
PHONIATRICS Brain damage motor handicap BDMH CORRECTED
"last update: 10 June 2024"
- Annexes
Editorial Independence:
· This guideline was developed without any external funding.
· All the guideline development group members have declared that they do not have any competing interests.
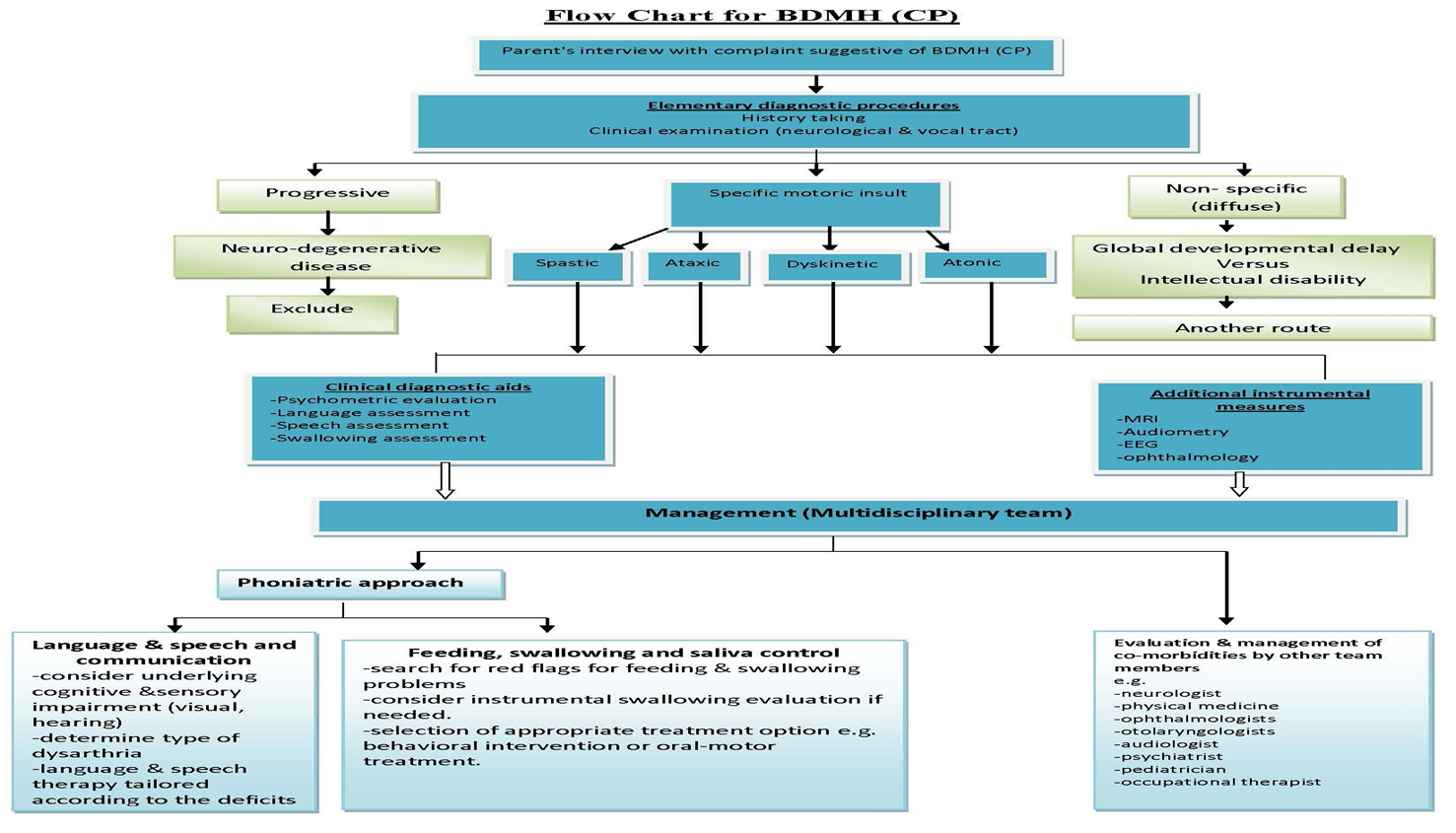
Annex 1: Guideline Flowchart
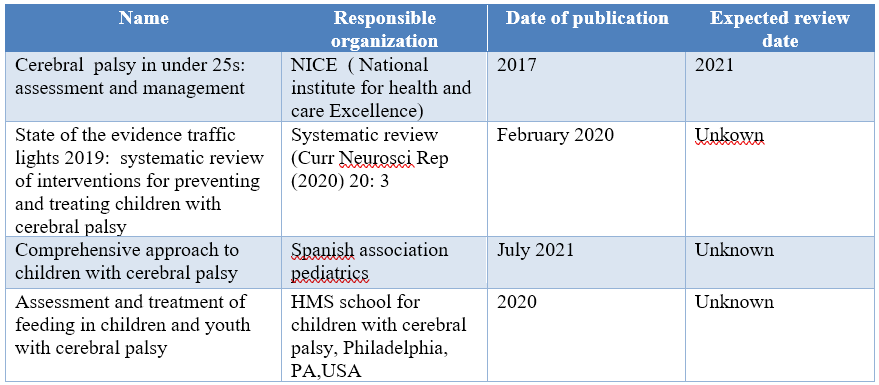
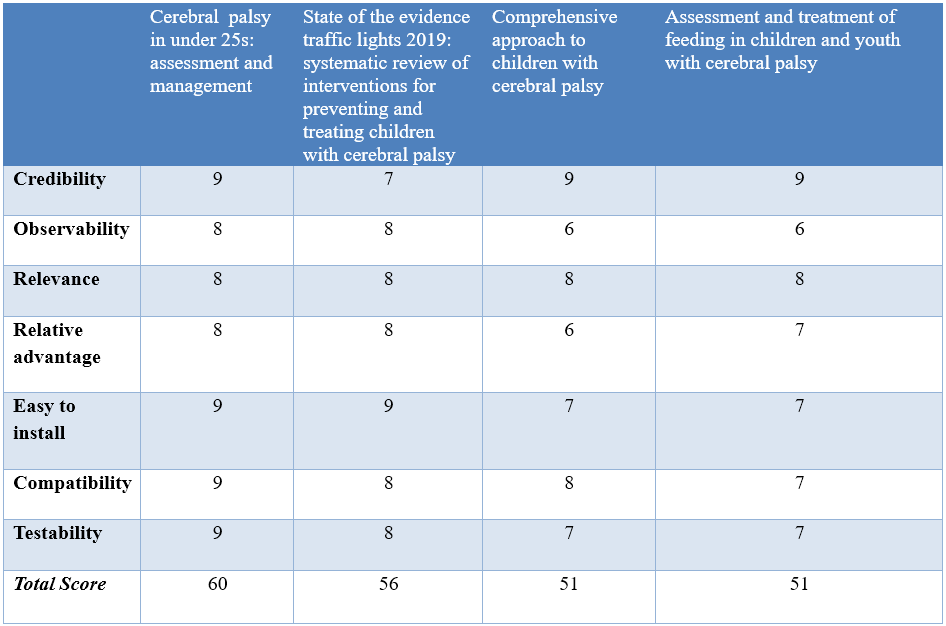
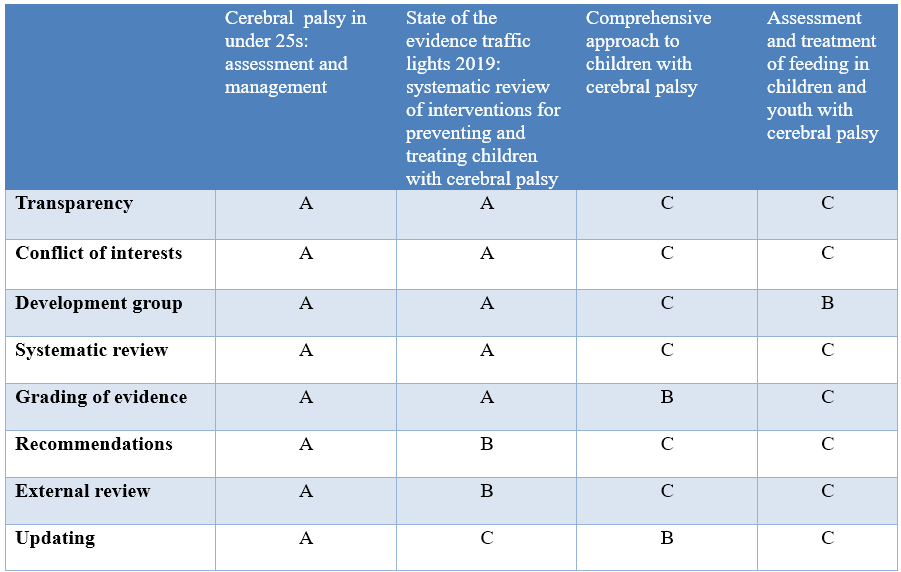
Annex 2: Tables of appraisal of selected guidelines:,
Currency (table 1)
Content (table 2)
Quality (table 3)
Annex 3: The risks and benefits of added and/or modified statements
|
STATEMENT |
RISK |
BENEFIT |
|
Assessment of Eating, drinking and swallowing difficulties Half of all children with BDMH (CP) have dysphagia and the prevalence is even higher in the infant population. Dysphagia management is extremely important because aspiration resulting in respiratory complication is a leading cause of death in individuals with BDMH (CP) (45%). The type of oral and pharyngeal problems in children with BDMH (CP) include reduced lip closure, poor tongue function, tongue thrust, exaggerated bite reflex, tactile hypersensitivity, delayed swallow initiation, reduced pharyngeal mobility & drooling. -Red flags for feeding/swallowing problems in children with BDMH(CP) are: · A feeding time of > 30 min on a regular basis. · Lack of weight gain for 2–3 months, not just weight loss particularly in the first 2 years of life. · Stressful mealtimes to the child or parents. · Increased congestion at mealtimes, gurgly voice quality, history of respiratory illnesses.
-A team approach is necessary for diagnosing and managing pediatric feeding and swallowing disorders. In addition to the phoniatrician, team members may include family and/or caregivers, dietitian, lactation consultant (infants), occupational therapist, physician (e.g., pediatrician, neonatologist, otolaryngologist, gastroenterologist), physical