Male Sexual Dysfunction
| Site: | EHC | Egyptian Health Council |
| Course: | Urology Surgery Guidelines |
| Book: | Male Sexual Dysfunction |
| Printed by: | Guest user |
| Date: | Tuesday, 24 December 2024, 4:59 AM |
Description
"last update: 15 Oct 2024"
- Acknowledgement
|
Guidelines Development Group (GDG) of Male Sexual Dysfunction committee.
Funding: - No funding resources for the development of the guidelines. |
- List of Abbreviations
|
Abbreviation |
Description |
|
AIPE |
Arabic Index of Premature Ejaculation |
|
ART |
Assisted reproductive technology |
|
AUA |
American Urological Association |
|
BSSM |
British Society for Sexual Medicine |
|
CCH |
Collagenase Clostridium histolyticum |
|
CDU |
Color duplex ultrasonography |
|
DE |
Delayed Ejaculation |
|
DM |
Diabetes mellitus |
|
EAU |
European Association of Urology |
|
ED |
Erectile dysfunction |
|
EDV |
End diastolic velocity |
|
EE |
Electo-ejaculation |
|
EMA |
European Medicines Agency |
|
eNOS |
Endothelial nitric oxide synthase |
|
ESWT |
Extracorporeal Shockwave Therapy |
|
FDA |
Food and drug administration |
|
FSH |
Follicular Stimulating Hormone |
|
ICI |
Intracavernous injection |
|
ICSI |
Intracytoplasmic sperm injection |
|
IELT |
Intravaginal ejaculation latency time |
|
IHD |
Ischaemic heart disease |
|
IIEF |
Iinternational Index of Erectile Function |
|
iNOS |
Inducible nitric oxide synthase |
|
ISSM |
International Society of Sexual Medicine |
|
IVF |
In-vetro fertilization |
|
LH |
Luteinizing Hormone |
|
LUTS |
Lower urinary tract symptoms |
|
nNOS |
Neuronal nitric oxide synthase |
|
NPT |
Nocturnal penile tumescence |
|
PD |
Peyronie’s disease |
|
PDE5Is |
Phosphodiesterase type 5 inhibitors |
|
PE |
Premature ejaculation |
|
PEDT |
Premature Ejaculation Diagnostic Tool |
|
PGE1 |
Prostaglandin E 1 |
|
PP |
Penile prosthesis |
|
PSA |
Prostate-specific antigen |
|
PSV |
Peak systolic velocity |
|
PVS |
Penile vibratory stimulation |
|
QoL |
Quality of life |
|
RI |
Resistive index |
|
RP |
Radical prostatectomy |
|
SCD |
Sickle cell disease |
|
SCI |
Spinal cord injury |
|
SCs |
Stem cells |
|
SSRIs |
Selective serotonin reuptake inhibitors |
|
TA |
Tunica albuginea |
|
TGF-β1 |
Transforming growth factor beta 1 |
|
VED |
Vacuum erection device |
|
VOD |
Veno-occlusive dysfunction |
- Glossary
|
|
1- Erectile Dysfunction (ED): The persistent or recurrent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance. 2- Premature Ejaculation: Ejaculation that always or nearly always occurs prior to or within about one minute of vaginal penetration (lifelong PE) or a clinically significant and bothersome reduction in latency time, often to about three minutes or less (acquired PE). 3- Delayed Ejaculation: Marked delay in ejaculation or marked infrequency or absence of ejaculation on almost all or all occasions (75-100% of the times) of partnered sexual activity without the individual desiring delay persisting for at least 6 months and causing significant distress to the individual. 4- Peyronie’s Disease (PD) is a symptomatic disorder characterized by a constellation of penile symptoms and signs, such as penile pain, curvature, shortening, narrowing, hinge deformity, and palpable plaque with subsequent ED. 5- Priapism is a persistent penile erection for more than four hours and not related to sexual stimulation or relieved by ejaculation. Priapism carries high risk of structural damage to the cavernosal tissue which may lead to permanent ED. 4- Anejaculation: The complete absence of ejaculation either antegrade or retrograde. Caused by failed seminal emission from the seminal vesicles, prostate, and ejaculatory ducts into the urethra. In true anejaculation, there is normal orgasmic sensation and is always associated with central or peripheral nervous system dysfunction or with drugs. 5- Painful Ejaculation: is a condition in which the patient may feel variable degrees of pain during or after ejaculation involving the penis, scrotum, and perineum. 6- Haemospermia: is the presence of blood in the seminal fluid ejaculate. The condition causes anxiety and may indicate underlying pathology in many cases.
|
- Executive Summary
|
|
Scope of the guidelines Sexual health-related issues are wide-ranging and of importance to the overall health and sense of well-being for couples and families, and to the social and economic development of communities and countries. Erectile dysfunction (ED) and disorders of ejaculation are frequent encounters in male sexual medicine in the Middle East with the association of different risk factors and medical comorbidities in Arab region countries. Pharmacological therapies have completely changed the diagnostic and therapeutic approach to ED. This article integrates recent international guidelines with local experience and highlights the apparent lack of congruency between available treatment and communication, cultural, and gender norms of Middle East populations that may inhibit treatment seeking. The Egyptian Urological Association (EUA) Male Sexual Dysfunction Guidelines aims to present the contemporary evidence for medical practice in Egypt for the diagnosis and treatment of patients suffering from sexual dysfunction. Recommendations of the Male Sexual Dysfunction
|
- Introduction, purpose, scope, and audience
|
➡️Introduction Strategies for diagnosis and treatment of male sexual problems should consider the sociocultural factors that influence diagnosis and treatment seeking and engagement behaviours necessary for successful outcomes. Specifically, the detrimental effects of sexual problems on quality of life and the potential benefits of proper diagnosis and treatment should be more widely communicated to diminish the social disgrace associated with sexual problems and their management. Erectile dysfunction (ED) and premature ejaculation (PE) are the two main complaints in male sexual medicine in the Middle East (1-2). Pharmacological therapies have completely changed the diagnostic and therapeutic approach to ED (3,4). The prevalence of ED is 20–90% among patients with different risk factors and medical comorbidities in Arab region countries and severe ED in patients in this region could be attributed to: (1) the high prevalence of risk factors; (2) the poor control of those risk factors; (3) the delay in seeking medical advice; and (4) the non-compliance with treatment (1-2). Unfortunately, in Arab countries there are no firm data on the true prevalence of sexual dysfunction. This prompted several investigators in the region to conduct research to identify the magnitude of the current problem (1-2). This article integrates recent international guidelines with local experience and also highlights the apparent lack of congruency between available treatment and communication, cultural, and gender norms of Middle East populations that may inhibit treatment seeking. We clarified in our recent publication that strategies for diagnosis and treatment should consider the sociocultural factors that influence diagnosis and treatment seeking and engagement behaviours necessary for successful outcomes. Specifically, the detrimental effects of sexual problems on quality of life and the potential benefits of proper diagnosis and treatment should be more widely communicated to diminish the social disgrace associated with sexual problems and their management (5). Sexual dysfunction issues unique to our region: - Infertility and sexual dysfunction: Infertility is negatively linked to sexuality in couples seeking assisted reproductive technology (ART), suggesting the need for integrated management of psychosexual problems (6). Unique to infertile couples in Egypt, like the Arab and Muslim world, the option of donor insemination is not accepted. The challenge of unsuccessful fertility issues in Egyptians may even further have a detrimental effect on the couple's sexual function. Infertility and sexual dysfunction are associated (7). Lack of sexual awareness and education contribute to this problem. Psychosexual management is warrantied in these couples. - Unconsummated marriage: A specific situation urologist face in our region is unconsummated marriage. It is a social challenge for the man to deal with his wife's virginity on the wedding night. Such stress may lead to performance anxiety and failure, accumulating into a full-blown