Cochlear Implantation: Phoniatric perspective
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Cochlear Implantation: Phoniatric perspective |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:13 PM |
Description
"last update: 27 August 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdel Aziz,6 Tarek Ghanoum,7 Mahmoud Yousef8
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 MahmoudAbdelAziz,5 MohamedGhonaim,6 TarekGhanoum,7 MahmoudYoussef8
Phoniatrics Chief Manager: MahmoudYoussef8
Phoniatrics Executive Manager: Dalia Mostafa9
Assembly Board: Samia Bassiouny,8 TamerAbou-Elsaad,10 Ayman Shawky,11 Ahlam A.N.El-Adawy,12 Yossra Abdel Naby Sallam,13 Effat Zaky,14 Ahmed Ali15
Grading Board (In alphabetical order)
SafaaElSady,8 AishaFawzy,9 NirvanaHafez,8 Dalia Mostafa9
Reviewing
Board: MarwaSaleh,8 RehamElMaghraby16
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University,
2Otorhinolaryngology Department, Faculty of Medicine/Menoufia University,
3Otorhinolaryngology Department,FacultyofMedicine/MiniaUniversity,
4Otorhinolaryngology Department,FacultyofMedicine/Beni-SuefUniversity,
5Otorhinolaryngology Department,FacultyofMedicine/TantaUniversity,
6Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University,
7AudiovestibularUnit, Otorhinolaryngology Department, FacultyofMedicine/CairoUniversity,
8Phoniatrics Unit,OtorhinolaryngologyDepartment, FacultyofMedicine/ Ain ShamsUniversity,
9Phoniatrics Unit, Otorhinolaryngology Department,Faculty ofMedicine/ Cairo University,
10Phoniatrics Unit,Otorhinolaryngology Department,FacultyofMedicine/MansouraUniversity,
11Phoniatrics Unit,Otorhinolaryngology Department,FacultyofMedicine/MilitaryArmedForces,
12Phoniatrics Unit,OtorhinolaryngologyDepartment,FacultyofMedicine/ SohagUniversity,
13Phoniatrics Unit,OtorhinolaryngologyDepartment,FacultyofMedicine/Al-AzharUniversity,
14Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Minia University,
15PhoniatricsUnit, Otorhinolaryngology Department, Faculty ofMedicine/ Beni-SuefUniversity, 16PhoniatricsUnit, Otorhinolaryngology Department,Faculty of Medicine/Alexandria University.
Other specialties related to this guideline: Audiology, Paediatrics, and Radiology.
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Abbreviations
CI Cochlear Implant
GRADE Grading of Recommendations Assessment, Development and Evaluation
SNHL Sensorineural Hearing Loss- Executive Summary
The goals of cochlear implantation in children are acquiring normal speech and language development, achieving higher levels academically, enrolling in main streaming and developing better sense of security and better quality of life (Strong recommendation).
As for adult recipients of CI, main goals are improved social and work quality of life, with less stressful events (Strong recommendation).
- Duration of deafness, hearing aid use prior to implantation, and age at implantation, can affect candidacy and predict post-operative outcomes (Strong recommendation).
- Pre lingually deafened adolescents and adults may benefit from cochlear implantation and should not be excluded from candidacy (Conditional recommendation).
- Children with disabilities in addition to deafness may benefit from cochlear implantation in quality-of-life outcomes and environmental awareness. These groups should not be excluded from candidacy. Families should be counseled regarding realistic expectations (Strong recommendation).
- A speech and language evaluation may be recommended in adult candidacy evaluations and could be considered critical in pediatric candidacy evaluations (Strong recommendation).
- High performance in children who use a cochlear implant has been linked to full-time use of the cochlear implant in home and school environments (Strong recommendation).
- The amount and quality of language used by parents/caregivers of children who use cochlear implants has a strong influence on these children’s linguistic development. (Strong recommendation).
- Bilateral stimulation should be considered for all individuals who use a cochlear implant, if not otherwise contraindicated.
