Articulation Disorders (Speech Sound Disorders)
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Articulation Disorders (Speech Sound Disorders) |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:03 PM |
Description
"last update: 29 August 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mahmoud Abdel Aziz,5 Mohamed Ghonaim,6 Tarek Ghanoum,7 Mahmoud Youssef8
Phoniatrics Chief Manager: Mahmoud Youssef8
Phoniatrics Executive Manager: Dalia Mostafa9
Assembly Board: Nirvana Gamal El Din Hafez Helmy,8 Rasha Shoeib,8 Yossra Abdel Naby Sallam10
Grading Board (In alphabetical order)
Ahlam Abdel Salam,11 Omayma Afsa,12 Ahmad Ali,13 Essam Eldin Aref,14 Ahlam A. N. El-Adawy,14 Asmaa El-Dessouky,15 Iman ElRouby,16 Safaa ElSady,8 Aisha Fawzy,9 Dalia Mostafa,9 Aya Sheikhany9
Reviewing Board: Hasnaa Othman,17 Yomna Hassan,8 Hedia Serry8 , Shaimaa Kabil18, Eatemad Nabil19
Ministry of health ECPG steering committee: Reda Kamel1, Ahmed Ragab2, Mahmoud Abdelaziz5, Mohamed Elsheikh5, Sherif Guindi20, Ali Mahrous21, Louay Sharkawy1, Saad Elzayat22, Ahmed Abu Elwafa23, Iman Sadek24, Mahmoud Yousef8, Samir Halim25, Ahmed Mustafa26, Ehab Seifein26, Ashraf Lotfy27, Mohamed Eltokhy28, Tamer Azzam28
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University,
2Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University,
3Otorhinolaryngology Department, Faculty of Medicine/ Minia University,
4Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University,
5Otorhinolaryngology Department, Faculty of Medicine/ Tanta University,
6Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University,
7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University,
8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/Ain Shams University,
9Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University,
10Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine for girls/ Al-Azhar University,
11Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Sohag University,
12Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University,
13Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University,
14Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Assuit University,
15Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University,
16Phoniatrics Unit, Otorhinolaryngology Department/ Hearing and Speech Institute,
17Phoniatrics Unit, Medical Studies for Children Center at the Faculty of Postgraduate Childhood Studies, 18Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine for girls/ Al Azhar University,
19 Pediatrics Department, Faculty of Medicine for girls/ Al Azhar University.
20 Otorhinolaryngology Dep. Faculty of Medicine/Fayoum University
21 Otorhinolaryngology Dep. Faculty of Medicine/Al Azhar University
22 Otorhinolaryngology Dep. Faculty of Medicine/Kafr El Shiekh University
23 Otorhinolaryngology Department, Faculty of Medicine/ Assiut University
24 Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University
25 Otorhinolaryngology Department Mataria Teaching Hospital
26 Otorhinolaryngology Department, Faculty of Medicine/ Hearing and Speech Institute
27 Otorhinolaryngology Department Secretariat of the Ministry of Defense,
28 Otorhinolaryngology Department Ministry of Interior Medical Services Sector
Specialties related to this guideline: Audiology and paediatrics
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Abbreviations
SSD speech sound disorders
GRADE Grading of Recommendations Assessment, Development and Evaluation- Executive Summary
1. How to identify speech sound disorders from organic causes of impaired speech production:
a. History taking: to exclude delayed developmental milestones, sensori-neural hearing loss, cleft palate, and dysarthria. (strong recommendation)
b. Thorough general and otolaryngological examination. (strong recommendation)
2. Speech sound assessment: formal language and articulation tests to assess language and phonology, followed by:
a. Phonetic transcription for the phonological errors and any special context where they occur. (strong recommendation)
b. Identify error pattern: omission, substitution, or distortion. (strong recommendation)
c. Stimulability. (strong recommendation)
d. Intelligibility. (strong recommendation)
3. Treatment options:
a. Contextual therapy: this approach utilizes that speech sounds are produced in syllable- based contexts in connected speech and some phonemic/phonetic contexts can facilitate correct production of a particular sound. (conditional recommendation)
b. Contrast therapy: minimal opposition, maximal opposition, or multiple opposition therapy. (strong recommendation)
c. Cycle approach: the child is provided with a practice on a given target for a predetermined period, before moving to another target for a predetermined period, and then cycles again. (strong recommendation)
d. Metaphone therapy: bringing about phonological change through increasing the metalinguistic awareness. (conditional recommendation)
e. Naturalistic intelligibility intervention: naturalistic intervention refers to the notion that phonological disorders should be corrected in communication situations that resemble everyday life. (strong recommendation)
- Introduction, scope and audience
➡️Introduction
Speech sound disorders include sound substitutions, omissions, distortions and additions 1.
