Benign paroxysmal positional vertigo (ECPG)
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Benign paroxysmal positional vertigo (ECPG) |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:06 PM |
Description
"last update: 27 August 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdel Aziz,6 Tarek Ghanoum,7 Mahmoud Yousef8
Audiology Executive Manager: Iman El-Danasoury9
Assembly board: Nagwa Hazzaa,9 Mohamed El Badry,10 Nahla Gad,11 Lamees El-Amragy9
Grading Board (In alphabetical order)
Adel Abdel Maksoud,9 Abeir Dabbous,7 Iman El Adawi,12 Iman El-Danasoury,9 Tarek ElDessouky,13 Mai El Gohary,14 Wafaa El Kholy,9 Trandil El Mehallawi,15 Enass Sayed,16 Reham Elshafei,17 Amira El Shennawy,7 Naema Ismail,12 Enaas Kolkaila,15 Rabab Koura,13 Salwa Mahmoud,14 Radwa Mahmoud,18 Soha Mekki,11 Iman Mostafa,13 Mona Mourad,19 Abir Omara,14 Mohamed Salama,16 Hesham Sami,10 Hesham Taha,9 Somia Tawfik,9 Ragaey Youssef13
Reviewers: Mohamed Shabana,7 Alaa Abou-Setta,20 Hossam A.Ghaffar21,Mohammed A. Gomaa22, Sayed Sobhy Sayed23
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 3Otorhinolaryngology Department, Faculty of Medicine/Minia University, 4Otorhinolaryngology Department, Faculty of Medicine/ Bani- Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 6Otorhinolaryngology Department, Faculty of Medicine/Tanta University, 7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University,10 Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Minia University, 11Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Zagazig University, 12Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Al Azhar University, 13Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Bani-Suef University, 14Audiovestibular Unit, Otorhinolaryngology Department/ Hearing and Speech Institute, 15Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 16Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 17Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Fayoum University,18Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Banha University, 19Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Alexandria University, 20Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Suez Canal University, 21Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Helwan University.22 Professor of Otorhinolaryngology, Faculty of Medicine /Minia University. 23 Professor of Neurology, Faculty of Medicine/ Fayoum University
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Abbreviations
AAO-HNS American Academy of Otolaryngology—Head and Neck Surgery
BPPV Benign paroxysmal positional vertigo
BPPN Benign paroxysmal positional nystagmus
CRP Canalith repositioning procedure
MD Meniere’s Disease
VR Vestibular rehabilitation- Executive Summary
Clinicians should diagnose posterior semicircular canal BPPV when vertigo associated with torsional, up beating nystagmus is provoked by the Dix-Hall pike maneuver, performed by bringing the patient from an upright to supine position with the head turned 45° to one side and neck extended 20° with the affected ear down. The maneuver should be repeated with the opposite ear down if the initial maneuver is negative. (Strong recommendation)
If the patient has a history compatible with BPPV and the Dix-Hallpike test exhibits horizontal or no nystagmus, the clinician should perform, or refer to a clinician who can perform, a supine roll test to assess for lateral semicircular canal BPPV. (Strong recommendation)
Clinicians should differentiate, or refer to a clinician who can differentiate, BPPV from other causes of imbalance, dizziness, and vertigo. (Strong recommendation)
Clinicians should assess patients with BPPV for factors that modify management, by the recommended repositioning maneuvers, including impaired mobility or balance, central nervous system disorders, a lack of home support, and/or increased risk for falling. (Strong recommendation)
Clinicians should not obtain radiographic imaging in a patient who meets diagnostic criteria for BPPV. (Strong recommendation against)
