Phoniatrics Late Language Emergence / Language Delay Language Disorders / Autism Spectrum Disorder
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Phoniatrics Late Language Emergence / Language Delay Language Disorders / Autism Spectrum Disorder |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:08 PM |
Description
"last update: 10 June 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mahmoud Abdel Aziz,5 Mohamed Ghonaim,6 Tarek Ghanoum,7 Mahmoud Youssef8
Phoniatrics Manager: Mahmoud Youssef8
Phoniatrics Executive Manager: Dalia Mostafa9
Assembly Board: Dalia Mostafa Osman,9 Yossra Abdel Naby Sallam,10 Rehab Abd ElHafeez Zaytoun,11 Ahmed Ali AbdelMonem12
Grading Board (In alphabetical order)
Ahlam A. N. El-Adawy,17 Ahmed Ali,12 Aisha Fawzy,9 Asmaa El Dessouky,18 Aya Sheikhany,9 Azza Abdel Aziz,13 Dalia Mostafa,9
Essam Aref,16 Hemmat El Baz,15 Iman El Roubi,13 Mahmoud Youssef,8 Nervana Hafez,8 Omayma Afsah,15 Rasha Safwat,9 Rehab
Zaytun,11 Safaa El Sady,8 Salwa Ahmed,14 Yossra Abdel Naby Sallam10
Reviewing Board: Hossam El Dessouky,9 Sahar Shohdi,9 Azza Adel Aziz9, Eatemad Nabil Abdelhalim19 , Reham Mohamed Kamel20 , Aisha Ghanem Abd El Lateef21, Mona Sayed Hassan22
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/Menoufia University, 3Otorhinolaryngology Department, Faculty of Medicine/ Minia University, 4Otorhinolaryngology Department, Faculty of Medicine/Beni-Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 6Otorhinolaryngology Department, Faculty of Medicine/Mansoura University, 7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 10Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Al-Azhar University, 11Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Fayoum University, 12Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University, 13Phoniatrics Unit, Otorhinolaryngology Department/Hearing and Speech Institute, 14Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Banha University, 15Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 16Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 17Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Sohag University, 18Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 19Pediatrics Department, Faculty of Medicine for Girls, Al Azhar University, 20Psychiatry Department, Faculty of Medicine, Cairo University. 21Psychiatry Department, Faculty of Medicine for Girls, Al Azhar University, 20Psychiatry Department, Faculty of Medicine, Beni-Suef University.
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah.
- Abbreviations
AAC Augmentative & Alternative Communication
ADHD Attention Deficit Hyperactivity Disorder
ASD Autism Spectrum Disorder
CAPD Central Auditory Processing Disorder
GRADE Grading of Recommendations Assessment, Development and Evaluation
IQ Intelligent Quotient
Lang Language delay / late language emergence
RCSLT Royal College of Speech & Language Therapy
SCD Social Communication Disorder
TEACCH Treatment and Education of Autistic and Related Communication Handicapped Children
- Executive Summary
The scope of the guideline is the diagnosis, assessment and intervention of communication difficulties in children with late language emergence or autism spectrum disorder.
Late Language Emergence
▪️ When a child is first referred for a delay in his/her language development, a detailed thorough history taking should be carried out in order to learn more about the child’s perinatal, developmental, medical, behavioral, social and educational history and to double check the possible existence of any comorbid disorders and/or associated syndromes (Strong recommendation).
▪️ Based on the information gathered during the initial parent interview, necessary referrals are recommended such as audiological assessment (mandatory), neurological examination, physical therapy examination (based on concerns raised by caregivers or deduced during professional observation), special tests related to Autism spectrum disorder (if related features have been reported during the initial parent interview or clinically observed), occupational therapy (if motor programming and/or sensory issues are suspected), etc. (Strong recommendation)
▪️ Following the initial interview, the evaluation process takes place. (Strong recommendation).
▪️ Assessment can be preceded by a screening process (Conditional recommendation).
▪️ A thorough assessment is recommended in order to closely inspect the child’s language skills and establish a proper baseline for future realistic as well as effective therapeutic plans (Strong recommendation).
▪️ Differential diagnosis along with interpretation of all findings and sharing results within the family need to follow the assessment (Strong recommendation).
▪️ Following the evaluation phase, the child is referred for intervention. Intervention can be in the form of indirect intervention; carried out through a series of systematic parent counseling sessions that involves close observation to the child’s skills. This is usually recommended for very young children. For older children, direct intervention takes place (Strong recommendation).
▪️ Direction intervention procedures and strategies can vary depending on the child’s needs, developmental level, family circumstances and other factors. It can be in the form of regular individual therapeutic sessions, group therapy, tasks during naturalistic settings, or a hybrid approach involving a mixture of various direct and indirect approaches all together (Strong recommendation).
▪️ Family involvement is very important in every step as it can help foster, maintain and generalize language skills acquired during formal therapeutic settings and facilitate their generalization to daily life activities and interactions (Strong recommendation).
▪️ Multidisciplinary team involvement is important whenever needed (Strong recommendation).
▪️ In severe case, augmented communication needs to be considered along with working on enhancing spoken language skills (Strong recommendation).
▪️ Equally important to family involvement, is regular data collection for the child’s response to therapy and his/her benefit from selected objectives (Strong recommendation).
Autism Spectrum Disorder (ASD)
▪️ Dealing with a child suspected to be on the Autism Spectrum Disorder (ASD) follows the same management steps mentioned above but with particular focus on collecting additional data and carrying out further testing in order to confirm or exclude the existence of the warning signs of this disorder in addition to particular stress on the child’s social communication skills (Strong recommendatio
▪️ Following initial interview, the child’s eye gaze, joint attention, social interactions, imitation skills, non-verbal means of communication, language skills, facial expressions, repetitive movements, etc. are thoroughly screened and closely observed (Strong recommendation).
▪️ Screening can be followed by a formal testing for cooperative children in order to reach a better understanding of the child’s needs and difficulties (Conditional recommendation).
▪️ The assessment process should also include input from other professionals involved in the inter/multi-disciplinary team dealing with the child (Conditional recommendation).
▪️ If a diagnosis of ASD is proven, relevant therapeutic procedures should immediately follow (Strong recommendation).
▪️ Based on the assessment findings, therapy is provided (Strong recommendation).
▪️ In ASD children, management usually occurs within the frame of a multidisciplinary approach; with all professionals involved collaborating together in order to confirm / exclude the preliminary diagnosis given, plan future therapy, provide support to parents and work towards achieving future targeted goals (Conditional recommendation).
▪️ It is essential that all the professionals involved in the multidisciplinary team possess knowledge of typical and atypical patterns of development in the domains of cognition; communication; emergent literacy; and motor, sensory, and social-emotional and work collaboratively together (Strong recommendation)
▪️ Intervention can vary based on the severity of the disorder and associated problems. Treatment can include activity schedules, visual support aids, or even augmentative and alternative communication (to be used in an augmentative rather than alternative method; i.e., always linked to a verbal message) (Strong recommendation).
▪️ Among the intervention procedures in such cases are also different behavioral intervention techniques and cognitive behavioral therapy (Conditional recommendation).
▪️ Therapy can also include spoken language intervention, parent-mediated intervention, applied behavior analysis, and social-communication intervention (Strong recommendation).
▪️ Socio-pragmatic skills are crucial to address during every stage in the intervention process. Pragmatic skills are usually an area of particular need for patients having Autism Spectrum Disorder (Strong recommendation).
▪️ Transitioning with youth and adults is also very important to consider when children get older in order to help them face high social demands, overcome communication challenges, and better cope with colleagues and peers in all educational as well as vocational and social settings (Conditional recommendation).
Monitoring progress achieved in every stage, not only in structured therapeutic sessions but also during various daily life activities and interactions, can help in consistently updating the child’s therapeutic plan; based on achieved progress and in the highlight of his capabilities; thereby helping him reach the best utmost level; each within his own learning potential (Strong recommendation).- Introduction, scope and audience
➡️Introduction
Late language is diagnosed when language development skills are below age expectations (1). On the other hand, Autism spectrum disorder is a neurodevelopmental disorder characterized by social communication deficits, along with restricted, repetitive behaviors (2). Children, with such difficulties, are expected to be at risk for developing literacy, social and academic difficulties if left untreated. Thus, it is crucial to properly evaluate and intervene such children; each according to his/her areas of need and strength, using proper evaluation & therapeutic techniques.
➡️Scope
The scope of the guideline is the diagnosis and management of language and communication problems in male and female children having language delay and / or disorders including those having Autism Spectrum Disorders.
➡️Target audience
Phoniatricians, Pediatricians and family physicians, to be used for management and/or appropriate referral of children with language delay and/or disorders.
- Methods of development
➡️Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Phoniatrics Chief Manager, Phoniatrics Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
➡️Search Method
Electronic database searched:
Pubmed, Google, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar
➡️Keywords
Late language emergence, autism spectrum disorder, delayed language development, autism, late talkers, language delay, language disorders.
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Time period searched: from 2005 to 2020.
➡️Results
Four national phoniatricians reviewed the guidelines available. The American Speech-Language-Hearing Association (ASHA) Practice Portal (3) had the highest scores as regards to the currency, content and quality. Some of the statements were also obtained from the Royal College of Speech & Language Therapists Clinical Guidelines (RCSLT) (4)
It was graded GRADE by eighteen experts and reviewed by seven expert reviewers to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
Most of the statements were taken from The American Speech-Language-Hearing Association (ASHA) Practice Portal. Some were based on ASHA evidence maps and others were taken from the Royal College of Speech and Language Therapists Guidelines.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention (5)
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. |
- Recommendations
The following statements and flowchart were adapted from the American Speech-Language-Hearing Association Practice Portal which received the highest scores as regards the currency, contents, and quality.
