Third part
- A - General work procedures
· Infection control procedures in the burns unit
· Basic cardiopulmonary resuscitation
. Advanced cardiopulmonary resuscitation in hospital
· Nursing evaluation
· Measuring vital signs
· Temperature measurement
· Pulse measurement
· Spirometry
· Blood pressure measurement
· Spare parts for wounds
· Installation of a peripheral intravenous catheter
· Perform an enema
· Installation of a urinary catheter
· Drawing blood samples
· Do a sugar analysis
· Method of giving treatment
· Transfusion
· Oxygen therapy
Infection control within the burn unit
Burn patients are among the patients in hospitals most exposed to microbial colonization and most susceptible to infection, so infection control methods must be adhered to when dealing with burn patients.
Types of burns:
Burns resulting from direct exposure to fire, hot liquids, or hot surfaces, or from direct exposure to chemicals, electrical current, and radiation
Sources of infection and types of microbes that cause them
Ò Either internal sources (from the patient himself), or external sources from the environment, surfaces, devices, supplies, and service providers
Ò Microbes from external sources are more resistant to antibiotics
Ò Microbial from internal microbes.
If the burn is delayed, antibiotic-resistant microbes are added
Strategies to reduce the risk of infection in a burn unit
1. Hand hygiene:
Hands are considered the most common means of transmitting infection, so visitors and workers must adhere to hand hygiene
2- Wearing personal protection:
Gloves must be worn as used when dealing with patients, changed and hands cleaned after finishing
You should also wear a plastic apron when handling bodily fluids
3- Precautions for providing intravenous treatment
Hands must be washed, a head covering, face mask, medical gown, and gloves must be worn, sterile brushes must be provided, and a sterile atmosphere must be provided.
Possibility of infection
Ò The infection rate decreases if the burn does not exceed 30% of the body area
Outbreak of infection within the burn unit
1- Dealing with burns
A. Periodic evaluation of the burn
B. Commitment to following pollution-preventing methods
C. If there is dead tissue, it is removed
D. A room is allocated for the nurse if the burn rate exceeds 30%
2 - Patient equipment and environmental monitoring:
A. Diagnostic tools must be customized for each patient
B. Give the patient a water bath on a flat surface
C. Preventing the presence of plants and children’s toys
Care of patients connected to a ventilator:
A. Raise the bed at an angle of 30-45 degrees
B. Do not overuse antiacid drugs
C. Quickly start physical therapy and breathing exercises
D. The oxygen humidifier should be changed every 24 hours
Place where the medicine is prepared
Patients should be separated from rooms
Ventilation: The outlets remain closed and ventilation is centralized
Customize tubs and containers for rubbing alcohol
It must be located near the entrance to the unit
Ò Location of the unit:
The unit must be located near operations or the emergency entrance
Ò Antibiotics:
Topical antibiotics are used
Ò Health service providers:
Service providers must be vaccinated with the necessary vaccinations
Ò Cleanliness of the unit:
Cleaning and disinfection must be done according to the periodic schedule and after patients leave
Ò Isolating patients:
Patients with suspected or proven infection should be isolated
Ò Visit:
Visitation in the unit should be limited
Ò Patient care equipment:
Washing, cleaning and sterilizing the machines should not be done in the unit, but rather they should be transported for sterilization
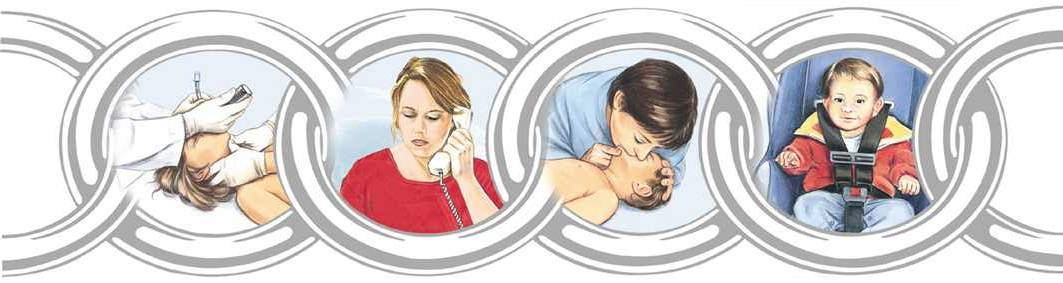
Basic CPR
Basic CPR
An injured adult on the street
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who does not breathe, does not speak, and does not respond, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total obstruction of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Steps:
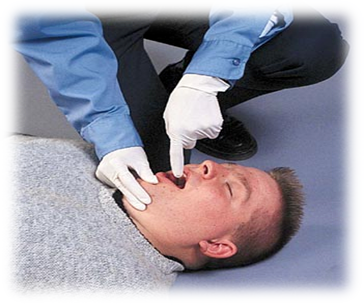
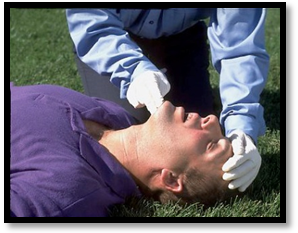
1. An initial assessment of the environment surrounding the injured person and ensuring that it is free of any dangerous factors (electricity, fire, drowning, etc.).
2. In the first 10 seconds from the beginning of seeing the injured person, the injured person is placed lying on his back, his degree of consciousness is assessed, and he is called in a loud voice with a shrug of the shoulders, “Are you okay??” '.
· No response or abnormal breathing.

