Third part
| Site: | EHC | Egyptian Health Council |
| Course: | Procedural work guide for the burns unit |
| Book: | Third part |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 5:10 PM |
- A - General work procedures
· Infection control procedures in the burns unit
· Basic cardiopulmonary resuscitation
. Advanced cardiopulmonary resuscitation in hospital
· Nursing evaluation
· Measuring vital signs
· Temperature measurement
· Pulse measurement
· Spirometry
· Blood pressure measurement
· Spare parts for wounds
· Installation of a peripheral intravenous catheter
· Perform an enema
· Installation of a urinary catheter
· Drawing blood samples
· Do a sugar analysis
· Method of giving treatment
· Transfusion
· Oxygen therapy
Infection control within the burn unit
Burn patients are among the patients in hospitals most exposed to microbial colonization and most susceptible to infection, so infection control methods must be adhered to when dealing with burn patients.
Types of burns:
Burns resulting from direct exposure to fire, hot liquids, or hot surfaces, or from direct exposure to chemicals, electrical current, and radiation
Sources of infection and types of microbes that cause them
Ò Either internal sources (from the patient himself), or external sources from the environment, surfaces, devices, supplies, and service providers
Ò Microbes from external sources are more resistant to antibiotics
Ò Microbial from internal microbes.
If the burn is delayed, antibiotic-resistant microbes are added
Strategies to reduce the risk of infection in a burn unit
1. Hand hygiene:
Hands are considered the most common means of transmitting infection, so visitors and workers must adhere to hand hygiene
2- Wearing personal protection:
Gloves must be worn as used when dealing with patients, changed and hands cleaned after finishing
You should also wear a plastic apron when handling bodily fluids
3- Precautions for providing intravenous treatment
Hands must be washed, a head covering, face mask, medical gown, and gloves must be worn, sterile brushes must be provided, and a sterile atmosphere must be provided.
Possibility of infection
Ò The infection rate decreases if the burn does not exceed 30% of the body area
Outbreak of infection within the burn unit
1- Dealing with burns
A. Periodic evaluation of the burn
B. Commitment to following pollution-preventing methods
C. If there is dead tissue, it is removed
D. A room is allocated for the nurse if the burn rate exceeds 30%
2 - Patient equipment and environmental monitoring:
A. Diagnostic tools must be customized for each patient
B. Give the patient a water bath on a flat surface
C. Preventing the presence of plants and children’s toys
Care of patients connected to a ventilator:
A. Raise the bed at an angle of 30-45 degrees
B. Do not overuse antiacid drugs
C. Quickly start physical therapy and breathing exercises
D. The oxygen humidifier should be changed every 24 hours
Place where the medicine is prepared
Patients should be separated from rooms
Ventilation: The outlets remain closed and ventilation is centralized
Customize tubs and containers for rubbing alcohol
It must be located near the entrance to the unit
Ò Location of the unit:
The unit must be located near operations or the emergency entrance
Ò Antibiotics:
Topical antibiotics are used
Ò Health service providers:
Service providers must be vaccinated with the necessary vaccinations
Ò Cleanliness of the unit:
Cleaning and disinfection must be done according to the periodic schedule and after patients leave
Ò Isolating patients:
Patients with suspected or proven infection should be isolated
Ò Visit:
Visitation in the unit should be limited
Ò Patient care equipment:
Washing, cleaning and sterilizing the machines should not be done in the unit, but rather they should be transported for sterilization
Basic CPR
Basic CPR
An injured adult on the street
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who does not breathe, does not speak, and does not respond, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total obstruction of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Steps:
1. An initial assessment of the environment surrounding the injured person and ensuring that it is free of any dangerous factors (electricity, fire, drowning, etc.).
2. In the first 10 seconds from the beginning of seeing the injured person, the injured person is placed lying on his back, his degree of consciousness is assessed, and he is called in a loud voice with a shrug of the shoulders, “Are you okay??” '.
· No response or abnormal breathing.

1. Call for emergency medical assistance by calling the local number.
2. Make sure there is a clear pulse (no less than 5 seconds and no more than 10 seconds).
· Pulse in the carotid artery (on both sides of the larynx for ease of identifying the presence of a pulse since it is the largest artery in the body) from the side opposite the paramedic.
3. When there is no confirmed pulse within 10 seconds, perform cardiopulmonary resuscitation as follows:
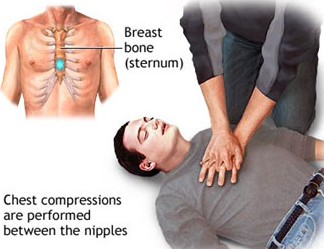
· Never expose the injured person’s chest.
· Place the palm of one hand (the whole hand) vertically in the middle of the sternum between the nipples.
· Start doing chest compressions at a rate of 30 compressions in a period not exceeding 18 seconds, or less if there are one or two paramedics.
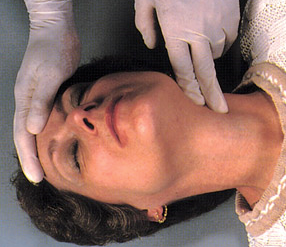
To perform cardiopulmonary resuscitation in a correct and effective manner, the following must be taken into account:
· Place the injured person on a hard surface.
· Begin compressions on the casualty’s chest within 10 seconds.
· Press hard, quickly, and to a depth of 5 cm in adults over 18 years of age
· Allow the rib cage to take its natural space after each compression
· Reduce external influences (as long as they are less than 10 seconds)
· Give the injured person an effective breath (by opening the airway by tilting the head back, pulling the chin forward, and opening the airway - but in the case of injuries to the cervical vertebrae, stabilize the injured person’s head)
· Give 2 breaths if there is one or two paramedics present to the seriously injured person, within a period not exceeding three seconds.
· Five consecutive cycles of compressions and breathing are performed (for a period of two minutes), with re-evaluation of breathing and pulse.

|
Note: When following these steps, take into account infection control policies for administering treatment. |
Basic CPR
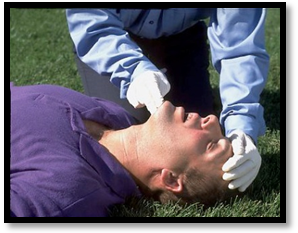
For an injured child on the street
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who is not breathing, speaking, or responding, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total blockage of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Action Steps :
· An initial assessment of the environment surrounding the injured person and ensuring that it is free of any dangerous factors (electricity, fire, drowning, etc.)
· In the first 1k0 seconds from the beginning of seeing the injured person, the injured person is placed lying on his back, his degree of consciousness is assessed, and he is called out in a loud voice while shaking his legs, “Are you okay??” '.
· No response or abnormal breathing.
· Ask for emergency medical assistance by calling the local number.
· Make sure there is a clear pulse (no less than 5 seconds and no more than 10 seconds).
· The pulse in the brachial artery (the inner side of the arm for easy identification of the presence of a pulse, given that it is the largest artery in the body on the side opposite the paramedic.
5. When it is confirmed that there is no confirmed pulse within 10 seconds, perform cardiopulmonary resuscitation as follows:
· Never expose the injured person’s chest.
Place the index and middle fingers of the hand vertically in the middle of the sternum between the nipples if there is a single paramedic and the thumbs of both hands if there are two paramedics.
· Start doing chest compressions at a rate of 30 compressions in a period not exceeding 18 seconds, or less if there is one paramedic, and if there are two paramedics, give 15 compressions.
To perform cardiopulmonary resuscitation in a correct and effective manner, the following must be taken into account:
· Place the injured person on a hard surface.
· Begin compressions on the injured person’s chest within 10 seconds.
· Press hard, quickly, and to a depth of 4 cm in children from one to eight years of age.
· Make the rib cage take the natural space after each compression
· Reduce external influences (as long as they are less than 10 seconds).
· Give the injured person an effective breath (by opening the airway by tilting the head back and pulling the chin forward and opening the airway - or in the case of injuries to the cervical vertebrae, immobilize the injured person’s head).
· Give 2 breaths if there is one or two paramedics present.
6. Five successive cycles of compressions and breathing are performed (for a period of two minutes), with re-evaluation of breathing and pulse.



Note: When following these steps, take into account the infection control policies for administering the treatment
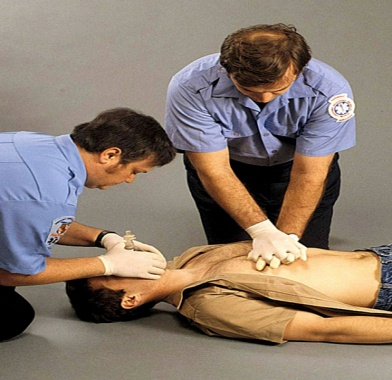
Advanced cardiopulmonary resuscitation in hospital
The Definition :
The process of pumping blood through heart massage while artificially supplying air to the lungs for a person who does not breathe, does not speak, and does not respond, so that no movement is noticed above the level of the chest, and no sound of breathing is heard.
The Reasons :
Total obstruction of the airways - accidents such as drowning - suffocation - exposure to a strong electric shock - some diseases such as asthma - pulmonary edema.
The person in charge:
Nursing team.
Tools :
Hands.
Action Steps :
· Ensure that the surrounding environment is safe for the workers and the patient (in a period not exceeding 10 seconds).
· Adjusting the patient’s position.
· Ensure the level of consciousness of the injured person (by gently shaking the shoulders and speaking to the patient in a loud voice, “Are you okay?” for a period not exceeding 10 seconds).
· If the patient answers, this indicates that the heart and lungs are working well, and in this case it is evaluated whether the patient needs other assistance or not.
1. If the patient does not answer, we begin by taking the following steps:
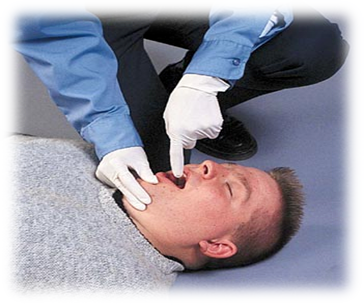
· Opening the patient’s airway:
· Opening the airway by installing a laryngeal tube - which is the best way to open the airway, but it is only installed in the hospital due to the lack of capabilities and human resources trained for this in the street.
· Assess the patient’s breathing:
· By looking at the patient’s chest (there is movement in the patient’s chest up and down), the duration of the breathing assessment is 10 seconds.
Evaluate the presence of a pulse or not:
· By checking the pulse with the carotid artery for no more than 10 seconds and no less than 5 seconds from the direction opposite the paramedic.
In the absence of breathing and pulse:
· Press on the sternum above the xiphoid process, 2 finger distances, in the middle of the line between the nipples.
· Interlock your fingers and press them together.
· The hands should be straight and perpendicular to the chest, the back should be straight, and the force of the pressure should come from the muscles of the pelvis and legs.
· Giving the patient breathing through a throat tube or using a tube mask (mouth-to-mouth breathing is not given).
· The ratio of chest compressions to the rate of breathing for the patient varies depending on whether a throat tube is present or not:
· In case of a throat tube:
· Perform 30 chest compressions for 2 breaths, whether by one paramedic or two paramedics.
In the absence of a throat tube:
· Perform 100 chest compressions per minute and at the same time give 8-10 breaths per minute.
· Perform five cycles of chest compressions and breathing, then re-evaluate breathing and pulse.
· If the heart returns to work, chest compressions are stopped and the patient is placed on a ventilator according to his condition.