Recommendations statements
Guidelines for Late Language Emergence
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of recommendation |
Study Type |
References |
|
Case history
|
1-Relevant case history, includes family’s concerns about the child’s speech and language; birth, medical, and developmental history; history of middle ear infections; family history of late language emergence or other language difficulties; language history and proficiency for children who are dual-language learners. |
6, high
7, high |
Strong recommendation |
6, systematic review and meta-analysis
7, systematic review and meta-analysis
|
6, 7 |
|
Referrals based on case history report
|
2-If motor/ neurological problems are re- ported by parents or observed during the initial interview or screening, a referral for neurological examination will be needed. |
High |
Strong recommendation |
Systematic review & meta-analysis
|
8 |
|
3-If syndrome features are suspected, a referral for genetic testing should be considered and discussed with parents. |
High |
Strong recommendation |
Meta-analysis
|
9 |
|
|
4-Psychometric and neurodevelopment assessments must be considered*. |
High |
Strong recommendation |
Systematic review & meta-analysis
|
8 |
|
|
5-If feeding and/or swallowing problem is suspected (including drooling, choking attacks, feeding difficulties, repeated attacks of chest infections), etc.; a referral for necessary instrumental assessment techniques and relevant therapeutic methods must be considered. |
High
|
Strong recommendation |
Systematic review |
10 |
|
|
6-Audiological assessment is crucial in the assessment process of any child presenting with language delay and/or disorder (including Autism Spectrum Disorder) in order to rule out the existence of any hearing impairment*. |
11, high 12, high |
Strong recommendation |
11-Systematic review
12- Systematic review & meta-analysis
|
11, 12 |
|
|
7-Electroencephalography can be recommended in certain cases particularly for children with history of absence ( pyknolepsy) and/or convulsions. |
High |
Strong recommendation |
Systematic review |
13 |
|
|
8-Brain imaging can be considered in children with history of serious head trauma; followed by loss of consciousness and/or vomiting. |
Moderate |
Strong recommendation |
Systematic review with limitations |
14 |
N.B.
*Psychiatric consultation can be considered in children with severe Attention Deficit Hyperactivity Disorders / Autism Spectrum disorders.
**Audiological assessments can include central auditory testing in school-aged children; referred for language difficulties & language-based
learning disabilities.
|
Clinical questions |
Action Recommendations |
Evidence quality |
Strength of recommendation |
Study Type |
References |
|
Medical/ health referrals whenever indicated
|
9- A child with a severe speech/language delay should receive a comprehensive health assessment to identify or rule out medical conditions that might be related to the delay. |
Moderate |
Conditional recommendation |
Cross sectional controlled study |
15 |
|
Screening
|
10-It is important that the phoniatrician uses screening and assessment tools that provide the most representative sample of the child’s behaviors across a range of people and activities within the child’s natural environments. |
Moderate |
Conditional recommendation |
Literature review |
16 |
|
Pre- assessment Planning
|
11-Pre-assessment planning involves one or more professionals who meet with the child and family to gather information and plan the upcoming assessment. Common goals for planning include identifying what the family needs and wants from the assessment process, the roles that family members (and caregivers) would prefer to take in the assessment, and the child’s areas of strength and need. |
Moderate |
Conditional recommendation |
Literature review |
17, 18
|
|
Assessment Measures
|
12-Assessment is accomplished using a variety of measures and activities, including both standardized and non-standardized measures, as well as formal and informal assessment tools. Phoniatricians have the obligation to ensure that standardized measures used in assessment show robust psychometric properties that provide strong evidence of their quality. |
Moderate
|
Conditional recommendation |
Literature review |
19 |
|
Assessment components
|
13-For each individual, assessment must take into account the body functions and structures, activity (e.g., communication skills), participation (e.g., functional use of language) and contextual factors (environ- mental and personal factors). |
Low |
Strong recommendation |
Qualitative study |
20 |
|
Oral mechanism examination & speech sounds assessment
|
1-Assessment includes oral mechanism ex- amination (structure, power function and programming) and speech sound assessment |
Moderate |
Strong recommendation |
Single comparative controlled study
|
21 |
|
Clinical questions |
Action Recommendations |
Evidence quality |
Strength of recommendation |
Study Type |
References |
|
Differential Diagnosis |
15-Following initial assessment, a differential diagnosis should be formed, taking into account all the available information in order to exclude the existence of any associated hearing impairment, autism spectrum disorder or social communication disorder, dyspraxia (verbal, oral ± motor), co-morbid attention deficit hyperactivity disorder, cognitive delay, global developmental delay or central auditory processing difficulties and learning disabilities. |
Very low
|
Strong recommendation |
Professional consensus
|
4 |
|
Interpretation of results
|
16-Screening and assessment results are interpreted within the context of a child’s overall development and in collaboration with family members and with other professionals as appropriate. |
Very low
|
Strong recommendation |
Clinical expertise |
3 |
|
Sharing results |
17-A clear explanation of the behavior/disorder will be offered to the individual and their family, with written information to reinforce this. |
Low |
Strong recommendation |
Non-experimental study
|
22
|
|
Special considerations in bilingualism |
18- For bilingual children, appropriate assessment in all languages is necessary to differentiate between a linguistic difference and a true communication disorder. |
Low
|
Strong recommendation |
Non-controlled study |
23 |
|
Clinical questions |
Action Recommendations |
Evidence quality |
Strength of recommendation |
Study Type |
References |
|
Special considerations in bilingualism |
19- In most bilingual cases, the use of standardized tests alone is not sufficient and cannot be used to decisively determine the presence or absence of a communication disorder. |
Moderate |
Conditional recommendation |
Meta analysis with limitations
|
24 |
|
Identification of severe speech/ language delay |
20- A severe speech/language delay can be indicated by no words at 18 months; fewer than 30 words at 24 months; or no word combinations at 36 months. However, it should be noted that at 18 months, the condition mentioned above can be considered as language delay but not necessarily severe as some children catch up, to some extent with their peers, provided that they are given the family is given the appropriate counselling Will be changed into modified |
Moderate
|
Conditional recommendation |
Clinical Practice Guidelines, Report of recommendations
|
25 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Identification of Specific Language Impairment
|
21- Children who continue to have poor language abilities below chronological age expectations (by late preschool or school age) that cannot be explained by other factors (e.g., low nonverbal intelligence, sensory impairments, or autism spectrum disorder) may be identified at that point as having Specific Language Impairment. |
26, high
27, moderate |
Conditional recommendation |
26, controlled study
27, review with limitations
|
26, 27 |
|
Hypothesis formation
|
22-Management will be planned, based on the results of information gathering/assessment and consequent hypothesis formation and understanding of the theoretical frameworks relevant to the behavior/disorder and knowledge of the different approaches to intervention/ management. |
Very low
|
Strong recommendation |
Professional consensus
|
4 |
|
Management Planning & Goal Setting
|
23-A management plan, with provisional timescales, will be drawn up in consultation with the individual. It will be shared with their caregiver and other professionals and will de- tail the aims, objectives and expectations of identified relating to the individual’s activity, participation and well-being. |
Moderate |
Strong recommendation |
Literature review
|
|
|
Initiation of therapy
|
24-For children between 18 and 36 months with a speech/language delay and no other apparent developmental issues, speech-language treatment should be initiated; whether direct / indirect methods. |
High
|
Strong recommendation |
Systematic review |
29 |
|
Indirect intervention
|
25-When no other developmental delays or disabilities have been identified or are suspected, the typical course for a late talker, less than 2 years, is regular monitoring or monitoring combined with indirect language stimulation. |
Moderate
|
Strong recommendation |
Review with limitations
|
30 |
|
Intervention for young children
|
26- Because young children (less than 2 years) learn through familiar, natural activities, it is important for the phoniatrician to provide information that promotes the parents’ and/or other caregivers’ abilities to implement communication-enhancing strategies during those everyday routines, creating increased learning opportunities and participation for the child. |
Very low
|
Strong recommendation |
Guidelines committee |
31 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Direct intervention
|
27- When language delays persist over time, or are present with other identified or suspected delays or disabilities (e.g., intellectual disabilities, autism spectrum disorder, hearing impairment), direct speech and language services are indicated; the phoniatrician coordinates services with other professionals working with the child. Family participation is very important. |
Moderate
|
Strong recommendation |
Literature review |
32 |
|
Intervention to promote various inefficient language skills
|
28-Speech and language intervention can include working on phonology, semantics, morphology and syntax, pragmatics (including narration), and literacy (+ other intervention methods used in written language disorders/learning disabilities*) |
33, Moderate 34, moderate 35, low |
Strong recommendation |
33, controlled study 34, single subject design 35, expert opinion |
33, 34,35
|
* Please refer to learning disabilities adapted guideline and its recommendations.
|
Clinical questions |
Action Recommendations |
Level of Evidence |
Strength of Recommendation |
Study Type |
References |
|
Management of phonology & articulation problems
|
29-Within an appropriate context & when- ever indicated, consideration needs to be given to the development of the child’s: · Phonological system · Phonological processes · Intelligibility · Phonetic system · Phonetic errors · Self-monitoring · Pre-literacy skills · Literacy skills · Prosody & resonance |
Very low
|
Strong recommendation |
Professional consensus
|
4
|
|
Management of Processing problems
|
30-The phoniatrician should consider the child’s ability to process speech as a critical skill for speech and language development. |
Moderate
|
Conditional recommendation |
Controlled study |
36 |
|
Multidisciplinary team
|
31-The multidisciplinary team may include an audiologist, early childhood general and special education teachers and interpreter (if needed), neurodevelopmental pediatrician, occupational therapist, physical therapist and school psychologist, phoniatrician, qualified speech & language therapist ± childcare providers, educational diagnosticians, educational therapists, reading specialists, social workers, child and developmental psychologists, pediatric neurologists, and child psychiatrists. |
Moderate |
Strong recommendation |
Review with limitations |
37
|
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Multidisci- plinary team
|
32-It is essential that all the professionals involved in the multidisciplinary team have the capacity to collaborate effectively and collectively. |
38, moderate
39, moderate |
Strong recommendation |
38, literature review 39, literature review |
|
|
Multidisci- plinary team
|
33-It is essential that all the professionals involved in the multidisciplinary team possess knowledge of typical and atypical patterns of development in the domains of cognition; communication; emergent literacy; and motor, sensory, and social-emotional functioning. |
Very low
|
Strong recommendation |
Expert opinion & reasoning from first principles
|
40 |
|
Augmentative & Alternative Communication
|
34-Augmentative or alternative communication methods may be considered as a temporary means of communication for late talkers, particularly in severe cases. Research shows that use of AAC may aid in the development of natural speech and language |
41, high
42, low
43, low
|
Strong recommendation
|
41, randomized controlled trial 42, case report 43, clinical trial
|
41, 42, 43 |
|
Augmented input
|
35-Augmented input is based on the concept that language input provides a model for language development. This approach can lead to increased symbol comprehension in young AAC* users and in users with severe cognitive or intellectual disabilities, as well as increased symbol comprehension and production. Augmented input—also called “natural aided language” or “aided language modeling”—is a receptive language training approach in which the communication partner provides spoken words along with AAC* symbols during communication tasks (e.g., partner points to the AAC* symbols while simultaneously talking). |
44, high 45, high 46, moderate 47, moderate |
Strong recommendation |
44, multiple-baseline design 45, multiple-probe design 46, literature review 47, literature review
|
44,45,46,47 |
* AAC=Augmentative & Alternative Communication.
