Acute Rhinosinusitis
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Acute Rhinosinusitis |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:01 PM |
Description
"last update: 5 August 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdelaziz,6 Tarek Ghannoum,7 Mahmoud Youssef8
Rhinology Chief Manager: Ashraf Khaled4
Rhinology Excutive Manager: Ahmed Elfarouk,1 Mohamed Elsharnouby,9 Hossam Elsherif6
Assembly Board: Ahmed Ragab,2 Reda Kamel,1 Ashraf Khaled,4 Baliegh Hamdy,3 Ahmed Elfarouk,1 Mohamed Elsharnouby,9 Hossam Elsherif6
Grading team (In alphabetical order)
Hesham Al Adl,5 Ibrahim Abd-elshafy,2 Anas Askora,9 Magdy Eisa,6 Diaa Elhinnawi,10 Esmail Elnashar,11 Hossam Elsisi,5 Amr Gouda,9 Islam H. Herzallah,11 Sayed Kaddah,12 Yaser Nour,13 Mohamed Qotb,14 Amr Rabie,9 Nassim Talaat,1 Mohamed Osama Tamoum6
Reviewing Board: Mohamed Hassab,13 Abdelaziz Elsherif,15 Alaa Ghita,16 Khaled Belasy17, Tagreed Farahat 18, Seham Ragab 19
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 3Otorhinolaryngology Department, Faculty of Medicine/Minia University, 4Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 6Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 10Otorhinolaryngology Department, Faculty of Medicine/ Suez Canal University, 11Otorhinolaryngology Department, Faculty of Medicine/ Zagazig University, 12Otorhinolaryngology Department, Faculty of Medicine/Al Azhar University, 13Otorhinolaryngology Department, Faculty of Medicine/ Alexandria University, 14Otorhinolaryngology Department, Faculty of Medicine/ Fayoum University, 15Otorhinolaryngology Department, Faculty of Medicine/ Al Azhar Assuit University, 16Otorhinolaryngology Department, Faculty of Medicine/ Military Medical Academy, 17Otorhinolaryngology Department, Police Academy, The Medical Sector MOI.18Family medicine departmentMenoufia University,Pediatric department,Menoufia university
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Abbreviations
AAP American academy of pediatricians
AAFP American academy of family practitioners
ARS Acute Rhinosinusitis
ABRS Acute bacterial rhinosinusitis
CPG Clinical Practice Guideline
ESS Endoscopic sinus surgery
INC Intranasal corticosteroids
GRADE Grading of Recommendations Assessment, Development and Evaluation
MM Middle meatus
RARS Recurrent acute rhinosinusitis
SPT Skin prick test
VRS Viral rhinosinusitis
- Executive Summary
1- Definition: Acute rhinosinusitis (ARS) is considered when symptoms and signs are present less than 4 weeks. (Strong recommendation)
2- Diagnosis of acute ARS through symptoms/signs and duration:
-Symptoms must include most of the followings (All can be included in CPODS)
C: Congestion, P: Pain, O: Obstruction,D: Drainage/Discharge,S: Smell affection
(Strong recommendation)
3- A thorough physical examination that includes inspection , palpation of the maxillary and frontal sinus, as well as anterior rhinoscopy (evidence of inflammation, mucosal oedema, and discharge). (Conditional recommendation)
4- Objective evidence of ARS on nasal endoscopy, antral puncture, or radiographic imaging (X-ray, ultrasonography, or CT) is not required for the diagnosis in uncomplicated cases. (Strong recommendation against)
5- ESR and CRP are inflammatory markers found to be elevated during ARS, but they are not routinely used for diagnosis because of their limited specificity. It can be used in COVID-19 . (Conditional recommendation)
6- Differentiate viral from bacterial ARS: -Duration is thought to be a key factor differentiating ABRS from AVR, with persistence of symptoms beyond 7-10 days or worsening of symptoms after 5 days being indicators of development of post-viral ABRS.
