The Embryos to Transfer in IVF/ICSI
| Site: | EHC | Egyptian Health Council |
| Course: | ِAssisted Reproductive Technologies Guidelines |
| Book: | The Embryos to Transfer in IVF/ICSI |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:25 PM |
Description
"last update: 6 August 2024"
- Acknowledgement
We would like to acknowledge the Egyptian health council committee of national Egyptian guidelines
Chair of the panel
Professor Mohammed Yehia.
Scientific group members
Professor Gamal Abu El Serour , professor Abdel Megid Ramsy, professor Hisham Salah Professor Omar Shabaan Dr Mohamed Elsherbiny Dr Amgad Monir and Dr Wafaa Bengamin
- Abbreviations
ASRM: American Society of reproductive medicine.
DET : double embryo transfer.
eSET: Elective single embryo transfer.
ESHRE: European Society of human reproductive and the and Embryology.
ET: Embryo transfer.
FET frozen embryo transfer.
HOM: high order multiple pregnancy.
IVF: in vitro fertilization.
LBR :live birth rate.
MPR :multiple pregnancy rate.
SART: Society for assistive reproductive technology.
TA-USG: Trans abdominal ultrasound .
PGT : preimplantation genetic testing.
PGT-A : preimplantation genetic testing aneuploidy .
- Scope
This guideline predominantly covers the recommendations for safe and effective embryo transfer after IVF to achieve the highest possible life birth rate without subjecting the patient to the risk of multiple pregnancy. It also aims to examine different evidence based procedures and the different steps that should be used during the embryo transfer procedures. It also examines many of the procedures that should be abandoned because there is no evidence to support their practice.
- Executive Summary
● It is recommended that clinicians should perform single embryo transfer (strong recommendation).
● Medical SET is indicated for women in whom multiple pregnancy represents an a priori increased risk compared to the overall population such as women with congenital uterine anomalies (e.g. septate uterus), bad obstetric history (e.g. previous premature birth <32 gestational weeks) and severe systemic diseases (e.g. insulin-dependent diabetes).(strong recommendation).
● Elective single embryo transfer should be used in cases with PGTA (strong recommendation) .
● It is recommended to encourage eSET in good-prognosis patients although a maximum of two embryos is allowed after proper counseling. In cases of DET, a written consent explaining the risks of multiple pregnancies should be signed. (conditional recommendation).
➡️Good prognosis patients include:
- First or second IVF attempt whether fresh or frozen ET and excellent embryo quality by morphology. It should be emphasized that DET may have in most studies a higher LBR compared to eSET, but this is at the expense of significantly higher MPR. The higher MPR with DET is a consistent finding whether the embryos are fresh or frozen, cleavage stage or blastocysts, good-quality or mixed (one good & one poor-quality) or two poor-quality embryos.16-21
- Surplus embryos of sufficient quality to warrant cryopreservation, or in cases of FET, the availability of vitrified high-quality day 5 or day 6 blastocysts for transfer.22
- Previously pregnancy/live birth particularly if resulting from IVF. This is associated with an increased chance of LBR and MPR.23,27 Other studies confirmed the association of previous pregnancy with LBR but with no correlation with MPR.27,30
● Females <38 years of age should be strongly encouraged to transfer one embryo especially if they meet the criteria of good prognosis. Emphasis on eSET is highly recommended if the female age is <35 years (strong recommendation).
● Females between 38 and 40 years are allowed to transfer two embryos, however, eSET can still be encouraged especially if they have good prognosis. (strong recommendation).
● Females 41-42 years of age should receive no more than two embryos. (strong recommendation).
● In FET cycles, the decisions should be based on the age of the woman when the embryos were cryopreserved. (strong recommendation).
● Trans-abdominal ultrasound guidance during embryo transfer is recommended as it improves clinical pregnancy rate and live-birth rate. (strong recommendation).
● It is recommended to use a soft embryo transfer catheter as it improves the pregnancy rate in fresh and Frozen cycles. (strong recommendation).
● Anesthesia during embryo transfer does not improve pregnancy rates. Given that there are added risks associated with anesthesia, routine anesthesia is not recommended in IVF-embryo transfer. ( strong recommendation).
● It is recommended to place the catheter tip in the upper or middle (central) area of the uterine cavity, greater than 1 cm from the fundus as this decreases embryo expulsion and optimizes pregnancy rates. (Conditional recommendation).
● It is not recommended to prescribe antibiotics with embryo transfer. (conditional recommendation).
● Bed rest is not recommended after embryo transfer as it does not increase pregnancy rates (Strong recommendation).
● No enough evidence to recommend routine removal of cervical mucous from the cervix before embryo transfer (conditional recommendation).
● There is No specific time to recommend removal of the embryo transfer catheter after embryo transfer. (conditional recommendation).
- Introduction
Embryo transfer is the last and one of the most important steps in IVF procedures . It entails deposition of fertilized and divided embryo (s) inside the uterine cavity. Over the years many changes have occurred regarding the number and technique of embryo transfer. It has been shown repeatedly that the results of IVF in the same institution differ dramatically in pregnancy rate depending upon that clinician performing the procedure. A survey of sorts demonstrated that essentially all practitioners are allowed to perform embryo transfer if they desire no matter what their skill level is.
