
Infertility in Cattle
"last update: 25 Sep. 2024"
A) Cystic Ovarian Disease (COD)
- Causes of cystic ovarian disease:
- The actual mechanism leading to the development of cystic ovaries is unknown.
- Hereditary predisposition should put in mind.
It is probably due to:
-- Deficiency of LH released prior to time of ovulation.
-- Imbalance between FSH and LH
-- Lack of GnRH from the hypothalamus.
-- High level of LTH in high milk producing animal.
- Diagnose cystic ovarian disease:
- History of high milking animals of 4–8-year-old, within 3–8 weeks of parturition.
- Symptoms vary from signs of nymphomania with frequent irregular or continuous estrus to anestrum according to type of the cyst present in the ovary. The sexual behavior of the animal shows more bull-like, pawing the ground, bellowing and riding other females. Relaxation of the vulva, perineum, and the large pelvic ligaments, which causes the tail head to be elevated (sterility hump) can occur in chronic cases.
- In rectal examination, ovaries generally are enlarged and rounded; however, their size varies by the number and size of the cysts. Their surface is smooth, elevated, and blister-like. In one or both ovaries there will be
-- Enlarged follicles 2-8 cm in diameter and 1-5 in number.
-- Small cysts in very large numbers
-- Thickened and edematous myometrium with normal size.
- Progetsrone hormone assay: Serum progesterone concentrations can be used to classify luteal (> 0.5 ng/ml) or follicular (≤ 0.5 ng/ml) cysts.
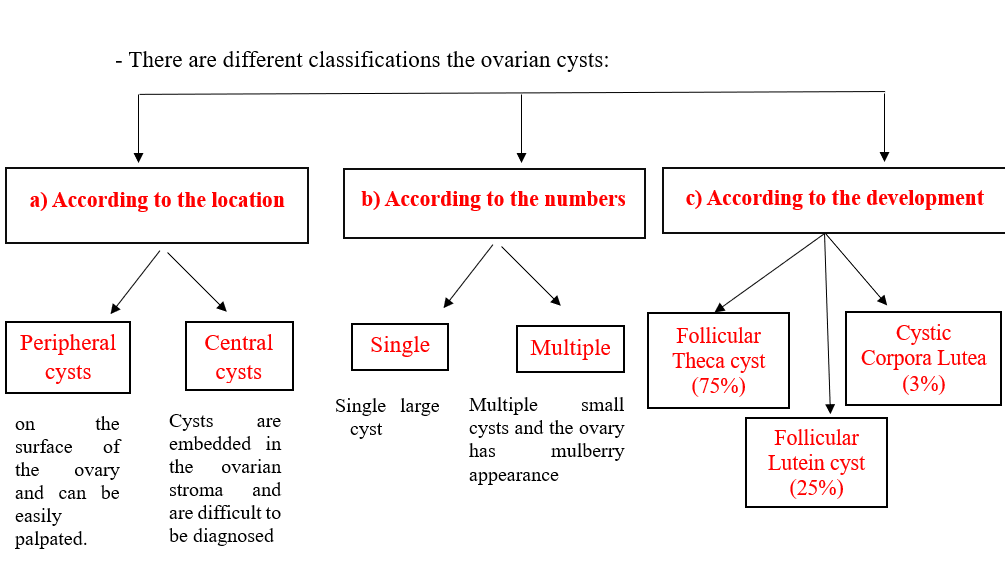
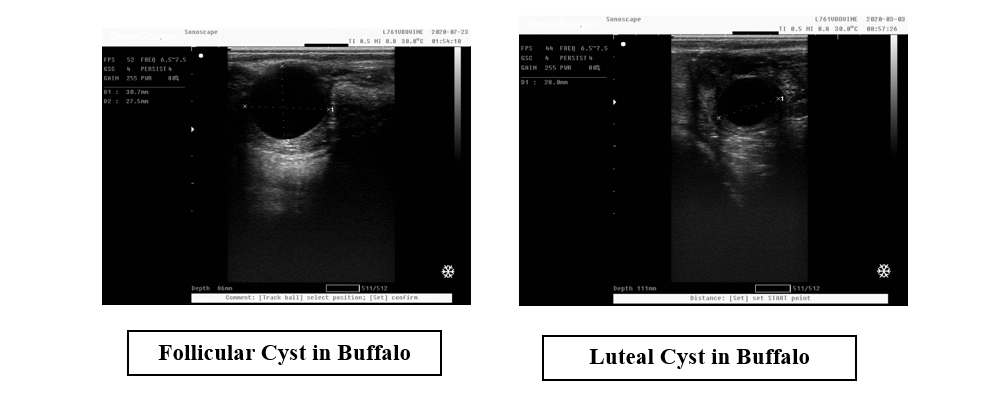
- In ultrasound examination: ultrasound technology is used the accuracy of a correct diagnosis of cyst type was 74% for follicular cysts and almost 90% for luteal cysts. Follicular cysts typically have a thin wall (≤3 mm) whereas luteal cysts typically have a thicker and more echogenic wall (≥3 mm). The follicular fluid is often hypoechoic in follicular cysts, whereas with luteal cysts echogenic strands may be present creating a cobweb-like appearance.
- The vaginal examination reveals that the estrus mucus is opaquer.
- Complications of the ovarian cysts are:
-- Accumulation of abnormal discharge in the uterus.
-- Atrophy of the endometrium after cystic hyperplasia
-- Fragility of bones and their liability for fractures
-- Sterility hump.
- Treatment of cystic ovarian disease:
- The earlier the cystic ovaries are diagnosed and treated, the better is prognosis.
- Large cysts in small numbers tend to respond more readily to treatment than multiple cysts.
- Cystic ovary disease may be refractory to initial treatment.
- Manual rupture of cysts is one method of treating cystic ovary disease; however, the potential danger of traumatizing the ovary and causing hemorrhage with subsequent local adhesions should not be overlooked.
- Medical treatment is directed towards luteinization of the cysts so that the luteal tissue is formed, regressed and the normal cycle is returned.
- Some cysts respond readily to treatment with human chorionic gonadotropin (hCG) at dose of 5000 – 10000 IU.
- Treatment with GnRH (Gonadorelin) at a dose of 100 mcg is effective and less antigenic than treatment with hCG, which may become less effective on subsequent treatments because of the immune response. To hasten the onset of the first estrus after treatment, prostaglandin F2alpha products can be administered 7-10 days after hCG or GnRH.
- The epidural administration of GnRH analogue (e.g., buserelin at a dose of 10 μg) promotes the remission of follicular cysts and an improvement of reproductive parameters.
- Ovsynch (consists of administering GnRH, then the prostaglandin 7 days later, then a second dose of GnRH 48 hours later) have been successfully used to treat cows with cystic ovaries..
- Intravaginal progesterone devices may also be used to treat cystic ovary disease as progesterone upregulates luteinizing hormone receptors before device removal and luteinizing hormone surge.
- Serial ultrasonography guided aspiration of the cystic fluid may provide benefit by removing physiologically active hormones.