ED situation in an otherwise healthy young man. Unconsummated marriage might occur in men with normal erection due to other causes as premature ejaculation, performance anxiety, lack of desire, hypogonadism, lack of knowledge, social pressure, and female factors (8,9). The most common female factor was vaginismus (10). Particular to our regions, male lack of sexual desire may be related to consanguinity (11). - Polygamy, motives, and sexual dysfunction: Egypt is among the countries where polygamy is legal (12). Polygamy has a psychosexual impact on the first wife, impacting intimacy with her husband and negatively affecting the dynamics of the family that is peculiar to these parts of the world (13). Non-monogamous female drive to sex includes coping mechanisms to keep the partner, maintain self-esteem, and seek higher levels of sexual pleasure (14). Men seek polygamy for a variety of reasons. For example, in a Turkish study, men reported that they had a second wife because of decreased satisfaction of sexual desires by a wife, falling in love with the second wife, and incompatibility with the first wife (15). In the Asian community, a prevalent polygamous practice has many underlying factors (16). These include prestige, economic advantage, social customs, and exposure to commercial sex. While polygamy may negatively affect wives and children, a couple of studies showed that polygamous men have less ED, less premature ejaculation, lower depression scores, and higher sexual satisfaction (15,17). Other male sexual problems include Premature Ejaculation: Ejaculation that always or nearly always occurs prior to or within about one minute of vaginal penetration (lifelong PE) or a clinically significant and bothersome reduction in latency time, often to about three minutes or less (acquired PE). Delayed Ejaculation: Marked delay in ejaculation or marked infrequency or absence of ejaculation on almost all or all occasions (75-100% of the times) of partnered sexual activity without the individual desiring delay persisting for at least 6 months and causing significant distress to the individual. Peyronie’s Disease (PD) is a symptomatic disorder characterized by a constellation of penile symptoms and signs, such as penile pain, curvature, shortening, narrowing, hinge deformity, and palpable plaque with subsequent ED. Priapism is a persistent penile erection for more than four hours and not related to sexual stimulation or relieved by ejaculation. Priapism carries high risk of structural damage to the cavernosal tissue which may lead to permanent ED. ➡️Purpose The Urologic Egyptian Guidelines on Male Sexual Dysfunction aim to present the contemporary evidence for medical practice in Egypt for the diagnosis and treatment of patients suffering from sexual dysfunction. ➡️Scope The Urologic Egyptian Guidelines on Male Sexual Dysfunction help and guide clinical practitioners to have knowledge of the incidence, pathophysiology, and strategies for diagnosis and treatment of male sexual problems. This document integrates recent international guidelines with local experts’ opinions based on Egyptian healthcare and socioeconomic circumstances. It also reflects the opinions of experts in Sexual Dysfunction and represents state-of-the art references for all clinicians, as of the publication date. ➡️Target audience The target audience refers to those that deliver or implement the recommendations as well as health policymakers and other stakeholders involved in the adoption, adaptation, and transfer of health policies. The target audience of the guideline should not be misunderstood with the beneficiaries of the interventions or target population described in the guideline. · Urologists · Dermatologists and Andrologists · Family medicine and general practitioners · Gynaecologists, psychiatrists and endocrinologists |
- Methods
|
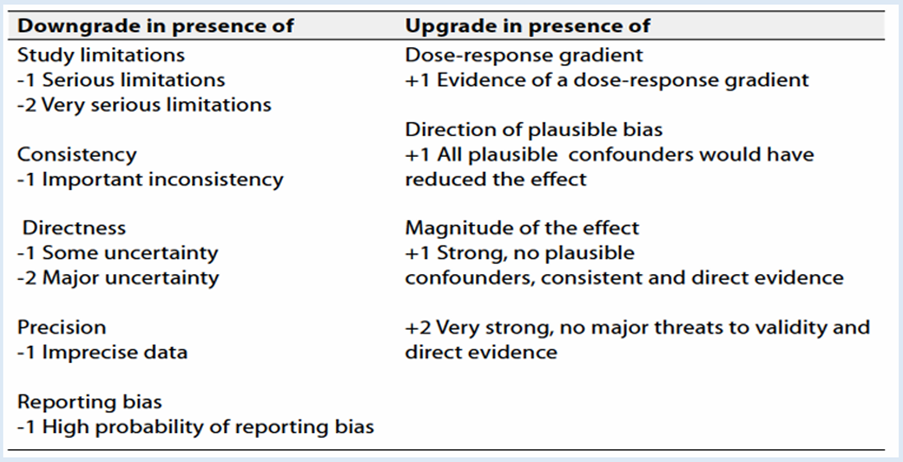
A comprehensive search for guidelines was undertaken to identify the most relevant guidelines to consider for adaptation. Inclusion/exclusion criteria followed in the search and retrieval of guidelines to be adapted: • Selecting only evidence-based guidelines (guideline must include a report on systematic literature searches and explicit links between individual recommendations and their supporting evidence) • Selecting only national and/or international guidelines • Specific range of dates for publication (using Guidelines published or updated 2015 and later) • Selecting peer reviewed publications only • Selecting guidelines written in English language • Excluding guidelines written by a single author not on behalf of an organization in order to be valid and comprehensive, a guideline ideally requires multidisciplinary input • Excluding guidelines published without references as the panel needs to know whether a thorough literature review was conducted and whether current evidence was used in the preparation of the recommendations The following characteristics of the retrieved guidelines were summarized in a table: • Developing organisation/authors • Date of publication, posting, and release • Country/language of publication • Date of posting and/or release • Dates of the search used by the source guideline developers All retrieved Guidelines were screened and appraised using AGREE II instrument (www.agreetrust.org) by at least two members. the panel decided a cut-off point or rank the guidelines (any guideline scoring above 50% on the rigour dimension was retained). Evidence assessment. According to WHO handbook for Guidelines we used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess the quality of a body of evidence, develop and report recommendations (18, 19). GRADE methods are used by WHO because these represent internationally agreed standards for making transparent recommendations. Detailed information on GRADE is available on the following sites: • GRADE working group: http://www.gradeworkingroup.org • GRADE online training modules: http://cebgrade.mcmaster.ca/ • GRADE profile software: http://ims.cochrane.org/revman/gradepro Table 1 Quality of evidence in GRADE
Table 2
Significance of the four levels of evidence Table 3: Factors that determine How to upgrade or downgrade the quality of evidence
The strength of the recommendation. The strength of a recommendation communicates the importance of adherence to the recommendation. Strong recommendations. With strong recommendations, the guideline communicates the message that the desirable effects of adherence to the recommendation outweigh the undesirable effects. This means that in most situations the recommendation can be adopted as policy. Conditional recommendations. These are made when there is greater uncertainty about the four factors above or if local adaptation has to account for a greater variety in values and preferences, or when resource use makes the intervention suitable for some, but not for other locations. This means that there is a need for substantial debate and involvement of stakeholders before this recommendation can be adopted as policy. When not to make recommendations. When there is lack of evidence on the effectiveness of an intervention, it may be appropriate not to make a recommendation. Databases searched included four resource categories: 1. Four international guidelines and recommendations, namely European Association of Urology [EAU], American Urological Association Guidelines [AUA], British Society for Sexual Medicine [BSSM], International Society of Sexual Medicine [ISSM] (20 – 24). 2. Review of several guides, reviews, statements, recommendations, and standards (23 – 25). 3. Relevant Egyptian publications. 4. A panel of 10 high-calibre urologists and andrologists representing different universities, institutions and private practice in Egypt. Adaptation of the Egyptian cultural aspects, the level of urologists’ capabilities and the availability of well-equipped hospitals were considered in the methodology of diagnosis and different treatment modalities.
|
- Recommendations
|
|
Recommendations for the diagnosis of Erectile Dysfunction:
Clinical Indicators for monitoring: 1. Thorough medical and sexual history using a validated questionnaire especially Arabic version. 2. Focused physical examination. 3. Testosterone and lipid profile. 4. Consider specific diagnostic tests when indicated.