- Scope and purpose
This guideline predominantly covers the recommendations for safe and effective embryo transfer after IVF to achieve the highest possible life birth rate without subjecting the patient to the risk of multiple pregnancy. It also aims to examine different evidence based procedures and the different steps that should be used during the embryo transfer procedures. It also examines many of the procedures that should be abandoned because there is no evidence to support their practice.
This is the first guideline in Egypt for regulation of IVF practice. Multiple embryo transfer is widely practiced in Egypt with a consequent high multiple twin and HOM rate. Both the clinician and the patient are responsible for that. The transition from no legislation to eSET cannot be taken abruptly. A gradual move to the limitation of the number of embryos to transfer is needed. The aim is the reduction of MPR to below 15% within the coming 4 years, with an ultimate goal of bringing it down below 10% in a second step. Patient's autonomy to consider placement of more than one embryo is respected, however, this requires a full discussion of the ethical and medical considerations, ensuring that a patient is able to make a fully informed decision. This guideline is meant to assist practitioners to properly counsel patients to take the right decision about the number of embryos to transfer.
- THE TARGET AUDIENCE
This guideline is directed towards healthcare professionals who are involved in the process of patient counseling and guidance regarding the IVF/ICSI procedures and the number of embryos to transfer. It includes reproductive medicine specialists, gynecologists, obstetricians, reproductive nurses, embryologists and neonatologists.
- Methods
A comprehensive search for guidelines was undertaken to identify the most relevant guidelines to consider for adaptation.
Inclusion/exclusion criteria followed in the search and retrieval of guidelines to be adapted:
● Selecting only evidence-based guidelines (guideline must include a report on systematic literature searches and explicit links between individual recommendations and their supporting evidence)
● Selecting only national and/or international guidelines
● Specific range of dates for publication (using Guidelines published or updated 2010 and later)
● Selecting peer reviewed publications only
● Selecting guidelines written in English language
● Excluding guidelines written by a single author not on behalf of an organization in order to be valid and comprehensive, a guideline ideally requires multidisciplinary input
● Excluding guidelines published without references as the panel needs to know whether a thorough literature review was conducted and whether current evidence was used in the preparation of the recommendations
The following characteristics of the retrieved guidelines were summarized in a table:
• Developing organization/authors
• Date of publication, posting, and release
• Country/language of publication
• Date of posting and/or release
• Dates of the search used by the source guideline developers
All retrieved Guidelines were screened and appraised using AGREE II instrument (www.agreetrust.org) by at least two members. the panel decided a cut-off point or rank the guidelines (any guideline scoring above 50% on the rigor dimension was retained)
These Guidelines were adapted mainly from” performing the embryo transfer: a guide” Practice committee of the American Society of Reproductive medicine 2017,“1ESHRE guidelines: number of embryos to transfer during IVF/ICSI” developed by the ESHRE guideline group on the number of embryos to transfer in 20242 and “Guidance on the limits to the number of embryos to transfer” developed by the Practice Committee of the American Society for Reproductive Medicine and the Practice Committee of the Society of Assisted Reproductive Technology in 20213.
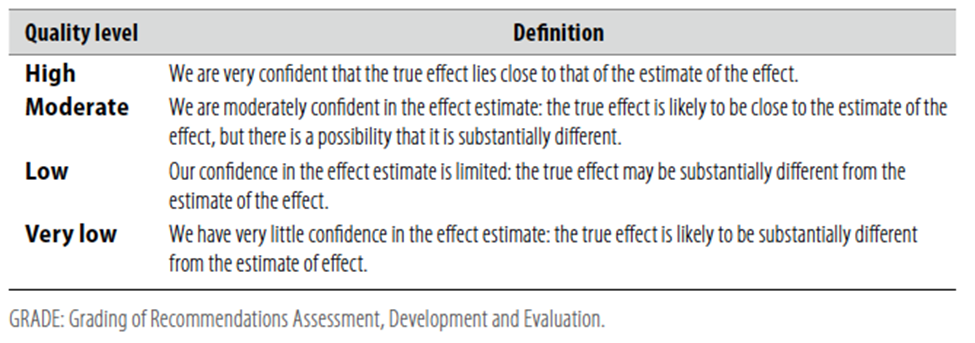
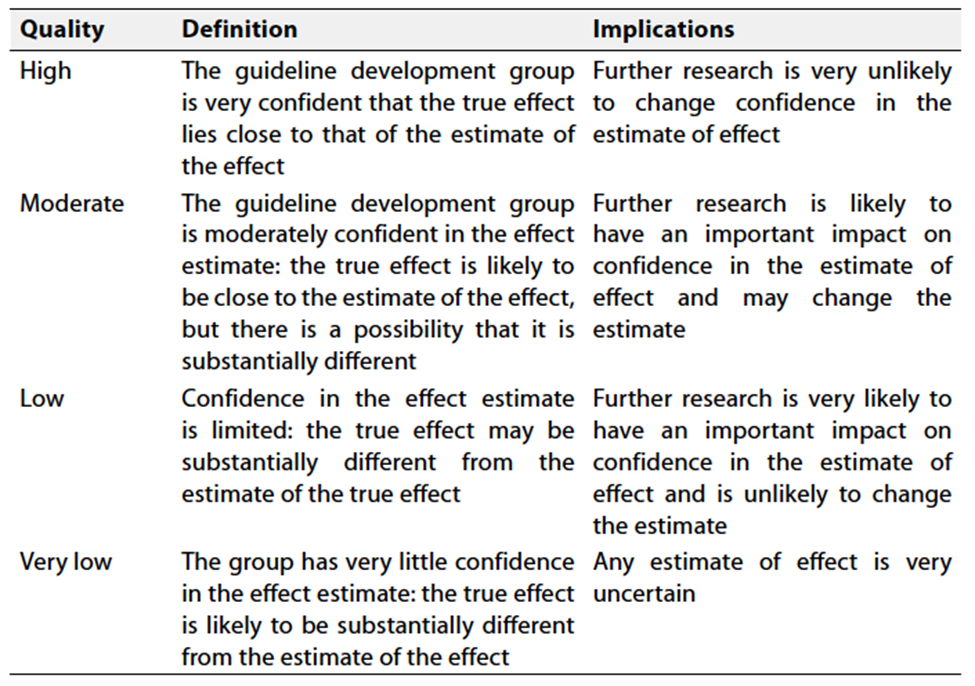