➡️Scope
The scope of this guideline is to deduce speech sound disorders from other articulation disorders through a stepwise assessment plan and highlight the appropriate rehabilitation programs.
➡️Target audience
Phoniatricians, audiologists, pediatricians and family physicians.
- Methods
➡️Methods of development
Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Phoniatric Chief Manager, Phoniatric Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
➡️Search method
Electronic database searched:
Pubmed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar
➡️Keywords:
Speech sound disorders, Guidelines, Children
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Results
Three national Phoniatricians reviewed the available guidelines; Evidence based management of phonological Impairment 2004 2, University of N. Carolina 2006 3, Child Speech Disorder Research Network (CSDRN)2017 4, and Clinical guideline speech therapy 2019 5
The guidelines of University of North Carolina and Clinical guidance speech therapy gained the highest scores as regards currency, contents and quality and were thus adopted then adapted.
It was graded GRADE6 by eleven experts and reviewed by five expert reviewers to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
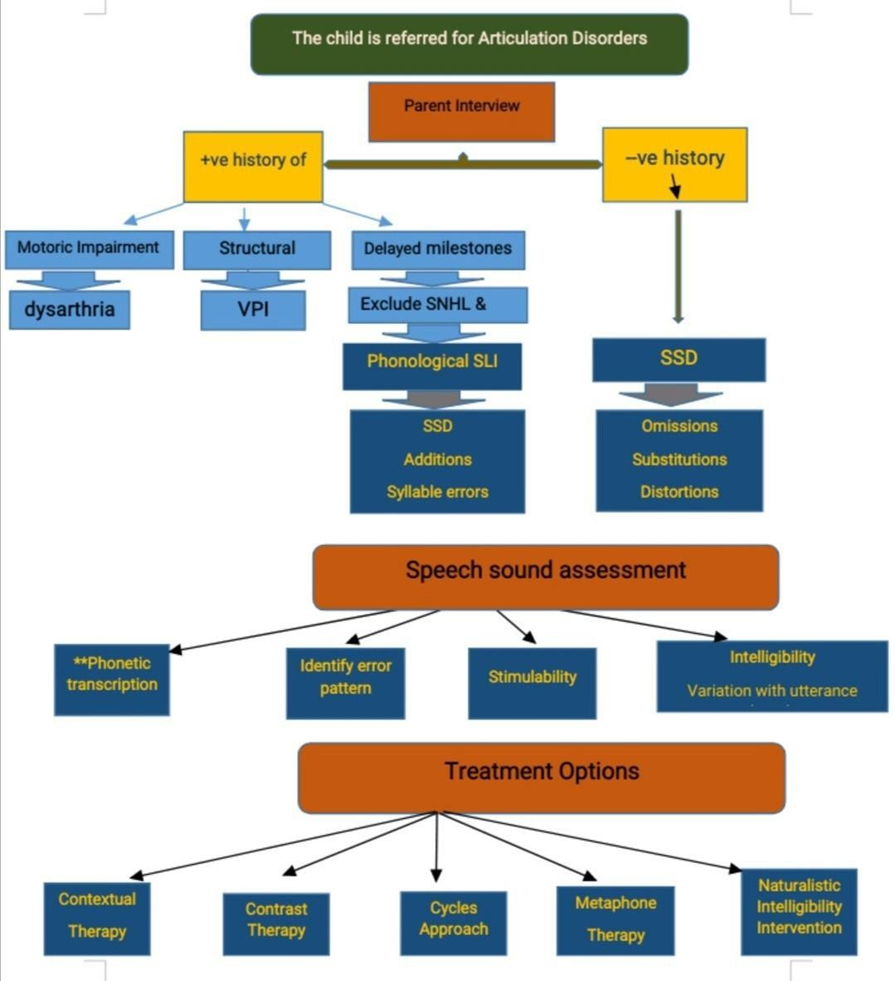
The following statements and flowchart were adapted from the Guidelines of University of North Carolina and Clinical guidance speech therapy which received the highest scores as regards the currency, contents, and quality.