-Clinical factors associated with symptoms and signs ABRS include:
Timing of the disease, worsening of the disease, purulent nasal discharge on rhinoscopy, localized unilateral pain, severe pain over the teeth and maxilla, and fever > 38˚C. (conditional recommendation)
7- Consider initial watchful waiting in uncomplicated cases with assurance of follow up. (conditional recommendation)
8- Institution of antibiotic therapy if:
A. No improvement after 4-7 days or worsening at any time,
B. Mitigating circumstances with drug resistance e.g., severe symptoms and immunocompromised states
C. Concern for impending complications
D. Suspected odontogenic source
E. Prior antibiotics (1 month), prior hospitalization (5 days) and comorbidities.
(Conditional recommendation)
9- If a decision is made to treat ABRS with an antibiotic, the clinician should prescribe amoxicillin with clavulanate (conditional recommendation)
10- First time non-responders can be based on lack of clinical improvement following treatment within 5 days in adults and 3 days in children. -Use second line antimicrobial agents. (Conditional recommendation)
11- In patients with ABRS suspected to have suppurative complications, axial, coronal and sagittal views with contrast-enhanced computed tomography (CT) is recommended. (Conditional recommendation)
12- Recurrent acute rhinosinusitis RARS is diagnosed when At least 4 attacks of ABRS/year are documented (Conditional recommendation)
-Consider Nasal endoscopy and/or CT imaging are an option during at least one episode of suspected RARS (Conditional recommendation)
-Endoscopic sinus surgery (ESS) is recommended for patients with RARS. (Conditional recommendation)
- Introduction, scope and audience
Rhinosinusitis affects about 1 in 8 adults. More than 1 in 5 antibiotics prescribed in adults are for rhinosinusitis, making it the fifth most common diagnosis responsible for antibiotic therapy. Rhinosinusitis is defined as symptomatic inflammation of the paranasal sinuses and nasal cavity. The term rhinosinusitis is preferred because sinusitis is almost always accompanied by inflammation of the contiguous nasal mucosa. Therefore, rhinosinusitis is used in the remainder of the guideline 1-5.
➡️Scope
The scopes are to improve diagnostic accuracy for acute rhinosinusitis, promote appropriate use of ancillary tests to confirm diagnosis and guide management, and promote judicious use of systemic and topical therapy specially for systemic antibiotic.
➡️Target audience: Otorhinolaryngology, Pediatricians and Family physicians,
- Methods
➡️Methods of development
➡️Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Chief Manager, Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Search method
Electronic database searched:
PubMed, Medline, Egyptian Knowledge Bank, Web of science, Scopus
➡️Keywords:
Acute sinusitis, Acute Rhinosinusitis, Guidelines
➡️Time period searched: from January 2010 to December 2022.
➡️Results
Five national otorhinolaryngologists reviewed the guidelines available. Guidelines from the American Academy of Otolaryngology--Head and Neck Surgery gained the highest scores as regards currency, contents and quality in comparison to other searched guidelines 5-13.
It was graded GRADE by twenty-two experts and reviewed by 6 expert reviewers from different related specialties ORL, Family Medicine and pediatrics. The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
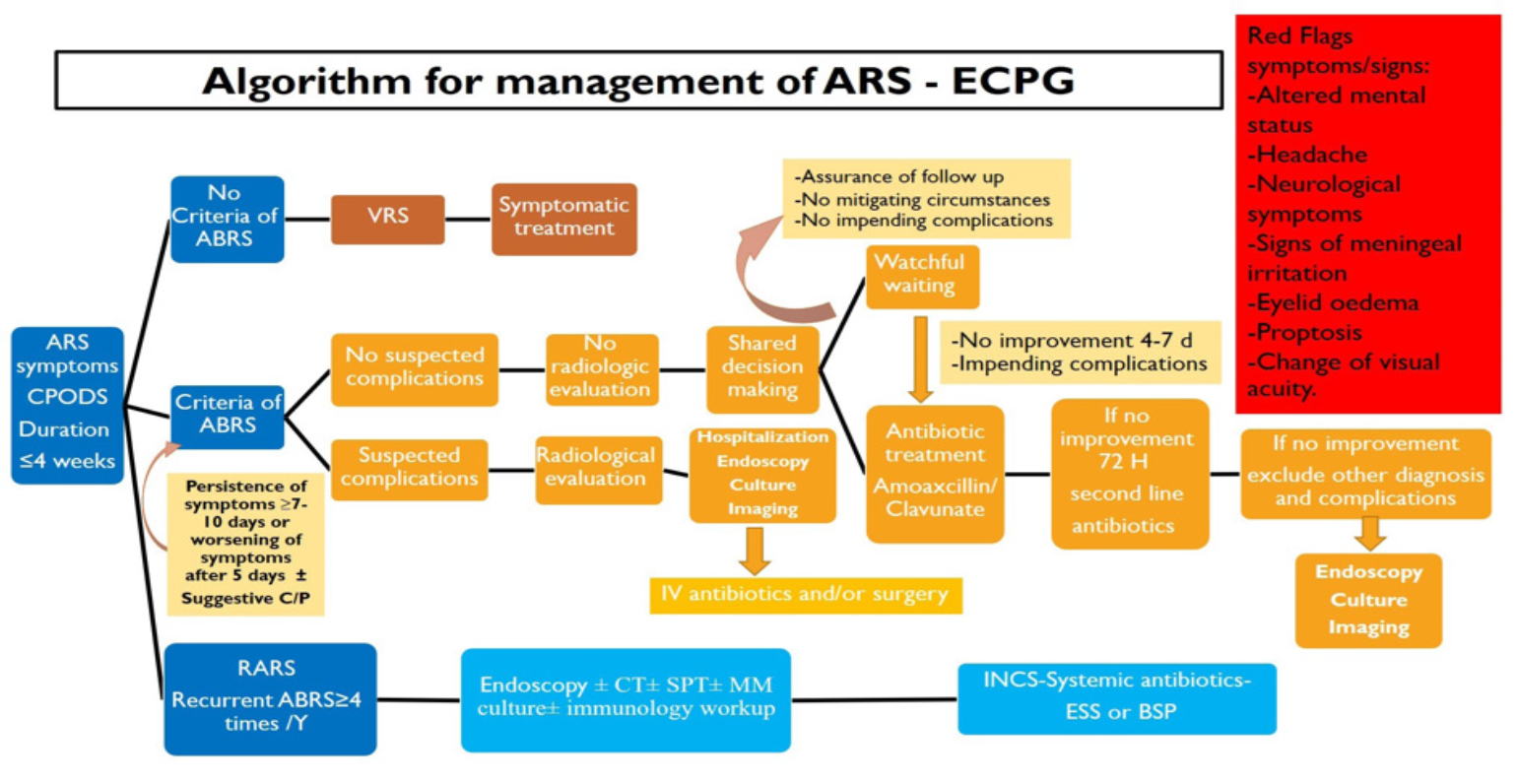