According to WHO handbook for Guidelines we used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess the quality of a body of evidence, develop and report recommendations. GRADE methods are used by WHO because these represent internationally agreed standards for making transparent recommendations. Detailed information on GRADE is available on the following sites:
■ GRADE working group: http://www.gradeworkingroup.org
■ GRADE online training modules: http://cebgrade.mcmaster.ca/
■ GRADE profile software: http://ims.cochrane.org/revman/gradepro
Table 1 Quality of evidence in GRADE
- Recommendation
1.Number of embryos transferred
It is recommended that clinicians should perform single embryo transfer (strong recommendation- high grade evidence) 4,9
Conditions of compulsory eSET
● Medical SET is indicated for women in whom multiple pregnancy represents an a priori increased risk compared to the overall population such as women with congenital uterine anomalies (e.g. septate uterus), bad obstetric history (e.g. previous premature birth <32 gestational weeks) and severe systemic diseases (e.g. insulin-dependent diabetes).(strong recommendation- high grade evidence) 4,9
Preimplantation genetic testing (PGT)
● Elective single embryo transfer should be used in cases with PGTA (strong recommendation- high grade evidence) 4,9 .PGT and particularly PGT-A is associated with a higher implantation rate regardless of the age, and double euploid embryo transfer may be associated with a higher MPR.5.6 Low- to moderate-quality evidence shows that eSET of euploid embryos minimizes the risk multiple pregnancies without affecting LBR.7,8 The ASRM guideline recommends the transfer of one euploid embryo regardless of the female’s age.9
Conditions of preferred eSET with a maximum of two embryos allowed
● It is recommended to encourage eSET in good-prognosis patients although a maximum of two embryos is allowed after proper counseling. In cases of DET, a written consent explaining the risks of multiple pregnancies should be signed. (conditional recommendation - very low gradeevidence) 4,9,10,14
Good prognosis patients include:
- Surplus embryos of sufficient quality to warrant cryopreservation, or in cases of FET, the availability of vitrified high-quality day 5 or day 6 blastocysts for transfer.22
- Previously pregnancy/live birth particularly if resulting from IVF. This is associated with an increased chance of LBR and MPR.23,27 Other studies confirmed the association of previous pregnancy with LBR but with no correlation with MPR.27,30
● Females between 38 and 40 years are allowed to transfer two embryos, however, eSET can still be encouraged especially if they have good prognosis. (strong recommendation- high grade evidence) 4,9 .
● Females 41-42 years of age should receive no more than two embryos. (strong recommendation- high grade evidence) 4,9 .
● In FET cycles, the decisions should be based on the age of the woman when the embryos were cryopreserved. (strong recommendation- high grade evidence) 4,9 .
2.Ultrasound guided embryo transfer
Trans-abdominal ultrasound guidance during embryo transfer is recommended as it improves clinical pregnancy rate and live-birth rate. (strong recommendation- high grade evidence ) 35,36 .
One of the most critical steps in the process of in vitro fertilization (IVF) is the embryo transfer. Studies have consistently demonstrated that embryo transfer pregnancy rates differ depending upon the clinician performing the procedure31.
Three randomized controlled trials compared TV-US versus TA-US 32,34comparing 93 TV-US and 93 TA-US, found no differences in implantation rates, clinical pregnancy rates and live birth rates between the two approaches.
The patient should attend the ET procedure with a full bladder. This straightens the angle between the uterine cervix and uterine body 35,36 and facilitates visualization using the transabdominal US scan. A straighter cervical canal and smaller inclination of the uterine body facilitate the effortless insertion of an ET catheter into the correct spot in the uterine cavity 37. It was suggested in a large study by 38 that performing ET with a full bladder increases the clinical pregnancy rate.