· The hands should be straight and perpendicular to the chest, the back should be straight, and the force of the pressure should come from the muscles of the pelvis and legs.
· Giving the patient breathing through a throat tube or using a tube mask (mouth-to-mouth breathing is not given).
The ratio of chest compressions to the rate of breathing for the patient varies depending on the presence of a throat tube or not:
· In the case of a throat tube:
· Perform 30 chest compressions for 2 breaths, whether by one paramedic or two paramedics.
In the absence of a throat tube:
· Perform 100 chest compressions per minute and at the same time give 8-10 breaths per minute.
· Perform five cycles of chest compressions and breathing, then re-evaluate breathing and pulse.
· If the heart returns to work, chest compressions are stopped and the patient is placed on a ventilator according to his condition.
Choking (respiratory obstruction)
Definition of a lump:
Bloating occurs when a solid or liquid object or the back of the tongue blocks the airway, and the victim may quickly stop breathing and lose consciousness. The blockage may be partial or complete, such as (false teeth, food debris, coins, etc.). This may affect the patient's breathing and may lead to loss of consciousness. If immediate intervention is performed, the blockage may be partial or complete.
The Reasons:-
◾ Trying to swallow large pieces of food without chewing them well.
◾ May result from muscle spasm.
◾ Use a denture. Artificial teeth make it difficult to feel the size of the bite while chewing and swallowing.
◾ Speaking emotionally or laughing while eating.
◾ Walking, playing, or running with objects in the mouth.
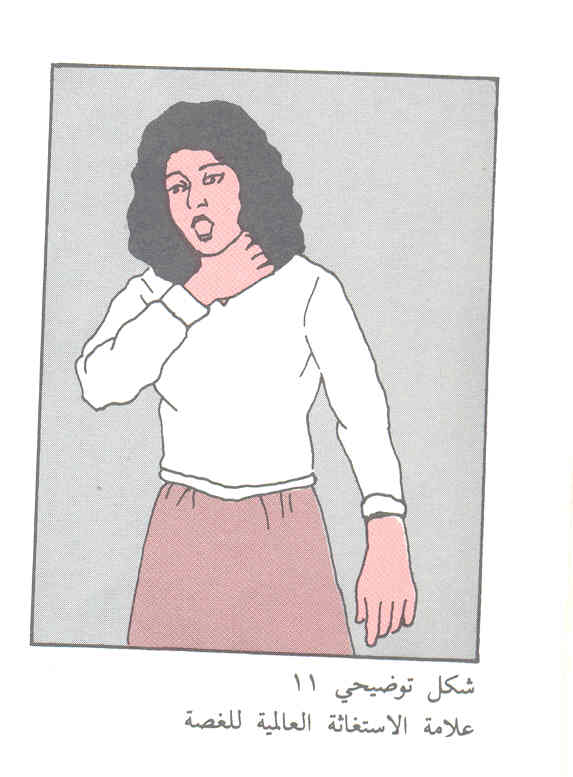
Tags:-
Partial airway obstruction:
◾ When the patient suffers from partial airway obstruction, he coughs forcefully in an attempt to dislodge the object blocking the airway, and he may be able to speak.
◾ Whistling may be heard when breathing.
◾ The injured person may hold his throat with one or both hands.
If the patient is conscious:
◾ Ask the patient to cough as this helps expel the foreign body.
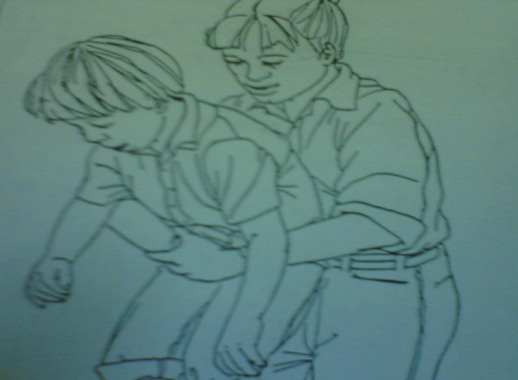
◾ If the patient cannot respond, the Hemlich-Hetti method is used
◾ The foreign body is expelled from the airway through...
◾ Stand behind the patient and wrap the arms around his waist.
◾ Place the thumb side of your fist in front of the injured person’s abdomen, just above the navel
◾ And clench your fist with the other hand.
Press inward and up the abdomen with quick pushes and repeat these pushes

1. In the case of pregnant women or an obese person, do not use the Hemlich method, but place the hands in the middle of the sternum so that the thrusts do not lose their strength.

2. If the patient is a child from the age of puberty, we use abdominal pressures while holding the child on the foot for five pressures.
3. If the patient is a child from one month to one year, the nurse uses five back compressions or five chest thrusts, but using the palm of the hand.

An unconscious patient
1. Place the patient on his back so that you can open the airway.
2. Bend the patient’s head backwards with a slight tilt to one side to facilitate the foreign body’s exit.
3. The finger is inserted to wipe the patient’s mouth from the inside using a hook method.
4. If the foreign body does not come out, the patient is given one count of exhalation and the chest is observed to rise
5. Follow Hemlich’s steps until the foreign body is out of the airway:
6. Sit on the knees so that they surround the patient’s thighs.
7. Place the palm of one hand above the stomach area.
8. You place the other hand on the first hand and press on the abdomen with five quick successive pushes to increase internal pressure to help push the foreign body out.
9. The steps are repeated until the patient expels the foreign body.
10. The pulse is checked. If there is no pulse, cardiopulmonary resuscitation procedures begin.
11. If the injured person loses consciousness, lower him to the ground, supporting his head and neck
12. Clean the mouth with your finger in the shape of a hook
13. If there is no response, apply pressure on the abdomen.


- Nursing evaluation
¨ The initial examination of the patient is considered very important because its steps are the highest priority. By evaluating the patient, sources of threat to the patient’s life can be identified.
· The nursing staff evaluates the patient upon admission to the hospital using the nursing staff evaluation form.
A form for evaluating the patient's condition upon admission to the hospital
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
· Initial information and data are recorded when the patient enters the department on the nursing staff evaluation form for the patient:
- Vital signs (pressure - pulse - respiratory rate - temperature).
- Weight and height.
- The presence of allergies.
- Pain assessment
- Evaluation of skin condition
- Assess the patient regarding the possibility of a fall
- Nutritional assessment.
- Evaluation of motor activity.
- The patient’s need for restraint or isolation.
- Informing the patient of his rights, responsibilities, and hospital policy within 24 hours of admission.
The nursing staff evaluates the patient and determines the following:
In critical cases: (intensive care)
1- Degree of awareness and awareness.
2- Vital signs.
3- Complications occur.
o The nursing evaluation rate is continuous and the doctor on duty in the department is called in the case of critical results (physiological - laboratory - x-ray) and when there is pain, and the doctor re-evaluates.
o The re-evaluation of the patient is documented and a follow-up note is recorded at least once per shift, and any procedures resulting from a call or emergency or important events for the patient are recorded with the date and time.
In non-critical cases
Are evaluated:
· Vital Signs .
· Patient’s compliance with treatment and medical instructions.
◼️ - This is done every 12 hours for the internal department by members of the nursing staff, unless the clinical evidence requires less than that and this is proven in the patient’s file.
Conditions that require long-term treatment (chronic diseases)
Nursing staff care for patients who need long-term or (chronic) treatment and ensure...
· Vital Signs .
· Complications occur
· Results of treatment
The nursing staff on duty also re-evaluates the patient every shift to determine the patient's needs
Items that need to be re-evaluated
· The treatment plan developed for the patient Individualized care plan
· Change in the patient's condition condition Change in patient
· Patient diagnosis
· Desired outcome of care, treatment or service
· The extent of the patient's response to treatment
The re-evaluation is documented in the patient's file with another evaluation form.
Content of nursing reassessment
1- Vital signs: every 6 hours in inpatient departments, every 2 hours in care and premature care, after blood transfusion, before surgical operations, during recovery, and when the patient complains that requires re-measurement, or according to the doctor’s instructions.
2- Pain:
3- The possibility of the patient falling: every shift.
4- Skin condition: all skin color during recovery.
5- Nutritional assessment: when the patient needs it, according to the doctor’s orders.
6- Measuring blood sugar: according to the doctor’s instructions.
7- The patient’s need for restraint or isolation: according to the doctor’s orders.
Pain assessment:
The responsible nursing staff assesses the pain (according to the following table), determines its severity, describes the pain and its frequency by asking the patient and looking at the patient’s facial expression (in the event that he is unable to speak or in the event that he is a child). This is recorded in the pain assessment form and kept in the patient’s file when Admission of the patient to the hospital.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 |
 |
 |
 |
 |
 |
|
The treating physician develops a pain treatment plan and records this in the patient’s medical file.
The responsible nursing staff implements the treatment and follow-up plan in accordance with the pain model and the doctor’s instructions.
The responsible nursing staff re-evaluates the pain and records it in the previous form and completes it with each nursing shift. The evaluation can be re-evaluated more than that depending on the patient’s condition:
1. The responsible nursing staff re-evaluates the pain once before surgeries and after surgeries, once every hour for 3 hours, then every shift, or according to the doctor’s orders.
2. The responsible nursing staff re-evaluates the pain if pain is present and after administering pain medication only
- Vital Signs
The Definition
These are indicators that health team members search for through a physical examination to determine the basic functions of the body, which include temperature, pulse, breathing, and blood pressure.
Oral temperature measurement
The Definition :
Temperature is a number that indicates the state of the body in terms of hotness and coldness.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
36.4 – 37.4 degrees Celsius.
The person in charge:
Nursing team.
Tools :
Mercury thermometer - alcohol - piece of gauze - timer.
Steps:
1. Getting to know the patient. (Patient's name and identification bracelet)
2. Explain the procedure to the patient.
3. Washing hands.
4. Prepare tools.
5. Maintain patient privacy.
6. Adjust the thermometer and move it vigorously until the mercury line reaches 35 degrees (the starting point).
7. Clean the thermometer from top to bottom with alcohol.
8. Place the thermometer at eye level to ensure that it reaches the starting point.
9. Place the mercury portion of the thermometer under the tongue for (three minutes) in the patient’s mouth.
10. Extract the thermometer from the patient’s mouth.
11. Clean the thermometer from bottom to top with a dry piece of gauze.
12. Reading the measurement Record the thermometer reading on the temperature recording form.
13. Move the thermometer vigorously to lower the mercury level.
14. Clean the mercury part of the thermometer from top to bottom with soap and water, dry it, and disinfect it with alcohol.
15. Place the thermometer in its designated container.
16. Hand washing.
17. Reassure the patient.
18. Record any emergency signs.
Measure the temperature through the armpit
The Definition :
Temperature is a number that indicates the state of the body in terms of hotness and coldness.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
36.4 – 37.4 degrees Celsius.
The person in charge:
Nursing team.
Tools :
Mercury thermometer - alcohol - piece of gauze - timer.
1. Steps:
2. Getting to know the patient. (Patient's name and identification bracelet)
3. Explain the procedure to the patient.
4. Washing hands.
5. Prepare tools.
6. Maintain patient privacy.
7. Adjust the thermometer and move it vigorously until the mercury line reaches 35 degrees (the starting point).
8. Clean the thermometer from top to bottom with alcohol.
9. Place the thermometer at eye level to ensure that it reaches the starting point.
10. Place the mercury part of the thermometer under the armpit, making sure that this place is dry for (five minutes).
11. Removing the thermometer from the patient’s mouth.
12. Clean the thermometer from bottom to top with a dry piece of gauze.
13. Reading the measurement Record the thermometer reading on the temperature recording form. Taking into account (half a degree increase when reading the thermometer) and signed.
14. Move the thermometer vigorously to lower the mercury level.
15. Clean the mercury part of the thermometer from top to bottom with soap and water, dry it, and disinfect it with alcohol.
16. Place the thermometer in its designated container.
17. Hand washing.
18. Reassure the patient.
19. Record any emergency signs.
Measuring temperature through the anus
The Definition :
Temperature is a number that indicates the state of the body in terms of hotness and coldness.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
36.4 – 37.4°C with half a degree increase.
The person in charge:
Nursing team.
Tools :
Mercury thermometer - alcohol - piece of gauze - timer.
Steps:
1. Getting to know the patient.
· (Patient’s name and identification bracelet)
2. Explain the procedure to the patient.
3. Hand washing.
4. Prepare tools.
5. Maintain patient privacy.
6. Adjust the thermometer and move it vigorously until the mercury line reaches 35 degrees (the starting point).
7. Clean the thermometer from the mercury part from top to bottom with alcohol.
8. Place the thermometer at eye level to ensure it reaches the starting point.
9. Place gel on the edge of the mercury part and place the thermometer for a minute, taking care that the patient is on his side.
10. Remove the thermometer and clean the mercury part from the bottom with a dry piece of gauze.
11. Read the measurement and record the thermometer reading on the temperature recording form. Taking into account (a decrease of half a degree when reading the thermometer).
12. Move the thermometer vigorously to lower the mercury level.
13. Clean the mercury part of the thermometer from top to bottom with soap and water, dry it, and disinfect it with alcohol.
14. Place the thermometer in its designated container.
15. Hand washing.
16. Reassure the patient.
17. Record any emergency signs.
Note: The anal measurement method is used in children and burn cases.
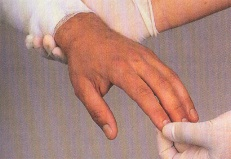
Pulse measurement
The Definition :
The pulse is the wave generated in the arteries as a result of the contraction of the heart. The pulse can be felt by feeling the large arteries in the human body, such as the neck and wrist. (As in the attached picture)