Clinicians should be able to:
-Work in a multidisciplinary team of related specialties to ensure proper candidate selection and successful outcomes post implantation.
- Acquire full history from the patient/caregiver.
- Perform evaluation of the preimplant auditory skills, speech, language and voice evaluation.
- Implement different strategies of auditory training to enhance auditory skills development in order to acquire normal spoken receptive and expressive language development (Strong recommendation).
All clinicians should be aware and informed to consider the following:
• Red Flags that need any referral for Assessment/ Management must be taken into consideration.
• Why and when to refer to other specialties .
• Management should be targeted towards implementation of proper auditory training for acquisition of spoken language skills, aiming to decrease the gap between the chronological age and the language age (Strong recommendation).
- Introduction, scope and audience
➡️Introduction
➡️Scope
The scope of the guideline provides a brief overview of the context (e.g. current policy and practice) as well as the key issues that will be considered in the guideline that is related to Phoniatric evaluation and management of patients undergoing cochlear implantation.
➡️Target audience
Phoniatricians, speech language pathologists, ENT, Audiologists, who are dealing with the process of Phoniatric evaluation and communicative rehabilitation of cochlear implanted children.
- Methods
Methods of development:
➡️Stakeholder Involvement: Individuals who were involved in the development process. Including the above-mentioned Audiology Chief Manager, Audiology Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
➡️Search method:
Electronic database searched:
- Pubmed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar
- The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Time period searched: From 2011 to 2019.
➡️Results : Seven authors searched five of the best evidence based guidelines. And selection of the most appropriate Guideline was based on having the highest score regarding the currency, contents and quality. The selected one was: The American Academy of Audiology, Clinical Practice Guidelines: Cochlear Implants 2019. It was then graded by 4 expert Phoniatricians, & reviewed by 2 expert reviewers, to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks
(GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
The following statements and flowchart were adapted from The American Academy of Audiology, Clinical Practice Guidelines: Cochlear Implants 2019, which received the highest scores as regards thecurrency, contents, and quality.
Recommendations statements
|
Statement topic |
Action recommendation |
Level of evidence |
Strength of recommendation. |
Study Type |
Reference |
|
1. Etiology
|
Perinatal problems, such as meningitis, hyperbilirubinemia, and other aetiologies associated with sensorineural hearing loss may affect candidacy and predict post-operative outcomes. Information should be documented clearly in the case history. |
High |
Strong recommendation |
Systematic review |
1, 20 |
|
2. Duration of deafness |
Duration of deafness can affect candidacy and predict post-operative outcomes. Information should be documented clearly in the case history
|
High
|
Strong recommendation |
Systematic review |
2, 19 |
|
3. Hearing aid use prior to implantation |
Hearing aid use prior to implantation can affect candidacy and predict post-operative outcomes. Information should be documented clearly in the case history.
|
High
|
Strong recommendation |
Systematic review |
7, 20
|
|
4. Age at implantation
|
Age at implantation can affect candidacy and predict post-operative outcomes. Information should be documented clearly in the case history.
|
High |
Strong recommendation |
Systematic review |
3, 4
|
|
5. Prelingually deafened adults
|
Prelingually deafened adolescents and adults may benefit from cochlear implantation and should not be excluded from candidacy. Families should be counseled regarding realistic expectations.
|
Low |
Conditional recommendation |
Cohort studies |
7, 21
|
|
6. Other disabilities
|
Children with disabilities in addition to deafness may benefit from cochlear implantation in quality-of-life outcomes and environmental awareness. These groups should not be excluded from candidacy. Families should be counseled regarding realistic expectations |
High |
Strong recommendation |
Systematic review |
8, 15
|
|
7. Assessment
|
Audiometric threshold testing is used to determine candidacy; better pre-operative hearing thresholds are associated with better post-operative outcomes in children and prelingually deafened adults.