3. Type of catheter
● It is recommended to use a soft embryo transfer catheter as it improves the pregnancy rate in fresh and Frozen cycles. (strong recommendation- high grade evidence ) 39,41
NB. Soft catheter is defined as any embryo transfer catheter with a soft inner catheter.
The pooled data of two randomized control trials and two cohort trials showed that pregnancy rates are higher using soft catheters for embryo transfer compared with firm catheters (RR 1.36, 95% CI 1.16–1.59) 39,41.No soft embryo transfer catheter is clearly superior and that commercially available soft catheters perform similarly. Personal choice and cost can guide differential use of one soft catheter over the other (ASRM practice committee 2017) Data not enough to recommend a certain type of soft catheters.
4. Anesthesia during transfer
● Anesthesia during embryo transfer does not improve pregnancy rates. Given that there are added risks associated with anesthesia, routine anesthesia is not recommended in IVF-embryo transfer. ( strong recommendation -high grade evidence ) 42 .
Large cohort study conducted by vander Van and colleagues 1988, showed a pregnancy rate of 18% in the embryo transfers without anesthesia, and 19% in the embryo transfers with anesthesia. In this larger comparison, general anesthesia did not have a beneficial impact on pregnancy rate 42.
5. Site of embryo placement
● It is recommended to place the catheter tip in the upper or middle (central) area of the uterine cavity, greater than 1 cm from the fundus as this decreases embryo expulsion and optimizes pregnancy rates. (Conditional recommendation -moderate grade evidence ) 44,45.
Avoiding touching the uterine fundus is one of the most important factors leading to a successful transfer. However the depth of the catheter inside the uterus and how far from the fundus should the embryo should be placed in the uterus was the subject of 4 randomized trials 43,46 . Coroleu et al 2002 43 studied a total of 180 consecutive patients undergoing ultrasound-guided embryo transfer were randomized to three study groups according to the distance between the tip of the catheter and the uterine fundus at the moment of the embryo deposition in the lumen of the endometrial cavity: group 1: 10 +/- 1.5 mm; group 2: 15 +/- 1.5 mm; group 3: 20 +/- 1.5 mm. the pregnancy rate higher in group 2 and 3 .Again in 2015 the same finding were found by Kwon et al 45, Francoet al 200444 in a randomized controlled study found no difference in implantation rate and pregnancy rate when the embryo was placed in the upper vs lower half of the endometrial cavity . while Kwon et al 201545 found no difference whether it was put 2 cm from the fundus vs the uterine cavity midpoint .
Abdelmassih et al 200747studied the effect of introducing the outer sheath inside the cavity and found that leaving the sheath outside the internal os increases the pregnancy rate.
6. Antibiotics
before embryo transfer
● It is not recommended to prescribe antibiotics with embryo transfer. (conditional recommendation - moderate grade evidence )49.
350 patients were randomized by Brook et al 2006 48 to receive either prophylactic antibiotics or no antibiotics. The antibiotic used was amoxicillin and clavulanic acid on the day before and the day of transfer. The catheter tips were cultured after the transfer. While the antibiotics significantly reduced catheter contamination rates, the clinical pregnancy rates between the two groups were not different.
Kroon et al 201249 performed systematic review and found no additional data to justify using antibiotic therapy before transfer with respect to increasing the life birth rate.
In women with symptoms of infection, it is recommended to perform specific microbiological testing and take appropriate actions 50.
7. Bed rest after transfer
Bed rest is not recommended after embryo transfer as it does not increase pregnancy rates (Strong recommendation- high grade evidence) 51,52.
Meta Analysis included 14 studies, none of them showed any benefit of bed rest of any duration. Three RCTs between 1997 and 2004 included 712 patients randomized to different periods of bed rest and showed no benefit of any of the following durations: 1 hour vs 24 hours (N1⁄4378), 20 minutes vs 24 hours (N1⁄4182), and immediate ambulation vs 30 minutes (N1⁄4152) .51
In contrast to the studies that have shown no benefit, one well-designed recent RCT demonstrated possible harm . Two hundred-forty patients undergoing their first IVF cycle were randomized to either 10 minutes of bed rest or immediate ambulation. This study demonstrated that the live-birth rates were significantly (P=.02) higher in the no bed rest group (56.7%) when compared to 10 minutes of rest (41.6%)52.
8. Removing mucus from the cervical canal
▪ No enough evidence to recommend routine removal of cervical mucous from the cervix before embryo transfer (conditional recommendation -very low grade evidence ) 53,55
Removing the cervical mucus might prevent clogging of the catheter tip , retraction of the embryos or displacing the mucous inside the uterine cavity which might affect the implantation . However manipulating the cervix can increase uterine contractility which decreases implantation 53,55.
Moini et al 2011 53did a randomized trial on mucous aspiration prior to ET. Five hundred patients were included and a significant difference was found both in the pregnancy rate and delivery rate (39vs 22% and 33.6 vs 17.4).However Craciunas et al 2014 54 compiled eight RCTs involving 1,715 women which were systematically analyzed. A meta-analysis from the available moderate to low quality trials provides very little evidence of an overall benefit of cervical mucus removal before embryo transfer for women undergoing IVF/ICSI.