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Reflective Practice |
36-Management aims and objectives must be reviewed regularly and frequently. If anticipated progress is not achieved the therapeutic intervention should be re viewed. |
Very low
|
Strong recommendation |
Professional consensus
|
4 |
|
Evaluation of outcome |
37-Outcomes of therapy should be routinely measured, reflecting the range of interventions delivered and the aims agreed for therapy (every 3-6 months; provided that the child regularly & consistently attends his/her previously scheduled sessions). |
Very low
|
Strong recommendation |
Professional consensus
|
4 |
B-Guidelines for Autism Spectrum Disorders
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Referral
|
1-If the child exhibits warning signs of autism spectrum disorder, the child, regardless of age, should receive a referral for “a communication and language assessment by a phoniatrician possibly specifying with rehabilitation if necessary”. |
Moderate
|
Strong recommendation |
literature review
|
48 |
|
Diagnostic Statistical Manual-V (DSM-5)
|
2-According to the DSM-5, individuals who meet the specified criteria are given the diagnosis of Autism Spectrum Disorder (ASD) with one of three levels of severity. N.B. DSM-5 reflects a number of changes from those in the DSM-IV. |
49, high 50, moderate 2, review & clinical expertise |
Strong recommendation |
49, meta-analysis
50, comparative study
|
49, 50, 2 |
|
Diagnosis
|
3-Current findings suggest that ADOS [Autism Diagnostic Observation Scale] is best for not missing children who have ASD and is similar to CARS [Childhood Autism Rating Scale] and ADI-R[Autism Diagnostic Interview - Revised] in not falsely diagnosing ASD in a child who does not have ASD. ADOS has acceptable accuracy in populations with a high prevalence of ASD. However, overdiagnosis is likely if the tool is used in populations with a low- er prevalence of ASD. This finding supports current recommended practice for ASD diagnostic tools to be used as part of a multi-disciplinary assessment, rather than as stand- alone diagnostic instruments. |
High
|
Strong recommendation |
Systematic review |
51 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Comprehensive assessment
|
9-Depending on the individual’s age and abilities, the phoniatrician typically assesses: · Receptive language · Expressive language · Literacy skills · Social communication · Conversational skills · Speech prosody |
65, high
66, low
|
Conditional recommendation |
65, systematic review
66, study but with no control
|
65, 66 |
|
Comprehensive assessment
|
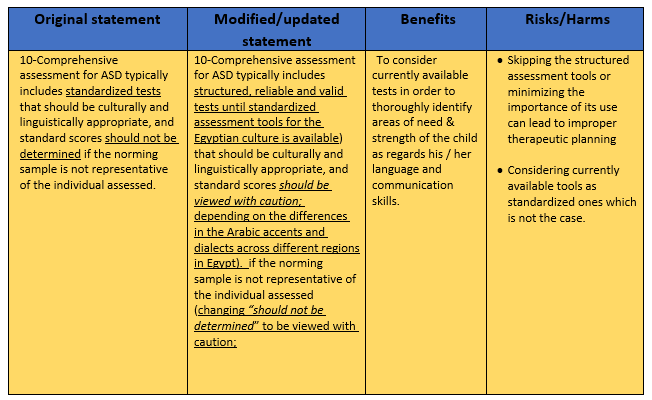
10-Comprehensive assessment for ASD* typically includes structured, reliable and valid tests (until standardized assessment tools for the Egyptian culture is available) that should be culturally and linguistically appropriate, and if the norming sample is not representative of the individual assessed, the standard scores should be viewed with caution; depending on the differences in the Arabic accents and dialects across different regions in Egypt). |
High |
Strong recommendation |
Systematic review |
67 |
|
Checklists
|
11-When possible, parent checklists should be provided in their native language to obtain the most accurate information. |
Very low |
Strong recommendation |
Expert opinion |
68 |
|
Clinical questions
|
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Naturalistic observation
|
12-Observation of the individual in everyday social settings with others. Criterion-referenced assessments may be used during naturalistic observations to document an individual’s functional use of language across social situations. |
Very low |
Strong recommendation |
Expert opinion |
68 |
|
Dynamic assessment
|
13-Dynamic Assessment seeks to identify an individual’s skills as well as his or her learning potential. Dynamic assessment is highly interactive and emphasizes the learning process over time. It can be used in conjunction with standardized assessments. |
69, high
70, high |
Conditional recommendation |
69, systematic review
70, systematic review |
69, 70 |
|
Evaluation of potential benefit of using AAC*
|
14-Assessment may also include evaluation of the potential benefit of using augmentative and alternative communication (AAC) to facilitate functional improvements |
Moderate |
Conditional recommendation |
Systematic review with limitations |
71 |
|
Differential Diagnosis ASD** vs. SCD***
|
15-It is important to differentiate between Autism Spectrum Disorder and social communication disorder. Phoniatricians will be instrumental in making this differential diagnosis. |
Moderate |
Conditional recommendation |
2, literature review |
2 |
* AAC=Augmentative & Alternative Communication.
**ASD=Autism Spectrum Disorder.
***SCD=Social Communication Disorder.
|
Statement Topic |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Ongoing assessment
|
16-As part of the ongoing assessment process, dynamic assessment procedures can be used to identify the skills that an individual has achieved, those that may be emerging, and the contextual supports that enhance communication skills (e.g., AAC* or modeling). |
High |
Conditional recommendation |
Systematic review |
72 |
|
Audiological assessment in ASD**
|
17-The similarities in communication and socialization symptoms between hearing impairment and ASD** populations, along with the possibility of dual diagnosis, can present challenges for differential diagnosis. An audiologic assessment is conducted when hearing loss and/or ASD** are suspected. Suggestions for assessing hearing in individuals with these and other challenging behaviors include, for example, minimizing distractions in using the individual’s primary/preferred language form, increasing the individual’s familiarity with assessment procedures prior to testing, allowing the individual to touch and explore earphones; considering the need for auditory brainstem response (ABR) testing when behavioral audiometry is not possible. |
73, moderate
74, very low
|
Conditional recommendation |
73, review
74, case study
|
73, 74 |
* AAC=Augmentative & Alternative Communication.
**ASD=Autism Spectrum Disorder.
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Genetic testing
|
18-Diagnostic evaluation may include genetic testing, particularly if there is a family history of intellectual disability or genetic conditions associated with ASD (e.g., fragile X, tuberous sclerosis) or if the child exhibits physical features suggestive of a possible genetic syndrome. |
High |
Conditional recommendation |
Systematic review with meta-analysis
|
75 |
|
Metabolic testing
|
19-Diagnostic evaluation may include metabolic testing, if the child exhibits symptoms such as lethargy, cyclic vomiting, pica, or seizures. |
High |
Conditional recommendation |
Systematic review with meta-analysis
|
76 |
|
Conveying information to parent
|
20-The phoniatrician’s role includes incorporating a family perspective into the assessment, effectively eliciting information from families about their concerns, beliefs, skills, and knowledge in relation to the individual being assessed. It is important to convey information to families clearly and empathetically. |
Moderate |
Conditional recommendation |
Literature review & Clinical expertise |
77 |
|
Language intervention
|
21-Phoniatricans will need to advocate for inclusion of language intervention for individuals diagnosed with Autism Spectrum Disorder and ensure that individuals with Autism Spectrum Disorder also receive a diagnosis of language disorder, when they meet the criteria. |
Moderate |
Conditional recommendation |
Literature review & clinical experience |
78 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Language intervention
|
22-Regardless of the presence or absence of difficulties acquiring the form and con- tent of language, all individuals with Autism Spectrum Disorder are eligible for speech-language pathology services due to the pervasive nature of the social communication impairment. |
High |
Strong recommendation |
Systematic review with meta-analysis
|
79 |
|
Social communication intervention
|
23-Social communication intervention can have moderate effectiveness in increasing early social communication outcomes (e.g., joint attention, synchronous engagement). |
High |
Strong recommendation |
Systematic review with meta-analysis
|
80 |
|
Intervention for high-functioning individuals with ASD
|
24-It is important to provide intervention to address the gap between cognitive potential and social adaptive functioning. As high-functioning individuals with ASD pose particular challenges both for identification and for determining eligibility for services. |
81, low
82, low
83, low |
Strong recommendation |
81, comparative study
82, qualitative study
83, descriptive study |
81, 82, 83 |
|
Verbal based intervention &Augmentative & Alternative Communication
|
25-The use of verbal-based intervention (i.e., focused play intervention) and augmentative and alternative communication (i.e., Picture Exchange Communication Systems [PECS]) improve spoken and non-verbal communication in minimally verbal children with autism spectrum disorder. |
84, high 85, very low 86, low
|
Strong recommendation |
84, meta analysis study with limitations 85, case study 86, scoping review with limitations
|
84, 85, 86 |
|
Augmentative & Alternative Communication
|
26-Augmentative and alternative communication can be considered an evidence-based practice for supporting social-communication skills in individuals with autism spectrum disorder or intellectual disabilities and complex communication needs. |
87, high 88, moderate
|
Strong recommendation |
87, meta-analysis study with limitations 85,Case study
86, scopin review with limitations
|
87, 88 |
|
Important recommendation
|
27-It is preferable not to recommend computer-based instructions and video modeling in the Egyptian culture for fear that these might be overused / misused by parents and caregivers; thereby increasing the echolalia and deteriorating the child’s social communication skills. |
89, high
90, high
|
Strong recommendation |
89, systematic literature review
90, review of evidence
|
89, 90 |
|
Recommendations regarding watching television & using cell phones and iPad
|
28-It is important to advice the parents and caregivers to reduce, or preferably, totally eliminate whenever possible) the child’s exposure to iPad, cell phones, computers, etc. in a systematically-planned manner and to try to replace these activities with more interactive, communicatively-enriching ones. |
Moderate
|
Strong recommendation |
systematic review with meta-analysis and limitations
|
91 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References
|
|
Auditory/ Sensory Integration Training
|
29-Sensory integration therapies are used to treat integration dysfunction in one or more sensory systems. Treatments can include physical exercise, sensory/tactile stimulation, and auditory integration training. |
92, for sensory integration therapy, insufficient evidence (very low) for sensory integration effectiveness in autism spectrum disorder 93, for auditory integration therapy: The 2002 ASHA Work Group on auditory integration therapy, after reviewing empirical research in the area to date, concludes that AIT has not met scientific standards for efficacy that would justify its practice by audiologists and speech-language pathologists. However, it was mentioned well-designed, institutionally approved, research protocols designed to assess the efficacy of Auditory Integration Therapy are encouraged. It is recommended that this position be reexamined should scientific, controlled studies. supporting AIT's effectiveness and safety become available. |