|
High |
Strong recommendation |
Systematic review |
10,12
|
|
8. Assessment
|
Cognitive evaluation or cognitive screener should be considered when evaluating children and older adults.
|
Very Low
|
Strong recommendation |
Expert opinion |
30,32 |
|
9. Assessment
|
A speech and language evaluation may be recommended in adult candidacy evaluations and could be considered critical in pediatric candidacy evaluations.
|
High |
Strong recommendation |
Systematic review |
8 |
|
10. Expectations
|
Counseling toward appropriate expectations should be done by the audiologist and the phoniatrician.
|
Moderate |
Strong recommendation |
Systematic review |
8 |
|
11. Follow up assessment
|
For children, evaluation of audibility and auditory, speech, and language development should be conducted routinely throughout development. More frequent monitoring of progress is warranted in those children who are in the period of developing language and auditory skills.
|
Low |
Strong recommendation |
Cohort studies |
4 |
|
12. Follow up assessment
|
Informational and adjustment counselling should be provided to support consistent device use, implementation of intervention strategies, and psychosocial well-being .
|
Low
|
Strong recommendation |
Cohort studies |
32 |
|
13. Consistent use of CI
|
High performance in children who use a cochlear implant has been linked to full-time use of the cochlear implant in home and school environments.
|
High
|
Strong recommendation |
Randomized control trial |
14 |
|
14. Bilingualism
|
Individuals who use cochlear implants can experience success in using multiple languages.
|
Moderate |
Strong recommendation |
Randomized control trial |
6 |
|
15. Assisstive hearing technology
|
All individuals who use a cochlear implant should be considered as a potential candidate for hearing assistive technology; particularly those who experience complex listening environments and school-aged children.
|
High |
Strong recommendation |
Systematic review |
31 |
|
16. Intervention
|
Intervention for adults may focus on auditory training. The specific intervention needs may vary based upon factors known to affect outcomes. |
High
|
Strong recommendation |
Systematic review |
18 |
|
17. Intervention
|
The amount and quality of language used by parents/caregivers of children who use cochlear implants has a strong influence on these children’s linguistic development. |
Moderate |
Strong recommendation |
Randomized control study |
13 |
|
18. Intervention
|
Engaging family members in therapy and coordinating efforts among therapists and educators is believed to result in the best outcomes for children and families
|
Moderate |
Strong recommendation |
Randomized control study |
2 |
|
19. Intervention
|
The likelihood of a child gaining high benefit in the areas of speech perception, speech production, and spoken language increases when more emphasis is placed on listening and spoken language in the child’s home and educational setting .
|
High
|
Strong recommendation |
Randomized control study |
9 |
|
20. Intervention with other disabilities
|
The progress of children with other comorbidities should be measured by criteria that are unique to them and that reflect the goals of the family. |
High
|
Strong recommendation |
Randomized control study |
17 |
|
21. Intervention
|
Bilateral stimulation should be considered for all individuals who use a cochlear implant, if not otherwise contraindicated. |
High
|
Strong recommendation |
Randomized control study |
11 |
- Research needs
There is a need to conduct research on the following areas:
• bilingualism in cochlear implant.
• Speech perception in noisy situations.
• Language development and Speech perception in bilateral cochlear implant.
• Language development in bilateral versus unilateral cochlear implantation
• Speech perception in bimodal hearing
• Language development in simultaneous versus sequential cochlear implant.
- Monitoring and evaluating the impact of the guideline
➡️Monitoring/Auditing Criteria: To assess guideline implementation or adherence to recommendations. This is accomplished if the CI child acquires normal speech and language development, achieves higher levels academically, and develops better sense of security and better quality of life. Monitoring criteria for adult reciepients of CI, are improved social and work quality of life.
Clinicians should be able to:
-Work in a multidisciplinary team of related specialties to ensure proper candidate selection and successful outcomes post implantation.
- Acquire full history from the patient/caregiver.
- Perform evaluation of the preimplant auditory skills, speech, language and voice evaluation.