therapist, psychologist, social worker Assessment of infants and young children with signs and symptoms of feeding and/or swallowing disorders is likely to encompass multiple dimensions that include, but may not be limited to: (a) Review of family, medical, developmental, and feeding history. (b) Clinical Feeding and Swallowing Assessment: This typically consists of a physical examination (pre feeding assessment),oral structure and function examination, and feeding observation. (c) Other considerations (e.g., somatic growth patterns, neuro developmental status, oro facial structures, cardio pulmonary and other GI function). (d) Instrumental swallowing evaluation.
Criteria for an instrumental swallowing study in children with BDMH include the following: (1) Risk of aspiration (by history or observation), (2) Prior aspiration pneumonia, (3) Suspicion of a pharyngeal or laryngeal problem (for example, breathy voice quality), 4) Gurgly voice quality. |
There is risk of pneumonia and chest infection if the clinicians not aware of the red flags |
To make the clinician aware of the red flags for feeding and swallowing and Instrumental swallowing evaluation to avoid the risk of pneumonia
instrumentation allows the phoniatricians to gain more information about how the anatomical structures within the larynx are working. And to know the extent of swallow dysfunction, safety for food and the effectiveness of therapeutic strategies
|
|
Management of Eating, drinking and swallowing difficulties -Treatment selection will depend on the child’s age, cognitive and physical abilities, and specific swallowing and feeding problems -Treatment Options: 1-Postural and Positioning Techniques These techniques serve to protect the airway and offer safer transit of food and liquid. Techniques include chin down, chin up, head rotation, upright positioning (90° angle at hips and knees, feet on floor, with supports as needed), head stabilization (supported so as to present in chin-neutral position), cheek and jaw assist, reclining position, and side-lying positioning for infants.