The following statements and flowchart were adapted from the Guidelines from the American Academy of Otolaryngology--Head and Neck Surgery 12 which received the highest scores as regards the currency, contents, and quality in comparison to other searched guidelines 6-13.
Recommendations statements
|
Statement topic |
Action recommendation |
Level of evidence |
Strength of recommendations |
Study type |
References |
|
1.Definition:according to the duration |
Acute rhinosinusitis (ARS) is considered when symptoms and signs are present less than 4 weeks. |
Very low |
Strong recommendation |
Expert opinion
|
12,14 |
|
2.Diagnosis:symptoms
|
Acute rhinosinusitis (ARS) usually presents with multiple symptoms including nasal congestion or blockage, nasal drainage or postnasal drainage (PND), and facial pressure/pain. |
Very low
|
Strong recommendation |
Expert opinion
|
12,14 |
|
3.Diagnosis:parameters
|
Diagnosis is clinical and depends on symptoms and signs rather than radiology. |
Very low |
Conditional recommendation |
Expert opinion
|
12,14 |
|
4.Diagnosis:Examination
|
A thorough physical examination that includes inspection, palpation of the maxillary and frontal sinus, as well as anterior rhinoscopy (evidence of inflammation, mucosal oedema, and discharge). |
Very Low |
Conditional recommendation |
Expert opinion
|
12,15 |
|
5.Diagnosis:Investigations
|
Objective evidence of ARS on nasal endoscopy, antral puncture, or radiographic imaging (X-ray, ultrasonography, or CT) is not required for the diagnosis in uncomplicated cases |
High |
Strong Recommendation (against) |
Systematic review
|
12,16 |
|
6.Diagnosis:Investigations
|
-ESR and CRP are inflammatory markers found to be elevated during ARS, but they are not routinely used for diagnosis because of their limited specificity. -They may have some role in COVID-19 related symptoms |
Moderate |
Conditional recommendation |
Systematic review
|
12,16 |
|
7. Differentiating viral from bacterial:
|
-Differentiating between Acute bacterial rhinosinusitis (ABRS) and acute viral rhinosinusitis (AVR) can be challenging even in the setting of endoscopy and cultures. Close follow-up of patient symptomology can often help in making the diagnosis, especially for patients that do not improve with supportive care. -Duration is thought to be a key factor differentiating ABRS from AVR, with persistence of symptoms beyond 7-10 days or worsening of symptoms after 5 days being indicators of development of post-viral ABRS. -Clinical factors associated with ABRS include without evidence: Timing of the disease, worsening of the disease, purulent nasal discharge on rhinoscopy, localized unilateral pain, severe pain over the teeth and maxilla, and fever > 38˚C. |
Moderate
|
Strong recommendation |
Systematic review |
12,17 |
|
8. Pathophysiology of ARS:-Anatomic variants and septal Deviation
-Nasal allergy
-Viruses
-Odontogenic rhinosinusitis |
-The evidence for association between ARS and anatomic variants is conflicting and limited and largely inferred from a small number of studies. -Population-based studies seem to support an association between allergic rhinitis (AR) and ARS. -The epidemiologic studies show that a subset of patients with viral URI will develop clinical ARS. -The current literature demonstrates an absence of a well-designed and published investigation into the role of odontogenic infections in ARS. |
Moderate
Low
High
Very Low
|
Conditional
Strong
strong
Conditional |
Systematic review
Cross sectional
Systematic review
Expert consensus |
18