Recommendation for assessment and management of Premature Ejaculation
Clinical Indicators for monitoring: 1. Medical and sexual history to diagnose and classify PE, use the patient-reported outcomes tools. 2. Focused physical examination. 3. Routine laboratory with seminal fluid culture and sensitivity to exclude underlying cause in patients with acquired PE
Recommendations for assessment of Delayed Ejaculation (107-109)
Clinical Indicators for monitoring: 1. Medical and sexual history with intravaginal ejaculatory latency time (IELT). 2. Focused physical examination. 3. Define if DE is lifelong or acquired, global or situational. 4. Specialized laboratory tests and radiologic investigation when indicated only. Recommendations for evaluation and management of Peyronie’s Disease (PD):
Clinical Indicators for monitoring: 1. Medical and sexual history. 2. Focused physical examination (self-photograph, or pharmacological-induced erection). 3. Penile length, curvature severity, and erectile function.
Recommendations for diagnosis of ischemic priapism
Recommendations for the treatment of ischemic priapism:
Recommendations for the treatment of non-ischemic priapism
Recommendations for the treatment of Stuttering priapism
Clinical Indicators for monitoring: 1. Medical and sexual history. 2. Focused physical examination. 3. laboratory investigations, complete blood count, coagulation profile and arterial blood gases. 4. Color duplex ultrasound of the penis and perineum |
- References
|
|
1- El-Sakka AI. Erectile dysfunction in Arab countries. Part I: Prevalence and correlates. Arab Journal of Urology (2012) 10, 97–103. 2- El-Sakka AI. Characteristics of erectile dysfunction in Saudi patients. Int J Impot Res 2004;16:13–20. 3- Lindau ST, Schumm LP, Laumann EO, Levinson W, O'Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007 Aug 23;357(8):762-74. doi: 10.1056/NEJMoa067423. PMID: 17715410; PMCID: PMC2426743. 4- Rosenberg MT, Sadovsky R. Identification and diagnosis of premature ejaculation. Int J Clin Pract. 2007 Jun;61(6):903-8. doi: 10.1111/j.1742-1241.2007.01337.x. PMID: 17504352. 5- El-Sakka A. I. Middle East Cultural Barriers and the Treatment of Sexual Problems. In., Cultural Differences and the Practice of Sexual Medicine, “Trends in Andrology and Sexual Medicine” (eds). Springer Science + Business Media, Chapter 8, P 135-148. 2020. 6- Luca G, Parrettini S, Sansone A, Calafiore R, Jannini EA. The Inferto-Sex Syndrome (ISS): sexual dysfunction in fertility care setting and assisted reproduction. J Endocrinol Invest. 2021 Oct;44(10):2071-2102. doi: 10.1007/s40618-021-01581-w. Epub 2021 May 6. PMID: 33956331; PMCID: PMC8421318. 7- Jain K, Radhakrishnan G, Agrawal P. Infertility and psychosexual disorders: relationship in infertile couples. Indian J Med Sci. 2000 Jan;54(1):1-7. PMID: 11214514. 8- Zargooshi J. Male sexual dysfunction in unconsummated marriage: long-term outcome in 417 patients. J Sex Med. 2008 Dec;5(12):2895-903. doi: 10.1111/j.1743-6109.2008.01004.x. PMID: 19090943. 9- Zargooshi J. Unconsummated marriage: clarification of aetiology; treatment with intracorporeal injection. BJU Int. 2000 Jul;86(1):75-9. doi: 10.1046/j.1464-410x.2000.00727.x. PMID: 10886087. 10- Ozdemir O, Simsek F, Ozkardeş S, Incesu C, Karakoç B. The unconsummated marriage: its frequency and clinical characteristics in a sexual dysfunction clinic. J Sex Marital Ther. 2008; 34(3):268-79. doi: 10.1080/00926230701866380. PMID: 18398764. 11- Addar MH. The unconsummated marriage: causes and management. Clin Exp Obstet Gynecol. 2004;31(4):279-81. PMID: 15672966. 12- Elbedour S, Onwuegbuzie AJ, Caridine C, Abu-Saad H. The effect of polygamous marital structure on behavioral, emotional, and academic adjustment in children: a comprehensive review of the literature. Clin Child Fam Psychol Rev. 2002 Dec;5(4):255-71. doi: 10.1023/a:1020925123016. PMID: 12495269. 13- Mengistu N, Shumye S, Tesfaye TS, Haile S, Bayisa Y, Yimer S, Tadesse M, Markos T, Madoro D, Assefa DG, Molla W, Abebe L, Molla A, Wudneh A, Duko B. Stressful life experience of the first married women in polygamous families in Gedeo zone, South Ethiopia: a qualitative study, 2021. BMC Psychol. 2022 Feb 22;10(1):40. doi: 10.1186/s40359-022-00753-4. Erratum in: BMC Psychol. 2022 Aug 2; 10(1):191. PMID: 35193677; PMCID: PMC8864848. 14- Kelberga AK, Martinsone B. Differences in Motivation to Engage in Sexual Activity Between People in Monogamous and Non-monogamous Committed Relationships. Front Psychol. 2021 Nov 3;12:753460. doi: 10.3389/fpsyg.2021.753460. PMID: 34803835; PMCID: PMC8595918. 15- Ekerbiçer HÇ, Resim S, Efe E, Bahar MR, Altunören Ö, Küçükdurmaz F, Benlioğlu C. A Comparison of Sexual Function, Psychological Status, and Sociodemographic Characteristics of Turkish Men within Polygamous and Monogamous Marriages. Balkan Med J. 2016 Jul;33(4):383-9. doi: 10.5152/balkanmedj.2016.16459. Epub 2016 Jul 1. PMID: 27606132; PMCID: PMC5001814. 16- Is one wife enough? Polygamy's increasingly threatened role in the modern world. Asiaweek. 1993 Dec 8:28-30, 35. PMID: 12346310. 17- Mohamed AH, Mohamud HA, Yasar A. The prevalence of premature ejaculation and its relationship with polygamous men: a cross-sectional observational study at a tertiary hospital in Somalia. BMC Urol. 2021 Dec 16;21(1):175. doi: 10.1186/s12894-021-00942-0. PMID: 34915878; PMCID: PMC8680334. 18- Guyatt, G.H., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ, 2008. 336: 924. 19- Guyatt, G.H., et al. What is “quality of evidence” and why is it important to clinicians? BMJ, 2008. 336: 995 20- Salonia (Chair), C. Bettocchi, P. Capogrosso, J. Carvalho, G. Corona, G. Hatzichristodoulou, et. al. EAU Guidelines. Edn. presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6. 21- Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh J, Khera M, McVary KT, Miner MM, Nelson CJ, Sadeghi-Nejad H, Seftel AD, Shindel AW . Erectile Dysfunction: AUA Guideline. J Urol. 2018 Sep;200(3):633-641. doi:10.1016/j.juro.2018.05.004. Epub 2018 May 7. 