2- Diet Modifications Typical modifications may include thickening thin liquids, softening, cutting/chopping, or pureeing solid foods to facilitate safety and ease of swallowing. Taste or temperature of a food may be altered to provide additional sensory input for swallowing. 3-Adaptive Equipment and Utensils These may be used with children who have feeding problems to foster independence with eating and increase swallow safety by controlling bolus size or achieving the optimal flow rate of liquids. Examples include modified nipples, cut out cups, angled forks and spoons, and sectioned plates. 4- Maneuvers Maneuvers are strategies used to change the timing or strength of movements of swallowing. Examples of maneuvers include Effortful swallow, Masako, or tongue hold, Mendelsohn maneuver, Supraglottic swallow, Super-supraglottic swallow. 5- Oral–Motor Treatments Oral–motor treatments include stimulation to—or actions of—the lips, jaw, tongue, soft palate, pharynx, larynx, and respiratory muscles. Oral–motor treatments range from passive (e.g., tapping, stroking, and vibration) to active (e.g., range-of-motion activities, resistance exercises, or chewing and swallowing exercises). Oral–motor treatments are intended to influence the physiologic underpinnings of the oropharyngeal mechanism in order to improve its functions. Some of these interventions can also incorporate sensory stimulation. 6- Feeding Strategies Feeding strategies include pacing and cue-based feeding. Pacing: Feeding strategies for children may include alternating bites of food with sips of liquid or swallowing 2–3 times per bite or sip. For infants, pacing can be accomplished by limiting the number of consecutive sucks. Strategies that slow the feeding rate may allow for more time between swallows to clear the bolus and may support more timely breaths.