Recommendations statements
|
Clinical questions |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Definition
Presentation
|
Speech sound disorders (SSD) include sound substitutions, omissions, distortions and additions. In addition, there can be errors that affect the word level and/or the rhythm and intonation characteristics of running speech. Speech sound disorders result from difficulties with speech, motor production and coordination of speech movements, as well as the lack of phonological knowledge or misapplication of the phonological rules associated with the child’s native language. All languages are governed by phonological rules which determine the appropriate speech sounds (or phonemes) and phoneme sequences that characterize a particular language. The cause of speech sound disorders in most children is unknown. The cause of some speech sound problems is known and can be the result of motor speech disorders (e.g., Apraxia and Dysarthria), structural differences (e.g., cleft-palate), syndromes (e.g., Down Syndrome) or sensory deficiencies (e.g., hearing loss). |
Low
High
High |
Strong recommendation
Strong recommendation
Conditional recommendation |
Cross sectional study
Systematic review
Systematic review |
1
7
7 |
|
Presentation
|
Apart from short term memory disorders, the exact cause of speech sound disorders in most children is unknown. The cause of other articulation disorders is known and can be the result of motor speech disorders (e.g., Apraxia and Dysarthria), structural differences (e.g., cleft-palate), syndromes (e.g., Down Syndrome) or sensory deficiencies (e.g., hearing loss). SSD have to be clearly differentiated from other organic articulation disorders as early as possible during preliminary diagnosis in order to direct the patient to the suitable diagnostic procedure |
High |
Strong recommendation |
Systematic review |
7 |
|
Clinical questions |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Risk factors.
Symptomatology
Assessment
|
• Gender-males being higher risk. • Ear, nose and throat problems. • Family history of speech and language problems. • Limited parental education/ learning support at home. • Omissions/deletions: Specific sounds are omitted or deleted (e.g., boo for book and geen for green). • Substitutions: One or more sounds are substituted (e.g., wed for red and dut for duck, widuh for rider). • Additions: One or more extra sounds are added into a word (e.g., bulack for black). • Distortions: Sounds are modified or altered (e.g., a slushy /s/). • Whole-word/syllable-level errors: Weak syllables are deleted (e.g., boon for balloon); a syllable is repeated or deleted (e.g., nana for candy). • Prosody errors: Errors that occur in stress, rhythm and intonation. Case history • Family history of speech/language difficulties. • Recurrent middle ear infections. • Child’s primary language used in the home. • Family and teacher concerns. • Age developmental milestones were met. • Medical history. |
High
High
Low |
Strong recommendation
Strong recommendation
Strong recommendation
|
Systematic review
Systematic review
Cohort study |
7
7
8
|
Clinical questions |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Assessment
|
Oral mechanism examination includes: • Assessment of dentition and alignment of teeth • Muscle movement as well as development of the jaw, lips and tongue and the integrity of the oral structures (hard and soft palate, jaw, maxilla, lips and tongue) • Oral motor reflexes as well as purposeful movement through imitation of non- speech actions • Diadokokinetic rate: muscle movement for coordination and sequencing • Assessment of tongue and mouth resting posture to determine existence of tongue thrust |
low
High |
Strong recommendation
strong recommendation
|
Cohort study
Systematic review |
8
9 |
|
Clinical questions |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Assessment Audiological assessment
Speech Sound Assessment
Assessment Stimulability