Strong recommendation
|
92, systematic review
93, empirical research review
|
92, 93 |
|
Applied Behavior Analysis (ABA)
|
30-Applied behavior analysis (ABA) programs are moderately effective in improving socialization skills in children with autism spectrum disorder. |
94, moderate
95, moderate |
Strong recommendation |
94, meta-analytic study with limitations
95, meta-analytic study with limitations |
94, 95 |
|
Early Intensive Behavioral Intervention
|
31-Early intensive behavioral intervention (EIBI) is an effective treatment for children diagnosed with autism spectrum disorders (ASD) with suggested gains in the areas of adaptive behavior, Intelligent Quotient (IQ), communication, socialization, and daily living skills, with the largest gains made in IQ and the smallest in socialization”. |
Moderate
|
Conditional recommendation |
Meta-analysis with limitations for behavioral intervention |
95 |
Intelligent Quotient
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Cognitive Behavioral Therapy (CBT)
|
32-Cognitive Behavioral Therapy (CBT) is an intervention approach with the underlying assumption that an individual’s behavior is mediated by maladaptive patterns of thought or understanding and that change in thinking or cognitive patterns can lead to changes in behavior. |
High
|
Conditional recommendation |
Randomized control trial - Pilot study
|
96 |
|
Parent-mediated
or implemented intervention
|
33-Parent-implemented interventions are likely to result in meaningful improvements in communication for children with Autism Spectrum Disorder (ASD). |
97, high
98, high
99, high
|
Strong recommendation |
97, systematic review 98, randomized controlled trial 99, randomized controlled trial |
97, 98, 99 |
|
Parent-implemented Functional Communication Training
|
34-Parent-implemented [functional communication training] FCT is suggested to produce meaningful reductions in challenging behavior and these changes tend to generalize to other situations and maintain over time. |
High |
Strong recommendation |
Systematic review
|
100 |
*ASD
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Peer- implemented Treatment
|
35-Peer-mediated or implemented treatment approaches incorporate peers as communication partners for children with ASD in an effort to minimize isolation, provide effective role models, and boost communication competence. |
Moderate |
Strong recommendation |
Systematic review with limitations
|
101 |
|
Generalization-promotion strategy
|
36-The use of generalization-promotion strategy (e.g., having a familiar person deliver intervention, teaching across various stimuli and responses) can support successful generalization. |
High
|
Strong recommendation |
Systematic review |
102 |
|
Teaching staff- mediated intervention
|
37-Interventions delivered by teaching staff in an inclusive preschool setting can be effective in improving outcomes for young children with ASD. |
Moderate |
Strong recommendation |
Systematic review with limitations
|
103 |
|
Social communication interventions
|
38-Social communication treatment approaches and frameworks are designed to increase social skills, using social group settings and other platforms. |
High |
Strong recommendation |
Randomized controlled trial |
104 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Group Social Skills Intervention
|
39-Social groups can positively affect social knowledge in youth with ASD. |
Moderate |
Conditional recommendation |
Systematic review with meta-analysis and limitations |
105 |
|
Social story intervention
|
40-Social story interventions can have a positive impact on the social interaction of students with autism spectrum disorder. |
Moderate
|
Conditional recommendation |
Literature review
|
106 |
|
Transition panning
|
41-Effective transition planning involves the student as an active, respected participant of the team as well as his/her family, who can provide valuable information about the student’s needs. |
Moderate |
Conditional recommendation |
Systematic with meta-analysis but additional high quality research was recommended |
107 |
|
Functional communication training in school-age children
|
42-Teachers and other school personnel can successfully implement functional communication training to increase appropriate communication in school-aged children having autism spectrum disorders. |
Moderate
|
Strong recommendation |
Literature review |
108 |
|
Role of peers in social skills modeling
|
43-A peer mentor can serve as a role model and source of social skills information and feedback in social settings providing opportunities for social involvement and the development of friendships. |
High |
Conditional recommendation |
Systematic review
|
109 |
|
Clinical questions |
Action Recommendations |
Evidence Quality |
Strength of Recommendation |
Study Type |
References |
|
Service delivery options
|
44-In addition to determining the type of speech and language treatment that is optimal for children with social communication disorders, phoniatricans consider other ser vice delivery variables—including format, provider, dosage, and timing—that may impact treatment outcomes. |
Moderate |
Conditional recommendation |
Review |
110 |
|
Generalization and maintenance of intervention
|
45-Generalization and maintenance of intervention outcomes are of paramount importance in achieving socially significant outcomes as they invite higher rates of initiation and generalization and enhance the ecological validity of the intervention. |
High |
Strong recommendation |
Systematic review |
111 |
|
Telehealth
|
46-The telehealth (telepractice) component of the intervention or assessment have high levels of program acceptability and parent satisfaction. |
High
|
Conditional recommendation |
Systematic research and review of literature
|
112 |
- Research needs
Suggestions for possible research areas that can be further investigated included:
▪️ Effectiveness of using augmented means in conjunction with verbal output and regular language enhancement therapy in children with severe communication disorders.
▪️ The importance of routine audiological assessment and tympanometry in children with language delay and with no reported hearing concerns.
▪️ Development of standardized Arabic assessment tools for all age groups
▪️ Evidence based proof which language to start to assess in bilingual children
▪️ Role of total communication vs verbal communication in mild-moderate cases of non-verbal children with autism spectrum disorder
▪️ Comorbidities in language disorders with Attention Deficit Hyperactivity Disorder
▪️ Comorbidities in language disorders with apraxia of speech (verbal dyspraxia)
▪️ Genetic basis of language disorders
▪️ The efficacy of using AAC among Egyptian children with autism
▪️ Vocabulary development across different curriculums/school systems in Egypt
▪️ Prevalence of oral motor dysfunction in children with delayed language development
▪️ Developmental norms for Egyptian children as regard all language skills
▪️ Language development in balanced bilingual children
▪️ A comparative study between communication profile of mild ASD associated with language disorders and Social Communication Disorders
▪️ Screening and early diagnosis of mild Autism Spectrum Disorders
▪️ Management of mild Autism Spectrum Disorders
▪️ Effect of ethnographic issues and culture biased issues related to parents’ responses to CARS (Childhood Autism Rating Scale)
▪️ Correlation between findings obtained by open-ended parent questionnaires and CARS findings
▪️ Effectiveness and efficacy of different language therapeutic programs
▪️ Etiological factors related to Specific Language Impairment
▪️ Etiological factors related to Autism Spectrum Disorder
▪️ Global assessment protocol for Autism Spectrum Disorder
▪️ Studying prognosis of autistic children having a metabolic disorder
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria: to assess guideline implementation or adherence to recommendations. This is accomplished if communication skills and quality of life of children with children having language delay and disorders or autism spectrum disorder is improved.
Clinicians should be able to:
▪️ Obtain a full detailed history from the parents
▪️ Provide proper evaluation and differential diagnoses during the assessment process
▪️ Provide the parents with realistic expectations
▪️ Regularly collect data
▪️ Consistent monitoring to the progress achieved with therapy
All clinicians should be aware and informed to consider the following:
▪️ Red Flags that need urgent referral for Assessment/ Management must be taken into consideration.
▪️ For Assessment it is crucial to perform a detailed history and thorough evaluation for all communication skills.
▪️ Intervention plan should focus on the areas of need and strength for each child.
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1- Marchman, V. A., & Fernald, A. (2013). Variability in real-time spoken language processing in typically developing and late-talking toddlers. In L. A. Rescorla & P. S. Dale (Eds.), Late talkers: Language development, interventions, and outcomes (pp. 145–166).
2-American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
3- https://www.asha.org/Practice-Portal/
4-Royal College of Speech & Language Therapists Clinical Guidelines (RCSLT): British Library Cataloguing in Publication Data, Speechmark Publishing Ltd. 2005.
5-WHO handbook for guideline development – 2nd ed. (ISBN 978 92 4 154896 0) © World Health Organization 2014
6- Fisher EL. A Systematic Review and Meta-Analysis of Predictors of Expressive-Language Outcomes Among Late Talkers. J Speech Lang Hear Res.2017 Oct 17;60(10):2935-2948. doi: 10.1044/2017_JSLHR-L-16-0310. PMID: 28915512.
7- Johanna M. Rudolph, Case History Risk Factors for Specific Language Impairment: A Systematic Review and Meta-Analysis, American Journal of Speech-Language Pathology, 2017
8-Aldharman SS, Al-Jabr KH, Alharbi YS, Alnajar NK, Alkhanani JJ, Alghamdi A, Abdellatif RA, Allouzi A, Almallah AM, Jamil SF. Implications of Early Diagnosis and Intervention in the Management of Neurodevelopmental Delay (NDD) in Children: A Systematic Review and Meta-Analysis. Cureus. 2023 May 8;15(5):e38745. doi: 10.7759/cureus.38745. PMID: 37303321; PMCID: PMC10248310.
9- Gidziela A, Ahmadzadeh YI, Michelini G, Allegrini AG, Agnew-Blais J, Lau LY, Duret M, Procopio F, Daly E, Ronald A, Rimfeld K, Malanchini M. A meta-analysis of genetic effects associated with neurodevelopmental disorders and co-occurring conditions. Nat Hum Behav. 2023 Apr;7(4):642-656. doi: 10.1038/s41562-023-01530-y. Epub 2023 Feb 20. PMID: 36806400; PMCID: PMC10129867.
10- Dharmarathna, I., Miles, A., et al. (2020). Twenty Years of Quantitative Instrumental Measures of Swallowing in Children: A Systematic Review, European Journal of Pediatrics, 179(2), 203-223.
11-Chinn, L.K., Zhukova, M.A., Kroeger, R.J. et al. Auditory brainstem response deficits in learning disorders and developmental language disorder: a systematic review and meta-analysis. Sci Rep 12, 20124 (2022). https://doi.org/10.1038/s41598-022-20438-7
12-Do B, Lynch P, Macris EM, Smyth B, Stavrinakis S, Quinn S, Constable PA. Systematic review and meta-analysis of the association of Autism Spectrum Disorder in visually or hearing impaired children. Ophthalmic Physiol Opt. 2017 Mar;37(2):212-224. doi: 10.1111/opo.12350. PMID: 28211175.
13- Taran S, Ahmed W, Bui E, Prisco L, Hahn CD, McCredie VA. Educational initiatives and implementation of electroencephalography into the acute care environment: a protocol of a systematic review. Syst Rev. 2020 Aug 10;9(1):175. doi: 10.1186/s13643-020-01439-x. PMID: 32778151; PMCID: PMC7418425.