19
20
21 |
|
9.Treatment: Antibiotics
|
- Consider initial watchful waiting in uncomplicated cases, with institution of antibiotic therapy if no improvement after 4-7 days or worsening at any time, or for mitigating circumstances with drug resistance e.g., including severe symptoms, immunocompromised state, concern for impending complications, suspected odontogenic source, prior antibiotics (1 month), prior hospitalization (5 days) and comorbidities. -Watchful waiting should be offered only when there is assurance of follow-up, such that antibiotic therapy is started if the patient’s condition fails to improve |
Moderate |
Conditional recommendation |
Systematic review |
12,22,23 |
|
10.Choice of antibiotic for ABRS
|
-If a decision is made to treat ABRS with an antibiotic agent, the clinician should prescribe amoxicillin with clavulanate as first-line therapy for 5 to 10 d for most adults. -Options after failing amoxicillin + clavulanate or for penicillin allergy include trimethoprim-sulfamethoxazole, doxycycline, or a fluoroquinolone. |
Moderate |
Conditional recommendation |
Systematic review |
12,22,23 |
|
11.Treatment:Corticosteroids (INC) -Systemic Corticosteroids
|
-INCS can be used according to the doctor judgment as monotherapy in mild to moderate ARS or as adjuvant to antibiotic therapy in severe cases of ARS. -Given the conflicting evidence, there is no recommendation for systemic corticosteroids in cases of uncomplicated ARS |
High
Moderate |
Strong recommendation
Strong recommendation against |
Systematic review
Randomized Controlled Trial |
12,24,25
26 |
|
12.Topical saline spray and irrigation
|
Saline irrigation may be used in adjunct with antibiotics for ABRS. |
Moderate |
Strong recommendation |
Systematic review |
12,27 |
|
13. Decongestant
|
Decongestants are an option in ABRS. Decongestants can reduce congestion in patients with ABRS however side effects should be considered. |
Moderate |
Conditional recommendation |
Systematic review |
12,28 |
|
14.Antihistamimine
|
Antihistamines are an option in ABRS with comorbid AR and can be used to decrease symptoms of AR. |
Moderate |
Conditional recommendation |
Systematic review |
12,29 |
|
15.Others
|
no recommendation can be given for mucolytics, herbals in ABRS. |
Very Low |
No recommendation |
Case series |
12,30 |
|
16.Treatment: Adjuvants for VRS
|
-Clinicians may recommend: Analgesics, topical intranasal steroids INC, and/or nasal saline irrigation NSI for symptomatic relief of VRS |
Moderate |
Conditional recommendation |
Systematic review
|
12,14,31 |
|
17.Treatment: Adjuvants for ABRS
|
- Clinicians may recommend analgesics, topical intranasal steroids, and/or NSI |
Moderate |
Conditional recommendation |
Systematic review
|
12,14,31 |
|
18.Complications:
|
- In patients with ABRS suspected to have suppurative complications, axial, coronal and sagittal views with contrast-enhanced computed tomography (CT) is recommended to localize the infection and to guide further treatment. -Magnetic resonance imaging (MRI) provides soft tissue visualization and is useful when there is concern for intracranial involvement. Magnetic resonance venography may be useful for evaluation of the cavernous sinus and other vasculature. -The hallmarks of management are swift diagnosis, rapid initiation of broad-spectrum intravenous antibiotics, and in many cases surgical intervention. -While endoscopic sinus surgery (ESS) is usually a sufficient approach for addressing orbital complications, open neurosurgical intervention is often required for even sub-centimeter intracranial abscess |