The Reasons :
Monitoring the patient's vital functions.
Normal rates:
70-100 N/Q per adult and 80-130 N/Q for children.
The person in charge:
Nursing team.
Tools :
Time timer.
Steps:
1. Getting to know the patient. (Patient's name and identification bracelet)
2. Explain the procedure to the patient.
3. Washing hands.
4. Prepare tools.
5. Choose a comfortable position for the patient.
6. Place the tip of two fingers of the hand (index and middle) on the artery (radial - carotid - femoral)
7. Using the watch with the other hand.
8. Count the pulse for one full minute. The normal pulse rate is 70-100 beats/s in an adult and 80-130 beats/s in children.
9. Record the pulse using the vital notes form and report if the pulse is (fast - slow - strong - weak - irregular).
10. Reassure the patient.
11. Hand washing.
◼️ Respiratory measurement
The Definition :
Evaluating the rate and regularity of breathing (which is the process of the body obtaining oxygen through breathing, which is necessary to carry out its activities and get rid of carbon dioxide).
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
12-20 N/Q per adult and 24-40 N/Q for children.
The person in charge:
Nursing team.
Tools :
Time timer.
Steps:
1. Getting to know the patient. (Patient's name and identification bracelet)
2. Explain the procedure to the patient.
3. Preparing tools.
4. Be careful not to measure breathing after muscular effort.
5. Place the patient in a comfortable position, preferably half-sitting.
6. Ensure that the patient’s chest movement is clear to her.
7. Observe the rise and fall of the patient’s chest.
8. Each inhalation and exhalation is counted as one breath for a full minute.
9. Notice any abnormal signs in breathing.
10. Observe the patient’s color, especially around the lips and fingernails.
11. Record the respiratory rate on the patient’s form.
12. Inform the doctor of any abnormal signs.
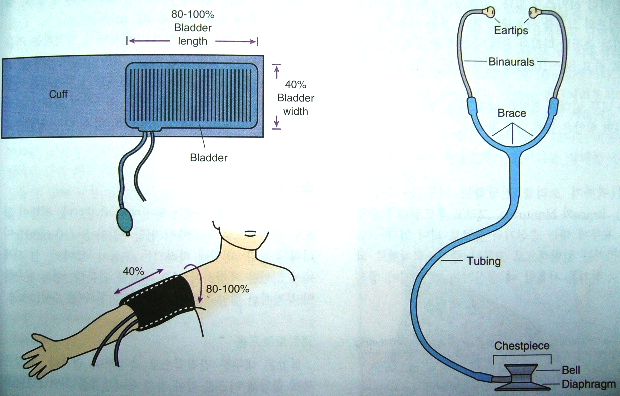
◼️ Measuring blood pressure:
The Definition :
Evaluating the movement of blood circulation by knowing the volume of blood, the blood returning to the heart, the extent of resistance of peripheral blood vessels, and the elasticity of the arteries.
The Reasons :
Monitoring the patient's vital functions.
Normal rates:
80/110 mm/Hg.
The person in charge:
Nursing team.
Tools :
Blood pressure device and stethoscope.
Steps:
1. Getting to know the patient. (Patient's name and identification bracelet)
2. Explain the procedure to the patient.
3. Prepare tools.
4. Be careful not to measure pressure after muscular effort.
5. Place the patient in a comfortable position.
6. Maintain patient privacy.
7. Measure blood pressure before and after giving high blood pressure medications.
8. Record your blood pressure measurement directly on the form designated for that purpose.
9. Determine the type of diet (low salt and fat).
10. Note the complications that may occur to the patient (nosebleeds).
- Spare parts for wounds
Definition of a wound: It is an abnormal cut or tear in body tissue.
Wound risks: bleeding, infection and shock
Steps to treat wounds
1. Stop the bleeding: Minor wounds and abrasions usually stop bleeding on their own. If this does not happen, apply gentle pressure with a clean cloth or bandage. Continue to apply pressure for 20 to 30 minutes. If possible, raise the wound to the top to help stop the bleeding. Do not open the wound to check whether the bleeding has stopped or not, because this may delay the clotting process, which will cause the bleeding to continue. If the blood continues to flow after continuous pressure.
2. Cleaning the wound: Rinse the wound with clear water. Soap can irritate the wound, so avoid using soap directly on the wound. If you find dust or fragments still in the wound after washing, use tweezers after disinfecting it with alcohol to remove any foreign particles in the skin. If Some splinters remain inside. See a doctor. Thorough cleaning reduces the risk of infection and tetanus. To clean the area around the wound, use only soap and a towel. There is no need to use hydrogen peroxide, iodine or antiseptics containing iodine.
3. Apply antibiotics: After cleaning the wound, apply a thin layer of antibiotic cream or ointment to help keep the wound surface moist. Antibiotics do not speed up healing, but they can suppress infection and help the body’s natural healing process. Some ingredients in some Ointments can cause skin rashes in some people. If a rash appears, stop using the ointment immediately.
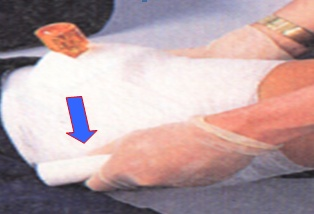
4. Cover the wound: Bandages can help keep the wound clean and keep harmful bacteria out of the wound. After the wound has healed enough that infection is unlikely, leave it exposed to the air to speed healing.
5. Change the wound: Change the wound at least daily or whenever it becomes wet or dirty. If you become allergic to the N8 adhesive used in most bandages, change to non-adhesive bandages or sterile gauze, which is held in place with paper tape, or The gauze roll is secured with an elastic band. These supplies are generally available in pharmacies.
6. Get stitches for deep wounds: If the wound is more than 6 millimeters deep, or if it is deep, it usually requires stitches. Adhesive tapes or bandages are suitable for minor wounds, but if it is difficult to close them easily, you should see a doctor as soon as possible. Proper closure. Within a few hours it reduces the risk of infection.

1. Watch for signs of wound infection and infection: See your doctor if the wound does not heal or you notice any redness, increased pain, pus drainage, warmth or swelling.
2. Get a tetanus vaccination: Doctors recommend getting a tetanus vaccination every 10 years. If your wound is deep or dirty and your last vaccination was more than five years ago, your doctor may recommend a tetanus booster shot.
Wounds are divided into:
(1) Closed wounds or bruises: where the skin remains intact, and the cut occurs in the subcutaneous tissue, the subcutaneous tissue may be severely injured.
Causes: Collision with a hard, blunt object that causes bleeding in the blood vessels under the skin
Symptoms: Pain, swelling, and discoloration in soft tissues.
First aid for closed wounds:
• Raising the injured arm or leg.
• Apply ice or cold water compresses to the affected area.
• Examine the injured person carefully for fractures and injuries.
• When an injury to an internal organ is suspected, the injured person is immediately sent to see a doctor.

(1) Open wounds: These are wounds in which a cut appears in the skin, and open wounds are usually accompanied by external bleeding.
Types of open wounds and their causes:
1. Abrasions: They are just skin abrasions, such as minor scratches or friction with objects such as the ground, and they often occur in children from falling to the ground.
The potential bleeding in these cases is no more than a simple leak of blood from the capillaries, but the possibility of contamination exists, as dust and bacteria may find their way into the open tissues.

First aid for abrasions:
• Wash the wound well with soap and water, and it can be disinfected with an antiseptic solution such as Betadine.
• It can be left without a cover, and if necessary, it can be covered with an adhesive plaster after applying a small piece of gauze.
• Look for any other injuries elsewhere
1. Incisional wounds: These are wounds in which tissue is cut and usually have regular edges and are caused by sharp objects such as knives and pieces of glass. Bleeding is frequent from these wounds.

First aid for incisional wounds:
• Medical gloves must be worn to prevent transmission of infection.
• Bleeding must be stopped immediately before cleaning and treating wounds.
• Press the wound site with sterile medical gauze or clean cloth, with the tip lifting the affected part up.
• After the bleeding stops, clean the wound by washing it gently with pure water only (keep soap away from reaching the wound opening directly because soap causes irritation of the broken tissue in the wound).
• If there are visible objects inside the wound even after washing it with water, use tweezers sterilized with alcohol to remove those objects.
• Wrap the wound, taking care not to apply too much pressure so as not to affect blood flow. Always make sure that the fingers and toes are warm and the injured person can move them.
• If you find the fingertips cold, loosen the bandage to allow blood to circulate in the limbs and transport the injured person to the hospital immediately.
• Deal with bleeding as mentioned above.
• It is best to change the bandage covering the wound every day if amounts of fluid and pus are coming out of it. However, if the wound is clean, the bandage or patch is changed whenever it gets externally dirty.
• After the wound begins to heal, the cover is opened because wounds heal faster when they are exposed to air.
• In some wounds, it may be necessary to place stitches to sew the two ends of the wound and bring them closer together to facilitate wound healing in the case of:
- If the wound exceeds 6 cm.
- There is a clear gap between the two ends of the wound.
- The cut in the wound reached the point where tissue from the fat or muscle layer began to appear through it.

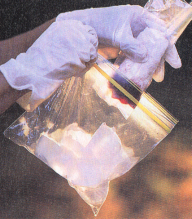
1. Extractive wounds: They are wounds in which part of the tissues of the injured person’s body is separated or torn, such as the removal of a finger, the tip of an ear, or one of the limbs of the body. They usually occur as a result
of animal bites or injuries from accidents, machinery, and explosives, and are usually followed by severe bleeding.

First aid for puncture wounds:
• Wear gloves to prevent transmission of infection.
• Press the wound with a clean cloth or sterile dressing, if available, to stop the bleeding.
• Raise the affected part above the level of the heart
• If the lacerated tissues (skin or muscles) are not separated, they are returned to their place and pressure is applied to the wound with bandages.
If the removed part is separated:
• Place the removed body (if possible) in a salt solution bag or place it in any clean bag
• This bag is placed in another bag filled with ice.
• The injured person and the removed part are transferred to the nearest (large) hospital immediately because it is possible for some surgeons to return the removed part to its place in the body.
If the bleeding does not stop with pressure and lifting:
• Pressure is placed on the artery supplying the site of the injury
• The turnkey should not be used unless there is a possibility of severe bleeding and delaying first aid.
1. Puncture or penetrating wounds: These are wounds caused by pointed objects such as nails and splinters. These wounds reach a deep distance into the tissues, and there is no visible external bleeding. However, the pointed object may penetrate the tissue to a great depth, infecting the viscera and organs, causing internal bleeding
These wounds are among the wounds most likely to become infected due to their depth and lack of external bleeding, and there is a high possibility of tetanus microbe activity.