|
Will be provided to children during the initial Speech and Language Evaluation unless results of a comprehensive audiological assessment has already been completed. Follow up audiological assessment is indicated when progress in speech development has not been achieved or is mini- mal and evidence suggests risk for hearing im- pairment. The evaluation process may include the selec- tion of administration of standardized tests, lan- guage/speech samples, or a descriptive analysis of informal findings. Assess articulation at the word, phrase and con- versational levels. Establish a phonetic inventory for the child (i.e., what sounds can the child produce?). Identify the error patterns the child uses and look for phonological process use in children who are less intelligible. Identify speech sound production inconsisten- cies. The child does not always misarticulate the error sound the same way in all words. Evaluate stimulability of error sounds. Evaluate intelligibility. Child’s ability to produce target sounds with cues • Used to select treatment targets based on the child’s ability to utilize these cues • Assists in determining prognosis. |
High
Low
low |
Strong recommendation
Strong recommendation
Strong recommendation
|
Systematic review
Cohort study
Cohort study |
10
8
8 |
|
Clinical questions |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Intelligibility
|
Intelligibility refers to the listener’s ability to understand the child’s speech. A guideline for expected conversational intelligibility levels of typically developing children talking to unfamiliar listeners is summarized below • 1 year- 25% intelligible • 2 year- 50% intelligible • 3 year- 75% intelligible • 4 year- 100% intelligible Intelligibility can be impacted by several factors including: • Length of utterance • Familiarity with child’s speech. • Child’s speech rate, intonation, loudness level, vocal quality and fluency • Contextual cues • Presence of ambient noise during conversation. |
Low |
Strong recommendation
|
Comparative study |
11 |
|
Onset of intervention
|
If SSD is not attributed to any other communication disorder, intervention should be started at the age of 5-6 years. Therapy should be postponed to give chance for completing the phonemic inventory and disappearance of all phonological processes including devoicing |
low |
Conditional recommendation
|
Cohort study |
12 |
|
Intervention Contextual utilization
Contrast therapy
|
Treatment starts with practicing syllable based contexts in which the sound is produced correctly. That syllable is used to train more difficult productions. For example, a /s/ may be more easily produced in the syllable with a high front vowel. Targets focus on a specific phoneme feature using contrasting word pairs. Minimal pairs are different by one feature or phoneme that changes the word meaning (tip vs. ship). Maximal pairs use a sound target differing by several distinctive features which affect phoneme placement and manner to introduce sounds that the child cannot produce ( beat vs. cheat) |
Low
High |
Conditional recommendation
Strong recommendation
|
Cohort study
Systematic review |
13
14 |
|
Clinical questions |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Core vocabulary approach
Cycles approach
Distinctive features approach
|
Used with children who are highly unintelligible due to inconsistent misarticulations and may not respond well to traditional therapy. This is a word-based approach as opposed to a phoneme-based technique. Words the child commonly uses are selected for practice and feedback is provided to reinforce the most accurate production of each word. Focuses on improving phonological patterns with a strategy similar to normal sound acquisition. It is used with children who have poor intelligibility, characterized by numerous omissions and limited phonemic inventories. Each cycle targets all phonological patterns in error until they emerge in spontaneous speech.