Low
|
Conditional recommendation |
Case series |
12,32 |
|
19.Recurrent Acute Rhinosinusitis (RARS) -Diagnosis: -Treatment: I-NC 2. Antibiotics 3. Endoscopic sinus surgery ESS /Balloon sinus dilatation (BSD)
|
- At least 4 attacks of ABRS are a required criterion -Nasal endoscopy and/or CT imaging are an option during at least one episode of suspected RARS to appropriately confirm and diagnose RARS, and distinguish it from other diagnoses such as allergy exacerbation or primary headache syndromes. -Consider immunologic testing, allergic testing, and bacterial culture in patients with concern for RARS -Option for use of INCS spray for sinonasal symptoms during acute exacerbations of RARS. -As in ABRS -ESS or BSD is recommended for patients with RARS. |
Low
Very low
Very Low
Very low
Low |
Conditionnel recommandation
Conditionnel recommandation
Conditionnel recommandation
Conditionnel
Conditionnel Recommandation |
Systematic review
Expert opinion
Expert opinion
Expert opinion
Expert opinion |
12,32,33
12,33
12,32,33
12,32,33
12,32,33
|
- Research needs
▪️ Conduct more and larger studies to correlate the clinical findings with various diagnostic criteria of acute bacterial rhinosinusitis
▪️ Develop imaging technology that differentiate bacterial from viral infections.
▪️ There is a need to conduct RCTs to determine the efficacy of wait and see policy.
▪️ There is a need to conduct randomized controlled trials (RCTs) to determine the efficacy and choice of antibiotics.
▪️ Determine the optimal antimicrobial therapy
▪️ Determine the causes, diagnosis and treatment of recurrent acute rhinosinusitis
▪️ Determine the bacterial resistance
▪️ Determine the role of adjuvant therapies
- Monitoring and evaluating the impact of the guideline
Clinicians should be able to:
▪️ Differentiate viral from bacterial ARS:
▪️ Timing to choose wait and see policy
▪️ Timing for Prescriptions of the proper antibiotic treatment
▪️ Managing patients with recurrent ARS
▪️ Know red Flags that need urgent referral for Assessment/ Management must be taken into consideration.
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. Orlandi RR, Kingdom TT, Smith TL, et al. international consensus statement on allergy and rhinology: rhinosinusitis 2021. Int Forum Allergy Rhinol. 2021;11(3):213-739. doi: 10.1002/alr.22741. PMID: 33236525.
2. Ragab A, Kamel R. Personal communication.
3. Schünemann H, Brożek J, Guyatt G et al. GRADE handbook 2013. https:// gdt.gradepro.org/app/ handbook/handbook.html.
4. Zhou,Yu Ting,Du Ronghui et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062.
5. Acute rhinosinusitis in adults. University of Michigan Health System (UMHS) December 2018. Available at http://www.med.umich.edu/1info/ FHP/practiceguides/Rhino/rhino.pdf. accessed 13/12/2019.
6. Chow AW, Benninger MS, Brook I, et al. Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8): e72–e112.
7. Sinusitis (acute). Antimicrobial prescribing NICE guideline Published: 27 October 2017. www.nice.org. uk/guidance/ng79 accessed 18/9/2019.
8. Desrosiers M, Evans GA, Keith PK, et al. Canadian clinical practice guidelines for acute and chronic rhinosinusitis. J Otolaryngol Head Neck Surg 2011;40(Suppl 2):S99-193.
9. Scadding GK, Durham SR, Mirakian R, et al. British Society for Allergy and Clinical Immunology. BSACI guidelines for the management of rhinosinusitis and nasal polyposis. Clin Exp allergy. 2008;38(2):260- 275.