Cue-based feeding: Most neonatal intensive care units (NICUs) have begun to move away from volume-driven feeding to cue-based feeding. In the NICU, the phoniatrician plays a critical role, supporting parents and other caregivers to understand and respond accordingly to the infant's communication during feeding. 7-Sensory Stimulation Techniques These may include thermal–tactile stimulation (e.g., using an iced lemon glycerin swab) or tactile stimulation (e.g., using a NUK brush) applied to the tongue or around the mouth. Sensory stimulation may be needed for children with reduced responses, overactive responses, or limited opportunities for sensory experiences. 8- Behavioral Interventions They are based on principles of behavioral modification and focus on increasing appropriate actions or behaviors and reducing maladaptive behaviors related to feeding. Examples include Feeding such as nasogastric tube, and gastrostomy. These approaches may be considered if the child’s swallowing safety and efficiency cannot reach a level of adequate function or does not adequately support nutrition and hydration. antecedent manipulation, shaping, prompting, modeling, stimulus fading, and differential reinforcement of alternate behavior, as well as implementation of basic mealtime principles (e.g., scheduled mealtimes in a neutral atmosphere with no food rewards). 9- Tube Non-nutritive sucking opportunities are thought to facilitate oral feeding skills in infants, most often via Pacifier. Children receiving nutrition and hydration via tube should be appropriate for brief ‘taste’ sessions over2–5 min multiple times per day. Spoon presentations with two to three drops of lemon juice or ice water may be tolerated without compromising pulmonary status and help to stimulate swallowing. Regular and thorough oral care is vital for all children. 10- Oral appliances or feeding devices 11-Neuromuscular electrical stimulation (NMES) |
Over time feeding, chewing and swallowing difficulties can lead to malnutrition and dehydration |
To maintaining respiratory health, optimising nutritional status
|
|
Managing saliva control - The reported prevalence of drooling ranges from 10% to 58%. In the assessment of affected patients, clinicians should determine its frequency, severity and impact on the quality of life of children and their caregivers. -A multidisciplinary team approach to the management of drooling is advisable. -Treatment Options: 1- Behavioral interventions: The aim of these interventions is to increase target behaviors, such as swallowing saliva, wiping lips and chin, improving head control, and teaching ways to manage drooling independently. Treatment techniques can include: instruction (e.g. please wipe your chin), prompting (e.g. giving a verbal prompt to swallow), positive reinforcement (e.g. praise), and/or self-management (instructions to swallow and wipe the chin) 2- Physical, oro-motor and oro-sensory therapies: These interventions involve correction of general body posture and head posture to eliminate the anterior loss of saliva from the oral cavity, therapy to improve lip and jaw closure as well as increasing tongue control, reducing tongue thrust , normalizing tone, and normalizing facial and oral sensation. 3- Pharmacologic treatments e.g. anticholinergic drugs 4-Botulinum toxin A injections to the salivary glands with ultrasound guidance if anticholinergic drugs provide insufficient benefit or are not tolerated. 5- Surgical interventions e.g. salivary gland excision, ligation, duct rerouting. 6- Intra-oral appliances e.g. the Exeter Lip Sensor, palatal training appliances. |
It affects the quality of life of those patients |
For clarification due to its importance |
|
Communication intervention The goal of communication therapy for children is to become active and independent Communicators in all of their daily environments.
A review of the evidence for language interventions showed that experimental studies exist to support intervention for vocabulary, grammar, narrative and social use of language. But, as with test materials, interventions may need to be adapted to meet the individual needs of children with restricted speech and movement and the impact of such adaptations on cognitive processing must be considered. To do this they need to develop as full a range of communication skills as possible and to have an Intelligible means of expressing all their needs and ideas.