Clinicians should not order laboratory vestibular testing in a patient who meets diagnostic criteria for BPPV in the absence of additional vestibular signs and/or symptoms inconsistent with BPPV that warrant testing. Vestibular testing may be ordered in case of recurrence, persistence of complaint after repositioning manoeuvre or in the presence of atypical nystagmus (Conditional recommendation against)
Clinicians should treat, or refer to a clinician who can treat, patients with posterior canal BPPV with a canalith repositioning procedure. Epley’s or Semont’s are equivocally effective for posterior canal BPPV. Semont’s is recommended in cupulolithiasis than Epley’s. (Strong recommendation)
The barbecue roll manoeuvre or Gufoni manoeuvre appear moderately effective for the geotropic form of lateral semi-circular canal BPPV. (Conditional recommendation)
Clinicians may not routinely recommend post procedural postural restrictions after canalith repositioning procedure for posterior canal BPPV. Post procedural postrural restriction might be recommended in selected cases as in failure (or repeated failure) of the repositioning maneuvers, recurrent cases, or cases associated with other vestibular pathology as MD or vestibular Migraine. (Conditional recommendation against)
1-2 sessions would resolve the condition in 87-100% of patients. A minority would require a 3ed trial. Otherwise persistent BPPV is suspected. (Strong recommendation)
Clinicians should start with CRP (or modified) even in those patients who are very obese; have severe cervical or lumber discs; or upon patient’s preference. In the latter case patients should be instructed to avoid activities that may increase the risk of falls until symptoms resolve. (Strong recommendation)
Clinicians may offer observation with follow up only if there is difficulty in performing successful manoeuvre after trials in some patients as : very obese; severe cervical or lumber discs; or upon patient’s preference not to repeat the manoeuvre. (Strong recommendation)
VR should be considered an option in the treatment of BPPV rather than a recommended first-line treatment modality. Home based Brandt-Daroff exercises is indicated in patients with persistent dizziness or imbalance after successful CRP or patients who refuse CRP.A more comprehensive customized VR program is indicated in patients with other vestibular pathology or with comorbid impairments that require balance rehabilitation specially in elderly. (Strong recommendation)
Clinicians should not treat BPPV with vestibular suppressant medications such as antihistamines and/ or benzodiazepines. Exceptions: Prior to CRP in patients with severe nausea and/or vomiting, or patients previously manifested severe nausea and/or vomiting during testing. (Strong recommendation against)
Clinicians should reassess patients within an initial period of observation following the canalith repositioning procedure (40 minutes up to one week) to document resolution, need for repetition of CRP session or persistence of symptoms. (Strong recommendation)
Clinicians should evaluate, or refer to a clinician who can evaluate, patients with persistent symptoms for unresolved BPPV and/or underlying peripheral vestibular or central nervous system disorders. (Strong recommendation)
Clinicians should educate patients regarding the impact of BPPV on their safety, the potential for disease recurrence, and the importance of follow-up. (Strong recommendation)
- Introduction, scope and audience
➡️ Introduction
➡️ Scope
The scope of the guideline is the diagnosis and management of BPPV. The guideline is required to increase the skills of all target specialists for proper diagnosis of cases of positional vertigo and avoid faulty diagnosis
➡️ Target audience
Audiovestibular physicians
Otolorhinolaryngologist
Neurologist
Physical Therapist
- Methods
Methods of development
➡️Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Audiology Chief Manager, Audiology Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️ Search Method
Electronic database searched:
Pubmed, Medline, and Medscape
➡️ Keywords
Benign paroxysmal positional vertigo; Otoconia; Utricle; repositioning maneuvers
➡️ Time period searched: June 2015 to December 2018.