10. Wald E. American Academy of Pediatrics. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262-e280.
11. Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50(1):1-12. doi: 10.4193/ Rhino50E2.
12. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS et al. Clinical practice guideline (update): Adult sinusitis. Otolaryngology- Head and Neck Surgery, 2015, 152:SI-S39. (Commissioned by the American Academy of Otolaryngology – Head and Neck Surgery Foundation).
13. Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012 Apr;54(8):e72- e112. doi: 10.1093/cid/cir1043. Epub 2012 Mar 20.
14. Meltzer EO, Hamilos DL, Hadley JA, et al. Rhinosinusitis: Establishing definitions for clinical research and patient care. Otolaryngol Head Neck Surg. 2004;131(6):S1-S62.
15. Setzen G, Ferguson BJ, Han JK, et al. Clinical consensus statement: appropriate use of computed tomography for paranasal sinus disease. Otolaryngol Head Neck Surg. 2012;147:808-816.
16. Ebell MH, McKay B, Guilbault R, Ermias Y. Diagnosis of acute rhinosinusitis in primary care: a systematic review of test accuracy. Br J Gen Pract. 2016 Sep;66(650):e612-32. doi: 10.3399/bjgp16X686581. Epub 2016 Aug 1. PMID: 27481857; PMCID: PMC5198696.
17. van den Broek MF, Gudden C, Kluijfhout WP, Stam-Slob MC, Aarts MC, Kaper NM, van der Heijden GJ. No evidence for distinguishing bacterial from viral acute rhinosinusitis using symptom duration and purulent rhinorrhea: a systematic review of the evidence base. Otolaryngol Head Neck Surg. 2014 Apr;150(4):533-7.
18. Papadopoulou AM, Bakogiannis N, Skrapari I, Bakoyiannis C. Anatomical Variations of the Sinonasal Area and Their Clinical Impact on Sinus Pathology: A Systematic Review. Int Arch Otorhinolaryngol. 2022 Jan 28;26(3):e491-e498. doi: 10.1055/s-0042-1742327.
19. Li S, Zhao CJ, Hua HL, Deng YQ, Tao ZZ. The association between allergy and sinusitis: a cross-sectional study based on NHANES 2005-2006. Allergy Asthma Clin Immunol. 2021 Dec 25;17(1):135.
20. Kumar N, Brar T, Kita H, Marks LA, Miglani A, Marino MJ, Lal D. Viruses in chronic rhinosinusitis: a systematic review. Front Allergy. 2023 Dec 5;4:1237068.
21. Lin, J., Wang, C., Wang, X. et al. Expert consensus on odontogenic maxillary sinusitis multi-disciplinary treatment. Int J Oral Sci 16, 11 (2024).
22. Lemiengre MB, van Driel ML, Merenstein D, Liira H, Mäkelä M, De Sutter AI. Antibiotics for acute rhinosinusitis in adults. Cochrane Database Syst Rev. 2018 Sep 10;9(9):CD006089. doi: 10.1002/14651858.CD006089.pub5. PMID: 30198548; PMCID: PMC6513448.
23. Burgstaller JM, Steurer J, Holzmann D, Geiges G, Soyka MB. Antibiotic efficacy in patients with a moderate probability of acute rhinosinusitis: a systematic review. Eur Arch Otorhinolaryngol. 2016 May;273(5):1067-77. doi: 10.1007/s00405-015-3506-z. Epub 2015 Jan 18. PMID: 25597034.
24. Zalmanovici Trestioreanu A, Yaphe J. Intranasal steroids for acute sinusitis. Cochrane Database Syst Rev. 2013 Dec 2;2013(12):CD005149. doi: 10.1002/14651858.CD005149.pub4. PMID: 24293353; PMCID: PMC6698484.
25.Venekamp RP, Thompson MJ, Hayward G, Heneghan CJ, Del Mar CB, Perera R, Glasziou PP, Rovers MM. Systemic corticosteroids for acute sinusitis. Cochrane Database Syst Rev. 2011 Dec 7;(12):CD008115.
26. Gehanno P, Beauvillain C, Bobin S, Chobaut JC, Desaulty A, Dubreuil C, et al. Short therapy with amoxicillin-clavulanate and corticosteroids in acute sinusitis: results of a multicentre study in adults. Scand J Infect Dis. 2000;32(6):679–684.
