocompromised (
• When changing bandages, and when dealing with cleaning any of the devices or other equipment contaminated with blood, urine, or
Stool or any other secretions.
• When dealing with samples of patient tissues or fluids or vessels containing them
• When performing respiratory suction or when dealing with mucous membranes, such as examination or care.
With the mouth.
• Cleaning and disinfecting traces of blood or body fluids.
C- Heavy-duty gloves: These gloves are used when dealing with waste or contaminated tools and when carrying out work
Cleaning, especially in the case of sharp residues. It can be used repeatedly after cleaning and disinfecting it appropriately once
Been punctured or torn.
Its uses:
• Dealing with medical waste (waste bags and safety boxes)
• Use of detergents, disinfectants and chemicals.
• Cleaning and disinfecting the environment.
• Cleaning machines
• Dealing with blood spills in the presence of sharp waste.
Abayas:
1) Unclean, non-sterile gowns:
It is worn while performing some medical procedures that could lead to the dispersion of spray, blood, and body fluids, or during
Procedures that lead to contamination of workers’ clothes or uniforms with microbes or infectious materials.
2) Sterile gowns:
Sterile gowns must be worn during all surgical operations and some important medical interventions (such as implantation).
Central venous catheterization, mixing solutions for immunocompromised patients and newborn children (preferably
It is made of materials impermeable to liquids.
- The abaya (whether clean or sterile) must be used once and then disposed of in the hazardous waste bin.
If it is single-use or in the laundry basket if it is frequently used.
- It is prohibited to use the same gown to care for more than one patient.
Medical gowns, like all personal protective equipment, are used for one provider to care for one patient and for one procedure
One.
Plastic bibs:
Single-use aprons are worn when performing some medical procedures that could lead to the dispersion of spray and blood.
And bodily fluids or while performing some procedures that lead to contamination of clothes or uniforms of workers with microbes
Or infectious materials.
Headwear:
It is recommended to wear single-use head coverings, which contain the hair to prevent hair loss or spreading
Microbes.
Examples of uses:
• Surgical procedures in the operating room.
• Mixing intravenous solutions.
• Sterilization department (packaging area)
• Kitchen (during cooking/preparing meals)
The traditional head covering (scarf or hijab) is not a substitute for the head covering intended for patient care.
Providing protection for the face (eyes, nose and mouth):
The health care provider should be careful to wear a face mask (face shield) or eye protection (goggles).
And the surgical mask together when the possibility of his face being exposed to blood spray or body fluids flying from the patient increases.
Respiratory masks:
1) Surgical mask: A mask that tightly covers the nose and mouth should be used when exposed to respiratory secretions.
of the patient or splashes of blood and other body fluids as part of standard precautions.
Indications :
• surgeries.
• Some invasive medical interventions (such as installation of a central venous catheter, spinal fluid aspiration, injections into
spinal fluid )
• With immunocompromised patients.
• When there is a possibility of exposure to any contaminated spray (such as exposure to surgical instrument washing spray or suctioning device secretions).
respiratory
In addition, patients and workers infected with droplet-borne diseases wear respiratory masks to prevent
Infection.
2) High-efficiency respiratory mask: used when exposed to airborne diseases
Indications for use:
• Preventing some diseases such as: (active tuberculosis, measles, chicken pox, infectious diseases)
The emerging coronavirus (SARS/Coronavirus/....) due to its seriousness.
Foot protectors:
Sabo: A protector that covers the foot, provided that it is not permeable to fluids.
Boot: A protective shoe that covers the foot and leg.
Indications for use:
• In operating rooms
• When cleaning surgical instruments
• Cleaning and disinfecting the environment
• Cooking, collecting and transporting waste.
Respiratory health precautions and cough etiquette.
1. Identifying the patient who may have a respiratory infection:
Health facility workers must pay attention to the need to quickly detect patients with an existing respiratory infection
Their arrival to the health facility.
Provide instructional panels explaining respiratory health precautions and cough etiquette, which include:
- Cover the mouth and nose when sneezing and coughing.
Use paper tissues only once and dispose of them in the trash.
Wash hands after contact with respiratory secretions.
The patient must provide information about his medical condition when logging in.
2. Providing the following supplies and supplies at the reception point and outpatient clinics: surgical masks, paper tissues, and a basket.
Trash, equipment and supplies for washing and disinfecting hands.
3. Apply the respiratory health precautions and cough etiquette mentioned above to all patients who show symptoms
Respiratory infection, including facility workers.
4. Isolating patients likely to have a respiratory infection from the rest of the patients.
5. Establish rules for visiting these patients, including:
Postpone the visit as much as possible if there is no urgent need.
Prevent visitors with symptoms of respiratory infection from entering the patient care area.
6. Responsibilities of health service providers:
- Monitor the application of respiratory health precautions in addition to precautions when dealing with patients who suffer from
Respiratory infection, and when there is suspicion that it may be an airborne infection, isolation precautions are applied
Airborne diseases.
- Prevent workers with respiratory infections from direct contact with patients. When necessary, they are obligated
By wearing a respiratory mask and washing hands frequently.