22- Hackett G, Kirby M, Wylie K, Heald A, Ossei-Gerning N, Edwards D, Muneer A. British Society for Sexual Medicine Guidelines on the Management of Erectile Dysfunction in Men-2017. J Sex Med. 2018 Apr;15(4):430-457. doi: 10.1016/j.jsxm.2018.01.023. Epub 2018 Mar 14. PMID: 29550461. 23- ISSM QUICK REFERENCE GUIDE ON TESTOSTERONE DEFICIENCY FOR MEN. Version: September 2015, International Society for Sexual Medicine - www.issm.info 24- ISSM QUICK REFERENCE GUIDE TO PE. Version: January 2015 International Society for Sexual Medicine - www.issm.info 25- Goodman N, Guay A, Dandona P, Dhindsa S, Faiman C, Cunningham GR; AACE Reproductive Endocrinology Scientific Committee.. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY POSITION STATEMENT ON THE ASSOCIATION OF TESTOSTERONE AND CARDIOVASCULAR RISK. Endocr Pract. 2015 Sep;21(9):1066-73. doi: 10.4158/EP14434.PS 26- Fode M, Salonia A, Minhas S, Burnett AL, Shindel AW. Late-onset Hypogonadism and Testosterone Therapy. A Summary of Guidelines from the American Urological Association and the European Association of Urology. Eur Urol Focus. 2019 Jul; 5(4): 539-544. doi:10.1016/j.euf.2019.02.021. Epub 2019 Mar 8. 27- Hatzichristou, D.G., et al. Nocturnal penile tumescence and rigidity monitoring in young potent volunteers: reproducibility, evaluation criteria and the effect of sexual intercourse. J Urol, 1998. 159: 1921. 28- Mulhall JP, Goldstein I, Bushmakin AG et al: Validation of the erection hardness score. J Sex Med 2007; 4: 1626. 29- Rosen RC, Cappelleri JC, Smith MD et al: Development and evaluation of an abridged, 5-item version of the international index of erectile function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 1999; 11: 319 30- Shamloul R, Ghanem H, Abou-zeid A. Validity of the Arabic version of the sexual health inventory for men among Egyptians. Int J Impot Res. 2004 Oct;16(5):452-5. doi: 10.1038/sj.ijir.3901248. PMID: 15175638. 31- Abdelrahman Elnashar, Amr M. Gadallah, Alaa A. Abdelaal, et al., Can the International Index of Erectile Function (IIEF-5) be used as a diagnostic tool to the severity of vasculogenic erectile dysfunction? Middle East Fertility Society Journal (2012) 17, 101–104. 32- Arthur L. Burnett, Ajay Nehra, Rodney H. Breau,et al., Erectile Dysfunction: AUA Guideline. J Urol, Vol. 200, 633-641, September 2018. 33- Kamel I, Gadalla A, Ghanem H, Oraby M. Comparing penile measurements in normal and erectile dysfunction subjects. J Sex Med 2009; 6:2305–10. 34- Davis-Joseph B, Tiefer L, Melman A. Accuracy of the initial history and physical examination to establish the etiology of erectile dysfunction. Urology 1995; 45:498–502. 35- Heidenreich, A., et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol, 2014. 65: 124. 36- Maggi, M., et al. Hormonal causes of male sexual dysfunctions and their management (hyperprolactinemia, thyroid disorders, GH disorders, and DHEA). J Sex Med, 2013. 10: 661. 37- El-Sakka AI, Hassoba HM, Sayed HM, Tayeb KA. Pattern of endocrinal changes in patients with sexual dysfunction. J Sex Med 2005;2:551–8. 38- El-Sakka AI, Hassoba HM, Elbakry AM, Hassan HA. Prostatic specific antigen in patients with hypogonadism: effect of testosterone replacement. J Sex Med 2005; 2:235–40. 39- Zohdy W, Kamal EE, Ibrahim Y. Androgen deficiency and abnormal penile duplex parameters in obese men with erectile dysfunction. J Sex Med 2007; 4:797–808. 40- Goodman N, Guay A, Dandona P, Dhindsa S, Faiman C, Cunningham GR; AACE Reproductive Endocrinology Scientific Committee.. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY POSITION STATEMENT ON THE ASSOCIATION OF TESTOSTERONE AND CARDIOVASCULAR RISK. Endocr Pract. 2015 Sep;21(9):1066-73. doi: 10.4158/EP14434.PS 41- Fode M, Salonia A, Minhas S, Burnett AL, Shindel AW. Late-onset Hypogonadism and Testosterone Therapy. A Summary of Guidelines from the American Urological Association and the European Association of Urology. Eur Urol Focus. 2019 Jul; 5(4): 539-544. doi:10.1016/j.euf.2019.02.021. Epub 2019 Mar 8. 42- McMahon CG. Current diagnosis and management of erectile dysfunction. Med J Aust. 2019 Jun;210(10):469-476. doi: 10.5694/mja2.50167. Epub 2019 May 17. PMID: 31099420. 43- Wiggins A, Tsambarlis PN, Abdelsayed G, Levine LA. A treatment algorithm for healthy young men with erectile dysfunction. BJU Int. 2019 Jan;123(1):173-179. doi: 10.1111/bju.14458. Epub 2018 Aug 28. PMID: 29993196. 44- Ismail EA, El-Sakka AI. Innovative trends and perspectives for erectile dysfunction treatment: A systematic review. Arab J Urol. 2016 May 18;14(2):84-93. Doi: 10.1016/j.aju.2016.04.002. PMID: 27493808; PMCID: PMC4963167. 45- seftel AD, Mohammed MA, Althof SE. Erectile dysfunction: etiology, evaluation, and treatment options. Med Clin North Am. 2004 Mar;88(2):387-416, xi. Doi: 10.1016/S0025-7125(03)00187-1. PMID: 15049584. 46- El-Sakka AI. Pharmacotherapy for erectile dysfunction in diabetic males. Expert Opin Pharmacother. 2018 Aug;19(12):1345-1356. Doi: 10.1080/14656566.2018.1505866. Epub 2018 Aug 14. PMID: 30106605. 47- Ventimiglia E, Capogrosso P, Montorsi F, Salonia A. The safety of phosphodiesterase type 5 inhibitors for erectile dysfunction. Expert Opin Drug Saf 2016;15:141–52. 48- El-Sakka AI, Anis T, Khadr N, Ismail TA, Hegazy AM, Fekry O, Youseif E. Sildenafil for erectile dysfunction in the Middle East: observational analysis of patients with diabetes and/or hypertension treated in the clinical practice setting. J Int Med Res. 2011;39(2):558-68. Doi: 10.1177/147323001103900225. PMID: 21672361. 49- Walker LM, Santos-Iglesias P. On the Relationship Between Erectile Function and Sexual Distress in Men with Prostate Cancer. Arch Sex Behav. 2020 Jul;49(5):1575-1588. doi: 10.1007/s10508-019-01603-y. Epub 2020 Feb 18. PMID: 32072396. 50- Goonewardene SS, Persad R. Psychosexual care in prostate cancer survivorship: a systematic review. Transl Androl Urol. 2015 Aug;4(4):413-20. doi: 10.3978/j.issn.2223-4683.2015.08.04. PMID: 26816840; PMCID: PMC4708596. 51- Ramirez-Fort MK, Suarez P, Carrion M, Weiner D, Postl C, Arribas R, Sayyah M, Forta DV, Niaz MJ, Feily A, Lange CS, Fort ZZ, Fort M. Prostatic irradiation-induced sexual dysfunction: A review and multidisciplinary guide to management in the radical radiotherapy era (Part III on Psychosexual Therapy and the Masculine Self-Esteem). Rep Pract Oncol Radiother. 