14- Lumba-Brown A, Yeates KO, Sarmiento K, et al. Diagnosis and Management of Mild Traumatic Brain Injury in Children: A Systematic Review. JAMA Pediatr. 2018;172(11):e182847. doi:10.1001/jamapediatrics.2018.2847
15- Sunderajan T, Kanhere SV. Speech and language delay in children: Prevalence and risk factors. J Family Med Prim Care. 2019 May;8(5):1642-1646. doi: 10.4103/jfmpc.jfmpc_162_19. PMID: 31198730; PMCID: PMC6559061.
16- Halle JW, Anderson SR. Natural environment language assessment and intervention with severely impaired preschoolers. Topics in Early Childhood Special Education. 1984 Jul;4(2):36-56.
17-Boone, H., & Crais, E. R. (1999). Strategies for achieving: Family-driven assessment and intervention planning. Young Exceptional Children, 3(1), 2–11. https://doi.org/10.1177/109625069900300101.
18-Crais, E. R., Roy, V. P., & Free, K. (2006). Parents’ and professionals’ perceptions of the implementation of family-centered practices in child assessments. American Journal of Speech-Language Pathology, 15(4), 365–377. https://doi.org/10.1044/1058-0360(2006/034).
19-Dollaghan, C. (2004). Evidence-based practice in communication disorders: What do we know, and when do we know it? Journal of Communication Disorders, 37(5), 391–400. https://doi.org/10.1016/j.jcomdis.2004.04.002.
20-Raaijmakers MF, Dekker J, Dejonckere PH & Zee J van der, 1995, ‘Reliability of the assessment of impairments, disabilities and handicaps in survey research on speech therapy’, Folia Phoniatrica Logopedica 47 (4):199–209.
21- Narayanan, S., Vijayan, K., Vastare Guruprasad, M., Prabhu P, P., & Barman, A. (2022). Oral and Verbal Praxis in Impaired Language Learners. Perceptual and Motor Skills, 129(1), 33-46. https://doi.org/10.1177/00315125211056421
22- Glogowska M, Campbell R, Peters TJ, Roulstone S, Enderby P. Developing a scale to measure parental attitudes towards preschool speech and language therapy services. Int J Lang Commun Disord. 2001 Oct-Dec;36(4):503-13. doi: 10.1080/13682820110075006. PMID: 11802500.
32 Guralnick, M. J. (2017). Early intervention for children with intellectual disabilities: An update. Journal of Applied Research in Intellectual Disabilities, 30(2), 211–229. https://doi.org/10.1111/jar.12233
33-Hirschman M, 2000, ‘Language repair via metalinguistic means’, International Journal
of Language & Communication Disorders 35 (2):251–68.
34-Ebbels S & Lely H van der, 2001, ‘Meta-syntactic therapy using visual coding for children with
persistent SLI’, International Journal of Language & Communication Disorders expressive specific language impairment (SLI) 36 (Suppl):345–50.
35-Bryan A, 1997, ‘Colourful Semantics’, in Chiat S, Law J & Marshall J (eds) Language Disorders in
Children and Adults: Psycholinguistic Approaches to Therapy, Whurr Publishers, London
36-Tallal P, Stark RE & Mellits ED, 1985, ‘Identification of language-impaired children on the basis of rapid perception and production skills’, Brain & Language 25 (2):314–22.
37- Michael O Ogundele (2017). A Multidisciplinary Approach to the Assessment and Management of Pre-school Age Neuro-developmental Disorders: A Local Experience. Clinical Journal of Nursing Care and Practice, 1(1), 1-12. https://www.europub.co.uk/articles/-A-560224
38-Idol, L., Nevin, A., & Paolucci-Whitcomb, P. (1994). Collaborative consultation. Austin, TX: Pro-Ed.
39-Paul, D. R., Blosser, J., & Jakubowitz, M. D. (2006). Principles and challenges for forming successful literacy partnerships. Topics in Language Disorders, 26(1), 5–23.
40- Shelden, M. L., & Rush, D. D. (2013). The early intervention teaming handbook: The primary service provider approach. Brookes
41- Romski M, Sevcik RA, Adamson LB, Cheslock M, Smith A, Barker RM, Bakeman R. Randomized comparison of augmented and nonaugmented language interventions for toddlers with developmental delays and their parents. J Speech Lang Hear Res. 2010 Apr;53(2):350-64. doi: 10.1044/1092-4388(2009/08-0156). PMID: 20360461
42- Lüke, C. (2016). Impact of speech-generating devices on the language development of a child with childhood apraxia of speech: a case study. Disability and Rehabilitation: Assistive Technology, 11(1), 80–88. https://doi.org/10.3109/17483107.2014.913715
43-Wright CA, Kaiser AP, Reikowsky DI, Roberts MY. Effects of a naturalistic sign intervention on expressive language of toddlers with Down syndrome. J Speech Lang Hear Res. 2013 Jun;56(3):994-1008. doi: 10.1044/1092-4388(2012/12-0060). Epub 2012 Dec 28. PMID: 23275419.
44-Drager KD, Postal VJ, Carrolus L, Castellano M, Gagliano C, Glynn J. The effect of aided language modeling on symbol comprehension and production in 2 preschoolers with autism. Am J Speech Lang Pathol. 2006 May;15(2):112-25. doi: 10.1044/1058-0360(2006/012). PMID: 16782684.
45- Harris MD, Reichle J. The impact of aided language stimulation on symbol comprehension and production in children with moderate cognitive disabilities. Am J Speech Lang Pathol. 2004 May;13(2):155-67. doi: 10.1044/1058-0360(2004/016). PMID: 15198634.
46-Binger, C., & Light, J. (2007). The effect of aided AAC modeling on the expression of multi-symbol messages by preschoolers who use AAC. Augmentative and Alternative Communication, 23(1), 30–43. https://doi.org/10.1080/07434610600807470
47- Goossens’, C., Crain, S. S., & Elder, P. (1992). Engineering the preschool environment for interactive symbolic communication 18 months to 5 years developmentally. Birmingham, AL: Southeast Augmentative Communication Publications.
48- Cui M, Ni Q, Wang Q. Review of intervention methods for language and communication disorders in children with autism spectrum disorders. PeerJ. 2023 Aug 9;11:e15735. doi: 10.7717/peerj.15735. PMID: 37576502; PMCID: PMC10422951.
49-Bennett, M., Goodall, E. A Meta-analysis of DSM-5 Autism Diagnoses in Relation to DSM-IV and DSM-IV-TR. Rev J Autism Dev Disord 3, 119–124 (2016). https://doi.org/10.1007/s40489-016-0070-4
50-Wiggins LD, Rice CE, Barger B, Soke GN, Lee LC, Moody E, Edmondson-Pretzel R, Levy SE. DSM-5 criteria for autism spectrum disorder maximizes diagnostic sensitivity and specificity in preschool children. Soc Psychiatry Psychiatr Epidemiol. 2019 Jun;54(6):693-701. doi: 10.1007/s00127-019-01674-1. Epub 2019 Mar 8. PMID: 30850887; PMCID: PMC6713264
51-Randall M, Egberts KJ, Samtani A, Scholten RJPM, Hooft L, Livingstone N, Sterling‐Levis K, Woolfenden S, Williams K. Diagnostic tests for autism spectrum disorder (ASD) in preschool children. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No.: CD009044. DOI: 10.1002/14651858.CD009044.pub2. Accessed 25 April 2024.
52-Baron-Cohen S, Allen J, Gillberg C. Can autism be detected at 18 months? The needle, the haystack, and the CHAT. Br J Psychiatry. 1992 Dec;161:839-43. doi: 10.1192/bjp.161.6.839. PMID: 1483172.
53-Mundy P, Sigman M, Kasari C. A longitudinal study of joint attention and language development in autistic children. J Autism Dev Disord. 1990 Mar;20(1):115-28. doi: 10.1007/BF02206861. PMID: 2324051.
54-Charman T, 1998, ‘Specifying the nature and course of the joint attention impairment in autism in the pre-school years: Implications for diagnosis and intervention’, Autism 2 (1):61–79.
55-Pascualvaca DM, Fantie BD, Papageorgiou M & Mirsky AF, 1998, ‘Attentional capacities in children with autism: Is there a general deficit in shifting focus?’, Journal of Autism and Developmental Disorders 28 (6): 40–46.
56-Cooper J, Moodley M & Reynell J, 1978, Helping Language Development, E Arnold, London.
57-Tofani M, Scarcella L, Galeoto G, Giovannone F, Sogos C. Behavioral gender differences across Pre-School Children with Autism Spectrum Disorders: a cross-sectional study. J Autism Dev Disord. 2023 Aug;53(8):3301-3306. doi: 10.1007/s10803-022-05498-y. Epub 2022 Mar 15. PMID: 35290561; PMCID: PMC10313842.
58-Dawson G, Meltzoff AN, Osterling J, Rinaldi J & Brown E, 1998, ‘Children with autism fail to orient to naturally occurring social stimuli’, Journal of Autism & Developmental Disorders 20 children two social and two non-social stimuli and in 28 (6):479–85.
59-Frith U, 1989, Autism: Explaining the Enigma, IV Blackwell Publishers, Oxford.
60-Happe F, 2001, ‘Social and nonsocial development in autism: Where are the links?’ in Burack JA, Charman T, Yirmiya N & Zelazo PR (eds) The Development of Autism: Perspectives from Theory and Research, Lawrence Erlbaum Associates, Mahwah, NJ.
61-Wimpory DC, Hobson RP, Williams JM & Nash S, 2000, ‘Are infants with autism socially engaged? A study of recent retrospective parental reports’, Journal of Autism & Developmental Disorders 30 (6):525–36.
62-Wing L & Gould J, 1979, ‘Severe impairments of social interaction and associated abnormalities in children: Epidemiology and classification’, Journal of Autism & Developmental Disorders 9 (1):11–29.
63-Baron-Cohen S, Wheelwright S, Cox A, Baird G, Charman T, Swettenham J, Drew A & Doehring P (2000)
64-Tincani, M., Travers, J., & Boutot, A. (2009). Race, Culture, and Autism Spectrum Disorder: Understanding the Role of Diversity in Successful Educational Interventions. Research and Practice for Persons with Severe Disabilities, 34(3-4), 81-90. https://doi.org/10.2511/rpsd.34.3-4.81
65-Broome K, McCabe P, Docking K, Doble M. A Systematic Review of Speech Assessments for Children With Autism Spectrum Disorder: Recommendations for Best Practice. Am J Speech Lang Pathol. 2017 Aug 15;26(3):1011-1029. doi: 10.1044/2017_AJSLP-16-0014. PMID: 28772287.