➡️ Results
Four national audio-vestibular experts reviewed the guidelines available. Guidelines from the American Academy of Otolaryngology—Head and Neck Surgery (2018) gained the highest scores as regards currency, contents and quality
It was graded GRADE by twenty six experts and reviewed by three expert reviewers to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks
(GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
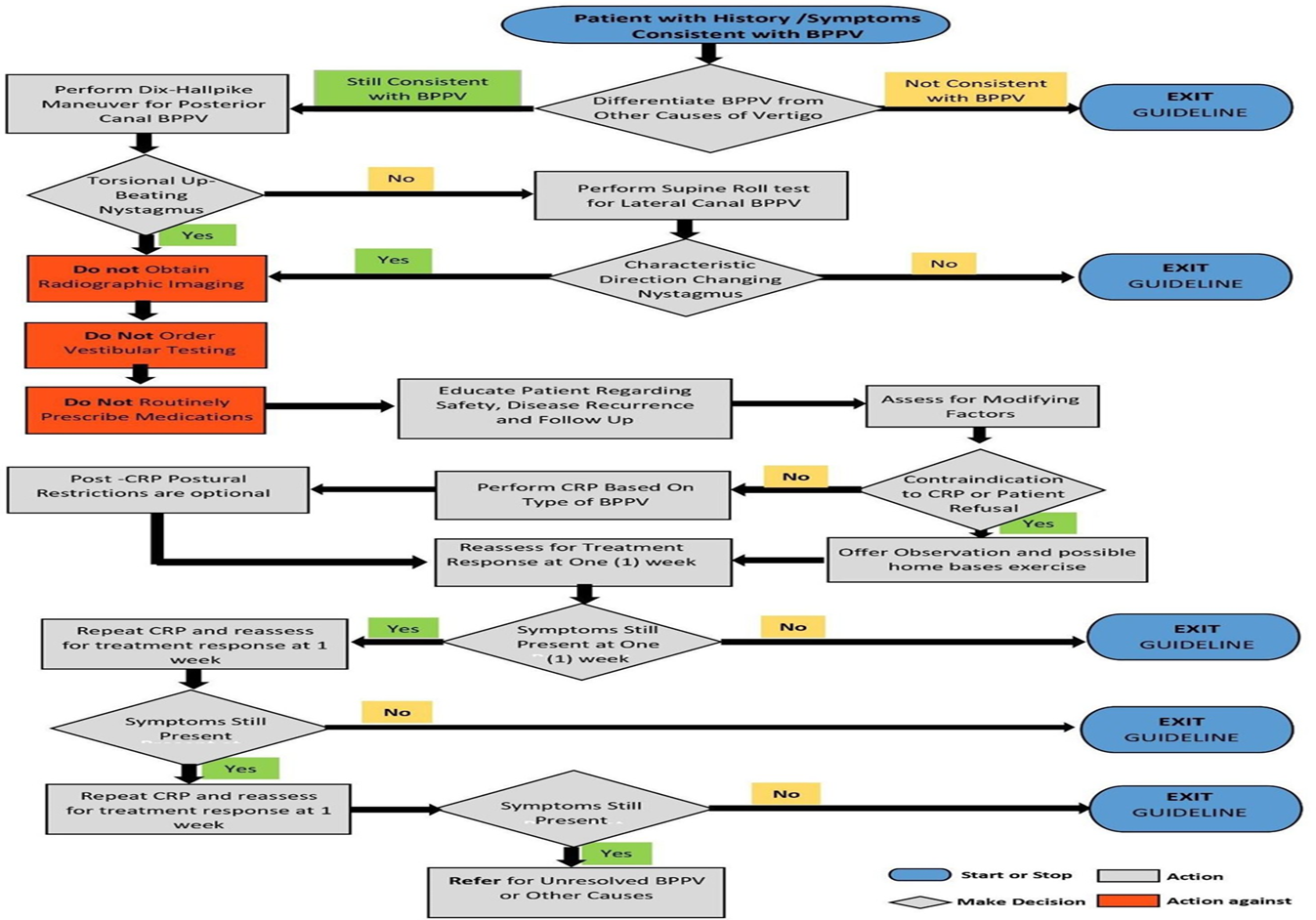
The following statements and flowchart were adapted from the Guidelines from American Academy of Otolaryngology—Head and Neck Surgery which received the highest scores as regards the currency, contents, and quality.