A Cochrane review on cervical mucous flushing prior to ET by Derks et al 2009 did not find any improvement in pregnancy rate with flushing55.
9. Timing to remove the catheter after deposition of the embryos.
▪ There is No specific time to recommend removal of the embryo transfer catheter after embryo transfer. (conditional recommendation-moderate grade evidence) 56
After deposition of the embryo there is evidence from one randomized trial that there is no difference between immediate withdrawal or waiting for 30 seconds (Martiniz et al 2001)56.
Similarly cohort study by Soroga et al 201057 found no difference between waiting 60 seconds versus immediate withdrawal
- Clinical indicators for monitoring
We recommend a strict follow up number of embryos transferred. Also follow up of the documentation of the reason for transferring more than one embryo.
➡️Update of guideline
This guideline will be updated whenever there is new evidence
➡️Research gaps:
There is a need to perform research on the prevalence of multiple pregnancy in Egypt following ART and ovulation induction and to follow up these dates after implementation of these guidelines .
- REFERENCES
1. Practice Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Performing the embryo transfer: a guideline. Fertil Steril. 2017 Apr;107(4):882-896. doi: 10.1016/j.fertnstert.2017.01.025. PMID: 28366416
2. Alteri A, Arroyo G, Baccino G, et al. ESHRE guideline: number of embryos to transfer during IVF/ICSI † ESHRE Guideline Group on the Number of Embryos to. Published online 2024. doi:10.1093/humrep/deae010
3. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2021;116(3):651-654. doi:10.1016/j.fertnstert.2021.06.050
4 .Gerris JMR. Single embryo transfer and IVF/ICSI outcome: A balanced appraisal. Hum Reprod Update. 2005;11(2):105-121. doi:10.1093/humupd/dmh049
5. Wyns C, De Geyter C, Calhaz-Jorge C, et al. ART in Europe, 2017: Results generated from European registries by ESHRE. Hum Reprod Open. 2021;2021(3). doi:10.1093/hropen/hoab026
6. Theobald R, SenGupta S, Harper J. The status of preimplantation genetic testing in the UK and USA. Human Reproduction. 2021;35(4):986-998. doi:10.1093/HUMREP/DEAA034
7. Forman EJ, Hong KH, Ferry KM, et al. In vitro fertilization with single euploid blastocyst transfer: A randomized controlled trial. Fertil Steril. 2013;100(1). doi:10.1016/j.fertnstert.2013.02.056
8. Grifo JA, Hodes-Wertz B, Lee HL, Amperloquio E, Clarke-Williams M, Adler A. Single thawed euploid embryo transfer improves IVF pregnancy, miscarriage, and multiple gestation outcomes and has similar implantation rates as egg donation. J Assist Reprod Genet. 2013;30(2):259-264. doi:10.1007/s10815-012-9929-1
9. Tobias T, Sharara FI, Franasiak JM, Heiser PW, Pinckney-Clark E. Promoting the use of elective single embryo transfer in clinical practice. Fertil Res Pract. 2016;2(1). doi:10.1186/s40738-016-0024-7
10 . Gardner DK, Phil D, Surrey E, et al. Single blastocyst transfer: a prospective randomized trial. doi:10.1016/j.fertnstert.2003
11. Gerris J, De Neubourg D, Mangelschots K, Royen E Van, Van De Meerssche M, Valkenburg M. Prevention of Twin Pregnancy after In-Vitro Fertilization or Intracytoplasmic Sperm Injection Based on Strict Embryo Criteria: A Prospective Randomized Clinical Trial. Vol 14. Templeton and Morris; 1999.
12 . Martikainen H, Tiitinen A, Tomás C, et al. One versus Two Embryo Transfer after IVF and ICSI: A Randomized Study. Vol 16.; 2001.
13 . Moustafa MK, Sheded SA, El Aziz Mousta MA. Elective single embryo transfer versus double embryo transfer in assisted reproduction. Reprod Biomed Online. 2008;17(1):82-87. doi:10.1016/S1472-6483(10)60297-0
14 . Thurin A, Hausken J, Hillensjö T, et al. Elective Single-Embryo Transfer versus Double-Embryo Transfer in in Vitro Fertilization. www.nejm.org
15. Impact of Transferring a Poor Quality Embryo Along with a Good Quality Embryo on Pregnancy Outcomes in IVF:ICSI Cycles- a Retrospective Study.