76- Dhanasekara CS, Ancona D, Cortes L, et al. Association Between Autism Spectrum Disorders and Cardiometabolic Diseases: A Systematic Review and Meta-analysis. JAMA Pediatr. 2023;177(3):248–257. doi:10.1001/jamapediatrics.2022.5629
77-Marcus, L. M., Kunce, L. J., & Schopler, E. (2005). Working with families. In F. R. Volkmar, R. Paul, A. Klin, & D. Cohen (Eds.), Handbook of autism and pervasive developmental disorders: Volume 1: Diagnosis, development, neurobiology, and behavior (pp. 1055–1086). Wiley.
78-American Speech-Language-Hearing Association. (2016). Scope of practice in speech-language pathology [Scope of Practice]. www.asha.org/policy/
79-Hampton LH, Kaiser AP. Intervention effects on spoken-language outcomes for children with autism: a systematic review and meta-analysis. J Intellect Disabil Res. 2016 May;60(5):444-63. doi: 10.1111/jir.12283. PMID: 27120988.
80-Defining Early Social Communication Skills: A Systematic Review and Analysis
81-Gilchrist, A., Green, J., Cox, A., Burton, D., Rutter, M., & Le Couteur, A. (2001). Development and current functioning in adolescents with Asperger syndrome: A comparative study. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42(2), 227–240. https://doi.org/10.1017/S0021963001006631
82-Müller, E.A. & Schuler, A. & Burton, B.A. & Yates, Gregory. (2003). Meeting the vocational support needs of individuals with Asperger Syndrome and other autism spectrum disabilities. Journal of Vocational Rehabilitation. 18. 163-175.
83-Tsatsanis, K. D., Foley, C., & Donehower, C. (2004). Contemporary outcome research and programming guidelines for Asperger syndrome and high-functioning autism. Topics in Language Disorders, 24(4), 249–259.Hansen, S. G., Carnett, A., et al. (2018). Advances in Neurodevelopmental Disorders, 2(1), 116-128.
84-Brignell A, Chenausky KV, Song H, Zhu J, Suo C, Morgan AT. Communication interventions for autism spectrum disorder in minimally verbal children. Cochrane Database Syst Rev. 2018 Nov 5;11(11):CD012324. doi: 10.1002/14651858.CD012324.pub2. PMID: 30395694; PMCID: PMC6516977.
85-Malhotra S, Rajender G, Bhatia MS, Singh TB. Effects of picture exchange communication system on communication and behavioral anomalies in autism. Indian J Psychol Med. 2010 Jul;32(2):141-3. doi: 10.4103/0253-7176.78513. PMID: 21716776; PMCID: PMC3122547.
86-Gibson JL, Pritchard E, de Lemos C. Play-based interventions to support social and communication development in autistic children aged 2-8 years: A scoping review. Autism Dev Lang Impair. 2021 Jun 8;6:23969415211015840. doi: 10.1177/23969415211015840. PMID: 36381525; PMCID: PMC9620698
87-Langarika-Rocafort A, Mondragon NI, Etxebarrieta GR. A Systematic Review of Research on Augmentative and Alternative Communication Interventions for Children Aged 6-10 in the Last Decade. Lang Speech Hear Serv Sch. 2021 Jul 7;52(3):899-916. doi: 10.1044/2021_LSHSS-20-00005. Epub 2021 Apr 28. PMID: 33909476.
88-Van der Meer, L. A. J., & Rispoli, M. (2010). Communication interventions involving speech-generating devices for children with autism: A review of the literature. Developmental Neurorehabilitation, 13(4), 294–306. https://doi.org/10.3109/17518421003671494
89-Slobodin O, Heffler KF, Davidovitch M. Screen Media and Autism Spectrum Disorder: A Systematic Literature Review. J Dev Behav Pediatr. 2019 May;40(4):303-311. doi: 10.1097/DBP.0000000000000654. PMID: 30908423.
90-Lane R, Radesky J. Digital Media and Autism Spectrum Disorders: Review of Evidence, Theoretical Concerns, and Opportunities for Intervention. J Dev Behav Pediatr. 2019 Jun;40(5):364-368. doi: 10.1097/DBP.0000000000000664. PMID: 30973425; PMCID: PMC6579611.
91-Ophir Y, Rosenberg H, Tikochinski R, Dalyot S, Lipshits-Braziler Y. Screen Time and Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. JAMA Netw Open. 2023 Dec 1;6(12):e2346775. doi: 10.1001/jamanetworkopen.2023.46775. PMID: 38064216; PMCID: PMC10709772.
92- Lang R, O'Reilly M, Healy O, et al. Sensory integration therapy for autism spectrum disorders: a systematic review. 2012. In: Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK100214/
93-American Speech-Language-Hearing Association. (2004). Auditory integration training [Position Statement]. Available from www.asha.org/policy.
94-Makrygianni MK, Gena A, Katoudi S, Galanis P. The effectiveness of applied behavior analytic interventions for children with autism spectrum disorder: A meta-analytic study. Research in Autism Spectrum Disorders. 2018;51(June 2017):18–31. doi: 10.1016/j.rasd.2018.03.006.
95-Westby, C. (2022). Meta-Analysis of Autism Interventions. Word of Mouth, 33(3), 1-6. https://doi.org/10.1177/10483950211059898
96-Scarpa A, Reyes NM. Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: a pilot study. Behav Cogn Psychother. 2011 Jul;39(4):495-500. doi: 10.1017/S1352465811000063. Epub 2011 Apr 4. PMID: 21457605.
97-Althoff, Colleen et al. “Parent-Mediated Interventions for Children With Autism Spectrum Disorder: A Systematic Review.” The American journal of occupational therapy : official publication of the American Occupational Therapy Association 73 3 (2019): 7303205010p1-7303205010p13.
98-Sofronoff K, Leslie A, Brown W. Parent management training and Asperger syndrome: a randomized controlled trial to evaluate a parent based intervention. Autism 2004;8(3):301-17.
99-Tonge B, Brereton A, Kiomall M, MacKinnon A, King N, Rinehart N. Effects on Parental Mental Health of an Education and Skills Training Program for Parents of Young Children With Autism: A Randomized Controlled Trial. J Am Acad Child Adolesc Psychiatry 2006;45(5):561-9.
100-Gerow, S., Hagan-Burke, S., et al. A Systematic Review of Parent-Implemented Functional Communication Training for Children With ASD, Behavior Modification, 2018; 423), 335-363.
101-Chang YC, Locke J. A systematic review of peer-mediated interventions for children with autism spectrum disorder. Res Autism Spectr Disord. 2016 Jul;27:1-10. doi: 10.1016/j.rasd.2016.03.010. Epub 2016 Mar 26. PMID: 27807466; PMCID: PMC5087797.
102-Gunning, Ciara & Holloway, Jennifer & Fee, Bairbre & Breathnach, Orfhlaith & Bergin, Ceara & Greene, Irene & Ní Bheoláin, Ruth. (2019). A Systematic Review of Generalization and Maintenance Outcomes of Social Skills Intervention for Preschool Children with Autism Spectrum Disorder. Review Journal of Autism and Developmental Disorders. 6. 1-28. 10.1007/s40489-019-00162-1.
103-Tupou, J., van der Meer, L., Waddington, H., & Sigafoos, J. (2019). Preschool interventions for children with autism spectrum disorder: A review of effectiveness studies. Review Journal of Autism and Developmental Disorders, 6(4), 381–402. https://doi.org/10.1007/s40489-019-00170-1
104-Adams, C., Lockton, E., Freed, J., Gaile, J., Earl, G., McBean, K., Green, J., Vail, A., & Law, J. (2012). The Social Communication Intervention Project: A randomized controlled trial of the effectiveness of speech and language therapy for school-age children who have pragmatic and social communication problems with or without autism spectrum disorder. International Journal of Language and Communication Disorders, 47(3), 233–244.
105-Hotton, M., Coles, S. The Effectiveness of Social Skills Training Groups for Individuals with Autism Spectrum Disorder. Rev J Autism Dev Disord 3, 68–81 (2016). https://doi.org/10.1007/s40489-015-0066-5
106-Karal, M. A., & Wolfe, P. S. (2018). Social Story Effectiveness on Social Interaction for Students with Autism: A Review of the Literature, Education & Training in Autism & Developmental Disabilities, 53(1), 44-58.
107-Sanderson, K. A., & Goldman, S. E. (2020). A Systematic Review and Meta-Analysis of Interventions Used to Increase Adolescent IEP Meeting Participation. Career Development and Transition for Exceptional Individuals, 43(3), 157-168. https://doi.org/10.1177/2165143420922552
108-Andzik, N. R., Cannella-Malone, H. I., & Sigafoos, J. (2016). Practitioner-Implemented Functional Communication Training: A Review of the Literature. Research and Practice for Persons with Severe Disabilities, 41(2), 79-89. https://doi.org/10.1177/1540796916633874
109-Laura Gehreke, Hannes Schilling, Simone Kauffeld (2024). Effectiveness of peer mentoring in the study entry phase: A systematic review. Review of Education 12(1). https://doi.org/10.1002/rev3.3462
110-National Research Council. (2001). Educating children with autism. National Academy Press.
111-Gunning, C., Holloway, J., Fee, B. et al. A Systematic Review of Generalization and Maintenance Outcomes of Social Skills Intervention for Preschool Children with Autism Spectrum Disorder. Rev J Autism Dev Disord 6, 172–199 (2019). https://doi.org/10.1007/s40489-019-00162-1
112-Sutherland, R., Trembath, D., & Roberts, J. (2018). Telehealth and autism: A systematic search and review of the literature. International Journal of Speech-Language Pathology, 20(3), 324–336. https://doi.org/10.1080/17549507.2018.1465123References for guidelines involved in the selection process:
▪️ Royal College of Speech & Language Therapists Clinical Guidelines (RCSLT): British Library Cataloguing in Publication Data, Speechmark Publishing Ltd. 2005.
▪️ Missouri Autism Guidelines Initiative: Autism Spectrum Disorders: Guidance to Evidence-based Practice. 2012.
▪️ NICE Guideline for Recognition: Referral, Diagnosis and Management of Adults on the Autism Spectrum. National Clinical Guideline Number 142, National Collaborating Centre for Mental Health commissioned by the National,Institute for Health & Clinical Excellence, The British Psychological Society & The Royal College of Psychiatrists. 2012.
▪️ KCE: Management of Autism in Children and Young People: A Good Clinical Practice Guideline, KCE Report.2014.
▪️ ht t ps://www.asha.or g/Pr ac t ic e -Por t al/Cl inic al- Topics/Autism/ American Speech-Language-Hearing Association.