Recommendations statements
|
Statement topic |
Egyptian Recommendation |
Evidence Quality |
Strength of Recommendations |
Study type |
Reference |
|
1.Diagnosis of posterior semicircular canal BPPV
|
Clinicians should diagnose posterior semicircular canal BPPV when vertigo associated with torsional, up beating nystagmus is 45° to one side and neck extended 20° with the affected ear down. The maneuver should be repeated with the opposite ear down if the initial maneuver is negative. |
Moderate |
Strong Recommendation |
Diagnostic study with minor limitation |
Honrubia V, Baloh RW, Harris MR, et al. Paroxysmal positional vertigo syndrome. Am J Otol. 1999;20:465-470. |
|
2.Diagnosis of lateral (horizontal) semicircular canal BPPV
|
If the patient has a history compatible with BPPV and the Dix-Hallpike test exhibits horizontal or no nystagmus, the clinician should perform, or refer to a clinician who can perform, a supine roll test to assess for lateral semicircular canal BPPV. |
Moderate |
Strong Recommendation |
Diagnostic study with minor limitation |
Baloh RW, Jacobson K, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology. 1993;43:2542-2549. |
|
3.Differential diagnosis
|
Clinicians should differentiate, or refer to a clinician who can differentiate, BPPV from other causes of imbalance, dizziness, and vertigo. |
Low |
Strong Recommendation |
Observational study |
Kentala E, Rauch SD. A practical assessment algorithm for diagnosis of dizziness. Otolaryngol Head Neck Surg. 2003;128:54-59. |
|
4.Modifying factors
|
Clinicians should assess patients with BPPV for factors that modify management ,by the recommended repositioning maneuvers, including impaired mobility or balance, central nervous system disorders, a lack of home support, and/or increased risk for falling. |
Low |
Conditional Recommendation |
Observational study |
Lawson J, Johnson I, Bamiou DE, et al. Benign paroxysmal positional vertigo: clinical characteristics of dizzy patients referred to a Falls and Syncope Unit. QJM. 2005;98:357-364. |
|
5.Radiographic testing
|
Clinicians should not obtain radiographic imaging in a patient who meets diagnostic criteria for BPPV. |
Low |
Strong Recommendation (against) |
Observational study |
Turski P, Seidenwurm D, Davis P; American College of Radiology. Expert Panel on Neuroimaging: Vertigo and Hearing Loss. Reston, VA: American College of Radiology; 2006. |
|
6.Vestibular testing
|
Clinicians should not order laboratory vestibular testing in a patient who meets diagnostic criteria for BPPV in the absence of additional vestibular signs and/or symptoms inconsistent with BPPV that warrant testing. Vestibular testing may be ordered in case of recurrence, persistence of complaint after repositioning manoeuvre or in the presence of atypical nystagmus . |
Low |
Conditional Recommendation (against) |
Observational study |
Baloh RW, Honrubia V, Jacobson K. Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology. 1987;37:371-378 |
|
7.Repositioning procedures as initial therapy (a)
|
Clinicians should treat, or refer to a clinician who can treat, patients with posterior canal BPPV with a canalith repositioning procedure. Epley’s or Semont’s are equivocally effective for posterior canal BPPV. Semont’s is recommended in cupulolithiasis than Epley’s. |
High |
Strong Recommendation |
Well designed RCT and systemic review with meta-analysis |
Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014;(12):CD003162.
Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E. Meta-analysis on the efficacy of Epley’s manoeuvre in benign paroxysmal positional vertigo. Neurologia. 2010;25:295-299. |
|
8.Repositioning procedures as initial therapy (b)
|
The barbecue roll maneuver or Gufoni maneuver appear moderately effective for the geotropic form of lateral semicircular canal BPPV. |
Moderate |
Conditional Recommendation |
RCT |
Kim JS, Oh S-Y, Lee S-H, et al. Randomized clinical trial for geotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;79:700-707. |
|
9.Post procedural restrictions
|
Clinicians may not routinely recommend post procedural postural restrictions after canalith repositioning procedure for posterior canal BPPV. Post procedural postrural restriction might be recommended in selected cases as in failure (or repeated failure) of the repositioning maneuvers, recurrent cases, or cases associated with other vestibular pathology as MD or vestibular Migraine. |
High |
Conditional Recommendation (against) |
Diagnostic study with minor limitation
Well-designed RCT |
Roberts RA, Gans RE, DeBoodt JL, et al. Treatment of benign paroxysmal positional vertigo: necessity of postmaneuver patient restrictions. J Am Acad Audiol. 2005;16:357-366.