Focuses on sound features the child cannot produce (nasals, fricative, voicing, placement) and is usually used with children who substitute. sounds. Error patterns are targeted using tasks such as minimal pair contrasts; usually once a contrast pattern emerges, it can be generalized. to other sounds that share the same feature. |
low
High
High |
Conditional recommandation
Conditional recommandation
Strong recommendation
|
Case study
Systematic review
Systematic review |
15
16
14 |
|
Clinical question |
Action recommendation |
Evidence quality |
Strength of recommendation |
Study type |
References |
|
Metaphone therapy
Naturalistic Speech Intelligibility Intervention
Speech sound Perception Training
|
Used with children who appear to have not mastered phonological system rules. Examples are descriptive and provide information about how a sound is produced, e.g., voiced (noisy) vs. voiceless (quiet). Sounds most impacting intelligibility are selected first. Uses everyday activities to elicit the target sound frequently during the session. For example, the child is asked about a toy that involves responses using the targeted sound. (i.e., “What color is the car?” “Red.”) Appropriate productions are recast (i.e., casually modeled by the clinician or parent). Speech perception tasks are used to help the child gain a consistent perception of the target sound. Tasks may include auditory bombardment and sound identification tasks. Usually used prior to or at the same time as speech production intervention. |
Low
Low
High |
Conditional recommendation
Strong recommendation
Strong recommendation |
Cohort study
Cohort study
Systematic review |
17
18
14 |
- Implementation considerations
Implementation:
The adapted guideline will be freely disseminated through both print and electronic versions as a portable document format (PDF) and through workshops and national conferences of ENT, Audio-Vestibular Medicine, Phoniatrics and related specialties.
Identification of potential barriers and facilitating factors through checklists with printed and electronic versions.
A guideline summary is provided together with a flowchart.
- Research needs
There is a need to conduct comparative studies to highlight the most effective therapy program.
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria
The clinicians should be able to:
- Differentiate between all disorders of articulation
- Exclude organic defects or sensory disabilities
- Seek appropriate help from other specialities when needed
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. American Speech-Language Hearing Association. Schools Survey report: Caseload characteristics. Rockville, MD: Author, 2006.
2. Baker E, McLeod S. Evidence-based management of phonological impairment in children. Journal of child language teaching and therapy. 2004; 261-285.
3. North Carolina Guidelines for Speech-Language Pathology Services in Schools, 2006.
4. Child Speech Disorder Research Network October, Good practice guideline for the analysis of child’s speech. 2017
5. Clinical guideline Speech therapy version 10, Regence speech service guideline. 2019
6. Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook. https://gdt.gradepro.org/app/ handbook/handbook.html. 2013
7. Fey, M. Clinical forum: Phonological assessment and treatment. Articulation and phonology: inextricable constructs in speech pathology. Journal of language, speech, and hearing services in schools, 1992: 23, 225-232,
8. Miccio, A. Clinical problem solving: assessment of phonological disorders. American journal of speech-language pathology, 2002: 11, 221-229.
9. Wong, E., Wong, M. and Velleman, S.: Assessment and diagnostic standards of apraxia of speech in Chinese-speaking adults and children: A scoping review; American journal of speech and languae pathology, 2023.
10. Drosos, K., Papanicolaou, A., Voniati, L., Panayidou, K. and Thodi, C.: Auditory processing and speech sound disorders; Journal of brain sciences, 2014; 14(3): 291-295.
11. Flipsen, P. Measuring the intelligibility of conversational speech in children, Clinical Linguistics and Phonetics, 2006 Jun; 20(4):303-12.
12. Tobolcea, I. and Danubianu, M. : Computer-based programs in speech therapy of dyslalia and dyslexia-dysgraphia, BRAIN. Broad Research in Artificial Intelligence and Neuroscience, 2010 April: 1(2) “Happy Spring 2010”
13. Bleile, K. Evaluating Articulation and Phonological Disorders When the Clock Is Running, American Journal of Speech-Language Pathology, 2002 Aug: 11(3): 243-249.
14. Wren, Y., Harding, S., Goldbart, J. and Roulstone, S. A systematic review and classification of interventions for speech-sound disorder in preschool children, International journal of language and communication disorders, 2018 May; 53(3): 446-467.