- Ensure the implementation of the policy of vaccinating health facility workers with the necessary vaccines, including influenza vaccination
Seasonal annually.
7. Communicate with the relevant departments in the Ministry to learn about the latest developments regarding influenza and systemic infections
Respiratory infection, and monitoring and follow-up activities are intensified to quickly discover new cases.
8. In the event of increasing rates of respiratory infections and a high rate of influx of cases into the facility, an allocation is made
A triage and classification area to isolate potentially infected patients from the rest of the patients and direct them to designated care areas
for them .
3- Safe injection:
A safe injection is one that does not cause harm to the recipient, nor does it expose the service provider to any risks that can be avoided.
It does not produce any waste that may harm others or the environment.
Examples of infections reported to occur through injections:
|
|
|
|
|
|
, |
|
The basic components of the injection:
1. Use sterile injection tools
2. Preventing contamination of injection tools and fluids.
3. Protecting the health service provider from acupuncture or sharp tools.
4. Protecting the environment and society by preventing access to waste from the injection process.
5. Some practical methods to be followed:
- Hand hygiene
- Use gloves
- Follow the necessary precautions when using multi-dose medication containers.
- Preparing the skin before injection: The skin must be cleaned before injection and then disinfected with a suitable antiseptic such as alcohol.
- Follow the closed system for intravenous injection.
- Follow the non-touch method: If any part of the syringe is touched, it is considered contaminated.
4 - Precautions for storing, preparing and handling medications:
The safe storage, preparation and handling of medical treatment that is injected, whether intravenously or otherwise, is considered one of the most important components.
Anti-contamination methods to reduce infection rates within health facilities.
Obligatory requirements:
1. Medications should not be prepared in syringes in advance and stored until treatment is carried out.
2. The new syringe should not be opened except for actual use.
3. One syringe should not be used for more than one patient, even if the tooth is changed.
4. The syringe must not be reused when withdrawing any treatment or solution from its designated container.
One syringe tooth - one syringe body - one procedure
5. It is prohibited to use solutions prepared for intravenous drip to dissolve medications (single ampoules of sterile water must be used
the use (
6. The rubber cover of treatment containers must be disinfected with a suitable disinfectant such as alcohol and left to dry before inserting the syringe tip.
7. Multi-dose containers should be allocated to one patient whenever possible, and if necessary, this should be done in one place
Designed for treatment preparation.
8. When mixing and compounding solutions and treatments, it is preferable to do so in the clinical pharmacy, in a central location in the medical facility.
If they are not available, a separate room must be prepared for mixing and installing solutions and treatments.
5 - Reprocessing medical machines and tools:
A. Cleaning: is the removal of suspended materials (such as organic and inorganic materials) present on the surface of the tools that should be
Reprocessed. It can be done either manually or automatically using washing machines, usually using running water and detergents.
B. Disinfection: Disinfection is done in one of two ways: either using heat or using chemicals. An operation must be performed
Careful cleaning before the disinfection process, as organic materials (such as blood and body fluids) hinder the efficiency of disinfection in the elimination
On microbes.
C. Sterilization: Eliminate all forms of microbial life, including bacterial sacs. Sterilization methods can be divided
Basically for the following:
First: thermal sterilization:
Wet heat sterilization: using steam under pressure from an autoclave.
Dry heat sterilization: Sterilization using dry heat using dry heat in an electric sterilization oven.
Second: Sterilization under low temperatures
Third: Other means of sterilization: such as sterilization with gamma rays and sterilization by filtration.
6 - Cleaning and disinfecting the environment:
Environmental cleanliness is the process of removing organic materials, dust, and dirt, which leads to the elimination of a large percentage of
Microbes.
Common cleaning methods:
1. Dry cleaning method (sweeping): Dry brooms, dry cloths, and dusters should not be used in places
Treating patients as it leads to the spread of bacteria-carrying particles.
2. Wet cleaning method: Wet cleaning is done using a damp cloth to clean surfaces with an additive
Detergents or disinfectants
7- Textile reprocessing:
Basic principles of infection control when dealing with sheets, covers and furnishings:
- Individuals who collect, transport, sort and wash sheets and blankets should receive the necessary training.
They should also wear the necessary protective clothing, in addition to facilitating their access to hand-washing areas.
Dirty sheets and blankets should be removed very carefully and quietly, while reducing the movements necessary for this as much as possible.
So that this does not cause the spread of microbes in the air.
- All used sheets and covers are considered contaminated and there is no need to distinguish the colors of collection bags.
- Moving dirty sheets and blankets. Bags containing dirty sheets and blankets are not allowed to be transported via
Carrying it by hand, it is preferable to use carts or containers with a lid.
- You should avoid touching dirty or contaminated sheets and covers.
8 - Health care waste management:
First: Ordinary (semi-domestic) waste: These wastes are similar in composition to household waste.
Second: Health care waste: It can be divided into two types:
1. Non-hazardous waste: examples include packaging papers for medical equipment and supplies.
2. Hazardous waste: includes: infectious waste, autopsy and surgical waste, sharp instrument waste, waste
Chemicals, pharmaceutical waste, radioactive materials, heavy metals, etc.