16. Theodorou E, Jones BP, Cawood S, Heath C, Serhal P, Ben-Nagi J. Adding a low-quality blastocyst to a high-quality blastocyst for a double embryo transfer does not decrease pregnancy and live birth rate. Acta Obstet Gynecol Scand. 2021;100(6):1124-1131. doi:10.1111/aogs.14088
17. Wang W, Cai J, Liu L, et al. Does the transfer of a poor quality embryo with a good quality embryo benefit poor prognosis patients? Reproductive Biology and Endocrinology. 2020;18(1). doi:10.1186/s12958-020-00656-2
18. Park DS, Kim JW, Chang EM, Lee WS, Yoon TK, Lyu SW. Strategies in the transfer of varying grades of vitrified-warmed blastocysts in women aged over 35 years: A propensity-matched analysis. Journal of Obstetrics and Gynaecology Research. 2019;45(4):849-857. doi:10.1111/jog.13897
19. Dobson SJA, Lao MT, Michael E, Varghese AC, Jayaprakasan K. Effect of transfer of a poor quality embryo along with a top quality embryo on the outcome during fresh and frozen in vitro fertilization cycles. Fertil Steril. 2018;110(4):655-660. doi:10.1016/j.fertnstert.2018.05.010
20. Arab S, Badegiesh A, Aldhaheri S, Son WY, Dahan MH. What Are the Live Birth and Multiple Pregnancy Rates When 1 Versus 2 Low-Quality Blastocysts Are Transferred in a Cryopreserved Cycle? a Retrospective Cohort Study, Stratified for Age, Embryo Quality, and Oocyte Donor Cycles. Reproductive Sciences. 2021;28(5):1403-1411. doi:10.1007/s43032-020-00404-2
21. Chen S, Du H, Liu J, Liu H, Li L, He Y. Live birth rate and neonatal outcomes of different quantities and qualities of frozen transferred blastocyst in patients requiring whole embryo freezing stratified by age. BMC Pregnancy Childbirth. 2020;20(1). doi:10.1186/s12884-020-03353-5
22. Richter KS, Ginsburg DK, Shipley SK, et al. Factors associated with birth outcomes from cryopreserved blastocysts: experience from 4,597 autologous transfers of 7,597 cryopreserved blastocysts. In: Fertility and Sterility. Vol 106. Elsevier Inc.; 2016:354-362.e2. doi:10.1016/j.fertnstert.2016.04.022.
23. Engmann L, Maconochie N, Tan SL, Bekir J. Trends in the Incidence of Births and Multiple Births and the Factors That Determine the Probability of Multiple Birth after IVF Treatment. Vol 16.; 2001.
24. Kupka MS, Dorn C, Richter O, Felberbaum R, Van Der Ven H. Impact of reproductive history on in vitro fertilization and intracytoplasmic sperm injection outcome: evidence from the German IVF Registry. doi:10.1016/S0015-0282(03)
25. Molloy D, Doody ML, Breen T. Second time around: A study of patients seeking second assisted reproduction pregnancies. Fertil Steril. 1995;64(3):546-551. doi:10.1016/s0015-0282(16)57790-5
26. Simon A, Ronit C, Lewin A, Mordel N, Zajicek G, Laufer N. Conception rate after in vitro fertilization in patients who conceived in a previous cycle. Fertil Steril. 1993;59(2):343-347. doi:10.1016/S0015-0282(16)55672-6
27. Bhattacharya S, Maheshwari A, Mollison J. Factors associated with failed treatment: An analysis of 121,744 women embarking on their first IVF Cycles. PLoS One. 2013;8(12). doi:10.1371/journal.pone.0082249
28. Lintsen AME, Eijkemans MJC, Hunault CC, et al. Predicting ongoing pregnancy chances after IVF and ICSI: A national prospective study. Human Reproduction. 2007;22(9):2455-2462. doi:10.1093/humrep/dem183
29. McLernon DJ, Steyerberg EW, Te Velde ER, Lee AJ, Bhattacharya S. Predicting the chances of a live birth after one or more complete cycles of in vitro fertilisation: Population based study of linked cycle data from 113 873 women. BMJ (Online). 2016;355. doi:10.1136/bmj.i5735
30. Roberts SA, Hirst WM, Brison DR, Vail A. Embryo and uterine influences on IVF outcomes: An analysis of a UK multi-centre cohort. Human Reproduction. 2010;25(11):2792-2802. doi:10.1093/humrep/deq213
31. Angelini A, Brusco GF, Barnocchi N, El-Danasouri I, Pacchiarotti A,
Selman HA. Impact of physician performing embryo transfer on pregnancy rates in an assisted reproductive program. J Assist Reprod Genet 2006;23: 329–32, Level II-2
32. Bodri, D., Colodrón, M., García, D., Obradors, A., Vernaeve, V., Coll, O., 2011. Transvaginal versus transabdominal ultrasound guidance for embryo transfer in donor oocyte recipients: a randomized clinical trial. Fertil. Steril. 95, 2263–2268, 2268.e1.
33. Karavani, G., Ben-Meir, A., Shufaro, Y., Hyman, J.H., Revel, A., 2017. Transvaginal ultrasound to guide embryo transfer: a randomized controlled trial. Fertil. Steril. 107, 1159–1165
34. Porat, N., Boehnlein, L.M., Schouweiler, C.M., Kang, J., Lindheim, S.R., 2010. Interim analysis of a randomized clinical trial comparing abdominal versus transvaginal ultrasound-guided embryo transfer. J. Obstet. Gynaecol. Res. 36,384–392.
35. Sundstro¨m P, Wramsby H, Persson PH, Liedholm P. Filled bladder sim- . plifies human embryo transfer. Br J Obstet Gynaecol 1984;91:506–507 Tıras B, Cenksoy PO. Practice of embryo transfer: recommendations during and after. Semin Reprod Med 2014;32:291–296
36. Lewin A, Schenker JG, Avrech O, Shapira S, Safran A, Friedler S. The . role of uterine straightening by passive bladder distension before . embryo transfer in IVF cycles. J Assist Reprod Genet 1997;14:32–34.