1. Call for emergency medical assistance by calling the local number.
2. Make sure there is a clear pulse (no less than 5 seconds and no more than 10 seconds).
· Pulse in the carotid artery (on both sides of the larynx for ease of identifying the presence of a pulse since it is the largest artery in the body) from the side opposite the paramedic.
3. When there is no confirmed pulse within 10 seconds, perform cardiopulmonary resuscitation as follows:
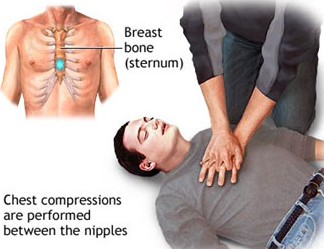
· Never expose the injured person’s chest.
· Place the palm of one hand (the whole hand) vertically in the middle of the sternum between the nipples.
· Start doing chest compressions at a rate of 30 compressions in a period not exceeding 18 seconds, or less if there are one or two paramedics.
To perform cardiopulmonary resuscitation in a correct and effective manner, the following must be taken into account:
· Place the injured person on a hard surface.
· Begin compressions on the casualty’s chest within 10 seconds.
· Press hard, quickly, and to a depth of 5 cm in adults over 18 years of age
· Allow the rib cage to take its natural space after each compression
· Reduce external influences (as long as they are less than 10 seconds)
· Give the injured person an effective breath (by opening the airway by tilting the head back, pulling the chin forward, and opening the airway - but in the case of injuries to the cervical vertebrae, stabilize the injured person’s head)
· Give 2 breaths if there is one or two paramedics present to the seriously injured person, within a period not exceeding three seconds.
· Five consecutive cycles of compressions and breathing are performed (for a period of two minutes), with re-evaluation of breathing and pulse.

|
Note: When following these steps, take into account infection control policies for administering treatment. |
Basic CPR
For an injured child on the street
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who is not breathing, speaking, or responding, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total blockage of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Action Steps :
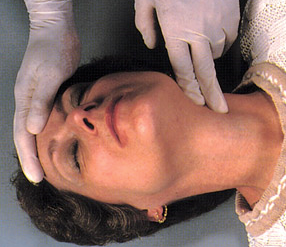
· An initial assessment of the environment surrounding the injured person and ensuring that it is free of any dangerous factors (electricity, fire, drowning, etc.)
· In the first 1k0 seconds from the beginning of seeing the injured person, the injured person is placed lying on his back, his degree of consciousness is assessed, and he is called out in a loud voice while shaking his legs, “Are you okay??” '.
· No response or abnormal breathing.
· Ask for emergency medical assistance by calling the local number.
· Make sure there is a clear pulse (no less than 5 seconds and no more than 10 seconds).
· The pulse in the brachial artery (the inner side of the arm for easy identification of the presence of a pulse, given that it is the largest artery in the body on the side opposite the paramedic.
5. When it is confirmed that there is no confirmed pulse within 10 seconds, perform cardiopulmonary resuscitation as follows:
· Never expose the injured person’s chest.
Place the index and middle fingers of the hand vertically in the middle of the sternum between the nipples if there is a single paramedic and the thumbs of both hands if there are two paramedics.
· Start doing chest compressions at a rate of 30 compressions in a period not exceeding 18 seconds, or less if there is one paramedic, and if there are two paramedics, give 15 compressions.
To perform cardiopulmonary resuscitation in a correct and effective manner, the following must be taken into account:
· Place the injured person on a hard surface.
· Begin compressions on the injured person’s chest within 10 seconds.
· Press hard, quickly, and to a depth of 4 cm in children from one to eight years of age.
· Make the rib cage take the natural space after each compression
· Reduce external influences (as long as they are less than 10 seconds).
· Give the injured person an effective breath (by opening the airway by tilting the head back and pulling the chin forward and opening the airway - or in the case of injuries to the cervical vertebrae, immobilize the injured person’s head).
· Give 2 breaths if there is one or two paramedics present.
6. Five successive cycles of compressions and breathing are performed (for a period of two minutes), with re-evaluation of breathing and pulse.