First aid for puncture or penetrating wounds:
• Fix the inserted part (knife or hacksaw) inside the body in order to prevent air entry, wound contamination, increased bleeding, and tissue damage.
• Remove the implanted object only if it is necessary to perform cardiopulmonary resuscitation and the object is implanted in the chest or if this object penetrates the respiratory tract.
• If there is a need to move the injured person, pressure is applied around the implanted object and it is secured with straps
• If the implanted object is long, it should be shortened if possible to reduce its movement and thus reduce damage to the surrounding tissues, reduce bleeding, and transport the injured person to the hospital as quickly as possible.
Signs of serious bleeding:
§ Heavy bleeding continues despite applying pressure on the bleeding site for at least 15 minutes.
§ Severe pain occurs.
§ Bleeding from the vagina of a pregnant or postpartum woman.
§ Blood coming out of openings in the human body.
§ Shock occurs.
Instruments used to change the wound:
Spare cart contains:
(The upper surface contains: solutions [alcohol 7% - Betadine 10% - salt solution - and other disinfectants according to the doctor’s instructions) sterile spare bags containing (2 spare dryers + 2 pieces of dressing + 5 pieces of gauze + a basin - the lower surface contains: a basin A large kidney to store the machines after use - tarpaulin, plastic bags to put the used machines in - clean gloves - gauze ties of different sizes - clean scissors).
Steps:
1. Hand washing (hygienic).
2. Prepare the tools
3. Explain the procedure that will be performed to the patient.
4. Ensure that the spare vehicle is clean and dry and that the wheel is intact.
5. Ensure that the vehicle is ready and complete (top and bottom deck).
6. Maintaining patient privacy.
7. The cover is lifted and the patient lies in a comfortable resting position.
8. Expose the wound site and place a tarp under the patient next to the wound.
9. Place the clean kidney pelvis on the linoleum.
10. Wear clean gloves and remove the adhesive plaster gently and quickly so that the patient does not suffer from pain.
11. Put the spare parts inside the bag inside the renal pelvis.
12. Assess the condition of the wound to determine its type.
13. The gloves are removed and another gloves are put on.
14. Open the sterile packet on the upper surface of the cart.
15. Picking up the peat end of the bag in case there is a doctor to make the change or an assistant nurse. With this peat, he picks up another peat and hands it to the second party, then covers the contents of the bag.
16. Determine the type of solution that will be used in the dressing according to your assessment of the wound or according to the doctor’s instructions.
17. Place the solution in the sterile renal basin.
18. Pick up a piece of gauze from the peat packet and then place it in the basin or lid.
19. Start cleaning the wound, starting from the inside out. You can use more than one piece.
20. Make sure to clean the wound and then dry it by following the previous step.
21. Observe the wound during dressing, the surface around it, and any local symptoms.
22. Place the sterile dressing and secure it using adhesive or gauze ties.
23. Clean the place of all used toiletries, then put them in the red bag.
24. Pull the tarpaulin from under the patient, then apply it inward and place it on the bottom surface of the cart.
25. Collect used instruments and place them in a kidney basin filled with soapy water.
26. Cover the patient and make the bed.
27. Hand washing (routine).
Installation of a peripheral intravenous catheter (cannula)
The Definition :
It is a device that is connected intravenously to administer intravenous medications and solutions.
Most exposed people:
All patients treated with intravenous injections.
Working team:
Nursing team.
Tools :
Tray with lid - cannulas of different sizes - medical cotton - plaster strips - latex gloves - 70% alcohol.
Steps:
1. Verify the patient’s identity and double-check the name.
2. Explain the procedure to the patient to reduce his anxiety.
3. Maintaining patient privacy.
4. Washing hands and wearing gloves.
5. Tie the forearm with a compression bandage, preferably the forearm that is least used.
6. Disinfect the catheter installation site with 70% alcohol and leave it to dry. Do not touch it after disinfection
7. Insertion of the cannula and observing the appearance of a spurt of blood in the place known as the cannula (as a sign of penetration of the vein wall) and completing the insertion slowly while pulling the metal insert out of the vein so as not to attempt to insert the same cannula again.
8. Remove the compression bandage from the forearm (tournament).
9. Connecting the solution device to the cannula to test the efficient operation of the cannula.
10. Secure the cannula with adhesive tape, noting the date of installation.
11. Leave the installation site dry and visible.
12. Dispose of the cannula tip immediately after use in the sharps waste safety box.
13. Clean the used tools, put everything back in its place, and prepare it for the next use.
Cannula removal should be considered in the following cases:
· Immediately after a blood transfusion.
· After completing the need for it, or after only 3 days have passed since installation.
· When redness or inflammation appears at the cannula site.
Make an enema
The Definition :
It is an injection that is given to the patient rectally according to the doctor’s instructions.
Most exposed people:
Patients with hepatic coma - patients with constipation - patients before surgeries
Tools :
(The tray contains: an enema device - water with a laxative dissolved in it - a solution as ordered by the doctor, the temperature of which is according to the gender and age for adults: 40: 43 degrees, for children 37.7 degrees Celsius - a rubber or plastic tube - a metal stopcock - a renal basin - a towel - a large piece of cotton -Linoleum).
Steps:
1. Hand washing (routine).
2. Wear rubber gloves (non-sterile).
3. Preparing patient confirmation.
4. Explain the procedure to the patient.
5. Maintain patient privacy.
6. Add the solution to the container, then allow it to move through the tube to the end and close the stopcock.
7. Place a tarp under the patient.
8. Place the patient on the left side or on his back, depending on the patient’s condition, with the anus exposed.
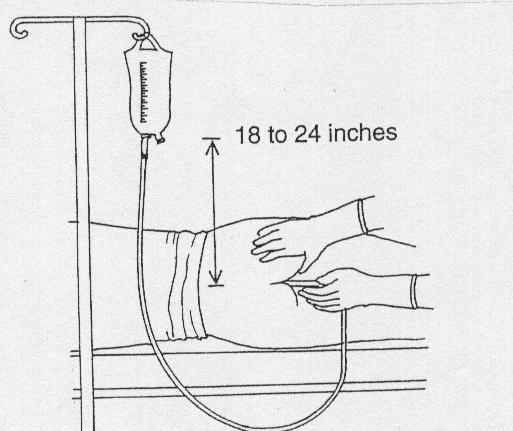
9. Raise the solution approximately 45cm above the patient’s level and plan to administer the solution slowly over a period of 5-10 minutes.
10. Apply a laxative to the end of the anal tube about 5-7 cm.
11. Gently insert the rectal tube into the anus about 10 cm. (Figure 1)
12. Inserting a small amount of solution. If resistance occurs, withdraw the tube slightly and continue inserting by asking the patient to take a deep inhale several times.
13. Introduce the solution slowly for 5-10 minutes.
14. Close the tube after giving the solution or when the patient wants to defecate. The tube is removed and the gloves are removed.
15. Help the patient to reach the toilet when he feels strong to defecate after 5-10 minutes.
16. Recording stool characteristics and the patient’s reaction to the enema.
17. Help the patient clean and wash the anal area with soap and water. Figure (1)
18. Tool care.
19. Hand washing (routine).
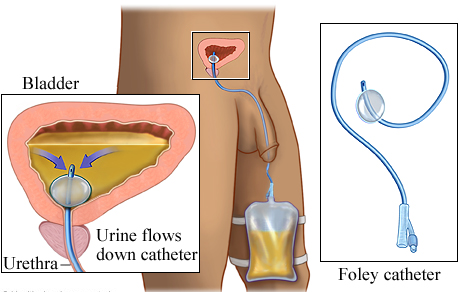
- Catheter installation
Installation of a urinary catheter
Definition :
It is a procedure performed for the patient in pathological conditions according to the doctor's instructions .
Causes :
Bladder emptying-estimating the amount of fluid coming out-surgical operations
The Working Group :
The nursing team.
Exposed persons :
Liver disease-kidney disease-urinary tract disease-bed disease
Tools :
A urinary catheter of a suitable size for the patient – a urine collection bag – a 10 cm syringe – salt solution – sterile Guante – gauze – Betadine for disinfection – KY gel-medical adhesive.
Steps:
1. To preserve the privacy of the patient, a paraffin is placed Oris installed in a spare booth.
2. Tell the patient what you will do and explain the medical reasons for installing the catheter.
3. Collects the necessary tools for the installation of a urinary catheter.
4. Surgical hand washing.
5. Wear a sterile glove.
6. Connect the urine collection bag to the catheter first.
7. Apply 3 mL of gel (or any anti-friction material).
8. First, a sterile catheter for the doctor to install.
After installing the catheter :
1. Fixation of the catheter in the thigh with a plastic.
2. Install the bag of all urine below the patient's bed level and place it on the urine carrier to prevent reflux of urine.
3. Bring a patient's own urinal to empty urine from the urine collection bag.
4. Dispose of the waste in its own red bag.
5. Routinely wash hands after taking off gloves and dry them thoroughly.
6. Note in the nurse's note the type of catheter, the time of installation and the doctor who installed the catheter by
Note and record the amount of urine and any changes from the presence of (blood-pus ) with informing the doctor
- Collect samples and perform analysis
Drawing blood samples
The Definition :
It is a procedure done to obtain a blood sample for analysis.
Most exposed people:
Patients in departments.
Working team:
Nursing team.
Tools :
70% alcohol - sterile and dry cotton - syringes measured according to the required quantity - tourniquet
Steps:
1. Explain the procedure to the patient.
2. Washing hands.
3. Place the tourniquet above the elbow and tie it.
4. Feeling the location of the vein and cleaning and disinfecting the location of the vein and its surroundings.
5. Choose the appropriate place and tighten the skin below the area chosen to take the sample.
6. Insert the tip of the needle into the vein at an angle of 30 degrees so that it enters the skin first and then enters the vein.
7. Raise the tourniquet and take the required amount of blood slowly.
8. Place a piece of sterile gauze over the place where the vein enters and apply pressure for 2-4 minutes until the blood stops.
9. Remove the syringe tip and place the amount of blood required for analysis into the tubes prepared for this purpose.
10. Place a sticker on each tube with the patient’s name and his file number (the department in which he is treated).
11. Dispose of used tools in the proper manner.
Do a sugar analysis
The Definition :
It is a procedure done to determine the blood sugar level.
Most exposed people:
Diabetics.
Working team:
Nursing team.
Tools :
Sugar analysis device - test strips with the same code as the device - sterile cotton or gauze - straws - alcohol - latex gloves.
Steps:
1. Washing hands.
2. Explain the procedure to the patient.
3. Wear a glove, hold the patient’s finger down and squeeze gently.
4. Wipe the tip of the finger with a piece of cotton containing alcohol and feel suspicious about the finger.
5. Place the tip of the strip or the designated place on the strip to place the drop of blood.
6. Press the finger with a cotton ball until the blood stops coming out.
7. Dispose of waste in the designated place.
8. The nurse records the blood sugar level on the relevant form and gives the insulin dose according to the doctor’s orders.
- Method of giving treatment
Giving treatment orally
The Definition :
These are medications that are given orally (such as tablets and syrup).
The Reasons :
Treating the patient's signs and symptoms.
The person in charge:
Nursing team.
Tools :
Medications dispensed to the patient.
It is important to follow the ten correct matters before giving the medicine (ten (10) Rights):-
1. The correct patient .
2. The correct medication.
3. The correct dose.
4. The correct way.
5. The correct time.
6. Healthy repetition.
7. Correct registration.
8. Required effectiveness.
9. The right to education.
10. Right of refusal.
Steps:
1. Washing hands.
2. Review the doctor’s order for the medication and prepare the treatment, taking into account the time coordination, unless the time at which administration is required is specified.
3. Verify the correct patient through the patient’s file and identification bracelet (full name and medical number).
4. Explain the procedure that will be performed to the patient.
5. Maintaining patient privacy.
6. Ask the patient to sit if possible so that he can take the medicine.
7. In the case of treatment with tablets, take the tablets to the patient with a glass of water, taking care not to touch the tablets with the hand.
Ensure that the patient takes the treatment dose on time in the presence of a nursing team member.
8. Notify the doctor if the patient refuses the medication to be given and write this down in the form designated for that purpose.
9. Securing the patient after giving medications that cause a change in the patient’s consciousness (narcotics, blood pressure medications, etc.) by raising the sides of the bed or warning the patient not to walk without assistance.
10. Notifying the treating physician in the event of any medication error, which is recorded in the form for reporting a medication error or the appearance of side effects of medications in the nursing registration form.
11. Recording the administration of treatment in the treatment implementation form.
Giving the treatment via intramuscular, subcutaneous, and intravenous injections
And allergy testing
The Definition :
These are medications that are given by intramuscular, intravenous, or subcutaneous injection (such as vials, ampoules, and diabetes treatment 'insulin').
The Reasons :
Treating the patient's signs and symptoms.
The person in charge:
Nursing team.
Tools :
Medicines - syringes - cotton - alcohol - solutions - intravenous devices - cannulas of different sizes - medical adhesive - tourniquet.
It is important to follow the ten correct matters before giving the medicine (ten (10) Rights):-
1. The correct patient.
2. The correct medication.
3. The correct dose.
4. The correct way.
5. The correct time.
6. Healthy repetition.
7. Correct registration.
8. Required effectiveness.
9. The right to education.
10. Right of refusal.
Steps:
· Hand washing.
· Verifying the patient (full name and medical number).
· Explaining the procedure that will be performed to the patient.
· Maintaining patient privacy.
Preparing treatment for intramuscular injection:
1. If it is a single ampoule, withdraw the treatment using a sterile syringe and expel the air from the syringe.
2. If the treatment needs to be analyzed, the water ampoule is withdrawn using a sterile syringe, then it is injected into the ampoule containing the powder, the bottle is shaken, then the specified dose is withdrawn using the syringe, then the air is expelled.
3. The site of intramuscular injection is determined.
4. Clean the site designated for the injection with a piece of cotton moistened with 70% alcohol in a circular manner and in one direction from the inside out without going back again.
5. Insert the tip of the syringe perpendicular to the injection site, then pull the syringe plunger out to confirm the injection site (if blood is drawn, the site is considered wrong and is changed, and if nothing is drawn, the site is correct and the treatment is injected).
Preparing treatment for a patient through intravenous injection:
1. Determine the location of the intravenous injection.
2. The place to be injected is tied with a tourniquet.
3. Feel the vein with the tip of the index finger.
4. Clean the site designated for the injection with a piece of cotton moistened with 70% alcohol in a circular manner and in one direction from the inside out without going back again.
5. The tip of the syringe is inserted at an angle slightly raised along a parallel line from the surface of the skin at the site of feeling the vein.
6. The syringe plunger is pulled out to confirm the location (blood flows into the syringe).
7. Loosen the tourniquet and inject the treatment slowly.
8. Press the injection site with a piece of cotton soaked in alcohol until the blood stops at the injection site.
9. Place a small piece of gauze at the injection site and secure it with adhesive tape.
10. Dispose of injection waste in a waste disposal bag.
11. Registration in the treatment description and implementation form.
Preparing treatment for a patient by subcutaneous injection:
1. Stabilize the skin at the injection site and, with a quick pricking motion, insert the needle at an angle of 90 degrees if the skin is thick and 45 degrees if the skin is thin.
2. Injecting the treatment to be given.
3. Remove the needle and press a piece of cotton soaked in alcohol on the injection site.
4. Dispose of all waste in accordance with infection control policy.
5. Recording the administration of treatment in the treatment description and implementation form.
Drug allergy test:
1. Perform the subcutaneous injection steps at a 45 degree angle in the case of a 3 cm syringe and a flat site in the case of an insulin syringe.
2. When injecting, inject only one ml of the drug to be tested.
3. Mark the injection site.
4. Observe the injection site for 10 minutes after the injection.
5. Notify the doctor if any reaction occurs (redness of the skin, visible swelling, tendency to scratch).
6. You record this on the patient’s ticket and allergy card.
7. The syringe containing the medication to be administered is prepared and the patient is injected if no reaction occurs.
8. The remaining steps are completed as usual for subcutaneous injection.
Note: When following these steps, infection control policies for administering treatment should be taken into account.
Transfusion
Definition: Giving a quantity of blood or its derivatives (plasma - platelets - red blood cells) to a patient according to the doctor’s instructions.
Reasons: Compensating blood loss from the patient’s body and treating an imbalance in blood components.
The person performing the work: the nursing team.
Tools: A bag of blood or its derivatives (usable) - a holder for solutions - a blood transfusion device - a spongy cotton with alcohol - medical tape - a large cannula.

