Deep Neck Space Infections (DNSIs)
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Deep Neck Space Infections (DNSIs) |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:34 PM |
Description
"last update: 5 August 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdelaziz,6 Tarek Ghannoum,7 Mahmoud Yousef8
Assembly Board: Eslam farid Abu shady 11, Mohammed Roushdy 9, Mohamed El rabiee 13, Mostafa Ammar 6
Grading Board (In alphabetical order): Ahmed Abdel Fattah,10 Hazem Abdel Tawab,1 Heba Abo Elnaga,2 Sherif Askar,12 Khaled Dahy,13 Ahmed El Batawi,1 Ahmad Eltelety,1 Ibrahim Khaled,12 Yaser Khalil,2 Emad Shehata,6 Mohamed Zahran14
Reviewing Board: Ali Tawfik,5 Mohamed Hegazy,1 Abdellatif Elrashidy2
Other related specialties Reviewing Board: Engy Adel Asker15.
1Otorhinolaryngology Department Faculty of Medicine/Cairo University, 2Otorhinolaryngology Department Faculty of Medicine/Menoufia University, 3Otorhinolaryngology Department Faculty of Medicine/Minia University, 4Otorhinolaryngology Department Faculty of Medicine/ Beni-Suef University, 5Otorhinolaryngology Department Faculty of Medicine/Mansoura University, 6Otorhinolaryngology Department Faculty of Medicine/Tanta University, 7Audiovestibular Unit, Otorhinolaryngology Department Faculty of Medicine/Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department Faculty of Medicine/Ain Shams University, 9Otorhinolaryngology, Department Faculty of Medicine / Assuit University, 10Otorhinolaryngology Department Faculty of Medicine / Al Azhar University, 11Otorhinolaryngology Department Faculty of Medicine / Banha University,12Otorhinolaryngology Department Faculty of Medicine / Zagazig University, 13Otorhinolaryngology Department Faculty of Medicine / Sohag University, 14Otorhinolaryngology Department Faculty of Medicine / Alxandria University, 15 Head nurse at Tanta University Hospitals.
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Acronyms and Abbreviations
DNSI Deep neck space infection
- Executive Summary
|
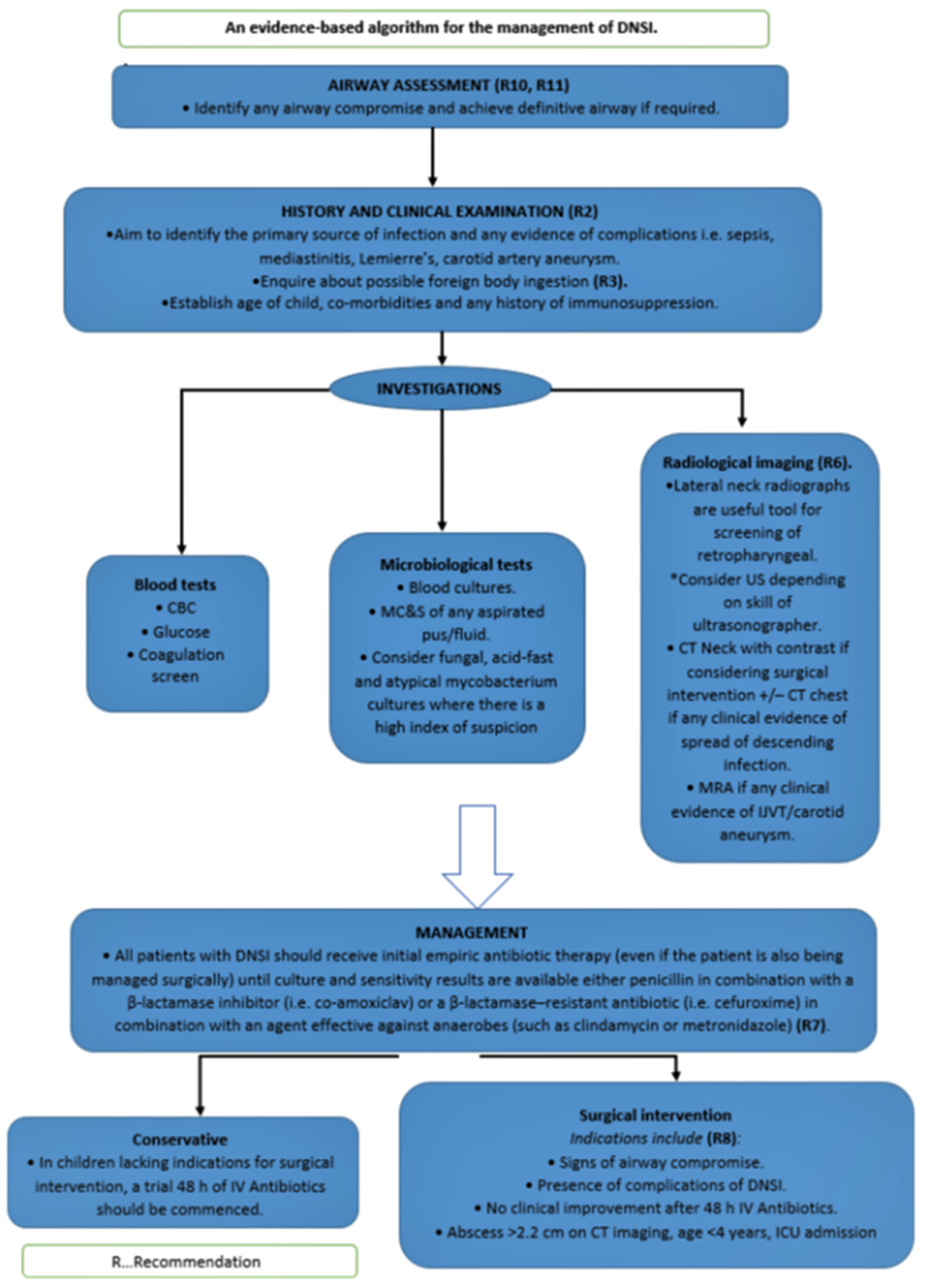
The following statement and flowchart were adopted/adapted/ from Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology, 2017, which had the highest scores as regards the currency, contents and quality. 2- detailed history, physical examination, and identification of any immediate or impending airway compromise: A detailed history and physical examination are both vital in identifying the presence, source and any complications of infection. (Strong recommendation) 3- Aetiology: a. Most cases of DNSI are bacterial in aetiology; however, the causative pathogens in the paediatric population differ to those in the adult. Sources in paediatric cases include tonsillitis, pharyngitis, haematogenous and suppurative cervical adenitis compared with adult DNSI, which often have an odontogenic origin. (Conditional recommendation) b. Sharp objects may cause perforation of the pharynx or oesophagus