Balikci HH, Ozbay I. Effects of postural restriction after modified Epley maneuver on recurrence of benign paroxysmal positional vertigo. Auris Nasus Larynx. 2014;41:428-431. |
|
10.Number of CRP repetitions
|
1-2 sessions would resolve the condition in 87-100% of patients. A minority would require a 3ed trial. Otherwise persistent BPPV is suspected. |
Low |
Strong Recommendation |
Observational study |
Kentala E, Pyykkö I. Vertigo in patients with benign paroxysmal positional vertigo. Acta Otolaryngol Suppl. 2000;543:20-22.
|
|
11.If there is difficulty in performing successful maneuver
|
Clinicians should start with CRP (or modified) even in those patients who are very obese; have severe cervical or lumber discs; or upon patient’s preference. In the latter case patients should be instructed to avoid activities that may increase the risk of falls until symptoms resolve. |
Low |
Strong Recommendation |
Observational study |
Kerber KA. Benign paroxysmal positional vertigo: opportunities squandered. Ann N Y Acad Sci. 2015;1343:106-112. |
|
12.Observation as initial therapy
|
Clinicians may offer observation with follow up only if there is difficulty in performing successful maneuver after trials in some patients as : very obese; severe cervical or lumber discs; or upon patient’s preference not to repeat the maneuver. |
Low |
Strong Recommendation |
Observational study |
Kerber KA. Benign paroxysmal positional vertigo: opportunities squandered. Ann N Y Acad Sci. 2015;1343:106-112.
|
|
Statement topic |
Egyptian Recommendation |
Evidence Quality |
Strength of Recommendations |
The statement is based up on: |
|
|
13.Vestibular rehabilitation
|
VR should be considered an option in the treatment of BPPV rather than a recommended first-line treatment modality. Home based Brandt-Daroff exercises is indicated in patients with persistent dizziness or imbalance after successful CRP or patients who refuse CRP.A more comprehensive customized VR program is indicated in patients with other vestibular pathology or with comorbid impairments that require balance rehabilitation specially in elderly. |
Moderate |
Strong Recommendations |
Systemic review |
Hillier SL, Hollohan V. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2007;(4):CD005397. |
|
14.Medical therapy
|
Clinicians should not treat BPPV with vestibular suppressant medications such as antihistamines and/ or benzodiazepines. Exceptions: Prior to CRP in patients with severe nausea and/or vomiting, or patients previously manifested severe nausea and/or vomiting during testing. |
Moderate |
Strong Recommendation (against) |
Diagnostic study with minor limitation |
Fujino A, Tokumasu K, Yosio S, et al. Vestibular training for benign paroxysmal positional vertigo: its efficacy in comparison with antivertigo drugs. Arch Otolaryngol Head Neck Surg. 1994;120:497-504. |
|
14.Outcome assessment
|
Clinicians should reassess patients within an initial period of observation following the canalith repositioning procedure ( 40 minutes up to one week) to document resolution, need for repetition of CRP session or persistence of symptoms. |
Very low |
Strong Recommendation |
Observational study |
Sekine K, Imai T, Sato G, et al. Natural history of benign paroxysmal positional vertigo and efficacy of Epley and Lempert maneuvers. Otolaryngol Head Neck Surg. 2006;135:529-533. |
|
15.Evaluation of treatment failure
|
Clinicians should evaluate, or refer to a clinician who can evaluate, patients with persistent symptoms for unresolved BPPV and/or underlying peripheral vestibular or or central nervous system disorders. |
Low |
Strong Recommendation |
Observational study |
Buttner U, Helmchen C, Brandt T. Diagnostic criteria for central versus peripheral positioning nystagmus and vertigo: a review. Acta Otolaryngol. 1999;119:1-5. |
|
16.Patient Education
|
Clinicians should educate patients regarding the impact of BPPV on their safety, the potential for disease recurrence, and the importance of follow-up. |
Low |
Strong Recommendation |
Observational study |
Brandt T, Dieterich M. Vestibular falls. J Vestib Res. 1993;3:3-14. |
- Research needs
No need for new study to confirm our choice of statements
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria
The audiovestibular physicians should:
· Search for spontaneous nystagmus
· Perform oculomotor tests (gaze, smooth pursuit, and saccading testing)
· Perform Dix-Hallpike test and other positional tests properly
· Proper diagnosis of the side (right vs left), canal affected, and type of BPPV (canalolithiasis vs. Cupulolithiais).