Steps:
1. Hand washing (routine).
2. Verifying the patient (full name and medical number)
3. Measure the patient’s vital signs to ensure that they are within normal levels.
4. Explain the procedure that will be performed to the patient.
5. Maintaining patient privacy.
6. Review the patient’s full name - blood types - and match the bag number with the delivery form number.
7. Preparing medications for recovery and incompatibility next to the patient.
8. Wash your hands (hygiene) immediately before installation.
9. Open the blood transfusion device, connect it to a bottle of saline solution, and fill it (to test the efficiency of its work).
10. Connect the device to the blood bag and transfer it to the patient very slowly for the first 15 minutes
11. Measure the patient’s vital signs every 5 minutes for the first 15 minutes.
12. Note the presence of any symptoms of blood incompatibility with the patient’s body (such as: tremors, back pain, headache, vomiting, rapid pulse, low blood pressure, rapid breathing, skin rash).
13. Increase the drip in the absence of signs indicating incompatibility according to the doctor’s instructions on the ticket.
14. Dispose of the empty blood bag after completing the administration of the required amount, connect the blood transfusion device to the salt solution, pass the solution through the device until the blood disappears from it, and dispose of it in hazardous waste.
15. Measuring vital signs after a blood transfusion.
16. Wash hands and record this nursing procedure on the designated form.
Oxygen therapy
The Definition :
Giving an amount of O2 gas at a specific rate according to the patient’s needs and the doctor’s recommendations.
The Reasons :
Replenishing the proportion of oxygen in the body - maintaining the vitality of tissues and cells.
The person in charge:
Nursing team.
Tools :
Oxygen catheter - oxygen connector - oxygen regulator - sterile gauze - water humidifier with distilled water - cup of water.
Steps:
1. Hand washing (routine).
2. Verifying the patient (full name and medical number)
3. Measure the patient’s vital signs to ensure that they are within normal levels.
4. Explain the procedure to the patient.
5. Prepare the necessary tools.
6. Make the patient in a comfortable position.
7. Connect the regulator to the oxygen tube valve.
8. Connect the humidifier to the oxygen cylinder (or if there are central connections).
9. Connect the connector to the humidifier (nasal tube - oxygen mask).
10. Test for the presence of oxygen by placing the tip of the catheter in a cup of water (bubbles appear).
11. Connect oxygen to the patient.
12. Monitor the patient’s breathing condition and implement the doctor’s instructions.
13. Register in the nursing care form to monitor the extent of the patient’s condition improvement.
14. Inform the doctor if any side effects occur.
- B - Specialized work procedures
· Anatomy of the skin and its functions
· Nursing care for a patient with burns
· Burn complications
· Nutrition of a burn patient
· Rehabilitation of a burn patient
· How to treat a burn patient
Anatomy of the skin and its functions
The skin is considered the largest organ in the body and represents about 16% of the body weight, and about 2 square meters of the body area. It consists of three layers, which are:
Skin
Dermis
Fatty layer
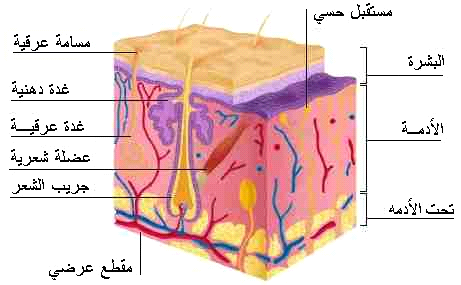
Skin functions: -
1. The skin protects the body from microbes.
2. Maintains body fluids.
3. It regulates body temperature.
4. It manufactures vitamin D.
5. It protects the body from the danger of solar radiation by secreting melanin, which absorbs ultraviolet rays.
6. It contains nerve endings that transmit sensation to the brain.
The general shape of the body is given
Nursing care of a patient with burns
Burns represent one of the most serious injuries to which humans are exposed in developing and industrialized societies. The burn patient remains in the hospital for long periods of time, accompanied by major physiological and psychological changes, such
as suffering from pain, severe pain, fear of death, deformities, separation from the family, immobility, and despair. Which affects the entire body and increases the death rate in burn patients. Therefore, the burn patient needs specialized treatment
to help adapt to the effects resulting from burns, whether physical, psychological, or social. Which shows the importance of the role of nursing with burn victims, as nursing helps the injured adapt to and deal with these injuries and also plays an
effective role towards the patients’ families.

First aid for minor burns:
• Quickly move the injured person away from the fire.
• Remove the watch or any jewelery or jewelry.
• Immerse the burned part in cold water for 10 minutes or until the pain disappears.
• Does not require a hospital.
Educating the patient on how to treat first-degree burns at home
First degree burns, such as minor burns, are treated at home as follows:
Cool the burn site by placing the burned part under cold water, not ice-cold water such as running tap water, or placing the burn site in a bowl of cold water, or by applying cold water compresses to the burn site for 10 to 15 minutes or until the severity
of the pain subsides.
The burn site is covered with a sterile gauze bandage, taking care not to pull the gauze tightly over the burn site to avoid pressure on the burned skin.
A pain reliever is given.
Unless the burns are in large parts of the hands, feet, face, thigh, buttocks, or a major joint in the body, these cases require going to the doctor immediately or to the nearest hospital.
Comments:
Cooling the burn site prevents swelling of the site by stopping more heat from the skin at the burn site.
1. Use cold water to cool the burn site, and do not use ice on the burn site, as it can increase the burn and damage the skin.
2. Place sterile gauze on the burn site and avoid placing cotton or any type of fabric that could stick to the burn site.
3. Do not put egg whites, butter, or toothpaste on the burn site.
4. Follow up on the burn site, as it often heals on its own, but if any signs of infection are observed, such as increased pain, redness, and swelling, or accompanied by a high temperature, a doctor must be consulted.
2- Second degree burn:
It affects the outer and inner layers of the skin, and is characterized by blisters and infiltration under the skin. Healing occurs within 2-3 weeks.
Symptoms:
It is characterized by the appearance of blisters, visible swelling, severe pain, subcutaneous seepage, and plasma exudation through the damaged layers of skin.
First aid for second degree burns
• Keep the injured person away from the heat source.
• Remove any clothing over the burn site.
• Immerse the burned part in cold water to reduce pain (cooling the tissue in this way reduces the heat on the tissues adjacent to the skin).
• Do not use ice or icy water because it causes tissue damage
• The area is then dried with sterile bandages or a cool, ironed cloth.
• Cover the burn with Vaseline gauze and then with a piece of dry bandage. Be careful not to remove the burned tissue or attempt to puncture it.
• The bandage is changed every 1-2 days or if it is wet with plasma fluid.
• Notice signs of infection, such as high temperature, unexplained pain, and the presence of pus.
• Second-degree burns of the face and neck or more than 3 cm require medical intervention.


(1) Third degree burn:
It affects all layers of the skin, and can affect tissues beneath the skin, such as muscles and bones, leading to the affected person losing the feeling of pain in the burned area as a result of damage to the sensory nerves and charring of the skin.
In third degree burns, the burn site appears waxy white or blackish. The injured person does not feel the burn due to damage
Nerve extremities. Pain after the occurrence



Do not remove clothing from the burn site so as not to tear the skin.
Do not apply cold water or medication to the burn.
Apply a clean, damp piece of gauze.
Rush him to the hospital.
If the injury is to the foot or hand, raise it higher than the level of the heart to “ease the blood flow.”
If the burning is on the face, watch if he has difficulty breathing.
(1) Fourth degree burns: -
Fire burns result from people who are in a coma and cannot stay away from the fire, during explosions, or from lightning or high-voltage electrical burns. These burns are treated with amputation of limbs and major cosmetic operations on the rest of the body’s organs.
Secondly, burns are divided according to the area of the affected part:
1- Minor burn: which affects less than 15% in adults and 10% in children.

- Moderate burns: This is a burn rate of 15-25% in adults, and 10-20% in children.
3- Severe burn:
These are burns that include the head and surrounding burns that include the limbs, chest, genital area, and joints. The injured person must go immediately to the burn center to receive the necessary treatment.
Throat and Airways Burns: - They result from inhaling caustic and burning fumes, hot water vapor, heated dry air, or hot and toxic fire fumes. This often occurs in closed, poorly ventilated spaces. Sometimes burns in the mouth, throat, and respiratory tract occur from drinking a chemical substance. Committed by mistake, as in children, or intentionally, as in incidents of assault or suicide, as a result of psychological disorders.
Symptoms and signs of burns affecting the throat and respiratory tract
When the respiratory tract or the throat and mouth area are affected by burns, we notice the following:
· Pimple or black spots around the mouth, or signs of burning of the lips.
· Noticing burn lesions on the head, face, or around the neck.
· Feeling a scratchy feeling in the throat or a burning pain sometimes.
· Change in tone of voice.
· Breathing difficulty.
· Bouts of annoying cough.
· Noticing the presence of burnt hair blades on the nose or eyebrows.
· Mucus coming out of the nose that is speckled with carbon and dark in colour.