2020 Jul-Aug;25(4):625-631. doi: 10.1016/j.rpor.2020.03.014. Epub 2020 Apr 30. PMID: 32536830; PMCID: PMC7276493. 52- Rajkumar RP, Kumaran AK. Depression and anxiety in men with sexual dysfunction: a retrospective study. Compr Psychiatry. 2015 Jul;60:114-8. doi: 10.1016/j.comppsych.2015.03.001. Epub 2015 Mar 19. PMID: 25818906. 53- Avasthi A, Grover S, Kaur R, Prakash O, Kulhara P. Impact of nonorganic erectile dysfunction on spouses: a study from India. J Sex Med. 2010 Nov;7(11):3666-74. doi: 10.1111/j.1743-6109.2009.01647.x. PMID: 20059659. 54- Montorsi F, Brock G, Lee J, Shapiro J, Van Poppel H, Graefen M, Stief C. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol. 2008 Oct;54(4):924-31. doi: 10.1016/j.eururo.2008.06.083. Epub 2008 Jul 9. PMID: 18640769. 55- Sari Motlagh R, Abufaraj M, Yang L, Mori K, Pradere B, Laukhtina E, Mostafaei H, Schuettfort VM, Quhal F, Montorsi F, Amjadi M, Gratzke C, Shariat SF. Penile Rehabilitation Strategy after Nerve Sparing Radical Prostatectomy: A Systematic Review and Network Meta-Analysis of Randomized Trials. J Urol. 2021 Apr;205(4):1018-1030. doi: 10.1097/JU.0000000000001584. Epub 2021 Jan 14. PMID: 33443457. 56- Feng D, Liu S, Yang Y, Bai Y, Li D, Han P, Wei W. Generating comprehensive comparative evidence on various interventions for penile rehabilitation in patients with erectile dysfunction after radical prostatectomy: a systematic review and network meta-analysis. Transl Androl Urol. 2021 Jan;10(1):109-124. doi: 10.21037/tau-20-892. PMID: 33532301; PMCID: PMC7844489. 57- Coombs PG, Heck M, Guhring P, Narus J, Mulhall JP. A review of outcomes of an intracavernosal injection therapy programme. BJU Int. 2012 Dec;110(11):1787-91. doi: 10.1111/j.1464-410X.2012.11080.x. Epub 2012 May 7. PMID: 22564343. 58- Mohamed M. Seftel AD. Althof S.et al. Office evaluation of male sexual dysfunction: detection of hypogonadism, depression and erectile dysfunction [abstract 1261 J Urol 2003; supple:169. 59- Elkamshoushi AM, Badae NM, Kabary MG, Omar SI. Evaluation of daily avanafil efficacy in improving the endothelial function in Egyptian males with erectile dysfunction. Andrologia. 2021 Feb;53(1):e13833. doi: 10.1111/and.13833. Epub 2020 Oct 28. PMID: 33112433. 60- Li J, Peng L, Cao D, He L, Li Y, Wei Q. Avanafil for the Treatment of men With Erectile Dysfunction: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am J Mens Health. 2019 Sep-Oct;13(5):1557988319880764. doi: 10.1177/1557988319880764. PMID: 31672076; PMCID: PMC6826932. 61- Ismail EA, Younis SE, Ismail IY, El-Wazir YM, El-Sakka AI. Early administration of phosphodiesterase 5 inhibitors after induction of diabetes in a rat model may prevent erectile dysfunction. Andrology. 2020 Jan;8(1):241-248. 62- Trost LW, Munarriz R, Wang R, Morey A, Levine L. External Mechanical Devices and Vascular Surgery for Erectile Dysfunction. J Sex Med. 2016 Nov;13(11):1579-1617. doi: 10.1016/j.jsxm.2016.09.008. PMID: 27770853. 63- Pajovic B, Dimitrovski A, Fatic N, Malidzan M, Vukovic M. Vacuum erection device in treatment of organic erectile dysfunction and penile vascular differences between patients with DM type I and DM type II. Aging Male. 2017 Mar;20(1):49-53. doi: 10.1080/13685538.2016.1230601. Epub 2016 Oct 1. PMID: 27690728. 64- El-Sakka AI. What is the current role of intracavernosal injection in management of erectile dysfunction? Int J Impot Res. 2016 May;28(3):88-95. doi: 10.1038/ijir.2016.14. Epub 2016 Apr 14. PMID: 27076113. 65- Capogrosso P, Frey A, Jensen CFS, Rastrelli G, Russo GI, Torremade J, Albersen M, Gruenwald I, Reisman Y, Corona G. Low-Intensity Shock Wave Therapy in Sexual Medicine-Clinical Recommendations from the European Society of Sexual Medicine (ESSM). J Sex Med. 2019 Oct;16(10):1490-1505. doi: 10.1016/j.jsxm.2019.07.016. Epub 2019 Aug 22. PMID: 31447380. 66- Chung E, Cartmill R. Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: an Australian first open-label single-arm prospective clinical trial. BJU Int. 2015 Apr;115 Suppl 5:46-9. doi: 10.1111/bju.13035. PMID: 25828173. 67- Young Academic Urologists Men's Health Group; Fode M, Hatzichristodoulou G, Serefoglu EC, Verze P, Albersen M. Low-intensity shockwave therapy for erectile dysfunction: is the evidence strong enough? Nat Rev Urol. 2017 Oct;14(10):593-606. doi: 10.1038/nrurol.2017.119. Epub 2017 Jul 25. PMID: 28741629. 68- Sokolakis I, Hatzichristodoulou G. Clinical studies on low intensity extracorporeal shockwave therapy for erectile dysfunction: a systematic review and meta-analysis of randomised controlled trials. Int J Impot Res. 2019 May;31(3):177-194. doi: 10.1038/s41443-019-0117-z. Epub 2019 Jan 21. PMID: 30664671. 69- Kalyvianakis D, Hatzichristou D. Low-Intensity Shockwave Therapy Improves Hemodynamic Parameters in Patients With Vasculogenic Erectile Dysfunction: A Triplex Ultrasonography-Based Sham-Controlled Trial. J Sex Med. 2017 Jul;14(7):891-897. doi: 10.1016/j.jsxm.2017.05.012. Erratum in: J Sex Med. 2018 Feb;15(2):270. PMID: 28673433. 70- Tao R, Chen J, Wang D, Li Y, Xiang J, Xiong L, Ji J, Wu J, Zhou S, Jia C, Lv J, Yang J, Tang Q. The Efficacy of Li-ESWT Combined With VED in Diabetic ED Patients Unresponsive to PDE5is: A Single-Center, Randomized Clinical Trial. Front Endocrinol (Lausanne). 2022 Jun 23;13:937958. doi: 10.3389/fendo.2022.937958. PMID: 35813628; PMCID: PMC9259797. 71- Mykoniatis I, Pyrgidis N, Zilotis F, Kapoteli P, Fournaraki A, Kalyvianakis D, Hatzichristou D. The Effect of Combination Treatment With Low-Intensity Shockwave Therapy and Tadalafil on Mild and Mild-To-Moderate Erectile Dysfunction: A Double-Blind, Randomized, Placebo-Controlled Clinical Trial. J Sex Med. 2022 Jan;19(1):106-115. doi: 10.1016/j.jsxm.2021.10.007. Epub 2021 Dec 2. PMID: 34866029. 72- Kalyvianakis D, Mykoniatis I, Pyrgidis N, Kapoteli P, Zilotis F, Fournaraki A, Hatzichristou D. The Effect of Low-Intensity Shock Wave Therapy on Moderate Erectile Dysfunction: A Double-Blind, Randomized, Sham-Controlled Clinical Trial. J Urol. 2022 Aug;208(2):388-395. doi: 10.1097/JU.0000000000002684. Epub 2022 May 6. PMID: 35830338. 