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol. 1980;106:484-485.
2. Brandt T, Steddin S, Daroff RB. Therapy for benign paroxysmal positioning vertigo, revisited. Neurology. 1994;44:796-800.
3. Gordon CR, Shupak A, Spitzer O, et al. Nonspecific vertigo with normal otoneurological examination: the role of vestibular laboratory tests. J Laryngol Otol. 1996;110:1133-1137.
4. Kentala E, Pyykkö I. Vertigo in patients with benign paroxysmal positional vertigo. Acta Otolaryngol Suppl. 2000;543:20-22.
5. Oghalai JS, Manolidis S, Barth JL, et al. Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000;122:630-634.
6. Casani AP, Vannucci G, Fattori B, et al. The treatment of horizontal canal positional vertigo: our experience in 66 cases. Laryngoscope. 2002;112:172-178.
7. Cohen HS, Kimball KT. Treatment variations on the Epley maneuver for benign paroxysmal positional vertigo. Am J Otolaryngol. 2004;25:33-37.
8. Gamiz MJ, Lopez-Escamez JA. Health- related quality of life in patients over sixty years old with benign paroxysmal positional vertigo. Gerontology. 2004;50:82-86.
9. Prokopakis EP, Chimona T, Tsagournisakis M, et al. Benign paroxysmal positional vertigo: 10- year experience in treating 592 patients with canalith repositioning procedure. Laryngoscope. 2005;115:1667-1671.
10. White J, Savvides P, Cherian Net al. Canalith repositioning for benign paroxysmal positional vertigo. Otol Neurotol. 2005;26:704-710.
11. Cakir BO, Ercan I, Cakir ZA, et al. What is the true incidence of horizontal semicircular canal benign paroxysmal positional vertigo? Otolaryngol Head Neck Surg. 2006;134:451-454.
12. Phillips JS, FitzGerald JE, Bath AP. The role of the vestibular assessment. J Laryngol Otol. 2009;123:1 212-1215.
13. Breverna MV, Bertholon BP, Brand TC, et al. Benign paroxysmal positional vertigo: Diagnostic criteria. Consensus document of the Committee for the Classification of Vestibular Disorders of the Bárány Society Journal of Vestibular Research 2015;25:105–117.
14. Howick, J, Chalmers, I, Glasziou; OCEBM Levels of Evidence Working Group. The Oxford 2011 levels of evidence. http://www.cebm.net/index.aspx?o=5653. Accessed October 22, 2015.
15. McDonnell MN, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2015;(1):CD005397.
16. Takao I, Noriaki T, Tetsuo I, et al. Classification, diagnostic criteria and management of benign paroxysmal positional vertigo. Committee for Standards in Diagnosis of Japan Society for Equilibrium Research Auris Nasus Larynx. 2017;44:1–6.
17. Bhattacharyya N , Gubbels SP , Schwartz SR, et al.Clinical practical guidelines : Benign paroxysmal positional vertigo (update).Otolaryngology– Head and Neck Surgery 2017, Vol. 156(3S) S1–S47.Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update); AAO-HNS Otolaryngol Head Neck Surg. 2017;156(3_suppl): S1-S47.