37. Lewin A, Schenker JG, Avrech O, Shapira S, Safran A, Friedler S. The . role of uterine straightening by passive bladder distension before . embryo transfer in IVF cycles. J Assist Reprod Genet 1997;14:32–34.
38. Abou-Setta AM, Mansour RT, Al-Inany HG, Aboulghar MM, Aboulghar MA, Serour GI. Among women undergoing embryo transfer, is the probability of pregnancy and live birth improved with ultrasound guidance over clinical touch alone? A systemic re- view and meta-analysis of prospective randomized trials. Fertil Steril 2007;88:333–341.
39. Abou-Setta A.M. Al-Inany H.G. Mansour R.T. Serour G.I. Aboulghar M.A. Soft versus firm embryo transfer catheters for assisted reproduction: a systematic review and meta-analysis.Hum Reprod. 2005; 20 (Level III): 3114-3121
40.van Weering H.G. Schats R. McDonnell J. Vink J.M. Vermeiden J.P. Hompes P.G. The impact of the embryo transfer catheter on the pregnancy rate in IVF.Hum Reprod. 2002; 17 (Level I): 666-670.
41.Ghazzawi IM, Al-Hasani S, Karaki R, Souso S. Transfer technique and catheter choice influence the incidence of transcervical embryo expulsion and the outcome of IVF. Hum Reprod 1999;14:677–82, Level I.
42. van der Ven H, Diedrich K, Al-Hasani S, Pless V, Krebs D. The effect of general anaesthesia on the success of embryo transfer following human in- vitro fertilization. Hum Reprod 1988;3(Suppl 2):81–3.
43.Coroleu B. Barri P.N. Carreras O. Martinez F. Parriego M. Hereter L. et al.The influence of the depth of embryo replacement into the uterine cavity on implantation rates after IVF: a controlled, ultrasound-guided study. Hum Reprod. 2002; 17 (Level I): 341-346
44. Franco Jr., J.G. Martins A.M. Baruffi R.L. Mauri A.L. Petersen C.G. Felipe V. et al.Best site for embryo transfer: the upper or lower half of endometrial cavity?.Hum Reprod. 2004; 19 (Level I): 1785-1790
45. Kwon H. Choi D.H. Kim E.K. Absolute position versus relative position in embryo transfer: a randomized controlled trial.Reprod Biol Endocrinol. 2015; 13 (Level I): 78
46. Pacchiarotti A. Mohamed M.A. Micara G. Tranquilli D. Linari A. Espinola S.M. et al.The impact of the depth of embro replacement on IVF outcome.J Assist Reprod Genet. 2007; 24 (Level I): 189-193.
47. Abdelmassih VG, Neme RM, Dozortsev D, Abdelmassih S, Diamond MP, Abdelmassih R. Location of the embryo-transfer catheter guide before the internal uterine os improves the outcome of in vitro fertilization. Fertil Steril 2007;88:499–503, Level II-2.
48. Brook N. Khalaf Y. Coomarasamy A. Edgeworth J. Braude P. A randomized controlled trial of prophylactic antibiotics (co-amoxiclav) prior to embryo transfer.Hum Reprod. 2006; 21 (Level I): 2911-2915
49. Kroon B. Hart R.J. Wong B.M. Ford E. Yazdani A. Antibiotics prior to embryo transfer in ART.Cochrane Database Syst Rev. 2012; (Level III): Cd008995
50.D'Angelo A, Panayotidis C, Amso N, Marci R, Matorras R, Onofriescu M, Turp AB, Vandekerckhove F, Veleva Z, Vermeulen N. et al.; ESHRE Working Group on Ultrasound in ART. Recommendations for good practice in ultrasound: oocyte pick up. Hum Reprod Open2019;2019:hoz025.
51. Sharif K, Afnan M, Lashen H, Elgendy M, Morgan C, Sinclair L. Is bed rest following embryo transfer necessary? Fertil Steril 1998;69:478–81, Level II-3.
52. Gaikwad S, Garrido N, Cobo A, Pellicer A, Remohi J. Bed rest after embryo transfer negatively affects in vitro fertilization: a randomized controlled clinical trial. Fertil Steril 2013;100:729–35, Level I.
53.Moini A, Kiani K, Bahmanabadi A, Akhoond M, Akhlaghi A.. Improvement in pregnancy rate by removal of cervical discharge prior to embryo transfer in ICSI cycles: a randomised clinical trial. Aust N Z J Obstet Gynaecol 2011;51:315–320.
54.Craciunas L, Tsampras N, Fitzgerald C.. Cervical mucus removal before embryo transfer in women undergoing in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril 2014;101:1302–1307.
55.Derks RS, Farquhar C, Mol BWJ, Buckingham K, Heineman MJ.. Techniques for preparation prior to embryo transfer. Cochrane Database of Systematic Reviews 2009;4:CD007682.