and may result in abscess formation in the adjacent neck spaces (Strong recommendation) 4- The management of a DNSI: The management of a DNSI is highly dependent on the location and extent of deep neck involvement (Conditional recommendation) 5- imaging in DNSI: a. Lateral neck radiographs are useful tool for screening of retropharyngeal and parapharyngeal abscesses (Conditional recommendation) b. Contrast enhanced CT imaging is an accurate and sensitive tool to differentiate a drainable abscess from cellulitis (Strong recommendation) c.MRI provides better soft tissue definition than CT and in addition avoids exposure to radiation. (Conditional recommendation) 6- Medical treatment in DNSIs: a. All patients with a DNSI should be given initial empiric antibiotic therapy (even if the patient is also being managed surgically) until culture and sensitivity results are available (Strong recommendation) b. Either penicillin in combination with a ß-lactamase inhibitor (such as amoxicillin with clavulanic acid) or a ß-lactamase–resistant antibiotic (such as cefoxitin, cefuroxime, imipenem or meropenem) in combination with a drug that is highly effective against most anaerobes (such as clindamycin or metronidazole) is recommended for optimal empiric coverage. (Strong recommendation) 7- Surgical drainage of DNSIs: a. Indications for surgical drainage include airway compromise, septicaemia, complications, extending or descending infection or no clinical improvement within 48 hours of the initiation of IV Antibiotics abscess >2.2 cm on CT imaging. (Strong recommendation) b. An external cervical approach is required for submandibular, prevertebral and carotid space infection. Parapharyngeal abscesses that are not obviously ‘pointing’ in the pharynx and complicated retropharyngeal abscesses that cannot be fully drained using an intraoral approach also require an external approach. (Strong recommendation) 8- Minimally invasive techniques in DNSIs: Minimally invasive techniques such as image-guided needle aspiration of abcesses measuring <3 cm in diameter (Strong recommendation) 9- Acute airway obstruction: Acute airway obstruction is one of the most alarming complications of DNSI. It is commonly encountered in Ludwig’s angina and is a significant risk with a retropharyngeal abscess due to the potential for rupture into the airway (Strong recommendation) 10- Monitoring of the airway in DNSIs: Monitoring of the airway is a priority when managing DNSI patients and should continue for at least 48 h after surgical intervention (Strong recommendation) |
- Introduction, scope and audience
➡️Introduction and background
Deep neck space infection (DNSI) is defined as infection in the potential spaces and fascial planes of the neck. Early recognition of DNSI can be challenging due to the complex head and neck anatomy; hence, a high index of suspicion is required to prevent a delay in diagnosis and appropriate management.