18. Pérez-Vázquez P, Franco-Gutiérrez V, Soto-Varela A, et al. Practice Guidelines for the Diagnosis and Managementof Benign Paroxysmal Positional Vertigo. Otoneurology Committee of Spanish Otorhinolaryngology and Head and Neck Surgery Consensus Document Acta Otorinolaringol Esp.2018;69(6):345-36
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
Annex 1: Guideline Flowchart
Annex 2: Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
Table 1: Currency
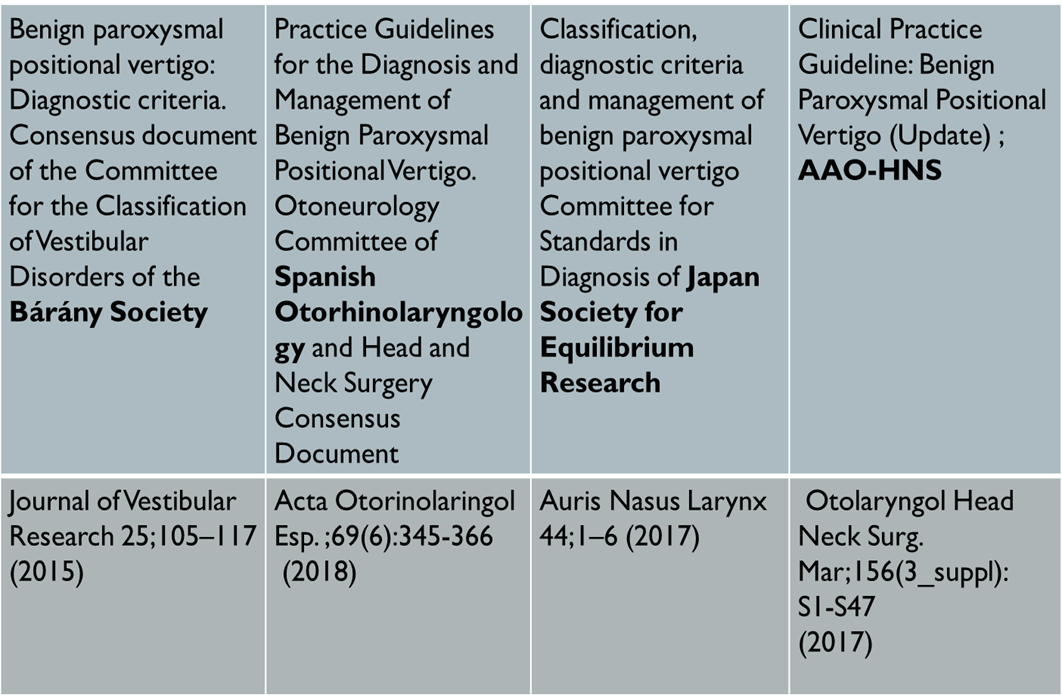
Table 2: Content
|
CRITERIA |
American Academy ORL-HNS |
Bárány Society |
Spanish ORL-HNS Consensus |
Japan Society for Equilibrium Research |
|
Credibility |
9/9 |
5.4/9 |
7.2/9 |
3.6/9 |
|
Observability |
9/9 |
7.2/9 |
3.6/9 |
3.6/9 |
|
Relevance |
9/9 |
7.2/9 |
7.2/9 |
5.4/9 |
|
Relative advantage |
7.2/9 |
7.2/9 |
7.2/9 |
7.2/9 |
|
Easy to install and understand |
9/9 |
9/9 |
7.2/9 |
5.4/9 |
|
Compatibility |
9/9 |
9/9 |
9/9 |
9/9 |
|
Testability |
9/9 |
9/9 |
9/9 |
9/9 |
|
Total |
61.2 |
54 |
50.4 |
43.2 |
Table 3: Quality
|
Domain |
AAO-HNS |
Bárány Society |
Spanish ORL- HNS Consensus |
Japan Society for Equilibrium Research |
|
1. Transparency |
A |
A |
C |
C |
|
2. Conflict of interest |
A |
A |
B |
B |
|
3. Development group |
A |
C |
C |
C |
|
4. Systematic review |
A |
B |
A |
B |
|
5. Grading of evidence |
A |
B |
B |
B |
|
6. Recommendations |
A |
C |
C |
C |
|
7. External review |
A |
A |
NR |
B |
|
8. Updating |
B |
B |
B |
B |
Annex 3: The risks and benefits of added and/or modified statements
|
Statement topic |
Original statement |
The statement action to be adapted |
Benefits |
Risk/Harm
|
|
Vestibular testing |
Clinicians should not order laboratory vestibular testing in a patient who meets diagnostic criteria for BPPV in the absence of additional vestibular signs and/or symptoms inconsistent with BPPV that warrant testing. |
Clinicians should not order laboratory vestibular testing in a patient who meets diagnostic criteria for BPPV in the absence of additional vestibular signs and/or symptoms inconsistent with BPPV that warrant testing. Vestibular testing may be ordered in case of recurrence, persistence of complaint after repositioning maneuver or in the presence of atypical nystagmus |
Diagnosis and treatment of possible causes of positional vertigo other than BPPV |
Cost of vestibular testing |
|
Repositioning procedures as initial therapy for posterior canal (a) |
Clinicians should treat, or refer to a clinician who can treat, patients with posterior canal BPPV with a canalith repositioning procedure |
Clinicians should treat, or refer to a clinician who can treat, patients with posterior canal BPPV with a canalith repositioning procedure. Epley or Semont are equivocally effective for post.canal BPPV |
High value ascribed to prompt resolution of symptoms and the ease with which the CRP may be performed |
No serious adverse events reported in controlled randomized trials |
|
Repositioning procedures as initial therapy for lateral canal (b) |
Not reported |
the barbecue roll maneuver or Gufoni maneuver appear moderately effective for the geotropic form of lateral semicircular canal BPPV |
Helps in resolution of patients symptoms |
None |
|
Post procedural restrictions |
Clinicians may not routinely recommend post procedural postural restrictions after canalith repositioning procedure for posterior canal BPPV. |