27. King D, Mitchell B, Williams CP, Spurling GK. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015 Apr 20;2015(4):CD006821.
28. Shaikh N, Wald ER. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2014 Oct 27;2014(10):CD007909.
29. Incorvaia C, Leo G. Treatment of rhinosinusitis: other medical options. Int J Immunopathol Pharmacol. 2010 Jan-Mar;23(1 Suppl):70-3.
30. Hallak B, Bouayed S, Ghika JA, Teiga PS, Alvarez V. Management Strategy of Intracranial Complications of Sinusitis: Our Experience and Review of the Literature. Allergy Rhinol (Providence). 2022 Sep 25;13:21526575221125031.
31. Hayward G, Heneghan C, Perera R, Thompson M. Intranasal corticosteroids in management of acute sinusitis: a systematic review and meta-analysis. Ann Fam Med. 2012 May-Jun;10(3):241-9.
32. Saltagi MZ, Comer BT, Hughes S, Ting JY, Higgins TS. Management of Recurrent Acute Rhinosinusitis: A Systematic Review. Am J Rhinol Allergy. 2021 Nov;35(6):902-909.
33. Saltagi MZ, Comer BT, Hughes S, Ting JY, Higgins TS. Diagnostic Criteria of Recurrent Acute Rhinosinusitis: A Systematic Review. Am J Rhinol Allergy. 2021 May;35(3):383-390.
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
Annex 1: Guideline Flowchart
Annex 2: Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
|
No |
Guideline Name |
Year of publication |
The Organization |
Age demography |
|
1. |
University of Michigan Health System guidelines on treatment for acute sinusitis UMHS |
2018 |
University of Michigan Health System(UMHS) |
Adult |
|
2. |
IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. IDSA-CPGABRS |
2012 |
Infectious Diseases Society of America |
Adult and children |
|
3. |
NICE |
2017 |
National Health System NHS England |
Adult and children |
|
4. |
Canadian guidelines for acute bacterial rhinosinusitis Canadian medical societies CMC |
2014 |
Canadian medical societies (Association of Medical Microbiology and Infectious Disease Canada, Canadian Society of Allergy and Clinical Immunology, Canadian Society of Otolaryngology—Head and Neck Surgery, Canadian Association of Emergency Physicians, and the Family Physicians Airways Group of Canada) |
Adult |
|
5. |
Standards of Care Committee of the BSACI BSACI |
2007 |
British Society for Allergy and Clinical Immunology. Standards of Care Committee of the BSACI |
Adult |
|
6. |
American Academy of Pediatrics clinical practice guideline EAACI |
2013 |
American Academy of Pediatrics |
Children |
|
7. |
EPOS |
Published 2012 Updated 2020 |
Task force commissioned by the EAACI |
Adult and children |
|
8. |
American Academy of Otolaryngology – Head and Neck Surgery AAO-HNSF |
Published 2007 Updated 2015 |
American Academy of Otolaryngology – Head and Neck Surgery Foundation |
Adult |
|
9. |
AAAAI/ACAAI practice parameter of ARS |
2014 |
American Academy of Allergy, Asthma & Immunology (AAAAI)/The American College of Allergy, Asthma & Immunology (ACAAI) |
Adult |
Table 1
|
Criteria |
Guideline A UMHS |
Guideline B NICE |
Guideline C EPOS |
Guideline D AAO-HNSF |
|
Credibility |
9 |
9 |
9 |
9 |
|
Observability |
8 |
7 |
8 |
8 |
|
Relevance |
7 |
7 |
7 |
8 |
|
Relative advantage |
7 |
7 |
7 |
8 |
|
Easy to install and understand |
7 |
7 |
7 |
9 |
|
Compatibility |
7 |
7 |
7 |
8 |
|
Testability |
7 |
7 |
7 |
8 |
|
Total score |
52 |
51 |
52 |
58 |
Table 2
|
Domain |
Guideline A UMHS |
Guideline B NICE |
Guideline C EPOS |
Guideline D AAO-HNSF |
|
B |
A |
B |
A |
|
2. Conflict of interest |
B |
NR |
NR |
A |
|
3. Development group |
B |
B |
B |
B |
|
4. Systematic review |
A |
A |
A |
A |
|
5. Grading of evidence |
A |
NR |
A |
A |
|
6. Recommendations |
B |
C |
B |
A |
|
7. External review |
B |
A |
A |
A |
|
8. Updating |
A |
A |
A |
A |
Table 3
Annex 3: The risks and benefits of added and/or modified statements
|
The statement to be adapted: Action |
Benefits |
Risk/Harm |
|
|
Symptoms must include: 1–Mucopurulent nasal drainage/discharge (anterior/ posterior) and 2–Nasal blockage/obstruction/congestion or facial pain/ pressure or both Symptoms may include smell affection and headache in adults and cough in children. All can be included in CPODS C: Congestion P: Pain O: Obstruction D: Drainage/Discharge S: Smell affection. |