- Implement different strategies of auditory training to develop normal spoken language skills.
All clinicians should be aware and informed to consider the following:
• Red Flags that need any referral for Assessment/ Management must be taken into consideration.
• Why and when to Refer to other specialties .
• Management should be targeted towards implementation of proper auditory training for acquisition of spoken language skills, aiming to decrease the gap between the chronological age and the language age.
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. Abdurehim, Y., Lehmann, A., & Zeitouni, A.G. (2016). Stapedotomy vs cochlear implantation for advanced otosclerosis: Systematic review and meta-analysis. Otolaryngology-Head and Neck Surgery, 155(5), 764-770.
2. Ambrose, S.E., Walker, E.A., Unflat-Berry, L.M., Oleson, J.J., & Moeller, M.P. (2015). Quantity and quality of caregivers’ linguistic input to 18-month and 3-year-old children
3. Blamey, P., Artieres, F. (2013). Factors affecting auditory performance of postlingually deaf adults using cochlear implants: An update with 2251 patients. Audiology & Neurotology, 18(1), 36-47.
4. Bradham, T.S., Snell, G., & Haynes, D. (2009). Current practices in pediatric cochlear implantation. Perspectives on Hearing & Hearing Disorders in Childhood, 19(1), 32-42.
5. Bruijnzeel, H., Ziylan, F., Stegeman, I., Topsakal, V., & Grolman, W. (2016). A systematic review to define the speech and language benefit of early (<12 months) pediatric cochlear implantation. Audiology & Neurotology, 21, 113-126.
6. Bunta, F., & Douglas, W.M. (2013). The effects of dual-language support on the language skills of bilingual children with hearing loss who use listening devices relative to their monolingual peers. Language, Speech, and Hearing Services in Schools, 44, 281-290.
7. Caposecco, A., Hickson, L., & Pedley, K. (2012). Cochlear implant outcomes in adults and adolescents with early-onset hearing loss. Ear & Hearing, 33(2), 2019-220.
8. Cejas, I., Hoffman, M.F., & Quittner, A.L. (2015). Outcomes and benefits of pediatric cochlear implantation in children with additional disabilities: a review and report of family influences on outcomes. Pediatric Health, Medicine and Therapeutics, 6, 45-63.
9. Ching, T.Y., Dillon, H., Leigh, G., & Cupples, L. (2018). Learning from the longitudinal outcomes of children with hearing impairment (LOCHI) study: summary of 5-year findings and implications. International Journal of Audiology, 57(2), S105-S111.
10. Chiossi, J.S.C., & Hyppolto, M.A. (2017). Effects of residual hearing on cochlear implant outcomes in children: A systematic review. International Journal of Pediatric Otorhinolaryngology, 100, 119-127.
11. Cullington, H.E. & Zeng, F.G. (2011). Comparison of bimodal and bilateral cochlear implant users on speech recognition with competing talker, music perception, affective prosody discrimination and talker identification. Ear & Hearing, 32(1), 16-30.
12. De Kleijn, J.L., van Kalmthout, L.W.M., van der Vossen, M.J.B., Vonck, B.M.D., Topsakal, V. (2018). Identification of pure-tone audiologic thresholds for pediatric cochlear implant candidacy: A systematic review. JAMA Otolaryngology-Head & Neck Surgery, 144(7), 630-638.
13. DesJardin, J.L. & Eisenberg, L.S. (2007). Maternal contributions: Supporting language development in young children with cochlear implants. Ear & Hearing, 28(4), 456-459.
14. Easwar, V., Sanfilippo, J., Papsin, B., & Gordon, K. (2016). Factors affecting daily cochlear implant use in children: Datalogging evidence. Journal of the American Academy of Audiology, 27, 824-838.
15. Eze, N., Ofo, E., Jiang, D., & O’Connor, A.F. (2013). Systematic review of cochlear implantation in children with developmental disability. Otology & Neurotology, 34(8), 1385-1393.