15. Dodd, B., Holm, A., Crosbie, S. and Mcintosh, B. A core vocabulary approach for management of inconsistent speech disorder, Advances in Speech–Language Pathology, September 2006; 8(3): 220 – 230
16. Arabi, A., Jalilevand, N. and Marefati, A. A Review on Evidence-Based Treatment in Phonological Interventions With Emphasis on Cycles Approach, Journal of Modern Rehabilitation, June 2018; 11(4):196.
17. Dean, E., Howell, J., Grieve, R. and Donaldson, M. Harnessing language awareness in a communicative context: a group study of the efficacy of Metaphon, International Journal of Language & Communication Disorders, April 2011; 30(S1):281 – 286.
18. Camarata, S. The application of naturalistic conversation training to speech production in children with speech disabilities, Journal of applied behavioral analysis, 1993; 26(2):173-82.
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
Annex 1: Articulation disorders Flowchart
Annex 2: Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
1- Currency (table 1)
|
Number |
Responsible Organization |
Date of Publication |
Review Date |
Original Details Date |
|
CPG1 |
Child lang. Teach. & Therapy |
2004 |
NR |
2001 |
|
CPG2 |
University of N Carolina |
2006 |
NR |
2011 |
|
CPG3 |
CSDRN |
2017 |
NR |
2013-2017 |
|
CPG4 |
Evicore |
2019 |
Annually |
2015-2018 |
2- Content (table 2)
|
Guideline 1 |
Guideline 2 |
Guideline 3 |
Guideline 4 |
|
|
Criteria |
Evidence-based management of ph. impairment 2004 |
University of N. Carolina 2006 |
Child Speech Disorder Research Network 2017 |
Clinical guideline Speech therapy 2019 |
|
Credibility |
9 |
8 |
5 |
8 |
|
Observability |
4 |
3 |
5 |
3 |
|
Relevance |
5 |
9 |
7 |
9 |
|
Relative advantage |
6 |
7 |
5 |
7 |
|
Easy to install and understand |
8 |
9 |
8 |
9 |
|
Compatibility |
6 |
9 |
7 |
8 |
|
Testability |
5 |
8 |
9 |
9 |
|
Total |
43 |
53 |
46 |
53 |
3- Quality (table 3)
|
Domain |
CPG1 |
CPG2 |
CPG3 |
CPG4 |
|
Transparency |
A |
A |
A |
A |
|
Conflict of Interest |
NR |
NR |
NR |
NR |
|
Development Group |
C |
C |
C |
C |
|
Systematic Review |
A |
A |
B |
B |
|
Grade of Evidence |
B |
B |
B |
C |
|
Recommendations |
C |
A |
B |
B |
|
External Review |
NR |
NR |
NR |
A |
|
Update |
C |
B |
B |
A |
|
CPG2: 3A, 2B, 1C, 2NR CPG4: 3A, 2B, 2C, 1NR |
||||
Annex 3: The risks and benefits of added and/or modified statements
|
Statement |
Risk |
Benefit |
|
Apart from short term memory disorders, the exact cause of speech sound disorders in most children is unknown. The cause of other articulation disorders is known and can be the result of motor speech disorders (e.g., Apraxia and Dysarthria), structural differences (e.g., cleft-palate), syndromes (e.g., Down Syndrome) or sensory deficiencies (e.g., hearing loss). SSD have to be clearly differentiated from other organic articulation disorders as early as possible during preliminary diagnosis in order to direct the patient to the suitable diagnostic procedure |
Late diagnosis and subsequently interference leads to development of disarticulation strategies that will postpone response to therapy program later on. |
Early identification of the cause of articulation disorders (other than SSD) helps to manage the underlying cause in the developmental period. |
|
If SSD is not attributed to any other communication disorder, intervention should be started at the age of 5-6 years. Therapy should be postponed to give chance for completing the phonemic inventory and disappearance of all phonological processes including devoicing |
Interference before completion of phonemic inventory is not effective in most cases |
Waiting for phonemic inventory completion is important to facilitate targeting the correct place and manner of articulation of the affected phoneme |