Burn complications:
Loss of blood serum (plasma)
Loss of body fluids
Body tissues are destroyed
Choking
Rule of Nines:
According to this rule, the body is divided into parts, and a percentage is given for each part, which is 9%. This is to give a quick estimate at the scene of the accident of the area of the injury.
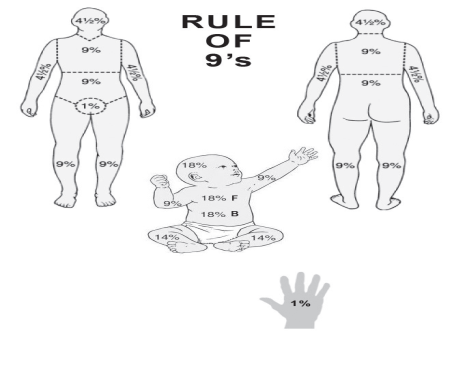
The body is divided as follows
. Head=9%
. Right arm = 9%
. Left arm = 9%
. Front part of onyx = 18%
. (chest = 9%, abdomen = 9%)
. Posterior part of onyx = 18%
. (back = 9%, seat = 9%)
. The front part of each lower limb = 9%
. Posterior part of each lower limb = 9%
. Genital area = 1%
. Degree of risk
The American Burn Association has devised a classification system to determine whether or not a patient needs to be referred to a specialized burn unit. Burns can be classified according to this system into severe, moderate and minor. This is estimated based on a number of factors, including the total area of the body affected, whether it covers specific anatomical areas, the age of the affected person, and associated injuries. Minor burns can usually be treated at home, moderate burns are usually treated in a hospital, and severe burns are usually treated at a burn center.
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Risk factors in burns
◼️ Area: The larger the area, the greater the risk (the law of nines). The area of the burned area exceeding 20% for adults and 10% for children of the body area constitutes a risk
◼️ Depth: This depends on the degree of burn, as the third degree is more dangerous than the second.
◼️ Location: The face, hands, chest, and genital area are considered one of the most dangerous places on the body. This is due to its sensitivity and the fact that it contains nerves and blood vessels
◼️ Age: Children and the elderly (due to weak immunity).
◼️ The general health condition of the injured person
Objectives of the burn first aid operation:
◼️ Alleviate and eliminate pain (by cooling to relieve fever)
◼️ Preventing dirt and contamination of the burner
◼️ Treating trauma
First aid for major burns
• If the injured person’s clothes are on fire, place the injured person on the ground, lying on his back, and cover the injured person with a blanket or rug.
• Open the airway and ensure breathing.
• Do not remove anything stuck to the burned part.
• Ointments and non-medicated materials are not applied.
• Do not apply cold or ice water to large areas of burns for fear of shock
• Cover the burned area with clean clothing or clothing to prevent contamination.
• Transfer the injured person to a medical center to provide medical care.
• To prevent shock, the patient is provided with fluids and mineral salts.

Chemical burns: These are burns resulting from the body being hit by some caustic chemical substances, such as concentrated acids or strong alkalis. These burns are characterized by being corrosive, necrotic to the body, and penetrating deeply.
First aid for chemical burns
• Make sure you are safe from burning chemicals.
• Remove clothing over the burned part.
• Remove any watch or accessories that have been exposed to the chemical.
• Wash the burned part with cold water for at least 20 minutes in the case of liquid chemicals, then apply cold compresses to it.
• Remove powdery chemicals with a brush before washing.
• Cover the entire burned area with clean cloth or clothing to prevent contamination.
• Transport the injured person to the nearest hospital if the burn becomes second-degree, or there is severe pain, or the burn extends to the eyes, face, or genitals.

Chemical burns:
These are burns resulting from the body being hit by some caustic chemical substances, such as concentrated acids or strong alkalis. These burns are characterized by being corrosive, necrotic to the body, and penetrating deeply.
First aid for chemical burns
• Make sure you are safe from burning chemicals.
• Remove clothing over the burned part.
• Remove any watch or accessories that have been exposed to the chemical.
• Wash the burned part with cold water for at least 20 minutes in the case of liquid chemicals, then apply cold compresses to it.
• Remove powdery chemicals with a brush before washing.
• Cover the entire burned area with clean cloth or clothing to prevent contamination.
• Transport the injured person to the nearest hospital if the burn becomes second-degree, or there is severe pain, or the burn extends to the eyes, face, or genitals.
• Spreading preventive awareness among children by teaching them safety and prevention methods in using devices, especially those that may be a source of fires. Fire safety rules must also be instilled by teaching them about the sources of danger from fire and informing them about the causes of burns in humans. These educational lessons must be given in Home and school together, and they should be advised to avoid playing with flammable materials such as gas stoves, playing with flammable materials that cause fires such as playing with matches and gasoline, lighting fireworks, playing with broken electrical appliances, playing with exposed electrical wires, placing conductive materials in electrical sockets, or playing Burning candles and many more.
• All human categories, including citizens, workers, and students, must be trained in the work of extinguishing fires in correct ways based on scientific foundations, and this must be done from time to time, and the authorities specialized in fires and burn treatment, such as the Civil Defense, the Red Crescent, and hospital emergency departments, must hold regular, supported practical training courses. By giving awareness lectures to make people understand the causes of fires, ways to combat them, and ways to prevent their occurrence or limit their spread, as well as teaching them how to deal with burns and administer first aid to the injured, to save their lives, prevent complications from occurring to them, and alleviate their terror and pain, before specialized medical services arrive.
• Strict laws must be enacted to impose the placement of stairs and emergency doors in every residential or commercial building, to be used for escape when fires occur.