Clinicians may not routinely recommend post procedural postural restrictions after canalith repositioning procedure for posterior canal BPPV. Post procedural postrural restriction might be recommended in selected cases as in failure (or repeated failure) of the repositioning maneuvers, recurrent cases, or cases associated with other vestibular pathology as MD or vestibular Migraine. |
Help patients to tolerate symptoms till complete recovery |
Possible musculoskeletal discomfort and cost of cervical collars |
|
Number of CRP repetitions |
Not reported |
1-2 sessions would resolve the condition in 87-100% of patients. A minority would require a 3ed trial. Otherwise persistent BPPV is suspected. |
Help the clinician to search for causes of resolution failure |
Cost of investigations |
|
If there is difficulty in performing successful maneuver |
Not reported |
Clinicians should start with CRP (or modified) even in those patients who are very obese; have severe cervical or lumber discs; or upon patient’s preference. In the latter case patients should be instructed to avoid activities that may increase the risk of falls until symptoms resolve. |
Faster recovery and resolution of BPPV |
Patient discomfort and difficulty of performing the maneuver |
|
Observation as initial therapy
|
Clinicians may offer observation with follow up as initial management for patients with BPPV |
Clinicians may offer observation with follow up only if there is difficulty in performing successful maneuver after trials in some patients as : very obese; severe cervical or lumber discs; or upon patient's preference not to repeat the maneuver |
Avoidance of increased risks of falls; the use of vestibular suppressants with their known side effects |
Prolonged symptoms compared with other interventions that may expose patients to increased risks for falls or lost days of work; indirect costs of delayed resolution compared with other measures |
|
Vestibular rehabilitation |
The clinician may offer VR in the treatment of BPPV |
VR should be considered an option in the treatment of BPPV rather than a recommended first-line treatment modality. Home based Brandt-Daroff exercises is indicated in patients with persistent dizziness or imbalance after successful CRP or patients who refuse CRP.A more comprehensive customized VR program is indicated in patients with other vestibular pathology or with comorbid impairments that require balance rehabilitation specially in elderly. |
Reduce patient symptom in the mentioned cases |
None for home-based exercise. Cost if formal VR program is recommended |
|
Medical therapy |
Clinicians should not routinely treat BPPV with vestibular suppressant medications such as antihistamines and/or benzodiazepines |
Clinicians should not treat BPPV with vestibular suppressant medications such as antihistamines and/or benzodiazepines. Exceptions: Severely symptomatic patients refusing other treatment options and patients requiring prophylaxis for CRP |
Avoidance of adverse effects from, or medication interactions with, these medications; prevention of decreased diagnostic sensitivity from vestibular suppression during performance of the Dix-Hallpike maneuvers |
None |
|
Outcome assessment |
Clinicians should reassess patients within 1 month after an initial period of observation or treatment to document resolution or persistence of symptoms |
Clinicians should reassess patients within time frame of 3 weeks following the canalith repositioning procedure to document resolution, need for repetition of CRP session or persistence of symptoms |
Confirming the success of the maneuver; avoidance of missing other versions of BPPV as multiple canals or central causes |
None |

















