
Deep Neck Space Infections (DNSIs)
"last update: 5 August 2024"
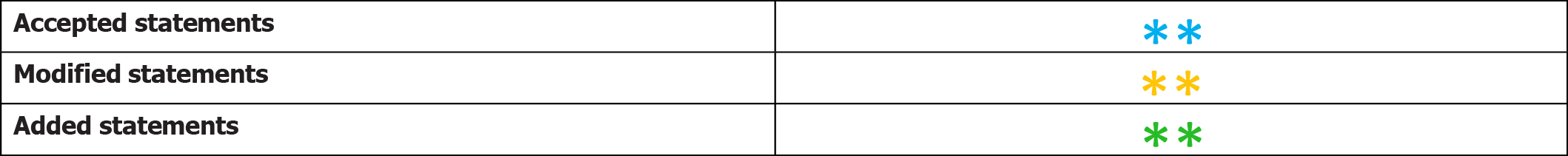
- Recommendations
The following statement and flowchart were adopted/adapted/ from Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology, 2017(1), which had the highest scores as regards the currency, contents and quality.
Recommendations statements
|
Statement topic |
Action recommendation |
Evidence quality |
Strength of Recommendation |
Study type |
Reference |
|
1- Definition
|
Deep neck space infection (DNSI) is defined as infection in the potential spaces and fascial planes of the neck. Early recognition of DNSI can be challenging due to the complex head and neck anatomy; hence, a high index of suspicion is required to prevent a delay in diagnosis and appropriate management. |
Moderate |
Strong recommendation |
Systematic review |
(1) |
|
2. detailed history, physical examination and identification of any immediate or impending airway compromise
|
A detailed history and physical examination are both vital in identifying the presence, source and any complications of infection. The priority in all patients should be the identification of any immediate or impending airway compromise, which should be imminently managed. |
Moderate |
Strong recommendation |
Systematic review |
(1) |
|
3. Aetiology
|
a.Most cases of DNSI are bacterial in aetiology; however, the causative pathogens in the paediatric population differ to those in the adult. Sources in paediatric cases include tonsillitis, pharyngitis, haematogenous and suppurative cervical adenitis compared with adult DNSI, which often have an odontogenic origin. The organisms commonly isolated in DNSIs are Staphylococcus aureus and group A Streptococcus. Anaerobic species include Fusobacterium, Peptostreptococcus and Porphyromonas |
Low |
Conditional recommendation |
Observational study |
(2) |
|
b.Sharp objects may cause perforation of the pharynx or oesophagus and may result in abscess formation in the adjacent neck spaces, such as the retropharyngeal space and should therefore be considered in the history taking and differential diagnosis process. |
Low |
Strong recommendation |
|||
|
4. The management of a DNSI
|
The management of a DNSI is highly dependent on the location and extent of deep neck involvement, and diagnostic imaging is essential in nearly every case. |
Moderate |
Conditional recommendation |
Systematic review |
(1) |
|
5. imaging in DNSI
|
a. Lateral neck radiographs are useful tool for screening of retropharyngeal and parapharyngeal abscesses, Ultrasound more accurate role than CT imaging in differentiating a drainable abscess from cellulitis and can guide diagnostic and therapeutic needle or catheter aspiration of superficial, uniloculated fluid collections when imminent airway compromise is not evident. |
Moderate |
Conditional recommendation |
Systematic review |
(3, 4) |
|
b. Contrast enhanced CT imaging is an accurate and sensitive tool to differentiate a drainable abscess from cellulitis and also significantly contribute to surgical planning to drain deep neck space collections. |
Moderate |
Strong recommendation |
|||
|
c.MRI provides better soft tissue definition than CT and in addition avoids exposure to radiation. However, the time taken to perform MRI, and the nature of the scanner, often means that a general anaesthetic is required for this investigation in pediatric population. Magnetic resonance angiography (MRA) is used to evaluate potential vascular complications, such as IJVT and carotid artery aneurysm or rupture. |
Moderate |
Conditional recommendation |
|||
|
6.Medical treatment in DNSIs
|
a.All patients with a DNSI should be given initial empiric antibiotic therapy (even if the patient is also being managed surgically) until culture and sensitivity results are available and advised that therapy should be effectively targeted against the aerobic and anaerobic bacteria. |
Low |
Strong recommendation |
Systematic review |
(5) |
|
b. Either penicillin in combination with a ß-lactamase inhibitor (such as amoxicillin with clavulanic acid) or a ß-lactamase–resistant antibiotic (such as cefoxitin, cefuroxime, imipenem or meropenem) in combination with a drug that is highly effective against most anaerobes (such as clindamycin or metronidazole) is recommended for optimal empiric coverage. |
Low |
Strong recommendation |
|||
|
7. Surgical drainage of DNSIs
|
a. Indications for surgical drainage include airway compromise, septicaemia, complications, extending or descending infection or no clinical improvement within 48 hours of the initiation of IV Antibiotics abscess >2.2 cm on CT imaging. |
Low |
Strong recommendation |
Observational study |
(6, 7) |
|
b. An external cervical approach is required for submandibular, prevertebral and carotid space infection. Parapharyngeal abscesses that are not obviously ‘pointing’ in the pharynx and complicated retropharyngeal abscesses that cannot be fully drained using an intraoral approach also require an external approach. |
Low |
Strong recommendation |
|
|
|
|
8. Minimally invasive techniques in DNSIs
|
Minimally invasive techniques such as image-guided needle aspiration of abcesses measuring <3 cm in diameter, and ultrasound-guided catheter placement for unilocular abscesses measuring >3 cm in diameter, extending into deep neck spaces or located within a glandular structurehave been used to treat well-defined, unilocular abscesses in patients who do not have airway compromise. |
Low |
Strong recommendation |
Observational study |
(6, 7) |
|
9. Acute airway obstruction
|
Acute airway obstruction is one of the most alarming complications of DNSI. It is commonly encountered in Ludwig’s angina and is a significant risk with a retropharyngeal abscess due to the potential for rupture into the airway leading to aspiration in addition to potential airway obstruction. Most cases are successfully managed with endotracheal intubation. Rarely, and in severe cases, intubation with general anaesthesia may be difficult and may precipitate complete airway obstruction that necessitates an emergency tracheostomy. |
Moderate |
Strong recommendation |
Systematic review |
(3) |
|
10. Monitoring of the airway in DNSIs
|
Monitoring of the airway is a priority when managing DNSI patients and should continue for at least 48 h after surgical intervention because of the potential for increasing oedema in the postoperative period. The routine use of intravenous steroids in patients who have impending airway obstruction has been advocated with the aim of minimising oedema and thereby reducing the need for aggressive airway intervention. |
Moderate |
Strong recommendation |
Systematic review |
(3) |