The hearing problem should be assessed for the need of hearing aids and cochlear implant according to the profile of each CP case.
Children whose speech is often unintelligible may require augmentative and alternative systems of communication (AAC) to supplement their natural modes. The aim of AAC is to provide children all the vocabulary they need to communicate independently. AAC should be linked to verbal output from the conversational partner. |
Not to be missed |
For clarification |
|
Speech Manifestations Dysarthria in BDMH(CP) commonly affects all aspects of speech production: respiration, phonation, resonance, articulation and prosody. Impairments include: shallow, irregular breathing for speech; low pitched, harsh voice; reduced pitch variation/unexpected pitch breaks; hyper-nasality; and poor articulation. Although the underlying motor disorders vary (spasticity is associated with increased tone and reduced range of movement, choreo-athetosis is associated with involuntary movement and dysrhythmia), most characteristics (low pitch, poor breath control, imprecise articulation) affect the speech of children with both spastic and dyskinetic BDMH(CP) in addition to the cerebellar (with slowing down of articulatory movements, affected prosody with increased variability of pitch and loudness in addition to increased & equal stress) and mixed dysarthric types. The dyskinetic type is usually associated with severe degree of dysarthria up to anarthria due to the associated involuntary movements of the vocal tract. |
Not to be missed by clinicians |
To clarify speech manifestation to address these manifestations in rehabilitation programme |
|
Intervention for speech impairment Physiological approaches focusing on respiratory support and speech rate, which follow motor learning principles, show promise for children and young people with BDMH (CP).
PROMPT (Program for Restructuring Oral Musculature Phonetic Targets), a sensory-motor therapy in which therapists provide auditory, visual, tactile and kinesthetic cues for the production of speech sounds, help changes in lip and jaw control and gains improvement in intelligibility
Articulation therapy is not generally advised as a first line of treatment, due to the impaired control of multiple speech subsystems in BDMH dysarthria and the need for breath support to create clear vocal signal.
Oral motor therapy is widely used for improving chewing, swallowing and salivary control associated with dysarthria.
Careful application of articulation therapy techniques according to the dysarthric manifestations of the BDMH (CP) children. Syllable by syllable attack and multisyllabic segmentation are appropriate for spastic dysarthria rather than dyskinetic& cerebellar dysarthria that might get benefit from other techniques like soft articulatory contact and modeling respectively. |
Neglecting Oral motor therapy and speech therapy is affecting lip and jaw control and gains improvement in intelligibility
|
To clarify the steps of speech therapy in BDMH/CP patients improvement intelligibility of those patients |
|
Hearing impairment Discuss the following information: • Hearing impairment occurs in around 1 in 10 children and young people with BDMH (CP). • Prevalence of hearing impairment increases with increasing severity of motor impairment. • It is more common in people with dyskinetic or ataxic BDMH (CP) than in those with spastic BDMH (CP). • Regular ongoing hearing assessment is necessary & intervention with the use of hearing aids or cochlear implant should be discussed with the parents/ caregivers according to the profile of each patient. |
No risk |
To clarify that hearing impairment is common with dyskinetic BDMH(CP) |
|
Intellectual disability - Discuss the following: • Intellectual Disability (IQ below 70) occurs in around 1 in 2 children and young people with BDMH(CP). • Severe intellectual disability (IQ below 50) occurs in around 1 in 4 children and young people with BDMH(CP). • Intellectual disability increases with increasing severity of motor impairment. |
No risk |
Modification just for clarification |
|
Epilepsy -Epilepsy occurs in around 1 in 3 children with BDMH(CP) and 1 in 2 children with dyskinetic BDMH(CP). Dyskinetic movements should not be misinterpreted as epilepsy. -The seizures include focal, generalized & combined. -Diagnosis depends on family & personal history, characteristics of clinical events with electroencephalogram used as a gold standard. |
No risk |
To differentiate between epilepsy and dyskinetic movements |
|
Motoric problems The patient should be referred to the physiotherapist to assess the motoric condition Multiple techniques will be discussed with the parents including: -Bobath (neurodevelopmental approach) technique: it is multidisciplinary approach, involving physiotherapists, occupational therapists and speech language therapists. -Roods approach (neuro- physiological approach) dealing with the activation and de-activation of sensory receptors, which is concerned with the interaction of somatic, autonomic and psychic factors and their role in regulation of motor behavior. |
No risk |
to clarify the physiotherapy techniques |