16.Harris, M., Terlektsi, E., & Kyle, F.E. (2017). Literacy outcomes for primary school children who are deaf and hard of hearing: A cohort comparison study. Journal of Speech, Language, and Hearing Research, 60, 701-711.
17. Hayward, D.V., Ritter, K., Grueber, J., & Howarth, T. (2013). Outcomes that matter for children with severe multiple disabilities who use cochlear implants: The first step in an instrument development process. Canadian Journal of Speech-Language Pathology & Audiology, 37(1), 58-69.
18. Henshaw, H. & Ferguson, M.A. (2013). Efficacy of individual computer-based auditory training for people with hearing loss: A systematic review of the evidence. PLOS ONE, 8(5), 1-18.
19. Holden, L.K., Finley, C.C., Firszt, J.B., Holden, T.A., Brenner, C., Potts, L.G., Gotter, B.D., Vanderhoof, S.S., Mispagel, K., Heydebrand, G., & Skinner, M.W. (2013). Factors affecting open-set word recognition in adults with cochlear implants. Ear & Hearing, 34(3), 342-360.
20. Kang, D.H., Lee, M.J., Lee, K.Y., Lee, S.H., & Jang, J.H. (2016). Prediction of cochlear implant outcomes in patients with prelingual deafness. Clinical and Experimental Otorhinolaryngology. 9(3), 220-225.
21. Klop, W.M.C., Briaire, J.J., Stiggelbout, A.M., Frijns, J.H.M. (2007). Cochlear implant outcomes and quality of life in adults with prelingual deafness. Laryngoscope, 117(11), 1982-1987.
22. Knutson, J.F, Johnson, A., & Murray, K.T. (2006). Social and emotional characteristics of adults seeking a cochlear implant and their spouses. British Journal of Health Psychology, 11(Pt 2), 279-292.
23. Lammers, M.J.W., Versnel, H., Topsakal, V., van Zanten, G.A., & Wilko, G. (2018). Predicting performance and non-use in prelingually deaf and late-implanted cochlear implant users. Otology & Neurotology, 39(6), 436-452.
24. Lazard, D.S., Vincent, C., Venail, F., Van de Heyning, P., Truy, E., Sterkers, O., . . . Blamey, P.J. (2012). Pre-, per- and postoperative factors affecting performance of post linguistically Deaf adults using cochlear implants: A new conceptual model over time. PLOS ONE, 7(11), e48739.
25. Leigh, J.R., Moran, M., Hollow, R., & Dowell, R.C. (2016). Evidence-based guidelines for recommending cochlear implantation for postlingually deafened adult. International Journal of Audiology, 55(Suppl 2), S3-8.
26. Lin, F.R., & Niparko, J.K. (2006). Measuring health-related quality of life after pediatric cochlear implantation: A systematic review. International Journal of Pediatric Otorhinolaryngology, 70(10), 1695-1706.
27. Nittrouer, S., Caldwell-Tarr, A., Sansom, E., Twersky, J., & Lowenstein, J.H. (2014). Nonword repetition in children with cochlear implants: A potential clinical marker of poor language acquisition. American Journal of Speech-Language Pathology, 23, 679-695.
28. Nordvik, Ø., Heggdal, P.O.L., Brännström, J., Vassbotn, F., Aarstad, A.K., & Aarstad, H.J. (2018). Generic quality of life in persons with hearing loss: A systematic literature review. BMC Ear, Nose and Throat Disorders, 18(1). doi: 10.1186/s12901-018-0051-6
29. Philippon, D., Bergeron, F., Ferron, P., & Bussières, R. (2010). Cochlear implantation in postmenigenic deafness. Otology & Neurotology, 31(1), 83-87.
30. Roeser, R. & Clark, J. (2008). Live voice speech recognition audiometry: Stop the madness. Audiology Today, 20, 32-33.