Note: When following these steps, take into account the infection control policies for administering the treatment
Advanced cardiopulmonary resuscitation in hospital
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who does not breathe, does not speak, and does not respond, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total obstruction of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Action Steps :
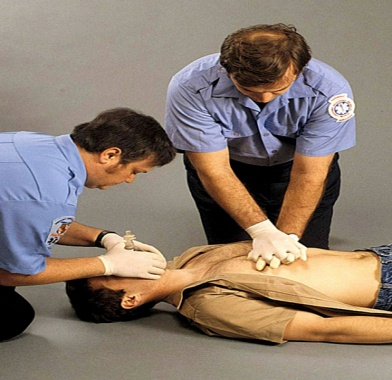
· Ensure that the surrounding environment is safe for the workers and the patient (in a period not exceeding 10 seconds).
· Adjusting the patient’s position.
· Ensure the level of consciousness of the injured person (by gently shaking the shoulders and speaking to the patient in a loud voice, “Are you okay?” for a period not exceeding 10 seconds).
· If the patient answers, this indicates that the heart and lungs are working well, and in this case it is evaluated whether the patient needs other assistance or not.
1. If the patient does not answer, we begin by taking the following steps:
· Opening the patient’s airway:
· Opening the airway by installing a laryngeal tube - which is the best way to open the airway, but it is only installed in the hospital due to the lack of capabilities and human resources trained for this in the street.
· Assess the patient’s breathing:
· By looking at the patient’s chest (there is movement in the patient’s chest up and down), the duration of the breathing assessment is 10 seconds.
Evaluate the presence of a pulse or not:
· By checking the pulse with the carotid artery for no more than 10 seconds and no less than 5 seconds from the direction opposite the paramedic.
In the absence of breathing and pulse:
· Press on the sternum above the xiphoid process, 2 finger distances, in the middle of the line between the nipples.
· Interlock your fingers and press them together.
· The hands should be straight and perpendicular to the chest, the back should be straight, and the force of the pressure should come from the muscles of the pelvis and legs.
· Giving the patient breathing through a throat tube or using a tube mask (mouth-to-mouth breathing is not given).
· The ratio of chest compressions to the rate of breathing for the patient varies depending on whether a throat tube is present or not:
· In case of a throat tube:
· Perform 30 chest compressions for 2 breaths, whether by one paramedic or two paramedics.
In the absence of a throat tube:
· Perform 100 chest compressions per minute and at the same time give 8-10 breaths per minute.
· Perform five cycles of chest compressions and breathing, then re-evaluate breathing and pulse.
· If the heart returns to work, chest compressions are stopped and the patient is placed on a ventilator according to his condition.