Definition of procedure:
• Obligating workers in internal departments to use safe methods to prevent hospital infections.
procedures :
First: Special procedures for the health service provider:
Medical service providers (doctors and nurses) do the following:
1. Wash hands hygienically before dealing with the patient.
2. Change gloves between one patient and another and between one procedure and another.
3. Wash hands hygienically when performing the following procedures: -
4. Before installing a peripheral cannula and urinary catheter.
5. Before giving non-oral solutions and medications
6. Wear a plastic apron when exposed to the patient's blood, fluids, and secretions
7. Change personal condoms if they are contaminated at any time, even if for the same patient.
8. Washing hands between one procedure and another, even if it is for the same patient.
9. Disposing of urine and feces in the patients’ bathroom and throwing in water and chlorine afterward.
Second: When preparing intravenous solutions:
1. The nurse prepares all tools before starting work (sterile gloves, dressing gown, and belts for mixing solutions).
2. The department supervisor allocates a clean place for preparing medications and solutions in the unit and is not used for any other purpose
3. The department supervisor assigns a nurse responsible for mixing solutions in case there is a need to mix solutions to prevent
The spread of hospital infections, and alternatives are also allocated in the event that the responsible nurse is not available.
4. The nurse washes hands hygienically before starting work on mixing solutions, and uses a new sterile syringe.
With each type of solution. (Every time you use a new sterile syringe.)
Third: When giving medications by injection:
1. The nurse washes hands hygienically, wears gloves, and disinfects the site of intervention with alcohol.
2. The nurse uses the ampoule with distilled water only, not salt solution, and the remainder is disposed of immediately
Fourth: Special procedures for patient care:
1. Every nurse responsible for a patient takes care of the patient’s general hygiene.
2. Doctors and nurses should avoid touching wounds with their hands, and non-contaminated methods should be followed when caring for wounds.
Use a sterile dressing bottle every time you change the patient's wound.
3. The doctor and nurse use sterile spare gloves on the wound and use the non-touch method
4. The doctor cleans the wound using a surgical mask and a piece of cotton or gauze moistened with an antiseptic solution, such as
Surgical alcohol or betadine. It is not allowed to touch the wound with the hands.
5. The doctor isolates patients with infectious diseases in an isolation room in a unit in the internal department.
6. The department supervisor and the responsible nurse follow isolation precautions with isolation patients as per policy
For insulation.
Fifth: Special procedures for employees within departments:
1. The infection control team vaccinates all employees in the unit against hepatitis B.
2. The occupational safety and health officer ensures that all employees in the department are free of infectious diseases.
3. All medical service providers wash hands before and after dealing with the patient.
4. All medical service providers wash hands between one procedure and another, even if it is for the same patient.
5. All medical service providers wear protective clothing while dealing with the patient.
6. All medical service providers are committed to not smoking, eating or drinking inside the burn unit.
Sixth: Special procedures for visitors:
1. The visiting officer limits the number of visitors to only two per patient, and then they do so in succession, as permitted
The patient's condition .
2. The doctor evaluates each patient individually and determines the duration of the visit so that it does not affect the patient’s general condition
3. The security officer warns visitors not to smoke, eat, or drink inside the department.
4. The nurse warns visitors not to touch any of the tools or devices around the patient.
Seventh: Department environment:
1. Sufficient space must be left around each patient's bed for the medical equipment used and for the service provider to pass through
Health care is easy to reduce the risk of transmitting infection between individuals.
2. There must be a safety box next to each bed to dispose of sharp waste.
3. There must be a physical separation between the patient and the other that is easy to clean weekly or when it becomes contaminated at any time or between
The patient leaves and before another patient enters.
Eighth: Cleanliness of the department environment:
1. The worker wet-cleans the unit and surfaces daily from top to bottom and at the beginning of each shift
Getting dirty at any time with soap and water, then with chlorine 1000 parts per million. Ask about dilution. Control unit.
The infection must be reduced according to the concentration of chlorine present in the institute.
2. The worker cleans the unit, surfaces, and all work areas (inventory) at least once every week or two
It starts from top to bottom in the previous manner.
3. The worker cleans the patient's area and changes the bedding daily between the patient and the other if they become dirty.
4. The worker removes a large blood spill immediately by first placing a single-use cloth on the area
Spillage, then concentrated chlorine is placed as it is from the bottle, then it is lifted from the ground, then cleaned a second time with a cloth with a soft cloth.
Single use in the same way if there are traces of it, then clean with soap and water and then dry.
5. The worker removes the small bloody spill immediately. First: Wipe the spill with a reusable cloth
One moistened with 5000 parts per million chlorine. The Infection Control Unit asks about dilution so that the dilution is done accordingly
The concentration of chlorine present in the institute, then the piece of cloth is disposed of in the red basket, and this process is repeated in its case
If there is a trace, then the place is cleaned with soap and water, then dried well.
6. All health service providers are committed to separating waste so that contaminated waste is disposed of in the red bin
Regular waste is in the black bin, and sharp waste is in the safety box.