73- Kalyvianakis D, Mykoniatis I, Memmos E, Kapoteli P, Memmos D, Hatzichristou D. Low-intensity shockwave therapy (LiST) for erectile dysfunction: a randomized clinical trial assessing the impact of energy flux density (EFD) and frequency of sessions. Int J Impot Res. 2020 May;32(3):329-337. doi: 10.1038/s41443-019-0185-0. Epub 2019 Sep 2. PMID: 31474753. 74- Adeldaeim HM, Abouyoussif T, Gebaly OE, Assem A, Wahab MMA, Rashad H, Sakr M, Zahran AR. Prognostic Indicators for Successful Low-intensity Extracorporeal Shock Wave Therapy Treatment of Erectile Dysfunction. Urology. 2021 Mar;149:133-139. doi: 10.1016/j.urology.2020.12.019. Epub 2020 Dec 26. PMID: 33373703. 75- Rho BY, Kim SH, Ryu JK, Kang DH, Kim JW, Chung DY. Efficacy of Low-Intensity Extracorporeal Shock Wave Treatment in Erectile Dysfunction Following Radical Prostatectomy: A Systematic Review and Meta-Analysis. J Clin Med. 2022 May 14;11(10):2775. doi: 10.3390/jcm11102775. PMID: 35628901; PMCID: PMC9145026. 76- Towe M, Peta A, Saltzman RG, Balaji N, Chu K, Ramasamy R. The use of combination regenerative therapies for erectile dysfunction: rationale and current status. Int J Impot Res. 2022 Dec;34(8):735-738. doi: 10.1038/s41443-021-00456-1. Epub 2021 Jul 12. PMID: 34253869. 77- Oudelaar BW, Peerbooms JC, Huis In 't Veld R, Vochteloo AJH. Concentrations of Blood Components in Commercial Platelet-Rich Plasma Separation Systems: A Review of the Literature. Am J Sports Med. 2019 Feb;47(2):479-487. doi: 10.1177/0363546517746112. Epub 2018 Jan 16. PMID: 29337592. 78- Poulios E, Mykoniatis I, Pyrgidis N, Zilotis F, Kapoteli P, Kotsiris D, Kalyvianakis D, Hatzichristou D. Platelet-Rich Plasma (PRP) Improves Erectile Function: A Double-Blind, Randomized, Placebo-Controlled Clinical Trial. J Sex Med. 2021 May;18(5):926-935. doi: 10.1016/j.jsxm.2021.03.008. Epub 2021 Apr 24. PMID: 33906807. 79- Zaghloul AS, El-Nashaar AM, Said SZ, Osman IA, Mostafa T. Assessment of the intracavernosal injection platelet-rich plasma in addition to daily oral tadalafil intake in diabetic patients with erectile dysfunction non-responding to on-demand oral PDE5 inhibitors. Andrologia. 2022 Jul;54(6):e14421. doi: 10.1111/and.14421. Epub 2022 Mar 17. PMID: 35301742. 80- Alkandari MH, Touma N, Carrier S. Platelet-Rich Plasma Injections for Erectile Dysfunction and Peyronie's Disease: A Systematic Review of Evidence. Sex Med Rev. 2022 Apr;10(2):341-352. doi: 10.1016/j.sxmr.2020.12.004. Epub 2021 Jul 2. PMID: 34219010. 81- Panunzio A, Labate C, Zacheo F, Orlando R, Rizzo FL, Porcaro AB, Migliorini F, Pagliarulo V, Tafuri A. Platelet-rich plasma intracavernosal injections for the treatment of primary organic erectile dysfunction: a systematic review and meta-analysis of contemporary controlled studies. Int J Impot Res. 2023 Nov 22. doi: 10.1038/s41443-023-00798-y. Epub ahead of print. PMID: 37993601. 82- Fazekas D, Campbell K, Ledesma B, Masterson T. Platelet-rich plasma for erectile dysfunction: a review of the current research landscape. Sex Med Rev. 2023 Sep 27;11(4):369-374. doi: 10.1093/sxmrev/qead032. PMID: 37786350. 83- Shaher H, Fathi A, Elbashir S, Abdelbaki SA, Soliman T. Is Platelet Rich Plasma Safe and Effective in Treatment of Erectile Dysfunction? Randomized Controlled Study. Urology. 2023 May;175:114-119. doi: 10.1016/j.urology.2023.01.028. Epub 2023 Feb 1. PMID: 36736914. 84- Reddy AG, Dick BP, Natale C, Akula KP, Yousif A, Hellstrom WJG. Application of Botulinum Neurotoxin in Male Sexual Dysfunction: Where Are We Now? Sex Med Rev. 2021 Apr;9(2):320-330. doi: 10.1016/j.sxmr.2020.05.004. Epub 2020 Jul 5. PMID: 32641225. 85- Ghanem H, Raheem AA, Abdel Rahman IFS, Johnson M, Abdel- Raheem T. Botulinum neurotoxin and its potential role in the treatment of erectile dysfunction. Sex Med Rev 2018;6(1):135– 42. doi:10.1016/j.sxmr.2017.07.008. 86- Abdelrahman IFS, Raheem AA, Elkhiat Y, Aburahma AA, Abdel-Raheem T, Ghanem H. Safety and efficacy of botulinum neurotoxin in the treatment of erectile dysfunction refractory to phosphodiesterase inhibitors: Results of a randomized controlled trial. Andrology. 2022 Feb;10(2):254-261. doi: 10.1111/andr.13104. Epub 2021 Oct 7. PMID: 34618409. 87- El-Shaer W, Ghanem H, Diab T, Abo-Taleb A, Kandeel W. Intra-cavernous injection of BOTOX® (50 and 100 Units) for treatment of vasculogenic erectile dysfunction: Randomized controlled trial. Andrology. 2021 Jul;9(4):1166-1175. doi: 10.1111/andr.13010. Epub 2021 Apr 20. PMID: 33784020. 88- Babaei, A.R., M.R. Safarinejad, and A.A. Kolahi, Penile revascularization for erectile dysfunction: a systematic review and meta-analysis of effectiveness and complications. Urol J, 2009. 6(1): p. 1-7. 89- Hellstrom, W.J., et al., Implants, mechanical devices, and vascular surgery for erectile dysfunction. J Sex Med, 2010. 7(1 Pt 2): p. 501-23. 90- Kawanishi, Y., et al., Penile revascularization surgery for arteriogenic erectile dysfunction: the long-term efficacy rate calculated by survival analysis. BJU Int, 2004. 94(3): p. 361-8. 91- Sohn, M., et al., Standard operating procedures for vascular surgery in erectile dysfunction: revascularization and venous procedures. J Sex Med, 2013. 10(1): p. 172-9. 92- Antonini, G., et al., Minimally invasive infrapubic inflatable penile prosthesis implant for erectile dysfunction: evaluation of efficacy, satisfaction profile and complications. Int J Impot Res, 2016. 28(1): p. 4-8. 93- Kramer, A.C. and A. Schweber, Patient expectations prior to coloplast titan penile prosthesis implant predicts postoperative satisfaction. J Sex Med, 2010. 7(6): p. 2261-2266. 94- Pisano F, Falcone M, Abbona A, Oderda M, Soria F, Peraldo F, Marson F, Barale M, Fiorito C, Gurioli A, Frea B, Gontero P. The importance of psychosexual counselling in the re-establishment of organic and erotic functions after penile prosthesis implantation. Int J Impot Res. 2015 Sep-Oct;27(5):197-200. doi: 10.1038/ijir.2015.17. Epub 2015 Aug 13. PMID: 26268774. 