➡️Scope
to identify quality improvement opportunities in the management of DNSIs and to create explicit and actionable recommendations in the clinical practice.
➡️Target audience: Target users are ENT clinicians and specialists and residents to be used for the management of patients present with deep neck space infection (DNSI- Methods
➡️Stakeholder Involvement: Individuals who were involved in the development process. included the above-mentioned Head and Neck Chief Manager, Head and Neck Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences, views and preferences were applicable for this topic.
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing and Other related specialties Reviewing Board including a nurse.
➡️Search sources included other previous guidelines:
Pubmed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar
➡️Search sources included other previous guidelines:
▪️ Tonsillitis, tonsillectomy, and deep neck space infections in England: the case for a new guideline for surgical and non-surgical management,2021.
▪️ Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology, 2017.
Time periods searched: from 2017 to 2021.
➡️Results
Three guidelines were assessed by 4 experts Laryngologists and Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology, 2017had the highest scores as regards the currency, contents, and quality. It was graded GRADE by 11 expert Laryngologists and reviewed by 3 expert reviewers. (Annexes tables 1-3) [1].
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policymaking will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed. Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
[2] http://www.gradeworkinggroup.org.
- Recommendations
The following statement and flowchart were adopted/adapted/ from Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology, 2017(1), which had the highest scores as regards the currency, contents and quality.
Recommendations statements
|
Statement topic |
Action recommendation |
Evidence quality |
Strength of Recommendation |
Study type |
Reference |
|
1- Definition
|
Deep neck space infection (DNSI) is defined as infection in the potential spaces and fascial planes of the neck. Early recognition of DNSI can be challenging due to the complex head and neck anatomy; hence, a high index of suspicion is required to prevent a delay in diagnosis and appropriate management. |
Moderate |
Strong recommendation |
Systematic review |
(1) |
|
2. detailed history, physical examination and identification of any immediate or impending airway compromise
|
A detailed history and physical examination are both vital in identifying the presence, source and any complications of infection. The priority in all patients should be the identification of any immediate or impending airway compromise, which should be imminently managed. |
Moderate |
Strong recommendation |
Systematic review |
(1) |
|
3. Aetiology
|
a.Most cases of DNSI are bacterial in aetiology; however, the causative pathogens in the paediatric population differ to those in the adult. Sources in paediatric cases include tonsillitis, pharyngitis, haematogenous and suppurative cervical adenitis compared with adult DNSI, which often have an odontogenic origin. The organisms commonly isolated in DNSIs are Staphylococcus aureus and group A Streptococcus. Anaerobic species include Fusobacterium, Peptostreptococcus and Porphyromonas |
Low |
Conditional recommendation |
Observational study |
(2) |
|
b.Sharp objects may cause perforation of the pharynx or oesophagus and may result in abscess formation in the adjacent neck spaces, such as the retropharyngeal space and should therefore be considered in the history taking and differential diagnosis process. |
Low |
Strong recommendation |
|||
|
4. The management of a DNSI
|
The management of a DNSI is highly dependent on the location and extent of deep neck involvement, and diagnostic imaging is essential in nearly every case. |
Moderate |
Conditional recommendation |
Systematic review |
(1) |
|
5. imaging in DNSI
|
a. Lateral neck radiographs are useful tool for screening of retropharyngeal and parapharyngeal abscesses, Ultrasound more accurate role than CT imaging in differentiating a drainable abscess from cellulitis and can guide diagnostic and therapeutic needle or catheter aspiration of superficial, uniloculated fluid collections when imminent airway compromise is not evident. |
Moderate |
Conditional recommendation |
Systematic review |
(3, 4) |
|
b. Contrast enhanced CT imaging is an accurate and sensitive tool to differentiate a drainable abscess from cellulitis and also significantly contribute to surgical planning to drain deep neck space collections. |
Moderate |
Strong recommendation |
|||
|
c.MRI provides better soft tissue definition than CT and in addition avoids exposure to radiation. However, the time taken to perform MRI, and the nature of the scanner, often means that a general anaesthetic is required for this investigation in pediatric population. Magnetic resonance angiography (MRA) is used to evaluate potential vascular complications, such as IJVT and carotid artery aneurysm or rupture. |