▪️ https://www.asha.org/Practice-Portal/Clinical-Topics/ Late-Language-Emergence/American Speech- Language-Hearing Association.
▪️ https://www.asha.org/Practice-Portal/About/.
▪️ https://www.asha.org/Practice-Portal/Clinical-Topics/ Spoken-Language-Disorders/.
▪️ Clinical Guidelines, Speech Therapy, Version 1: evicore Healthcare innovative solutions, American Medical Association. 2019.
Further readings:
▪️ Guidelines Review Committee, Quality Assurance of Norms and Standards. WHO handbook for guideline development, 2nd Edition, Chapter 10 page 129.
▪️ Schünemann, Brożek, Guyatt, Oxman GRADE Handbook, Chapter 5; Quality of evidence, 2013
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external
funding.
▪️ All the guideline development group members have
declared that they do not have any competing interests.
Annex 1: Guideline Flowcharts
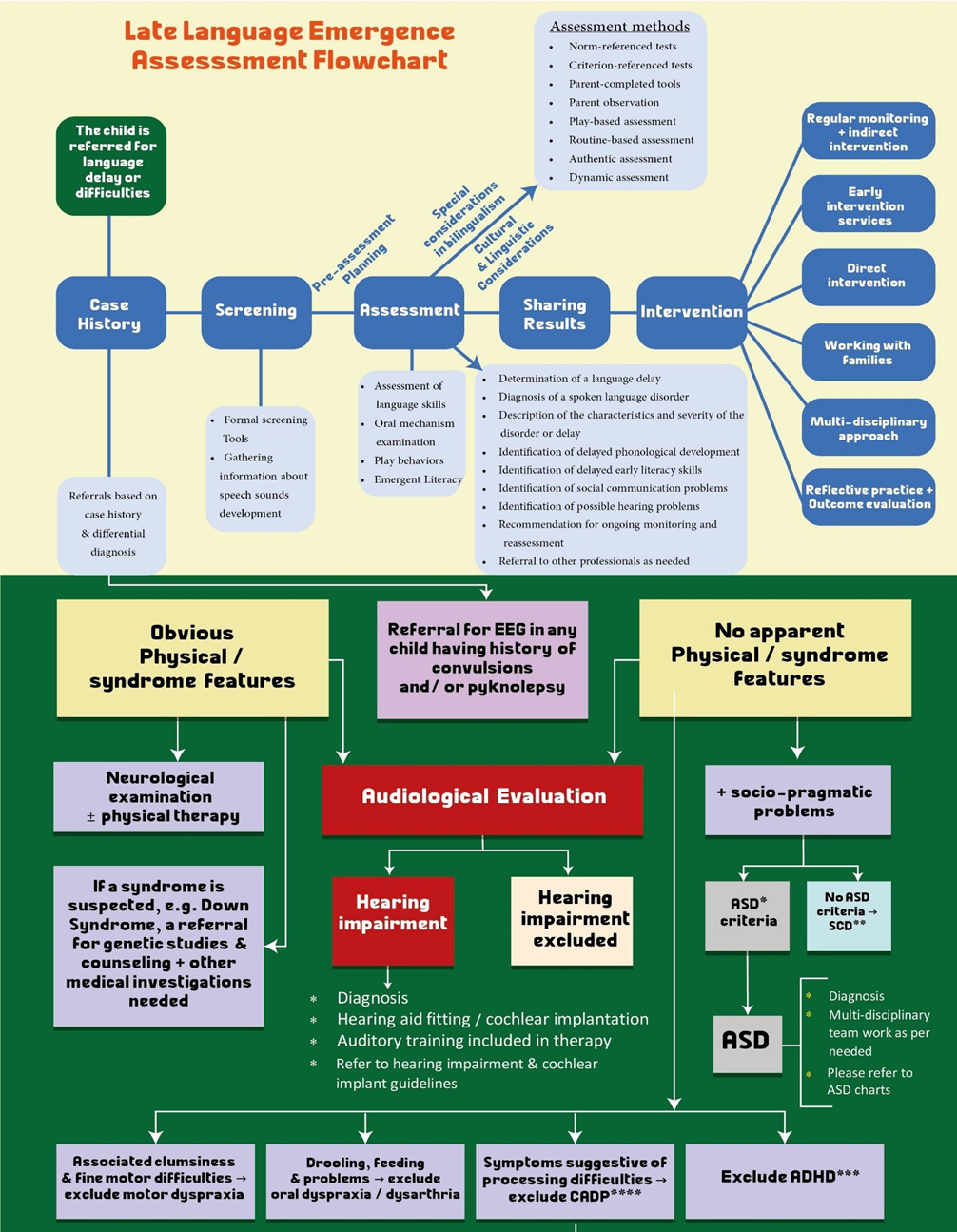
*ASD = Autism Spectrum Disorder.
**SCD = Social Communication Disorder.
***ADHD = Attention Deficit Hyperactivity Disorder.
****CAPD=Central Auditory Processing Disorder.
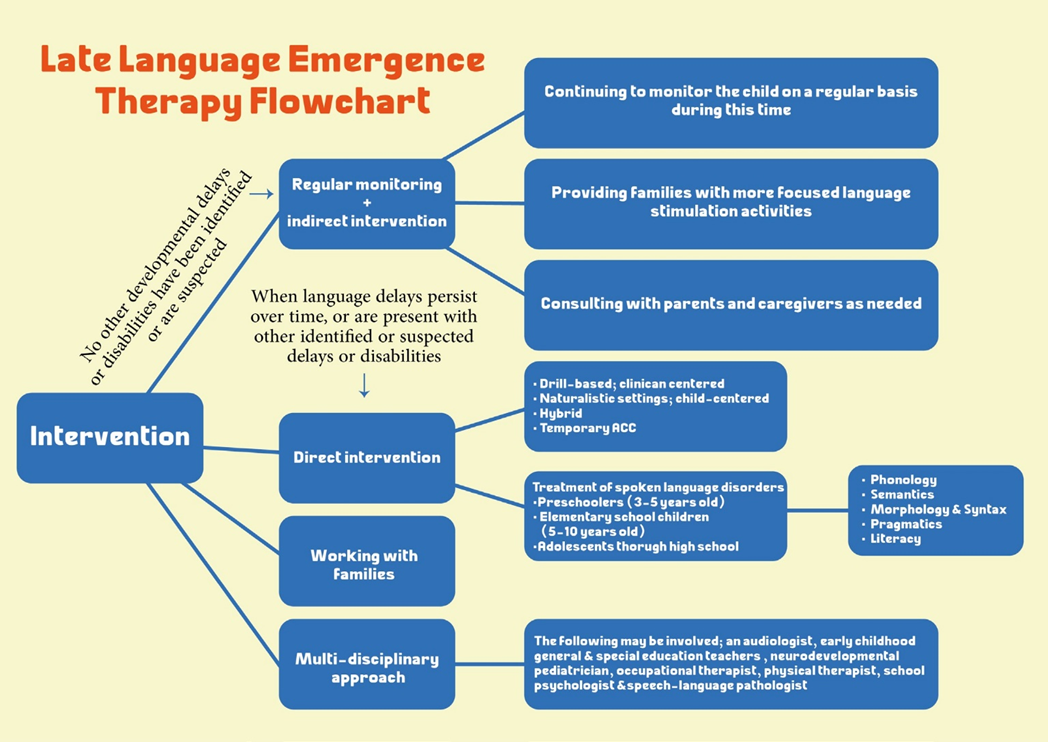
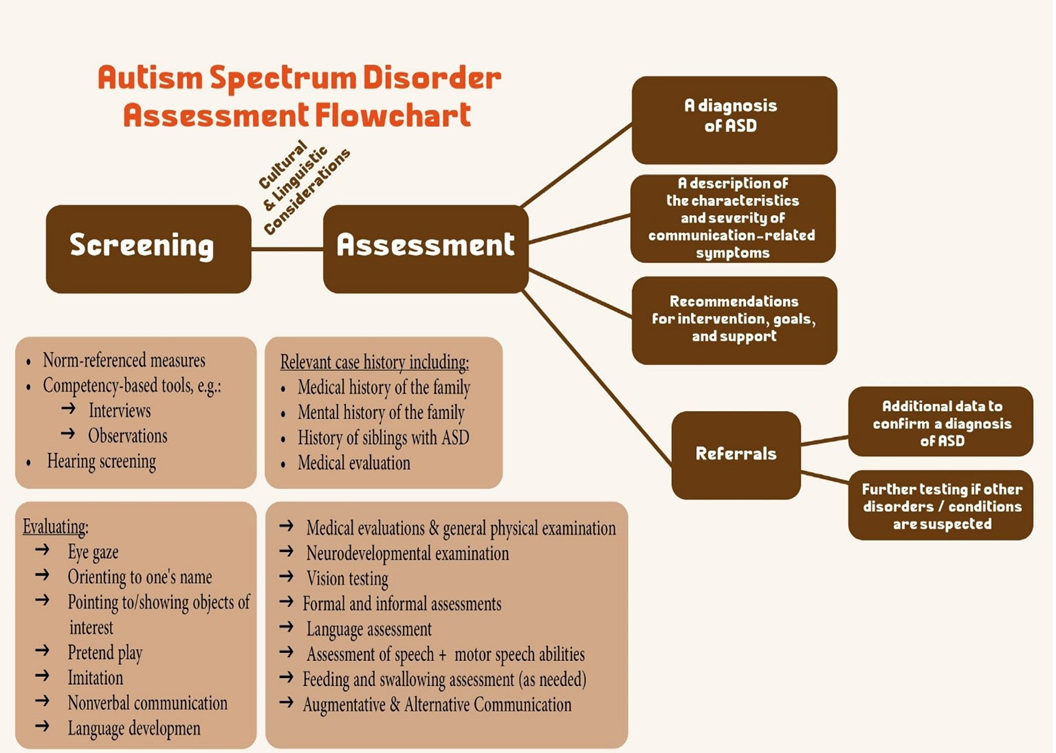
*ASD = Autism Spectrum Disorder.