· The hands should be straight and perpendicular to the chest, the back should be straight, and the force of the pressure should come from the muscles of the pelvis and legs.
· Giving the patient breathing through a throat tube or using a tube mask (mouth-to-mouth breathing is not given).
The ratio of chest compressions to the rate of breathing for the patient varies depending on the presence of a throat tube or not:
· In the case of a throat tube:
· Perform 30 chest compressions for 2 breaths, whether by one paramedic or two paramedics.
In the absence of a throat tube:
· Perform 100 chest compressions per minute and at the same time give 8-10 breaths per minute.
· Perform five cycles of chest compressions and breathing, then re-evaluate breathing and pulse.
· If the heart returns to work, chest compressions are stopped and the patient is placed on a ventilator according to his condition.
Choking (respiratory obstruction)
Definition of a lump:
Bloating occurs when a solid or liquid object or the back of the tongue blocks the airway, and the victim may quickly stop breathing and lose consciousness. The blockage may be partial or complete, such as (false teeth, food debris, coins, etc.). This may affect the patient's breathing and may lead to loss of consciousness. If immediate intervention is performed, the blockage may be partial or complete.
The Reasons:-
◾ Trying to swallow large pieces of food without chewing them well.
◾ May result from muscle spasm.
◾ Use a denture. Artificial teeth make it difficult to feel the size of the bite while chewing and swallowing.
◾ Speaking emotionally or laughing while eating.
◾ Walking, playing, or running with objects in the mouth.
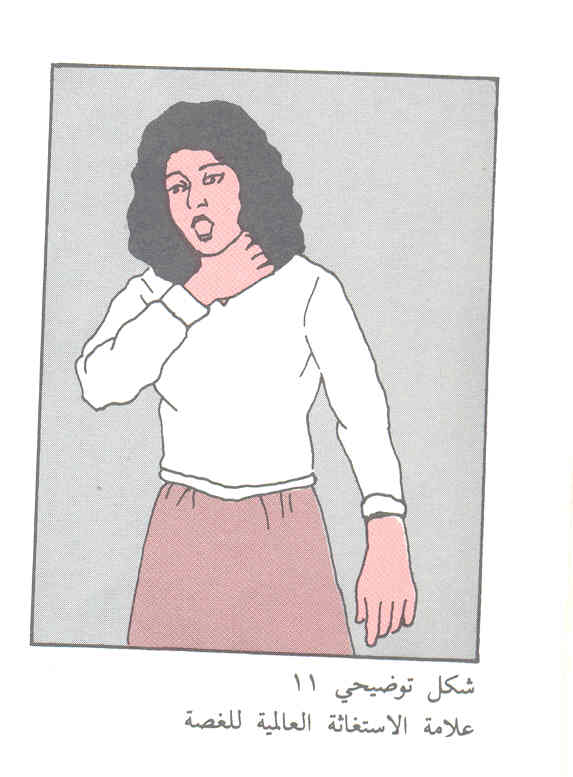
Tags:-
Partial airway obstruction:
◾ When the patient suffers from partial airway obstruction, he coughs forcefully in an attempt to dislodge the object blocking the airway, and he may be able to speak.
◾ Whistling may be heard when breathing.
◾ The injured person may hold his throat with one or both hands.
If the patient is conscious:
◾ Ask the patient to cough as this helps expel the foreign body.
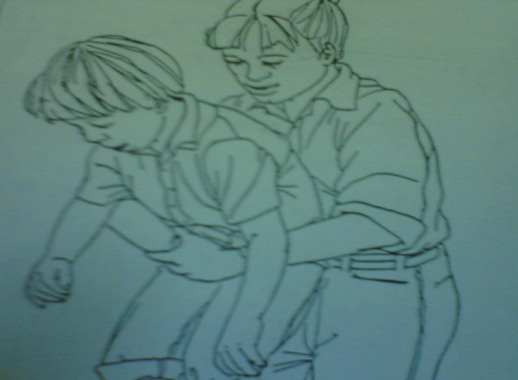
◾ If the patient cannot respond, the Hemlich-Hetti method is used
◾ The foreign body is expelled from the airway through...
◾ Stand behind the patient and wrap the arms around his waist.
◾ Place the thumb side of your fist in front of the injured person’s abdomen, just above the navel
◾ And clench your fist with the other hand.
Press inward and up the abdomen with quick pushes and repeat these pushes

1. In the case of pregnant women or an obese person, do not use the Hemlich method, but place the hands in the middle of the sternum so that the thrusts do not lose their strength.

2. If the patient is a child from the age of puberty, we use abdominal pressures while holding the child on the foot for five pressures.
3. If the patient is a child from one month to one year, the nurse uses five back compressions or five chest thrusts, but using the palm of the hand.

An unconscious patient
1. Place the patient on his back so that you can open the airway.
2. Bend the patient’s head backwards with a slight tilt to one side to facilitate the foreign body’s exit.
3. The finger is inserted to wipe the patient’s mouth from the inside using a hook method.
4. If the foreign body does not come out, the patient is given one count of exhalation and the chest is observed to rise
5. Follow Hemlich’s steps until the foreign body is out of the airway:
6. Sit on the knees so that they surround the patient’s thighs.
7. Place the palm of one hand above the stomach area.
8. You place the other hand on the first hand and press on the abdomen with five quick successive pushes to increase internal pressure to help push the foreign body out.
9. The steps are repeated until the patient expels the foreign body.
10. The pulse is checked. If there is no pulse, cardiopulmonary resuscitation procedures begin.
11. If the injured person loses consciousness, lower him to the ground, supporting his head and neck
12. Clean the mouth with your finger in the shape of a hook
13. If there is no response, apply pressure on the abdomen.