31. Schafer, E.C., Amlani, A.M., Paiva, D., Nozari, L., & Verret, S. (2011). A meta-analysis to compare speech recognition in noise with bilateral cochlear implants and bimodal stimulation. International Journal of Audiology, 50, 871-880. 43
32. Shapiro, W.H. & Bradham, T.S. (2012). Cochlear implant programming. Otolaryngologic Clinics of North America, 45, 111-127.
33. Shen, J., Anderson, M.C., Arehart, K.H., & Souze, P.E. (2016). Using cognitive screening tests in audiology. American Journal of Audiology, 25, 319-331.
34. Uhler, K., Warner-Czyz, A., Gifford, R., & PMSTB Working Group. (2017). Tutorial: Pediatric Minimum Speech Test Battery. Journal of the American Academy of Audiology, 28, 232-247.
35. Ventry, I.M., & Weinstein, B.E. (1982). The hearing handicap inventory for the elderly: A new tool. Ear & Hearing, 3(3), 128-134.
36. Wong, L.L.N., Yu, J.K.Y., Chan, S.S., & Tong, M.C.F. (2014). Screening of cognitive function and hearing impairment in older adults: A preliminary study. BioMed Research International, 2014, 1-7.
37. Yang, Z. & Cosetti, M. (2016). Safety and outcomes of cochlear implantation in the elderly: A review of recent literature. Journal of Otology, 11(1), 1-6.
38. Zwolan, T.A., Kilney, P.R., & Telian, S.A. (1996). Self-report of cochlear implant use and satisfaction by prelingually deafened adults. Ear & Hearing, 17(3), 198-210
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
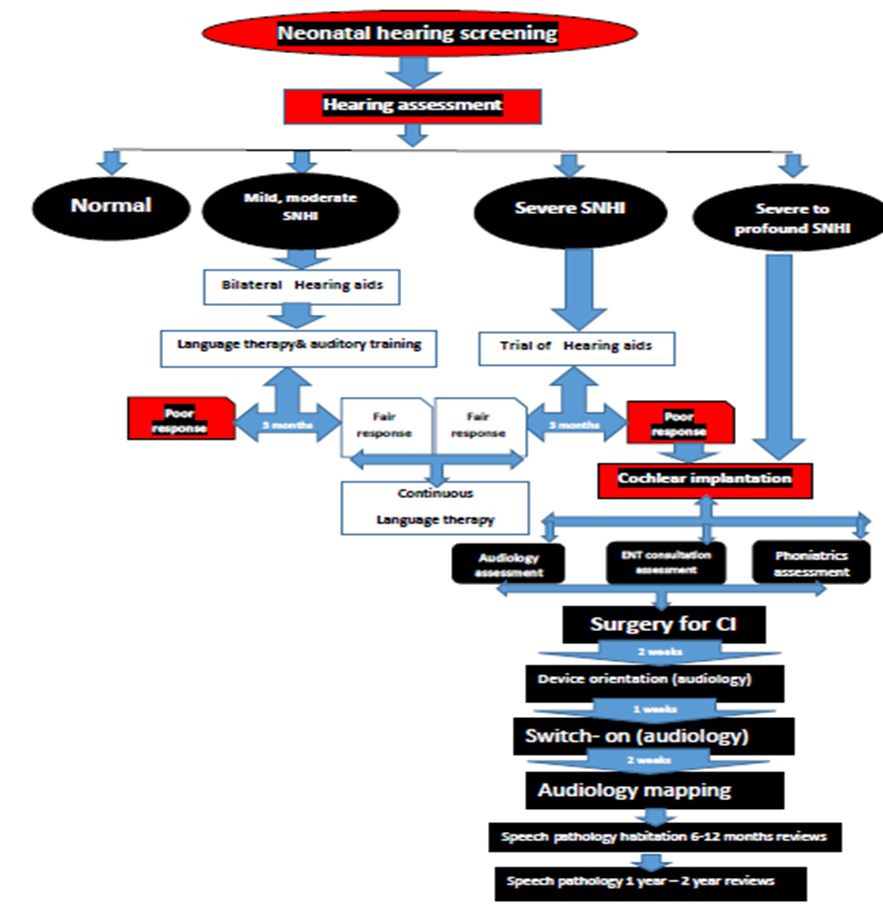
Annex1: Guideline Flowchart
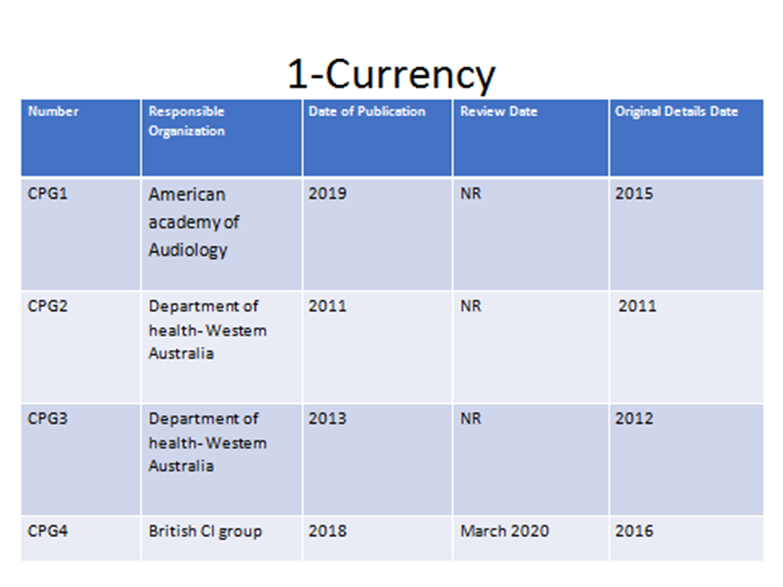
Annex2: Tables of appraisal of selected guidelines:Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