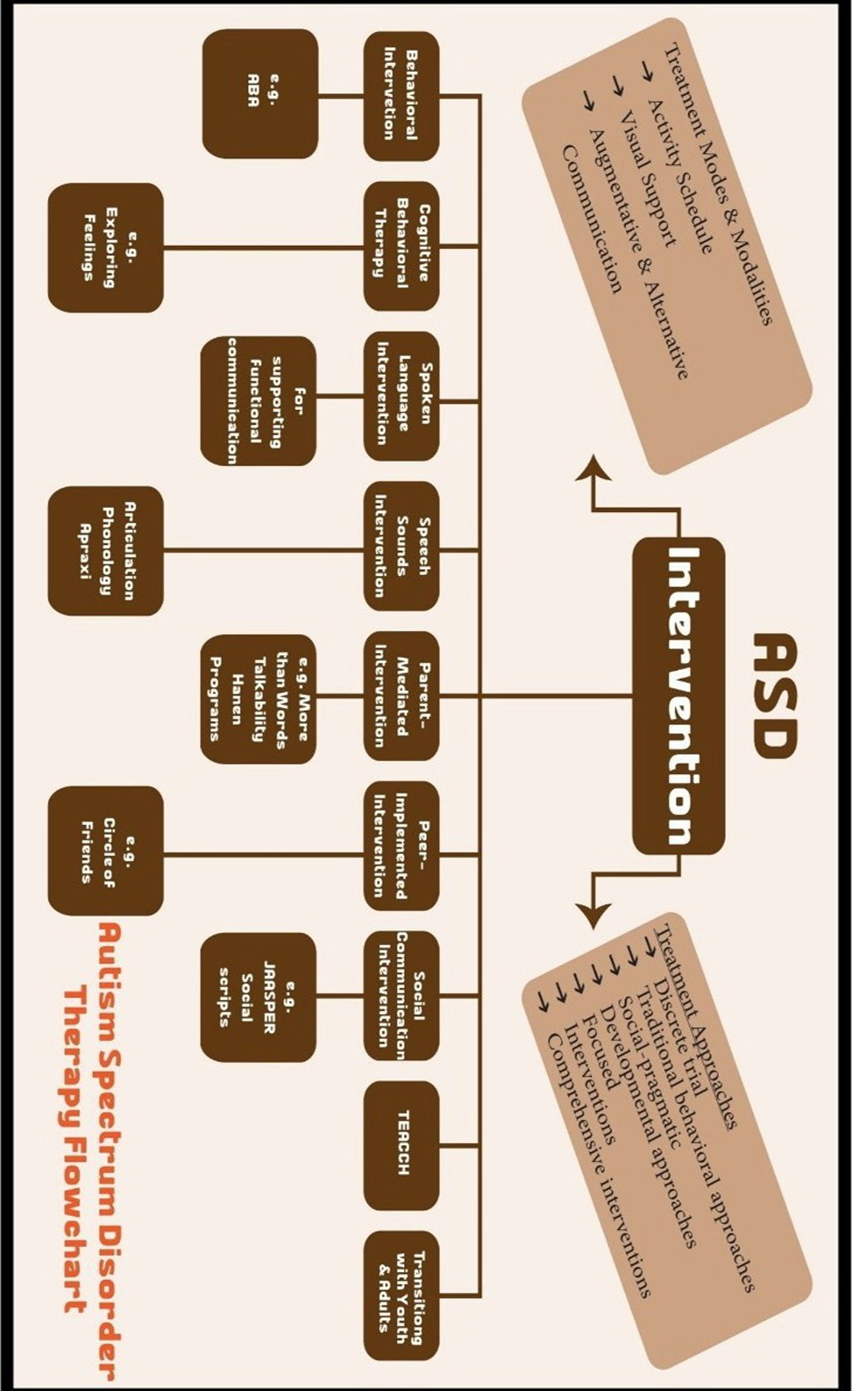
Annex 2: Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
Table 1: Assessment of Currency
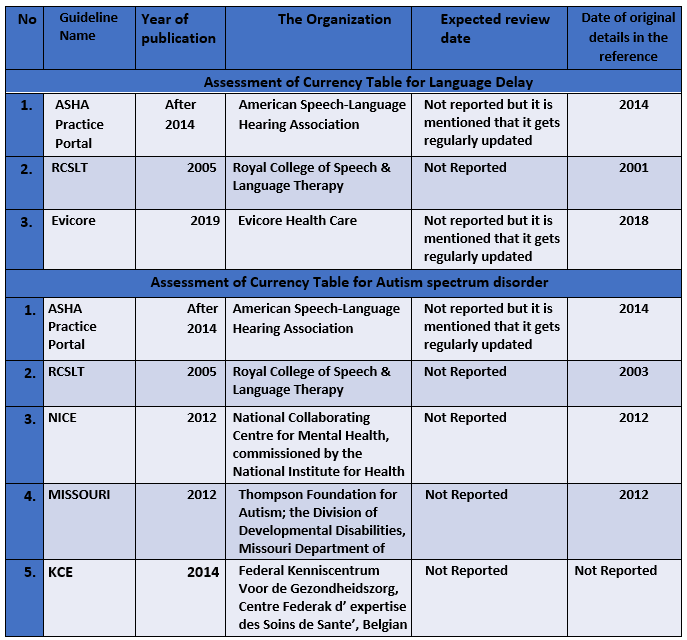
Table 2: Assessment of Content
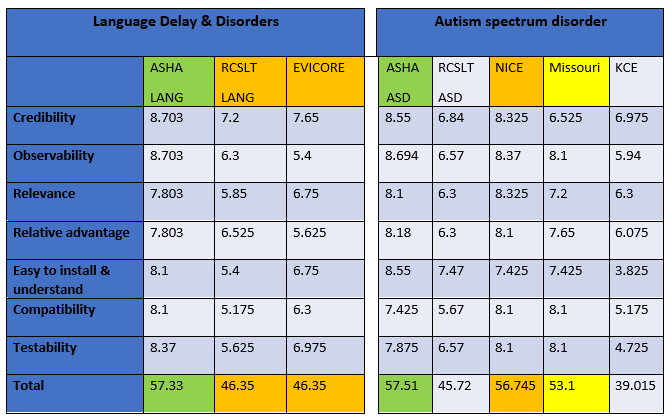
Table 3: Assessment of Quality
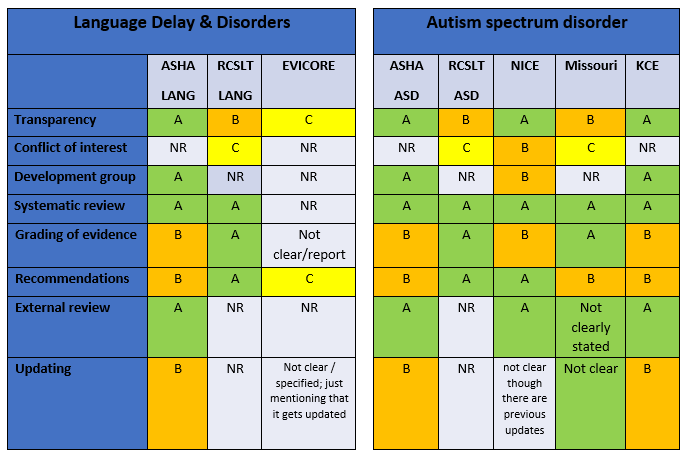
Annex 3: The risks and benefits of added and/or modified
statements
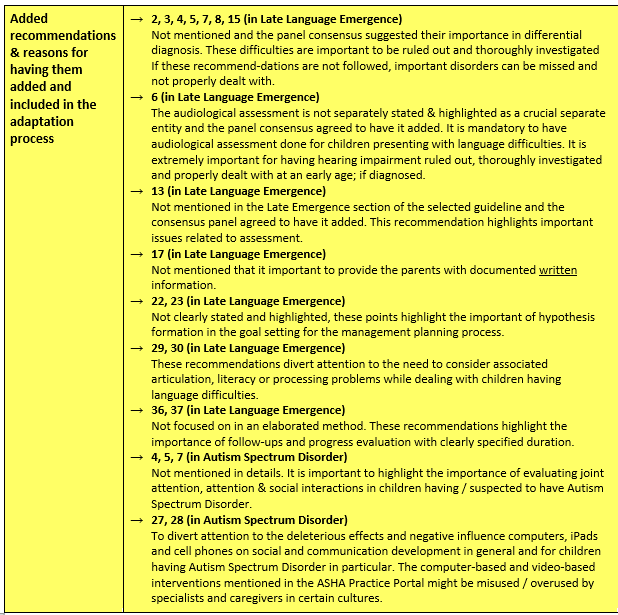
Benefits and Risks/ harms in relation to updated statements
For Late Language Emergence section:
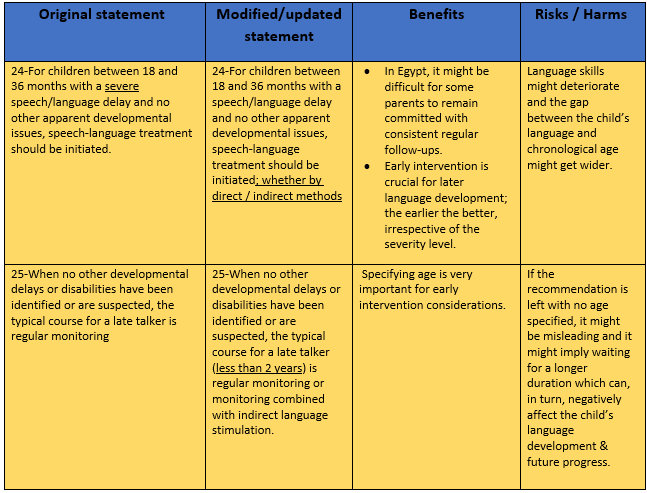
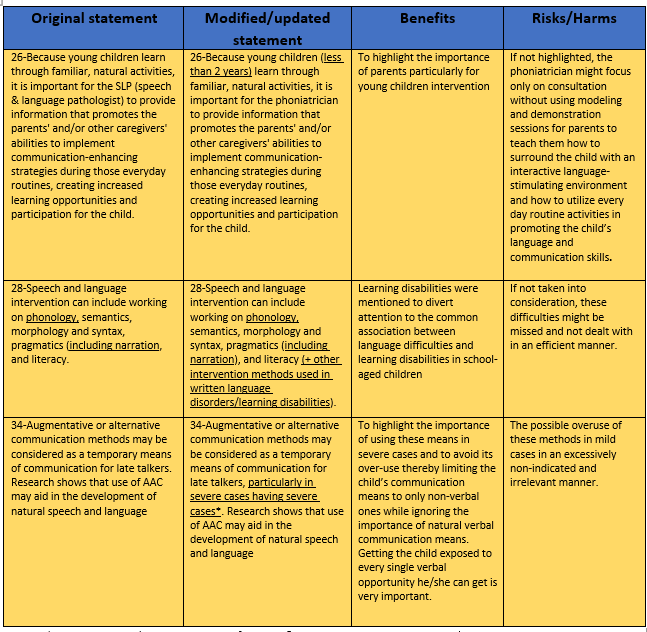
*Severe cases such as severe cases of apraxia & severe Autism Spectrum Disorder
For Autism Spectrum Disorder Section: