Rehabilitation of Laryngectomised Patients Adapted (ECPG)
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Rehabilitation of Laryngectomised Patients Adapted (ECPG) |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:00 PM |
Description
"last update: 10 June 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baleegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mahmoud Abdel Aziz,5 Mohamed Ghonaim,6 Tarek Ghanoum,7 Mahmoud Youssef8
Phoniatrics Manager: Mahmoud Youssef8
Phoniatrics Executive Manager: Dalia Mostafa9
Assembly Board: Amal Saeed10, Aya Sheikhany9, Hemmat El-baz11, Effat Zaky12
Grading Board (In alphabetical order)
Ahlam El Adawy13, Aisha Fawzy9, Asmaa El-Dessuky14, Dalia Mostafa9, Essam Aref15, Hanan Anwar14
Reviewing Board: Elham Magdy10, Eman Ezzat 14, Sabah Hassan8, Ibrahim Khaled16, Shaimaa Farouk17
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 3Otorhinolaryngology Department, Faculty of Medicine/ Minia University, 4Otorhinolaryngology Department, Faculty of Medicine/Beni-Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 6Otorhinolaryngology Department, Faculty of Medicine/Mansoura University, 7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 10Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Zagazig University, 11Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 12Phoniatrics Unit, Otorhinolaryngology Department/ Faculty of Medicine/ Minia University. 13Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Sohag University, 14Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 15Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 16Otorhinolaryngology Department, Faculty of Medicine/ Zagazig University. 17 Radiotherapy & Nuclear Medicine Department Zagazig university.
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Abbreviations
ASHA: American Speech-Language and Hearing Association.
CPG: Clinical Practical Guideline.
EBP: Evidence-based practice.
ECPG: Egyptian Clinical Practical Guideline.
GRADE: Grading of Recommendations Assessment, Development and Evaluation.
HME: Heat and Moisture Exchange.
TEP: Tracheoesophageal Puncture.
VFSS: Video-Fluoroscopic Swallow Study.
- Executive Summary
1- The patient is presented with severe dysphonia, dysphagia and/ or stridor (conditional recommendation).
2- Patient interview and data collection are needed followed by detailed endoscopic, radiological and laboratory investigations (conditional recommendation).
3- If assessment revealed the presence of extensive malignant laryngeal mass, patient should be informed about the possible lines of intervention, including total laryngectomy (conditional recommendation).
4- Pre-operative assessment of voice and swallowing is done (conditional recommendation).
5- Total laryngectomy decision is taken, based on all pre-operative assessment lines and the surgery is done (strong recommendation).
6- The post-operative anatomical and physiological changes have to be discussed with the patient as well as the expected communication and swallowing problems after intervention (conditional recommendation).
7- Post-intervention detailed assessment is needed (conditional recommendation) including:
▪️ Patient interview and case history.
▪️ Baseline assessments of communication and swallowing are done & instrumental assessments may be needed for evaluation of the oro-pharyngeal swallow using video-Fluoroscopic swallowing Study (VFSS).
▪️ Questionnaires about quality of life may be administered.
8- Then the rehabilitation plan is tailored according to the patient conditions and preferences (strong recommendation):
a. Voice and speech rehabilitation is done by any of the following methods:
▪️ Tracheo-esophageal puncture using speech valve e.g., Provox or Blom & Singer speech valves.
▪️ Esophageal speech (unaided) training sessions
▪️ Electro-larynx or external vibrator.
b. Swallowing and smell rehabilitation may be needed according to the difficulty (conditional recommendation).
c. Care of the neck stoma includes measures of protection against dust, dryness and droplet infection. The use of Heat and Moisture Exchanger (HME) system may help protection of the air way (conditional recommendation).
- Introduction, purpose, scope and audience
➡️Introduction
➡️Scope:
The scope of the guideline provides a brief overview of the rehabilitation of total laryngectomy (e.g. current policy and practice) as well as the key issues that will be considered in the guideline that is related to adult patients having total laryngectomy. The guidelines should improve the clinical practice of the clinicians in assessing and treating those patients with the best evidence-based practice methods.
➡️Target audience:
Phoniatricians, ENT surgeons, critical care physicians, radiotherapists, oncology physicians and nurses who are dealing with adults with total laryngectomy.
- Methods
Methods of development:
➡️Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Phoniatrics Chief Manager, Phoniatrics Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
➡️Search Method
Electronic database searched:
Pubmed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar
➡️Keywords:
Laryngectomized patients, guideline, rehabilitation, voice
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Time period searched: From 2002 to 2023.
➡️Results:Five guidelines were selected for assessment, treatment and rehabilitation of patients having extensive Cancer larynx which necessitates total laryngectomy,1,2,3,4,5. The selected guidelines were assessed by four experts in Phoniatrics and the ASHA (2015)1. Speech-Language Pathology Medical Review Guidelines had the highest scores as regards to the currency, contents and quality. It was graded by six expert phoniatricians and reviewed by three expert reviewers to improve quality, gather feedback on draft recommendations. The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
Audience Strong
recommendation Conditional recommendation Patients Most individuals in this situation
would want the recommended course of action; only a small proportion would
not. Formal decision aides are not likely
to be needed to help individuals make decisions consistent with their values
and preferences. Most individuals in this situation
would want the suggested course of action, but many would not Clinicians Most individuals should receive the
intervention. Adherence to the recommendation could
be used as a quality criterion or performance indicator. Different choices will be appropriate
for individual patients, who will require assistance in arriving at a
management decision consistent with his or her values and preferences.
Decision aides may be useful in helping individuals make decisions consistent
with their values and preferences.
|
WHO handbook for guideline development – 2nd ed. Chapter 10, page 129 The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013) 6 |
|
|
Grade |
Definition |
|
High ++++ |
We are very confident that the true effect lies close to that of the estimate of the effect |
|
Moderate +++ |
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low ++ |
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect |
|
Very Low + |
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
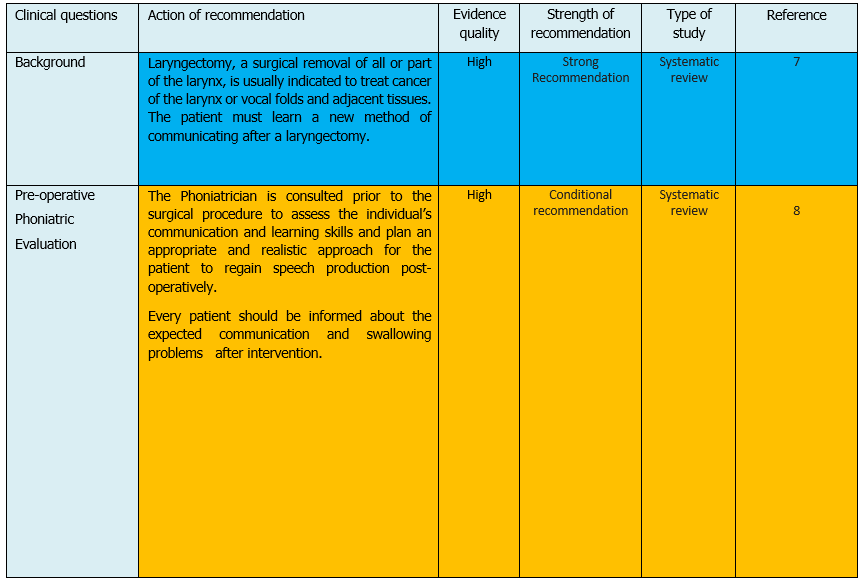
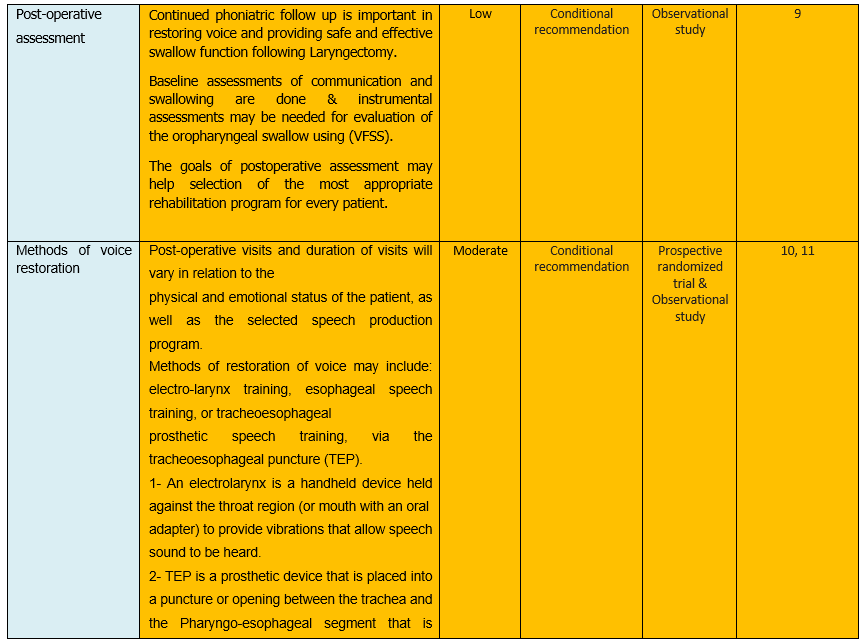
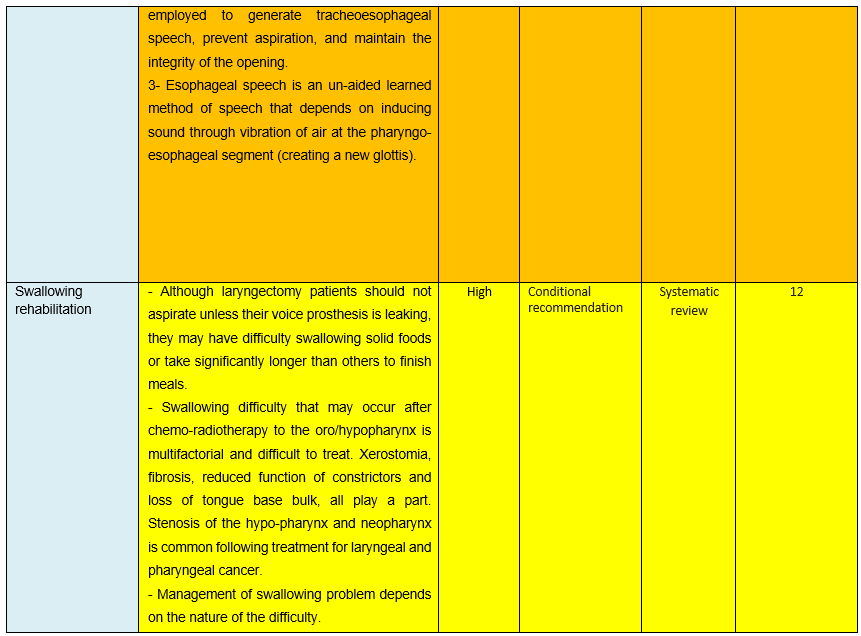
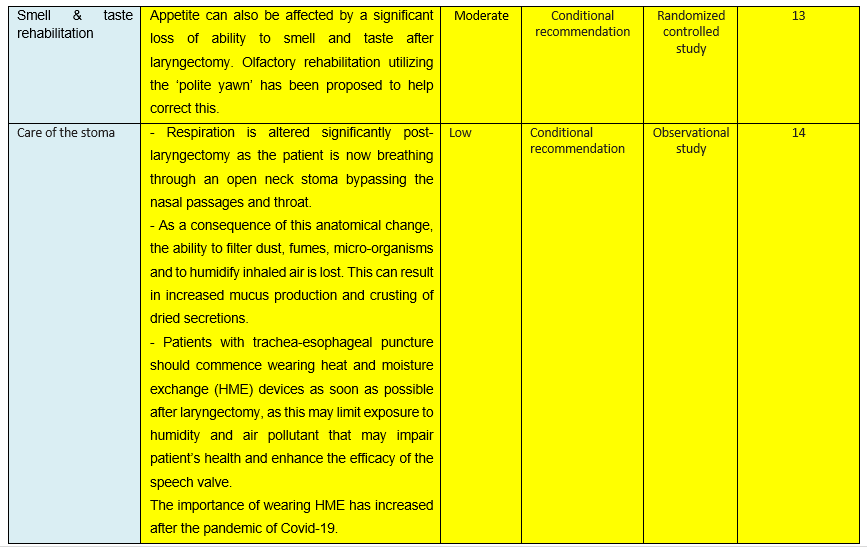
The following statements and flowchart were adapted from the Guidelines from (The ASHA, Speech-Language Pathology Medical Review Guidelines (2015) which received the highest scores as regards the currency, contents, and quality.
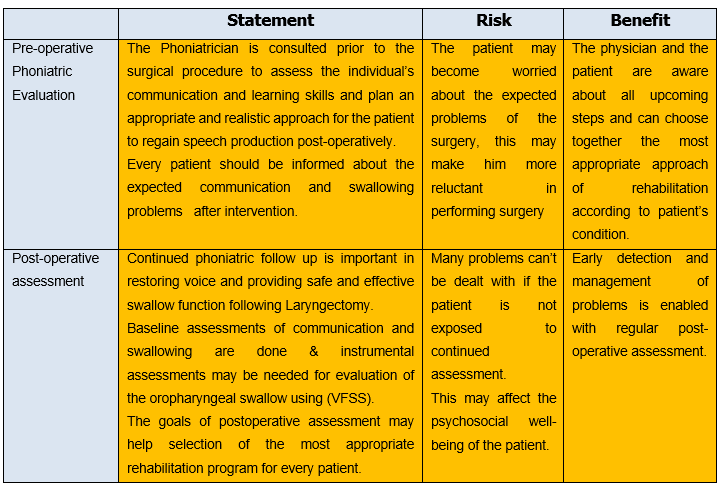
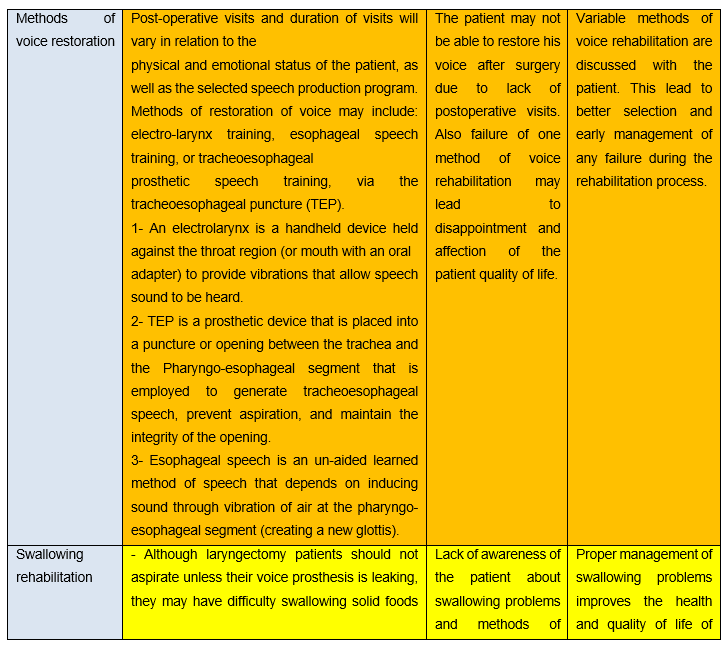
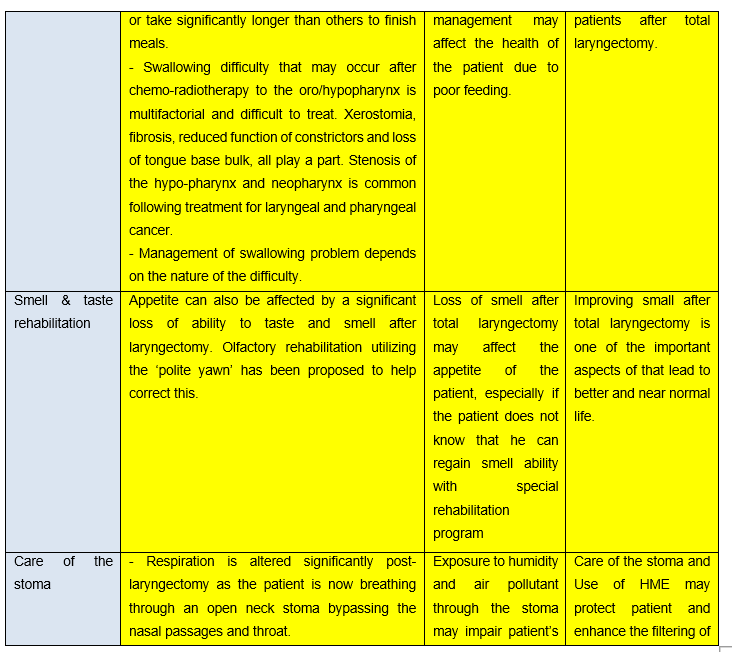
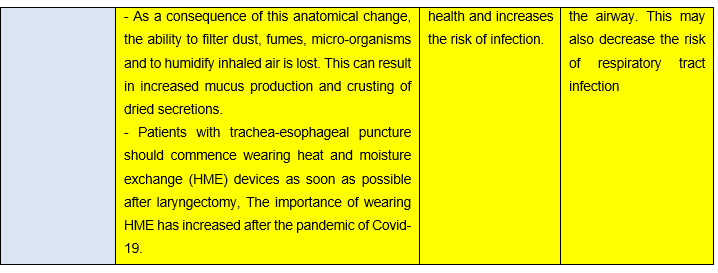
Recommendations statements:

- Research needs
There is a need to conduct randomized controlled trials (RCTs) to determine the efficacy of different methods of rehabilitation of voice, smell and swallowing in patients having total laryngectomies.
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria:
To assess guideline implementation or adherence to recommendations. This is accomplished if the quality of life of patients with total laryngectomy is improved with no increase in the rate of complications.
Clinicians should be able to:
- Acquire full history from the patient/caregiver.