|
Criteria |
Guideline 1 |
Guideline 2 |
Guideline 3 |
Guideline 4 |
|
Clinical practice guidelines 2019 |
Neuroscience 2011 (Pediatrics) |
Neuroscience 2013 (Adults) |
British CI 2018 |
|
|
Credibility |
9 |
6 |
6 |
8 |
|
Observability |
6 |
3 |
3 |
5 |
|
Relevance |
7 |
8 |
8 |
8 |
|
Relative advantage |
7 |
7 |
7 |
7 |
|
Easy to install and understand |
8 |
7 |
7 |
8 |
|
Compatibility |
8 |
6 |
6 |
8 |
|
Testability |
8 |
8 |
8 |
8 |
|
Total |
53 |
45 |
45 |
52 |
|
Domain |
CPG1 |
CPG2 |
CPG3 |
CPG4 |
|
Transparency |
A |
A |
A |
A |
|
Conflict of Interest |
NR |
NR |
NR |
NR |
|
Development Group |
A |
C |
C |
B |
|
Systematic Review |
A |
B |
B |
A |
|
Grade of Evidence |
A |
B |
B |
B |
|
Recommendations |
A |
B |
B |
B |
|
External Review |
C |
C |
C |
A |
|
Update |
B |
B |
B |
A |
|
CPG1: 5A, 1B, 1C, 1NR |
||||
Annex3: The risks and benefits of added and/or modified statements
|
Statement |
Risk |
Benefit |
|
The progress of children with other comorbidities should be measured by criteria that are unique to them and that reflect the goals of the family. |
Low family goals expected from implanting those children, can affect the outcomes. |
Those children should not be excluded from candidacy. They can benefit from implantation, with counselling given towards realistic expectations. |
|
Bilateral stimulation should be considered for all individuals who use a cochlear implant, if not otherwise contraindicated. |
No risk |
Bilateral stimulation should be considered for all individuals who use a cochlear implant, all of its benefits. |




