Moderate |
Conditional recommendation |
|||
|
6.Medical treatment in DNSIs
|
a.All patients with a DNSI should be given initial empiric antibiotic therapy (even if the patient is also being managed surgically) until culture and sensitivity results are available and advised that therapy should be effectively targeted against the aerobic and anaerobic bacteria. |
Low |
Strong recommendation |
Systematic review |
(5) |
|
b. Either penicillin in combination with a ß-lactamase inhibitor (such as amoxicillin with clavulanic acid) or a ß-lactamase–resistant antibiotic (such as cefoxitin, cefuroxime, imipenem or meropenem) in combination with a drug that is highly effective against most anaerobes (such as clindamycin or metronidazole) is recommended for optimal empiric coverage. |
Low |
Strong recommendation |
|||
|
7. Surgical drainage of DNSIs
|
a. Indications for surgical drainage include airway compromise, septicaemia, complications, extending or descending infection or no clinical improvement within 48 hours of the initiation of IV Antibiotics abscess >2.2 cm on CT imaging. |
Low |
Strong recommendation |
Observational study |
(6, 7) |
|
b. An external cervical approach is required for submandibular, prevertebral and carotid space infection. Parapharyngeal abscesses that are not obviously ‘pointing’ in the pharynx and complicated retropharyngeal abscesses that cannot be fully drained using an intraoral approach also require an external approach. |
Low |
Strong recommendation |
|
|
|
|
8. Minimally invasive techniques in DNSIs
|
Minimally invasive techniques such as image-guided needle aspiration of abcesses measuring <3 cm in diameter, and ultrasound-guided catheter placement for unilocular abscesses measuring >3 cm in diameter, extending into deep neck spaces or located within a glandular structurehave been used to treat well-defined, unilocular abscesses in patients who do not have airway compromise. |
Low |
Strong recommendation |
Observational study |
(6, 7) |
|
9. Acute airway obstruction
|
Acute airway obstruction is one of the most alarming complications of DNSI. It is commonly encountered in Ludwig’s angina and is a significant risk with a retropharyngeal abscess due to the potential for rupture into the airway leading to aspiration in addition to potential airway obstruction. Most cases are successfully managed with endotracheal intubation. Rarely, and in severe cases, intubation with general anaesthesia may be difficult and may precipitate complete airway obstruction that necessitates an emergency tracheostomy. |
Moderate |
Strong recommendation |
Systematic review |
(3) |
|
10. Monitoring of the airway in DNSIs
|
Monitoring of the airway is a priority when managing DNSI patients and should continue for at least 48 h after surgical intervention because of the potential for increasing oedema in the postoperative period. The routine use of intravenous steroids in patients who have impending airway obstruction has been advocated with the aim of minimising oedema and thereby reducing the need for aggressive airway intervention. |
Moderate |
Strong recommendation |
Systematic review |
(3) |
- Research needs
Research questions
▪️ Further research on aetiopathogenesis of deep neck space infections in pediatric age group.
▪️ Further research on efficacy of Minimally invasive techniques in DNSIs.- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria:
▪️ Monitoring of the airway is a priority when managing DNSI patients and should continue for at least 48 h after surgical intervention.
▪️ A detailed history and physical examination of patients with DNSIs.
▪️ Proper imaging study of patients with DNSIs.
▪️ All patients with a DNSI should be given initial empiric antibiotic therapy (even if the patient is also being managed surgically) until culture and sensitivity results are available.
▪️ Surgical drainage of patients with DNSIs when indicated.
▪️ Clinicians should document resolution, improvement, or worsened symptoms of neonatal stridor after treatment or observation.
All clinicians should be aware and informed to consider the following:
▪️ Red Flags that need urgent referral for Assessment/ Management must be taken into consideration.
▪️ For Assessment it is crucial to perform a detailed history/ clinical examination as a minimum patient assessment.
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.- References
1. Lawrence R, Bateman N. Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology. 2017;42(1):156-63.
2. Pardal-Peláez B, Pardal-Refoyo JL, Ochoa-Sangrador C, González-Serrano J, Montero-Martín J, López-Quiles J. Analysis of the prevalence of dental origin of deep neck infections. Journal of oral and maxillofacial surgery, medicine, and pathology. 2018;30(2):180-6.