◾ Do not use cotton directly to cover wounds, as it will stick to the burn | ◾ |
Burn complications
A- Rapid complications:
These are complications that occur within the first 72 hours of the burn
- Imbalances in body fluids and salts.
- Circulatory system disorders.
. Lack of oxygen reaching the cells
. Acute kidney failure due to lack of body fluids -
. - Irreversible visual impairment, and permanent blindness may occur as a result of not giving fluids in sufficient quantities
. Nervous shock due to pain -
. Hemorrhagic shock due to fluid loss
Complications with average time to occur:
These are complications that do not occur quickly or are late, and they occur after 72 hours of the burn until the burn heals
. Respiratory complications and infections
. Gastrointestinal complications. Urinary system complications -
. Osteitis usually occurs when there are injuries associated with fractures.
. Eye and ear infections-
. Liver diseases-
. Skin diseases-
. The presence of bacteria in the blood and blood poisoning -
. - Anemia due to the breakdown of red blood cells and because the bone marrow stops generating red blood cells due to infections.
- Late complications:
These are complications that occur after recovery, including:
. The appearance of skin scars and deformities
. Severe skin discolouration
. The appearance of bubbles in the healed burned area.
. The possibility of the burn occurring again, in a more severe form.
Other complications:
- It may occur quickly or moderately
. Fatty thrombus-
. Abortion for pregnant women-
Alarm
The prognosis of burns is poor in older burns, the elderly, and females. Smoke inhalation, other injuries such as fractures of long bones, and the presence of other serious diseases (such as heart disease, diabetes, mental illness, and suicide attempts) also affect the prognosis of the disease.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nutrition of a burn patient
The goal :
. Compensating the lost nutrients as a result of the burn and accelerating the wound healing process
. Balancing energy and nitrogen
. Increasing the body's immunity to resist any germ that enters through the wound
Dietary modifications: -
Dietary modifications depend on
. Patient age: Children, infants and the elderly are more susceptible to burn complications.
. Nutritional status of the patient before the burn.
Nutritional requirements:
Nutritional needs for adults and children who are sick are calculated according to the following: Energy
The energy required for the patient is calculated according to the following equation
From 16-59 years old
Energy = ]25 calories x the patient’s weight before burning (kg) [+ ]40 calories x % area
burned from the body)
Age 60 and above
Energy = (20 calories x patient’s weight before burning (kg) + 65 calories x % of body area burned)
** Important note:
If the burning percentage is more than (50%) of the body area, do not calculate more than (50%) in the equation to avoid overestimating the daily calorie needs.
Age 0 to 15 Energy is calculated as follows
From 0-1 years = (recommended basic daily needs).
15 calories x (% of body area)
From 1-3 years = (Recommended Basic Daily Needs per day + 25 calories x % of body area) From 4-15 years = (Recommended Basic Daily Needs per day + 40 calories x % of body area
Protein
If the burning percentage for adults and children is more than (10%) of the body area, the amount of protein is estimated to be equivalent to (20%) of the total estimated calories for adults and children.
Equivalent to (2 grams of protein/kg) of the patient’s weight/day
If the body burns (1-10%), the amount of protein is estimated at (15%) of the total daily calories.
For children under one year of age, the amount of protein is estimated at (3-4 gm/kg) of the child’s weight, due to the child’s inability to tolerate a high amount of salt.
Fats
The amount of fat is estimated to be equivalent to (10-15%) of the total estimated daily energy, with (5%) of these needs being linoleic acid.
Carbohydrates
The daily requirement of carbohydrates is estimated as follows:
For adults; Daily needs are calculated with the following equation:
5 mg glucose/kg body weight/minute.
*For children: The percentage of carbohydrates should be (50-55%) of the total calories
daily, and for children fed by parenteral nutrition (65-70%) of their total calories can be from carbohydrates.
Other factors that require adjusting the patient's nutritional needs:
. Other injuries such as (fractures and inhalation of fumes)
. The presence of a chronic disease (such as diabetes, high blood pressure)
. Nutritional status before burning (such as obesity, malnutrition, taking certain medications, drinking alcohol, and severe weight loss as a result of a certain disease)
. Patient's age (patients under 2 years old or over 60 years old are more exposed to health risks than other age groups)
. Size and depth of burn
. Signs of inflammation or the presence of bacteria in the blood (such as a positive blood culture result, high temperature and high blood sugar)
Start feeding
There are standards that must be paid attention to when starting to bring food to the patient after a burn. These standards include: age, percentage and location of the burn, the estimated amount of protein and calories for the patient, the ability to take food orally, the health status of the digestive and respiratory systems, fluids in the body, and nutritional status. For the patient, the surgical plan for treating the burn.
Oral food
A high-protein, high-calorie diet is prescribed for a patient who can eat normally. The diet includes additional meals and nutrient-concentrated foods taken as fortified meals. Nutritional formulas can be added in addition to meals. Food can also be used through a tube in the evening for patients who are unable to eat. Their nutritional needs.
- Food through a feeding tube
Tube feeding is prescribed for patients who are unable to take their nutritional needs orally and have a well-functioning digestive system. Tube feeding is an essential procedure for feeding patients with severe third- and fourth-degree burns. The sooner the patient is fed, the better and faster the results will be.
- Nutrition intravenously
Intravenous nutrition is prescribed for patients who suffer from poor bowel function, suffer from severe diarrhea, are unable to tolerate tube feeding for more than 2-3 days, or suffer from gastrointestinal diseases such as stomach or duodenal ulcers as a result of psychological stress, and burn patients ( Curling Ulcers) or pancreatitis.
Burns are considered one of the most damaging accidents or wounds on the body’s systems and tissues, as they lead to:
first degree:
These are minor burns in which the surface area of the burned body is less than 15-20% of the body area in the case of adults and 10% in the case of children.
As for the second degree of burns:
These are those in which the percentage of burned areas exceeds 20% of the body area.
In this case, the commander needs to quickly take care of the patient’s nutritional intake, and this can be done gradually to the next three stages
Stages of nutritional intervention
Nutrition during the first stage:
It usually occurs within the first 24 hours of the burns occurring.
The characteristics of this stage are:
1- The body loses a significant amount of its fluids through wounds and burns.
2- The amount of urine is less than normal.
3- Blood volume decreases, which may cause nervous shock.
4- The occurrence of edema at burn sites.
5- The blood becomes more acidic as a result of the accumulation of hydrogen and the release of bicarbonate ions from the blood.
Therefore, the goals of nutritional care at this stage are:
Correcting these disorders by supplying the body with abundant amounts of glucose, amino acids, and bicarbonate ions, and replacing lost fluids and mineral elements. It is usually preferable to feed such patients through a tube because the possibility of blood poisoning is higher in the case of intravenous feeding compared to tube feeding.
Nutrition during the second stage
It occurs two or three days after the burns occur, and this stage is characterized by the following:
1- Stops the breakdown of fatty and muscle tissue
2- The amount of urine produced returns to its normal level.
3- Achieving balance in the body’s fluid contents and essential nutrients.
To achieve this with:
4-Ensuring the provision of appropriate amounts of nutrients necessary to rebuild damaged tissue
And speedy wound healing.
5- To encourage the formation of autoimmune means.
The patient's nutritional needs must be carefully calculated.
Nutrition during the third stage:
At this stage, the patient does not need any additional foods as indicated. The metabolic factor has returned to its normal level, and most of the affected areas may have been covered with new tissue. However, it is important to ensure that the patient's diet is balanced in terms of quantity and quality.
Rehabilitation of burn patients
Modern rehabilitation for burn injuries is based on the principle of comprehensive care for all aspects of physical, psychological and social injury. It requires a rehabilitation team and is generally divided into two stages:
Acute phase
Which begins from the first day of burning and focuses on three priorities:
1. Orbit of motion exercises to maintain joints.
2. Placing the body and limbs in correct positions and using splints if necessary to prevent deformities, as the patient usually takes positions that are comfortable for him, and these positions often cause deformities.
3. Begin forming a sound professional relationship with the patient and his family, as this will have positive effects on the long-term rehabilitation program in the future.
In this acute stage, all obstacles to movement must be taken into account, especially pain and the presence of medical devices, solutions, spare parts and surgical interventions, so that the rehabilitation program does not conflict with the therapeutic program.
Chronic phase
The objectives of this stage are mainly to focus on functions and reintegration. This requires taking care of wounds, scars and their deformities, using special massage methods for this, as well as the use of compression girdles and silicone. The goals of the program are
1. Continue with range of motion and stretching exercises
2. The patient begins active exercises to move according to his ability and begins strengthening exercises gradually
3. Reducing swelling because it limits movement
4. Begin training on daily job tasks
Psychological and social support plays a major role at this stage of treatment, because burns are injuries that leave visible effects on the body, and the resulting psychological disturbances on the patient and his surroundings may limit his chance of reintegration into society if they are not taken into account in the rehabilitation program.
How to treat a burn patient
Treatment :
In order to prepare an appropriate treatment program, it is necessary in the first stage to conduct an assessment of the severity and seriousness of the injury, the extent of the burn’s spread, and the size of the affected areas.
The depth of the burn can be evaluated according to the color of the skin in the affected areas, the length of time during which the injured person was exposed to the cause of the burn, and of course the type of cause of the burn.
The size of the affected areas is evaluated according to the law of nines, as:
Head and neck - 9%, stomach and chest - 18%, back - 18%, 9%, each arm - 18%, each leg and pubic area - 1%.
If there is suspicion of smoke inhalation, the evaluation also includes performing an imaging of the chest area and endoscopy in order to determine whether the respiratory tract and lungs have been damaged. The medical evaluation also addresses the patient's health condition and age.
Medical treatment includes the following:
If the patient loses a large amount of fluid, he is given intravenous fluids, cleaning the burn, treating with antibiotics to prevent the spread of infection, using pain relievers, and dressing the burn. In bad cases, a surgical operation is performed during which the damaged layer is removed and skin tissue is transplanted in its place.
When redness, swelling, or severe pain appears in the burn area following the burn, and the burn does not heal within several weeks, the injured person must go to the doctor.
Treatment efforts are focused on preventing shock and microbial contamination or poisoning, such as an adult who has a burn area of 15% of his body surface and a child who has a burn area of 10%.
From the surface of his body, wherever the burn is, he must be admitted to the hospital and provided with intensive health care:
1- Treating the shock resulting from fear and intensity of pain by calming the patient, reassuring him, and giving him pain-relieving medications such as morphine and bathidine.
2- Remove the clothes, clean the burn with sterile water, and give a full body bath after shaving the hair
3- Various tests are taken, such as blood, urine, and areas of skin for transplantation
4- Giving the teatone serum.
5- Respiratory care
6- Giving intravenous fluids, especially ringer lactate, and the quantity is calculated as follows
The first 24 hours of burning
7- Monitoring the patient in terms of vital signs, estimating the surface area of the burn, checking for accompanying wounds and injuries, and evaluating general health.
8- A catheter is placed inside the bladder to collect urine and monitor the inside and outside
. Local burn care by cleaning the burn with medical soap.
Treating burns (making dressings): There are 3 ways to treat burns:
A- The open method is based on the principle that dryness of the burn area prevents the proliferation of germs. This method is done by applying cream or antibiotics to the patient and not applying any layer of gauze
Advantages of the open method:
Needs less and simpler nursing care
Easily monitor the burn site, examine it easily, and detect infections
Early possibility of caring for a large number of patients at once
The patient does not suffer from pain and does not require many tools
One of the disadvantages of this method
The injured person is exposed to cold.
Difficulty controlling pollution and infections.
Bed soiling
B - The semi-open method: This method is used for moderate and serious burns. It is done by kneading a single layer of gauze with medical cream (Safratol) and sticking it over the burn. The change is repeated every 24 hours.
Advantages of this method:
It keeps the wound clean during the treatment period.
One of the disadvantages of this method
It requires special skills and a sufficient number of people with this skill
Closed method:
It is based on the principle that 90% of the burn area is sterile immediately after the burn, so the burn is covered for 2-10 days without changing after applying a layer of medical cream and a thick layer of gauze.
Among the advantages of this method: .
1. It reduces the amount of fluid seeping from the burned surface.
Among the disadvantages of this method: -
1. Not monitoring the burn daily
2. Susceptibility to infections
3. The occurrence of pus
4. Converting a burn from a partial burn to a complete burn
5. It is not used in specialized burns departments
2) Surgical treatment of burns
Wounds requiring surgical closure should be treated with patching (usually in any case larger than a burn).
Circumferential burns in the extremities and chest may require urgent surgical intervention to loosen the skin. This is done to treat or prevent peripheral circulation problems or ventilation problems. Its effectiveness in neck and finger burns has not been proven. Electrical burns may require fasciotomy.
3) Exceptional methods of treatment:
Transplanting skin removed from another patient on the verge of death: -
As a result of an accident, heart disease, or something else. In this case, the skin is removed, and the heart, kidney, or other organs may also be removed. Skin is transplanted in place of another patient's burned skin in cases where the burns extend over large areas and there is not enough healthy skin left to complete the transplant surgery in third-degree burns. However, the affected person usually sheds this foreign skin after about 3 weeks due to its unsuitability. However, during this period, the condition of the burned patient may have improved, or the doctor may have been able to remove some of the healthy skin, or even benefit from the second technique of creating skin in the laboratory.
- Medicines and solutions
Medications used in the unit: -
Adrenaline
Atropine
Dopamine
Xylocaine
Sodium bicarbonate
Solutions used in the unit:-
Salt solution
Solution C 5%
Solution C 10%
Solution C 25%
Ringer's solution
Sodium bicarbonate
Potassium chloride
Blood
Plasma
Famine
Intralibid
Medicines and solutions used in the burn unit
Adrenaline
Cardiovascular stimulant
Dosage:
According to doctor's orders
Nurse's role:
Note the side effects
Tremors - vomiting - headache - sweating - yellowing - fear - increased heart rate - chest pain, and you must inform the doctor immediately.
Atropine
It is used in cases of low heart rate
Dosage:
According to the doctor's order
Side effects :
Dry throat - dilated pupils - high temperature - lack of concentration - hallucinations
Nurse's role:
It should be given with caution under the supervision of a physician, especially in cases of:
Low blood pressure - inability to breathe - electrical muscle disturbance in the heart.
Dopamine
It is used in cases of decreased blood circulation - heart enlargement
Dosage:
According to doctor's orders
Side effects :
Irregular heartbeats - feeling the heart beating strongly - low blood pressure - nausea - vomiting - headache
The role of the nurse:
Do not add to alkaline solution (sodium bicarbonate).
Place the patient on the monitor
Make a fluid map
Xylocaine
Antiarrhythmic, local anesthetic
Dosage:
Intravenously, 100 ml initial dose, then 1-2 g/500 mg 5% glucose at a speed of 1-4 mg/min. And according to the doctor's orders
Side effects :
Reduction of Blood pressure
Severe decrease in blood circulation
Cramps
Sodium bicarbonate
It is used to treat acidity in the body, an example of which is diabetic coma, and it is used according to blood gas analysis
Nurse's role:
It is not given with calcium solution
Note the occurrence of alkaline activity:
(Vomiting - diarrhea - weak breathing - lack of concentration - agitation - tremors)
Solutions used in the burns unit: -
Salt solution:
It is used in cases of lack of fluids in the body and after the operation
Solution C 5%: acute decline in blood circulation and cases of diabetic coma with insulin
Solution C 10%: acute decline in blood circulation and cases of diabetic coma with insulin
25% solution: It is used in cases of post-concussion and diabetic coma resulting from low blood sugar.
Ringer's solution: in cases of fluid deficiency
Sodium bicarbonate: It is used in cases of excess acidity in the body (cardiac and respiratory arrest).
Potassium chloride: in cases of potassium deficiency
Blood: Whole (red cells - platelets - plasma - clotting parameters) and is used in cases of shock due to fluid deficiency. Bleeding, decreased coagulation factors
Plasma: in cases of burns and protein deficiency in the body
Famine: It contains amino acids and proteins and is given in cases of severe protein deficiency, coma cases, and major surgical operations (not eating for a long time).
Intralipid: It is a solution containing fatty acids that the body needs (in cases of complete coma - in cases of cholesterol deficiency).
- Medical terms
A-general medical terminology
B-medical terminology of the burns department
C-abbreviations
الكلمة | الترجمة | الكلمة | الترجمة |
أوضاع الجسم | Body Position | تجاویف الجسم | Body Cavities |
الوضعیة التشریحیة | anatomical position | التجویف الباطني | Abdominal cavity |
وضعیة الإستلقاء | decubitus position
| التجویف القحفي | Cranial cavity |
وضعیة الإستلقاء الظھري | dorsal recumbent | التجویف الحوضي | Pelvic cavity |
وضعیة فاولر | Fowler position | التجویف النخاعي | Spinal cavity |
وضعیة ترندلبورج | trendelenburg position | التجویف الصدري | Thoracic cavity |
أصناف الامراض | Disease Categories | وصف المرض | Description of Disease |
الأمراض الإنحلالیة | Degenerative Diseases | حاد | Acute |
الاِضطرابات الھورمونی | Hormonal disorders | حمید | Benign |
الاِضطرابات المناعیة | Immune disorders | سرطانى | Carcinoma |
الأمراض المُعدیة | Infectious Diseases | مزمن | Chronic |
الاِضطرابات العقلیة والعاطفیة | Mental and emotional disorders | السبب | Etiology |
الاِضطرابات الأیضیة | Metabolic disorders | تورم | lesion |
السرطانية الامراض | Neoplastic Diseases | متكيس | Cyst |
احتشاء عضلة القلب | myocardial infarction | ورم | Parasite |
انسداد | occlusion | صبغه ملونه | Gram stain |
القنوات الشریانیة السالكة | Patent ductus arteriosus | التهاب | Inflammation |
التھاب الورید | phlebitis | فتق | Hernia |
السدة القلبية | plaque | امراض الروماتيزم | rheumatic heart disease |
الصمام الأبهرى | aortic valve | الأبهر | Aorta |
صدمة | Shock | جلطه | Thrombosis |
تسارع القلب | tachycardia | تضییق | Stenosis |
قمة | apex | سكتة | Stroke |
شريان | artery | اغماء | Syncope |
الشراين الصغيرة | arteriole | التھاب الورید الخثاري | Thrombophlebit |
العقدة الجيبة الأذينية | atrioventricular (AV) node | الحزمة الأذينية البطينية | AV bundle |
شعيرات دموية | bundle branches | الأذين | Atrium |
جهاز القلب والأوعية الدموية | cardiovascular system | الصمام الثنائى | bicuspid valve |
أصوات القلب | Heart sound | الوريد الأجوف السفلى | Inferior vena cava |
الشريان الرئوى | Pulmonary artery | الصمام المترالى | Mitral valve |
الوريد الرئوى | Pulmonary vein | عدم أنتظام ضربات القلب | Arrhythmia |
الذبحة الصدرية | Angina pectrosis | فشل القلب | Heart failure |
توقف القلب | Heart block | جلطة بالقلب | Myocardial infarction |
أحتشاء فى عضلة القلب | Ischemia | رجفان | Fibrillation |
التهاب بالوريد | Phlepites | جلطات وريدية | Deep venous thrombosis |
تصلب شراين | Athrosclerosis | جلطة | Thromposis |
حادثة وعائية دموية | Cebrovascular accident | تمدد بالأوعية الدموية | Anyorism |
عضلة القلب | myocardium | تجمع سوائل | odema |
الكلمة | الترجمة | الكلمة | الترجمة |
مريض | Patient | العلامات الحيوية | Vital signs |
اسم المريض | Patient name | الضغط | Blood Pressure |
السن | Age | النبض | Pulse |
النوع | Gender | الحرارة | Temperature |
ذكر | Male | التنفس | Respiration |
انثى | Female | الالم | Pain |
الوظيفة | Occupation | غرفة | Room |
الحالة الاجتماعية | Marital History | قسم | Department |
متزوج | Married | العمليات | Operation |
اعزب | Single | الطوارئ | Emergency |
متزوج ويعول | Married with | اقسام الداخلى | In patient |
مطلق | Divorced | العيادات | Clinics |
نعم | Yes | دخول جديد | New admission |
لا | No | خروج | Discharge |
عادات خاصة | Special Habits | وقت | Time |
تدخين | Smoking | تاريخ | Date |
كحوليات | Alcohol | دبلوم تمريض | Diploma nurse |
مرض | Diseases | ممرضة | Nurse |
حساسية | Allergy | طبيب | Doctor |
شكوى | Complaints | قبل الدخول | Before admission |
تعليق | Comment | دخول | Admission |
اجهزة الجسم | Body Systems | بعد الدخول | After admission |
طبيعى | Normal | ادوية | Medications |
غير طبيعى | Abnormal | حالى | Present |
عام | General | العلاج الحالى | Present medications |
ارتفاع | Height | الدواء | Drug |
الوزن | Weight | الجرعة | Dosage |
عينة | Specimen - Sample | عدد مرات | Frequency |
وريد | Vein | الوقت- الفترة | Duration |
شريان | Artery | المظهر العام | General Appearance |
دم | Blood | الجلد | Skin |
تاريخ المرض | Past History | الراس | Head |
محطة تمريضية | Nursing station | توقيع | Signature |
المرض عندالعائلة | Family History | العين | Eyes |
فحوصات الجسد | Physical Examination | الاذن | Ears |
فحص الصدر | Breast examination | الانف | Nose |
تنميل الاطراف | Numbness | الفم | Mouth |
ولادة طبيعية | Normal labor | اسنان | Teeth |
ولادة قيصرية | Cesarean section | رقبة | Neck |
عنق رحم | Cervix | الصدر | Chest |
المخ | Brain | بطن | Abdomen |
تورم | Edema | العظام | Bone |
ازرقاق | Cyanosis | الحالةالنفسية | Psychological Status |
صفرة | Jaundice | التشخيص | Diagnosis |
مرض السكر | Diabetes mellitus | العوامل الخطرة | Risk Factors |
الخطةالتمريضية | Nursing care plan | خطة رعاية | Care plan |
اختناق | Dyspnea | ملحوظة | Notes |
عسر هضم | Dyspepsia | وتر | Tendon |
صعوبة بالبلع | Dysphagia | متابعة | follow-up |
صعوبة فى النطق | Dysphonia | اسباب | Reason |
السابق | Previous | تحاليل المعمل | Laboratory Investigations |
اضطراب فى النوم | Dyssomnia | تخدير | Anesthesia |
صعوبة فى التبول | Dysuria | بدايةالتخدير | Start of anesthesia |
تقييم مجرى الهواء | Airway Assessment | نهاية التخدير | End of anesthesia |
مجرى الهواء | Airway | مساعدة | Assistant |
فصيلةالدم | Blood Group | نوع التخدير | Type of anesthesia |
شمع الاذن | Ear wax | موضعى | Local |
وجع الاذن | Earache | كلى | General |
منظار بطن | Laparoscope | اجراءات | Procedures |
استكشاف بطن | Laparotomy | قبل العملية | Pre-operative |
التهاب الحنجرة | Laryngitis | بعد العملية | Post-operative |
ورم ليمفاوى | Lymphoma | اثناء العملية | Intra-operative |
دم النفس | Lochia | تقييم | Sheet |
وجع فى الظهر | Back pain | تحويل المريض | Referral |
صداع | headache | حساسية | Sensitivity |
جرح | wound | الزهرى | Syphilis |
جرح نافذ | Stab wound | الحنجرة | Larynx |
وريد | Vein | بولينا | Uremia |
شريان | Artery | حصوة المثانة | Bladder Stone |
التهاب الفم | Stomatites | كلي | Kidney |
يعانى من | Suffer from | ارتفاع الضغط | Hypertension |
مضاد حيوى | Antibiotic | انخفاض الضغط | Hypotension |
مضاد الحساسية | Anti-allergic | غيبوبة | Coma |
مضاد للفطريات | Anti-fungal | شبه غيبوبة | Semi coma |
مضاد للفطريات | Anti-parasitic | نزيف من الانف | Epistaxis |
مانع الالتهاب | Ant-inflammatory | نبض سريع | Tachycardia |
مضاد التسمم | Anti-toxic | نبض بطئ | Bradycardia |
مطهر | Antiseptic | منتظم | Regular |
مضاد الحساسية | Antihistaminic | غير منتظم | Irregular |
غيرواعى | Unconscious | شحوب | Pallor |
واعى | conscious | المعدة | Stomach |
مانع لافراز البول | Anti-diuretic | امعاء | Intestine |
مضاد للتسمم | Antitoxic | بول | Urine |
مانع تكون الجلطة | Anti-thrombosis | براز | Stool |
تطبيق عملى | application | جراحة | Surgery |
التهاب مفاصل | Arthritis | شهية | Appetite |
رحمى | uterine | شريان ابطى | Axillary artery |
مهبلى | vaginal | شريان عضد | Brachial artery |
الربو | Asthma | شريان سباتى | Carotid artery |
سماعةالجنين | Fetoscope | شريان فخذى | Femoral artery |
حمى | Fever | سائل | Fluid |
مصاب بالحمى | Feverish | خريطة السوائل | Fluid chart |
غرغرينا | Gangrene | توازن السوائل | Fluid balance |
العقد العصبية | Ganglion | افرازات | Secretion |
جهاز التنفس | Respiratory System | بلغم | Sputum |
الجهاز الدورى | Cardiovascular System | يعصر | Squeeze |
الامعاء والمعدة | Gastrointestinal System | يلاحظ | Observe |
الجهاز التناسلى | Genitourinary System | حمام سرير | Bed bath |
جهازالغدد الصماء | Endocrine System | معايير الجودة | Quality standard |
الجهاز العصبى | Neurological System | التحكم بالعدوى | Infection control |
إستغاثة إنعاش قلب رئوي | Code Blue | تصنيف المرضى | Triage |
- Medical terms and abbreviations
|
|
|
|
Burn |
|
|
Skin - derm |
|
|
Epidermis |
|
|
Dermis |
|
|
Subcutaneous tissue |
|
|
Thermal burn injury |
|
|
Dry Thermal burn injury |
|
|
Moist Thermal burn injury |
|
|
Electrical burn injury |
|
|
Chemical burn |
|
|
Radiation burn |
|
|
Inhalation |
|
|
Carbon monoxide poisoning |
|
|
Respiratory distress |
|
|
First degree of burn |
|
|
Second degree of Burn |
|
|
Third degree of burn |
|
|
fourth degree of burn |
|
|
Minor burn injury |
|
|
Moderate burn injury |
|
|
Major burn injury |
|
|
Rule of nines |
|
|
Extinguish the flames |
|
|
Cool the burn |
|
|
Remove restrictive objects |
|
|
Cover the wound |
|
|
Colloid |
|
Abbreviations
|
AF |
Atrial fibrillation |
|
APB |
Atrial premature beats |
|
APC |
Atrial premature contraction |
|
AV block |
Atrio ventricular block |
|
AV Junction |
Atrioventricular |
|
A-V valve |
Atrio ventricular valve |
|
AVF |
Augmented vector foot |
|
AVR |
Augmented vector right |
|
AVL |
Augmented vector left |
|
CBS |
Catheter By bass surgery |
|
ECD |
Electro cardio Defibrillator |
|
ECG |
Electrocardiography |
|
ID |
Implantable Defibrillator |
|
IVC |
inferior vena cava |
|
LA |
Left atrium |
|
LOC |
Level of Consciousness |
|
NGCP |
Nursing Care Plan |
|
PACS |
Premature atrial contraction |
|
PVC |
Premature ventricular contraction |
|
RA |
Right atrium |
|
SCA |
Sudden Cardiac Arrest |
|
SA node |
Sino atrial node |
|
SND |
Sinus node dysfunction |
|
SVC |
superior vena cave |
|
SVT |
Supra ventricular tachycardia |
|
VF |
Ventricular fibrillation |
|
VT |
Ventricular tachycardia |
|
MI |
Myocardial infaraction |
|
ECG |
Elecrtocardial gram |
|
CPR |
Cardiopulmonary resussitation |
|
DC |
Defibrillator shock |
|
|
|
|
Dreesing |
التغطية |
|
Eschsnial debridement |
إزالة الطبقة السوداء ألياً |
|
Enzymatic depr |
إزالة الطبقة السوداء بالإنزيمات |
|
Surgical depr |
إزالة الطبقة السوداء بالجراحة |
|
Reepithelilization |
نمو الخلايا الحية |
|
Escar |
طبقة الجلد الجافة ( القشرة ) |
|
Debriement |
تنظيف الجرح |
|
Escharotomy |
الشق الجراحى |
|
Nosocomial infection |
العدوى المكتسبة |
|
Hydrotherapy |
الغسل |
Abbreviations
|
AF |
Atrial fibrillation |
|
APB |
Atrial premature beats |
|
APC |
Atrial premature contraction |
|
AV block |
Atrio ventricular block |
|
AV Junction |
Atrioventricular |
|
A-V valve |
Atrio ventricular valve |
|
AVF |
Augmented vector foot |
|
AVR |
Augmented vector right |
|
AVL |
Augmented vector left |
|
CBS |
Catheter By bass surgery |
|
ECD |
Electro cardio Defibrillator |
|
ECG |
Electrocardiography |
|
ID |
Implantable Defibrillator |
|
IVC |
inferior vena cava |
|
LA |
Left atrium |
|
LOC |
Level of Consciousness |
|
NGCP |
Nursing Care Plan |
|
PACS |
Premature atrial contraction |
|
PVC |
Premature ventricular contraction |
|
RA |
Right atrium |
|
SCA |
Sudden Cardiac Arrest |
|
SA node |
Sino atrial node |
|
SND |
Sinus node dysfunction |
|
SVC |
superior vena cave |
|
SVT |
Supra ventricular tachycardia |
|
VF |
Ventricular fibrillation |
|
VT |
Ventricular tachycardia |
|
MI |
Myocardial infaraction |
|
ECG |
Elecrtocardial gram |
|
CPR |
Cardiopulmonary resussitation |
|
DC |
Defibrillator shock |
1- How to remove an electrical burn victim using an electrical insulator