95- Montague, D.K., Penile prosthesis implantation in the era of medical treatment for erectile dysfunction. Urol Clin North Am, 2011. 38(2): p. 217-25. 96- Mulcahy, J.J., et al., The penile implant for erectile dysfunction. J Sex Med, 2004. 1(1): p. 98-109. 97- Natali, A., R. Olianas, and M. Fisch, Penile implantation in Europe: successes and complications with 253 implants in Italy and Germany. J Sex Med, 2008. 5(6): p. 1503-12. 98- Akakpo, W., M.A. Pineda, and A.L. Burnett, Critical Analysis of Satisfaction Assessment After Penile Prosthesis Surgery. Sex Med Rev, 2017. 5(2): p. 244-251. 99- Carson, C.C., J.J. Mulcahy, and F.E. Govier, Efficacy, safety and patient satisfaction outcomes of the AMS 700CX inflatable penile prosthesis: results of a long-term multicenter study. AMS 700CX Study Group. J Urol, 2000. 164(2): p. 376-80. 100- Henry, G.D., et al., An outcomes analysis of over 200 revision surgeries for penile prosthesis implantation: a multicenter study. J Sex Med, 2012. 9(1): p. 309-15. 101- Serefoglu EC, McMahon CG, Waldinger MD, Althof SE, Shindel A, Adaikan G, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. J Sex Med. 2014 Jun;11(6):1423-41. doi: 10.1111/jsm.12524. Epub 2014 May 22. PMID:24848805. 102- Waldinger, M.D., et al. The use of old and recent DSM definitions of premature ejaculation in observational studies: a contribution to the present debate for a new classification of PE in the DSM-V. J Sex Med, 2008. 5: 1079. 103- cMahon CG. Clinical trial methodology in premature ejaculation observational, interventional, and treatment preference studies–part I–defining and selecting the study population. J Sex Med. 2008;5(8):1805–1816. 104- Arafa M, Shamloul R. Development and validation of the Arabic Index of Premature Ejaculation (AIPE). J Sex Med. 2007;4:1750–1756. 105- El-Sakka AI. Severity of erectile dysfunction at presentation: effect of premature ejaculation and low desire. Urology. 2008;71(1):94–98. 106- Althof SE, McMahon CG, Waldinger MD, et al. An update of the International Society of Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE). J Sex Med. 2014;11(6):1392–1422. 107- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. 108- Abdel-Hamid IA and Ali OI: Delayed Ejaculation: Pathophysiology, Diagnosis, and Treatment World J Mens Health 2018 January 36(1): 22-40. 109- Abdel-Hamid IA, Elsaied MA and Mostafa T. The drug treatment of delayed ejaculation. Transl Androl Urol 2016;5(4):576-591. 110- Burri A, Porst H. The relationship between penile deformity, age, psychological bother, and erectile dysfunction in a sample of men with Peyronie's Disease (PD). Int J Impot Res. 2018 Aug;30(4):171-178. doi: 10.1038/s41443-018-0029-3. Epub 2018 May 25. PMID: 29795530. 111- Zachalski W, Krajka K, Matuszewski M. Evaluation of the Treatment of Congenital Penile Curvature Including Psychosexual Assessment. J Sex Med. 2015 Aug;12(8):1828-35. doi: 10.1111/jsm.12933. Epub 2015 Jul 2. PMID: 26139203. 112- Paulis G, Romano G, Paulis A. Prevalence, psychological impact, and risk factors of erectile dysfunction in patients with Peyronie's disease: a retrospective analysis of 309 cases. Res Rep Urol. 2016 Jul 18;8:95-103. doi: 10.2147/RRU.S109319. PMID: 27486570; PMCID: PMC4958366. 113- Low P, Wang L, Li KD, Shibley WP, Cedars BE, Holler JT, Enriquez A, Sadeghi-Nejad H, Amend GM, Breyer BN. Thematic analysis of the psycho-sexual symptoms in patients with Peyronie's disease present on online forums. Int J Impot Res. 2022 Jun 16. doi: 10.1038/s41443-022-00589-x. Epub ahead of print. PMID: 35710605. 114- El-Sakka A. I. Medical, Non-invasive and Minimally Invasive Treatment for Peyronie’s Disease: A Systematic Review. Andrology. 2021; 9:511–528. https://doi. org/10.1111/andr.12927 115- Nehra A, Alterowitz R, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh JJ, et al. American Urological Association Education and Research, Inc., Peyronie's Disease: AUA Guideline. J Urol. 2015 Sep;194(3):745-53. doi: 10.1016/j.juro.2015.05.098. Epub 2015 Jun 9. PMID: 26066402; PMCID: PMC5027990. 116- Yang D, Hatzichristodoulou K, Hebert J, etal. Multi-Center Experience Utilizing Collagen Fleece for Plaque Incision with Grafting to Correct Residual Curvature at Time of Inflatable Penile Prosthesis Placement in Peyronie's Disease Patients. J Sex Med 2020;17:S27-120. 117- Lue TF, El-Sakka AI. Venous patch graft for Peyronie’s disease. Part I: Technique. J Urol 1998;160:2047-9. 118- Carson CC, Levine LA. Outcomes of surgical treatment of Peyronie’s disease. BJU Int 2014;113:704-13. 119- Montague, D., Jarow, J., Broderick, G., Dmochowski, RR., Heaton, JP., Lue, TF. et al. (2003) American Urological Association guideline on the management of priapism. J Urol 170: 1318–1324. 120- Bivalacqua, T. and Burnett, A. (2006) Priapism: new concepts in the pathophysiology and new treatment strategies. Curr Urol Rep 7: 497–502. 121- Lue, T., Hellstrom, W., McAninch, J. and Tanagho, E. (1986) Priapism: a refined approach to diagnosis and treatment. J Urol 136: 104–108. 122- Broderick, G., Kadioglu, A., Bivalacqua, T., Ghanem, H., Nehra, A. and Shamloul, R. (2010) Priapism: pathogenesis, epidemiology, and management. J Sex Med 7: 476–500. 123- Ralph, D., Garaffa, G., Muneer, A. Freeman, A., Rees, R., Christopher, AN. et al. (2009) The immediate insertion of a penile prosthesis for acute ischaemic priapism. Eur Urol 56: 1033–1038. 124- Emad A. Salem and Ola El Aasser Management of Ischemic Priapism by Penile Prosthesis Insertion: Prevention of Distal Erosion The Journal Of Urology JUNE 2010. 183, 2300-2303. 125- Yafi FA, Hellstrom WJG. Immediate Placement of Penile Prosthesis for the Management of Ischemic Priapism as First-line Treatment. Eur Urol Focus. 2019 Jul;5(4):531-532. doi: 10.1016/j.euf.2019.01.001. Epub 2019 Jan 11. PMID: 30639251. 126- Capece M, La Rocca R, Mirone V, Bivalacqua TJ, Castiglione F, Albersen M, Ralph DJ, Muneer A, Garaffa G. A Systematic Review on Ischemic Priapism and Immediate Implantation: Do We Need More Data? Sex Med Rev. 2019 Jul;7(3):530-534. doi: 10.1016/j.sxmr.2018.10.007. Epub 2019 Mar 19. PMID: 30898595.