3. Vieira F, Allen SM, Stocks RMS, Thompson JW. Deep neck infection. Otolaryngologic Clinics of North America. 2008;41(3):459-83.
4. Yellon R. Head and neck space infections. Pediatric otolaryngology. 2003;2:1681-701.
5. Carbone PN, Capra GG, Brigger MT. Antibiotic therapy for pediatric deep neck abscesses: a systematic review. International journal of pediatric otorhinolaryngology. 2012;76(11):1647-53.
6. Biron VL, Kurien G, Dziegielewski P, Barber B, Seikaly H. Surgical vs ultrasound-guided drainage of deep neck space abscesses: a randomized controlled trial: surgical vs ultrasound drainage. Journal of Otolaryngology-Head & Neck Surgery. 2013;42(1):18.
7. Yeow K-M, Liao C-T, Hao S-P. US-guided needle aspiration and catheter drainage as an alternative to open surgical drainage for uniloculated neck abscesses. Journal of Vascular and Interventional Radiology. 2001;12(5):589-9- Further Reading
▪️ Lawrence, R. and N. Bateman, Controversies in the management of deep neck space infection in children: an evidence‐based review. Clinical Otolaryngology, 2017. 42(1): p. 156-163. https://pubmed.ncbi.nlm.nih.gov/27288654/
▪️ Maharaj, S., S. Ahmed, and P. Pillay, Deep neck space infections: a case series and review of the literature. Clinical Medicine Insights: Ear, Nose and Throat, 2019. 12: p. 1179550619871274.
▪️ Bakir, S., et al., Deep neck space infections: a retrospective review of 173 cases. American journal of otolaryngology, 2012. 33(1): p. 56-63.
▪️ Das, R., G. Nath, and A. Mishra, Clinico-pathological profile of deep neck space infection: a prospective study. Indian Journal of Otolaryngology and Head & Neck Surgery, 2017. 69(3): p. 282-290.
▪️ Kataria, G., et al., Deep neck space infections: a study of 76 cases. Iranian journal of otorhinolaryngology, 2015. 27(81): p. 293.
▪️ Pankhania, M., et al., Tonsillitis, tonsillectomy, and deep neck space infections in England: the case for a new guideline for surgical and non-surgical management. The Annals of The Royal College of Surgeons of England, 2021. 103(3): p. 208-217. https://pubmed.ncbi.nlm.nih.gov/33645267/
- Annexes
Annex 1: Guideline development contributors and participants, with their declarations of interests
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
Annex 2: Guideline Flowchart
Annex 3: Tables of appraisal of selected guidelines: content (table 1), quality (table 2), , and currency (table 3), of the selected guidelines .
|
Tonsillitis, tonsillectomy, and deep neck space infections in England: the case for a new guideline for surgical and non-surgical management |
Controversies in the management of deep neck space infection in children: an evidence‐based review |
|
|
9 |
7 |
Credibility |
|
7 |
7 |
Observability |
|
7 |
9 |
Relevance |
|
8 |
8 |
Relative advantage |
|
8 |
7 |
Easy to install/understand |
|
7 |
7 |
Testability |
|
7 |
8 |
Compatibility |
|
53 |
63 |
Total score |
1. Assessment of content table:
Controversies in the management of deep neck space infection in children: an evidence‐based review had the highest scores.
2. Assessment of quality (CPG Appraisal tool):
|
Controversies in the management of deep neck space infection in children: an evidence‐based review |
Tonsillitis, tonsillectomy, and deep neck space infections in England: the case for a new guideline for surgical and non-surgical management |
|
|
1.Transparency |
A |
A |
|
2. Conflict of interest |
A |
A |
|
3. Development group |
A |
B |
|
4. Systematic review |
A |
A |
|
5. Grading of evidence |
A |
B |
|
6.Recommendations |
A |
B |
|
7. External review |
A |
B |
|
8.Updating |
A |
C |
3.Assessment of Currency table:
|
No |
Guideline Name |
Year of publication |
The organization |
Age demo-graphy |
|
1 |
Controversies in the management of deep neck space infection in children: an evidence‐based review |
2017 |
Clin Otolaryngol
. |
Adults and children |
|
2 |
Tonsillitis, tonsillectomy, and deep neck space infections in England: the case for a new guideline for surgical and non-surgical management |
2021 |
Ann R Coll Surg Engl
|
Adults and children |
No statements of the original guidline were modified, added nor omitted.