Easy to remember letters |
No |
|
|
A thorough physical examination that includes inspection, palpation of the maxillary and frontal sinus, as well as anterior rhinoscopy (evidence of inflammation, mucosal oedema, and discharge). |
-Allow physician to assess the patient without radiological diagnostics. -Little skills and Equipment's are needed |
More time needed for settlement of appointments |
|
|
ESR and CRP are inflammatory markers found to be elevated during ARS, but they are not routinely used for diagnosis because of their limited specificity. They may have some role in COVID-19 related symptoms in Chinese guidelines for COVID-19: CRP test together with other clinical parameters for initial evaluation and follow-up of coronavirus infection. Cut-off for CRP: 40–50 mg/L (4). |
Easy and rapid laboratory investigation that have some values to diagnose covid patients |
Low evidence and it can be elevated with other causes |
|
|
Consider initial watchful waiting in uncomplicated cases, with institution of antibiotic therapy if no improvement after 4-7 days or worsening at any time, or for mitigating circumstances with drug resistance e.g., including severe symptoms, immunocompromised state, concern for impending complications, suspected odontogenic source, prior antibiotics (1 month), prior hospitalization (5 days) and comorbidities. Watchful waiting should be offered only when there is assurance of follow-up, such that antibiotic therapy is started if the patient’s condition fails |
Decrease the use of antibiotics with limited duration of waiting policy and criteria of assurance of follow up |
The patient need to improve rapidly and the high burden over doctors |
|
|
An alternative management strategy is recommended if symptoms worsen after 48–72 hours of initial empiric antimicrobial therapy or fail to improve despite 3–5 days of initial empiric antimicrobial therapy If symptoms persist or worsen despite 72 hours of treatment with a second-line regimen, Additional investigations (such as sinus puncture or acquisition of cultures of the middle meatus, and CT or MRI studies) should be initiated. |
Provide a systematic and algorithm-based approach to antimicrobial therapy of patients failing initial therapy. |
The potential for adding more selection pressure for resistance due to ‘‘antimicrobial surfing’’ and adding adverse effects without antimicrobial benefit. |
|
|
INCS can be used according to the doctor judgment as monotherapy in mild to moderate ARS or as adjuvant to antibiotic therapy in severe cases of ARS.
|
Doctors' judgment can allow building the balance between benefits and harms |
Cost and local side effects |
|
|
-First time non-responders can be based on lack of clinical improvement following treatment within 5 days in adults and 3 days in children. -B-lactamase producing penicillin resistance H.Influenzae in > 30 % and S.pneumoniae. -Use second line antimicrobial agents. -Second time non responders who fail to improve with second line antibiotic therapy should be evaluated for other diagnosis or considered for sinus aspiration or endoscopically guided middle meatus culture and sensitivity. |
Decrease the time that the patient to be left without follow up and improvement |
Increase the risk of bacterial resistance |
|
|
At least 4 attacks of ABRS/year are a required criterion -Nasal endoscopy and/or CT imaging are an option during at least one episode of suspected RARS to appropriately confirm and diagnose RARS, and distinguish it from other diagnoses such as allergy exacerbation or primary headache syndromes. -Consider immunologic testing, allergic testing, and bacterial culture in patients with concern for RARS -Option for use of INCS spray for sinonasal symptoms during acute exacerbations of RARS. -Follow other ABRS management options -Endoscopic sinus surgery (ESS) is recommended for patients with RARS. |
Baloon sinusoplasty was excluded as there are limited evidence for improvement |
High cost with limited benefit |
|


