56. Martinez F. Coroleu B. Parriego M. Carreras O. Belil I. Parera N. et al. Ultrasound-guided embryo transfer: immediate withdrawal of the catheter versus a 30 second wait.Hum Reprod. 2001; 16 (Level I): 871-874
57.Sroga J.M. Montville C.P. Aubuchon M. Williams D.B. Thomas M.A. Effect of delayed versus immediate embryo transfer catheter removal on pregnancy outcomes during fresh cycles.Fertil Steril. 2010; 93 (Level II-2): 2088-2090
58. Alteri A, Arroyo G, Baccino G, et al. ESHRE guideline: number of embryos to transfer during IVF/ICSI † ESHRE Guideline Group on the Number of Embryos to. Published online 2024. doi:10.1093/humrep/deae010
59. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2021;116(3):651-654. doi:10.1016/j.fertnstert.2021.06.050
60. Urman B, Yakin K. New Turkish legislation on assisted reproductive techniques and centres: A step in the right direction? Reprod Biomed Online. 2010;21(6):729-731. doi:10.1016/j.rbmo.2010.06.030
61. Practice Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Performing the embryo transfer: a guideline. Fertil Steril. 2017 Apr;107(4):882-896. doi: 10.1016/j.fertnstert.2017.01.025. PMID: 28366416.
2-896, APRIL 2017
62. Gerris JMR. Single embryo transfer and IVF/ICSI outcome: A balanced appraisal. Hum Reprod Update. 2005;11(2):105-121. doi:10.1093/humupd/dmh049
63. Forman EJ, Hong KH, Ferry KM, et al. In vitro fertilization with single euploid blastocyst transfer: A randomized controlled trial. Fertil Steril. 2013;100(1). doi:10.1016/j.fertnstert.2013.02.056
64. Grifo JA, Hodes-Wertz B, Lee HL, Amperloquio E, Clarke-Williams M, Adler A. Single thawed euploid embryo transfer improves IVF pregnancy, miscarriage, and multiple gestation outcomes and has similar implantation rates as egg donation. J Assist Reprod Genet. 2013;30(2):259-264. doi:10.1007/s10815-012-9929-1
65. Gardner DK, Phil D, Surrey E, et al. Single blastocyst transfer: a prospective randomized trial. doi:10.1016/j.fertnstert.2003
66. Gerris J, De Neubourg D, Mangelschots K, Royen E Van, Van De Meerssche M, Valkenburg M. Prevention of Twin Pregnancy after In-Vitro Fertilization or Intracytoplasmic Sperm Injection Based on Strict Embryo Criteria: A Prospective Randomized Clinical Trial. Vol 14. Templeton and Morris; 1999.
67. Martikainen H, Tiitinen A, Tomás C, et al. One versus Two Embryo Transfer after IVF and ICSI: A Randomized Study. Vol 16.; 2001.
68. Moustafa MK, Sheded SA, El Aziz Mousta MA. Elective single embryo transfer versus double embryo transfer in assisted reproduction. Reprod Biomed Online. 2008;17(1):82-87. doi:10.1016/S1472-6483(10)60297-0
69. Thurin A, Hausken J, Hillensjö T, et al. Elective Single-Embryo Transfer versus Double-Embryo Transfer in in Vitro Fertilization. www.nejm.org
70. Penzias A, Bendikson K, Butts S, et al. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901-903.
71. Engmann L, Maconochie N, Tan SL, Bekir J. Trends in the Incidence of Births and Multiple Births and the Factors That Determine the Probability of Multiple Birth after IVF Treatment. Vol 16.; 2001.
72. Kupka MS, Dorn C, Richter O, Felberbaum R, Van Der Ven H. Impact of reproductive history on in vitro fertilization and intracytoplasmic sperm injection outcome: evidence from the German IVF Registry. doi:10.1016/S0015-0282(03)
73. Molloy D, Doody ML, Breen T. Second time around: A study of patients seeking second assisted reproduction pregnancies. Fertil Steril. 1995;64(3):546-551. doi:10.1016/s0015-0282(16)57790-5
74. Simon A, Ronit C, Lewin A, Mordel N, Zajicek G, Laufer N. Conception rate after in vitro fertilization in patients who conceived in a previous cycle. Fertil Steril. 1993;59(2):343-347. doi:10.1016/S0015-0282(16)55672-6
75. Bhattacharya S, Maheshwari A, Mollison J. Factors associated with failed treatment: An analysis of 121,744 women embarking on their first IVF Cycles. PLoS One. 2013;8(12). doi:10.1371/journal.pone.0082249
76. Lintsen AME, Eijkemans MJC, Hunault CC, et al. Predicting ongoing pregnancy chances after IVF and ICSI: A national prospective study. Human Reproduction. 2007;22(9):2455-2462. doi:10.1093/humrep/dem183
77. McLernon DJ, Steyerberg EW, Te Velde ER, Lee AJ, Bhattacharya S. Predicting the chances of a live birth after one or more complete cycles of in vitro fertilisation: Population based study of linked cycle data from 113 873 women. BMJ (Online). 2016;355. doi:10.1136/bmj.i5735
78. Roberts SA, Hirst WM, Brison DR, Vail A. Embryo and uterine influences on IVF outcomes: An analysis of a UK multi-centre cohort. Human Reproduction. 2010;25(11):2792-2802. doi:10.1093/humrep/deq213