2- Skin components
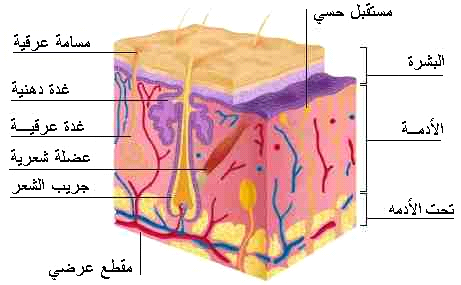
3- degrees of burns
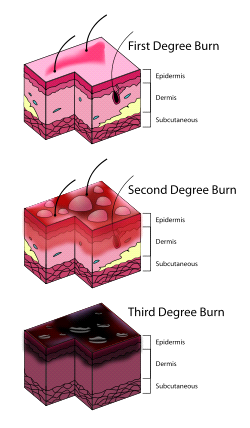
4- rule of nine
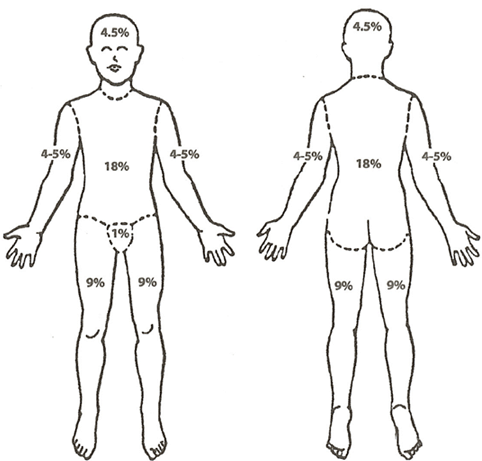
5- Powder bed in the burns department

6- Bathtub for water treatment

7- A patient in the burns department
 t
t


The Reviewer
Nursing procedures manuals were prepared for 2012 and updated for 2017
Guide for nurses working in reception and emergency departments (Central Administration of Nursing)
Guide for nurses working in intensive care departments (Central Administration of Nursing)
Emergency nurses training manual
First aid guide
(The American Hope Project in cooperation with the Egyptian Red Crescent)
Nursing Procedures Quality Handbook
Your guide to the basics and skills of nursing (Egyptian-Korean side)