|
- Annexes
Figure 1: Personalized Management Algorithm:
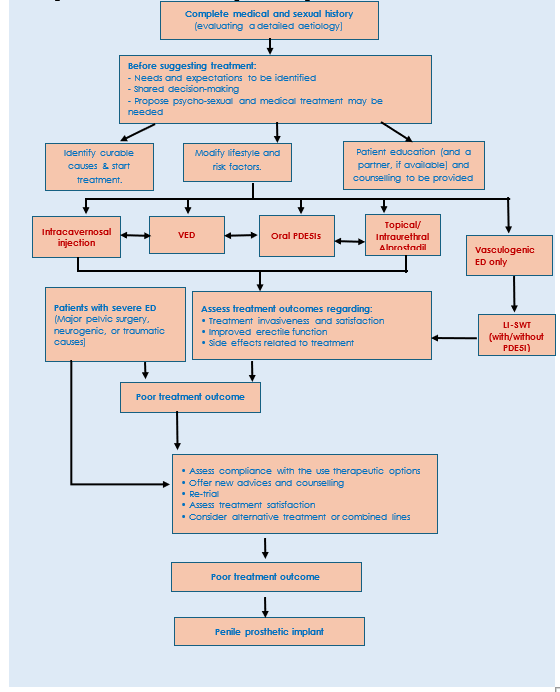
Figure
2: Management algorithm for
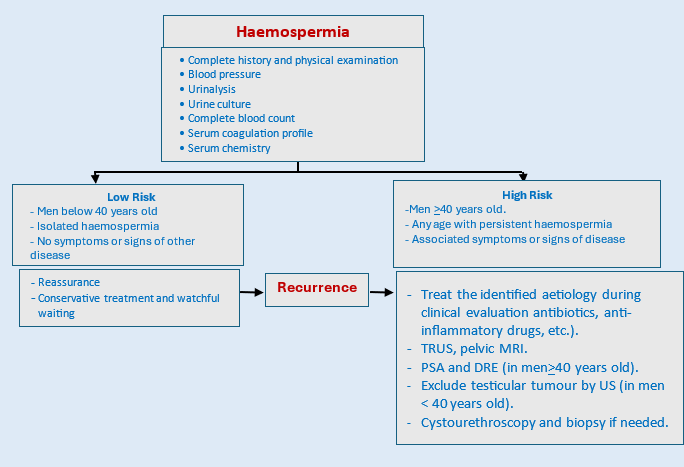
Table 4: Comparison of the properties of phosphodiesterase type 5 inhibitors (PDE5i) (42)
|
Property |
Sildenafil |
Tadalafil |
Vardenafil |
Avanafil |
|
|
TMAX |
30–120min |
30–360min |
30–120min |
30–45min |
|
|
Terminal half life |
4h |
17.5h |
4h |
6–17h |
|
|
Available doses |
25mg,50mg,100mg |
5mg,10mg,20mg |
5mg,10mg,20mg |
50mg,100mh,200mg |
|
|
Max dose |
100mg |
20mg |
20mg |
200mg |
|
|
Efficacy |
Each offer similar efficacy |
||||
|
Side effects (5 most common) |
Headache, flushing, dyspepsia, nasal congestion, alteration in color vision |
Headache, dyspepsia, back pain, myalgia, nasal congestion |
Headache, flushing, rhinitis, dyspepsia, sinusitis |
Headache, flushing, rhinitis, dyspepsia, sinusitis |
|
|
Use with α-blockers.
|
- Concomitant use of selective α-blockers does not present a risk for significant hypotension - There is a risk of significant hypotension when using non-selective α-blockers |
||||
|
Contraindications
|
- Regularly or intermittent use of organic nitrates. - Known hypersensitivity to any component of the tablet |
||||
|
Dose adjustments that may be needed |
· Patients aged > 65 years. · Hepatic impairment · Renal impairment · Concomitant use of potent cytochrome P450 3A4 inhibitors (e.g. ritonavir, cobicistat and erythromycin) · Concomitant use of cimetidine with sildenafil |
||||
|
TMAX = time to maximum plasma concentration. |
|||||
Table 5: Clinical History, Physical Examination, Laboratory Investigations and Radiologic Assessment in Different Types of Priapism (119,120).
|
Variant |
History and clinical examination |
Penile blood appearance |
Penile blood gas findings |
Color Duplex ultrasonography findings |
|
Ischemic priapism |
Tender and rigid corpora cavernosa |
Corpus cavernosum testing: blood is hypoxic and dark in color |
pO2> 30 mmHg pCO2>60 mmHg pH<7.25 |
Minimal or absent blood flow |
|
Nonischemic priapism |
Perineal or penile trauma; non tender, partially tumescent corpora cavernosa |
Corpus cavernosum testing: blood is oxygenated and red |
pO2<90 mmHg pCO2<40 mmHg pH=7.4 similar to normal arterial blood) |
Blood flow is normal to high in velocity |
|
Stuttering (recurrent) priapism |
Similar attacks |
Corpus cavernosum testing: blood is hypoxic and dark in color |
Blood gases: pO2<30 mmHg; pCO2>60 mmHg pH <7.25 |
Minimal or absent blood flow during acute priapism; normal blood flow otherwise |
|
pCO2, partial pressure of carbon dioxide; pO2, partial pressure of oxygen. |
||||
Table 6: Percutaneous distal shunts, open distal shunts, open proximal shunts, and vein anastomoses/shunts
|
Distal shunts |
|
Example |
Technique |
|
Percutaneous distal shunts |
Winter (corporoglanular) |
shunt large biopsy needle is inserted through glans |
|
|
Ebbehoj (corporoglanular) |
shunt #11 blade scalpel is percutaneously passed |
||
|
T shunt (corporoglanular shunt) |
Modified Ebbehoj using #10 blade scalpel and introducing the scalpel rotating it inside 90° |
||
|
Open distal shunt |
Al-Ghorab
|
A 1 cm incision is made distal to coronal sulcus with excision of 5 × 5 mm cone segment of distal tunica albuginea from each corporal body |
|
|
Burnett ‘snake’ maneuver
|
Modification of Al-Ghorab shunt. A Hegar dilator is used to evacuate ischemic blood through a distal tunical window |
||
|
Proximal shunts |
Open proximal shunt |
Quackels or Sacher (corporospongiosal) shunt
|
In lithotomy position, bulbocavernosus muscle is dissected from corpus spongiosum and 1 cm staggered ellipses of tissue are incised/excised from spongiosal/corporal bodies, and the defects anastomosed together |
|
Corporo saphenous vein or superficial/deep dorsal vein shunts |
Grayhack shunt
|
The saphenous vein is ligated and anastomosed with corpora cavernosa |
|
|
Barry shunt
|
The superficial or deep dorsal vein is ligated and anastomosed to the corpora cavernosa |