- Perform preoperative and postoperative assessment of voice, swallowing and smell functions and interpret the results.
- Perform and instruct patients about the methods of rehabilitation of voice, swallowing and smell functions after total laryngectomy.
- Choose the appropriate methods which are suitable for every patient conditions.
- Work in a team of related specialties for the best outcome of the patients.
All clinicians should be aware and informed to consider the following:
▪️ It is crucial to perform frequent assessment visits to detect any problem and deal with it in order improve the quality of life of the patients.
▪️ It is necessary to make sure that the patient is able to use and satisfied with the applied method of rehabilitation.
▪️ Red Flags that need an urgent referral for Assessment/ rehabilitation must be taken into consideration.
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. ASHA, Speech-Language Pathology Medical Review Guidelines. 2015, 18.
2. Clarke, P., Radford, K., Coffey, M., & Stewart, M. (2016). Speech and swallow rehabilitation in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. The Journal of Laryngology & Otology, 130(S2), S176–S180.
3. Díaz de Cerio Canduela, P., Arán González, I., Barberá Durban, R., Sistiaga Suárez, A., Tobed Secall, M., & Parente Arias, P. L. (2019). Rehabilitation of the Laryngectomised Patient. Recommendations of the Spanish Society of Otolaryngology and Head and Neck Surgery. Acta Otorrinolaringologica (English Edition), 70(3), 169–174.
4. Papadas, T., Charokopos, N., Karamouzis, M. V., Pierakeas, C., Symeonidi, M., Economou, G., & Goumas, P. (2002). Rehabilitation after laryngectomy: A practical approach and guidelines for patients. Journal of Cancer Education, 17(1), 37–39.
5. Pfister, D. G., Laurie, S. A., Weinstein, G. S., Mendenhall, W. M., Adelstein, D. J., Ang, K., Wolf, G. T. (2006). American Society of Clinical Oncology clinical practice guideline for the use of larynx-preservation strategies in the treatment of laryngeal cancer. Journal of Clinical Oncology, 24(22), 3693–3704.
6. Mustafa R et al. (2013). The GRADE Approach is reproducible in assessing the quality of evidence of quantitative evidence. J Clin Epidemiol. 66(7):736-42.
7. Lagha, A., Chraiet, N., Labidi, S., Rifi, H., Ayadi, M., Krimi, S., Allani, B., Raies, H., Touati, S., Boussen, H., Kochbati, L., & Mezlini, A. (2013). Larynx preservation: What is the best non-surgical strategy? Critical Reviews in Oncology/Hematology, 88(2), 447–458.
8. Fitzgerald E, Perry A (2016), Pre-operative counselling for laryngectomy patients: a systematic review. J Laryngol Otol.130(1), 15-20
9. Coffey M, Tolley N, Howard D, Drinnan M, Hickson M. (2018) An Investigation of the Post-laryngectomy Swallow Using Videofluoroscopy and Fiberoptic Endoscopic Evaluation of Swallowing (FEES) Dysphagia, 33, (3), 369-379
10. Harms, K., Post, W. J., Van De Laan, K. T., Van Den Hoogen, F. J. A., Eerenstein, S. E. J., & Van Der Laan, B. F. A. M. (2011). A prospective randomized multicenter clinical trial of the Provox2 and Groningen Ultra Low Resistance voice prostheses in the rehabilitation of post-laryngectomy patients: A lifetime and preference study. Oral Oncology, 47(9), 895–899.
11. Liao J, (2016). An Acoustic Study of Vowels Produced by Alaryngeal Speakers in Taiwan American Journal of Speech-Language Pathology, 25, 481–492.
12. Mendez, A., Wihlidal, J., Eurich, D., Nichols, A., MacNeil, S., & Seikaly, H. (2022). Validity of functional patient-reported outcomes in head and neck oncology: A systematic review. Oral Oncology, 125, 105701.
13. Gürbüz, D., Kesimli, M. C., Bilgili, A. M., & Durmaz, H. Ö. (2022). Olfactory rehabilitation and olfactory bulb volume changes in patients after total laryngectomy: a prospective randomized study. Brazilian Journal of Otorhinolaryngology, 88(4), 607–612.
14. Boot I., Roth M., Skovgaard R, Kelley A., Tiedemann J., Smedby T. Esmann J. and Vrijhoef H. (2023). CO191 Effectiveness of New Generation Heat and Moisture Exchangers and Adhesives for Laryngectomized Patients in Portugal Value in Health,; 26 (12) S48-S48
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
Annex 1: Guideline Flowchart
Flow chart for rehabilitation of voice & swallowing after
total 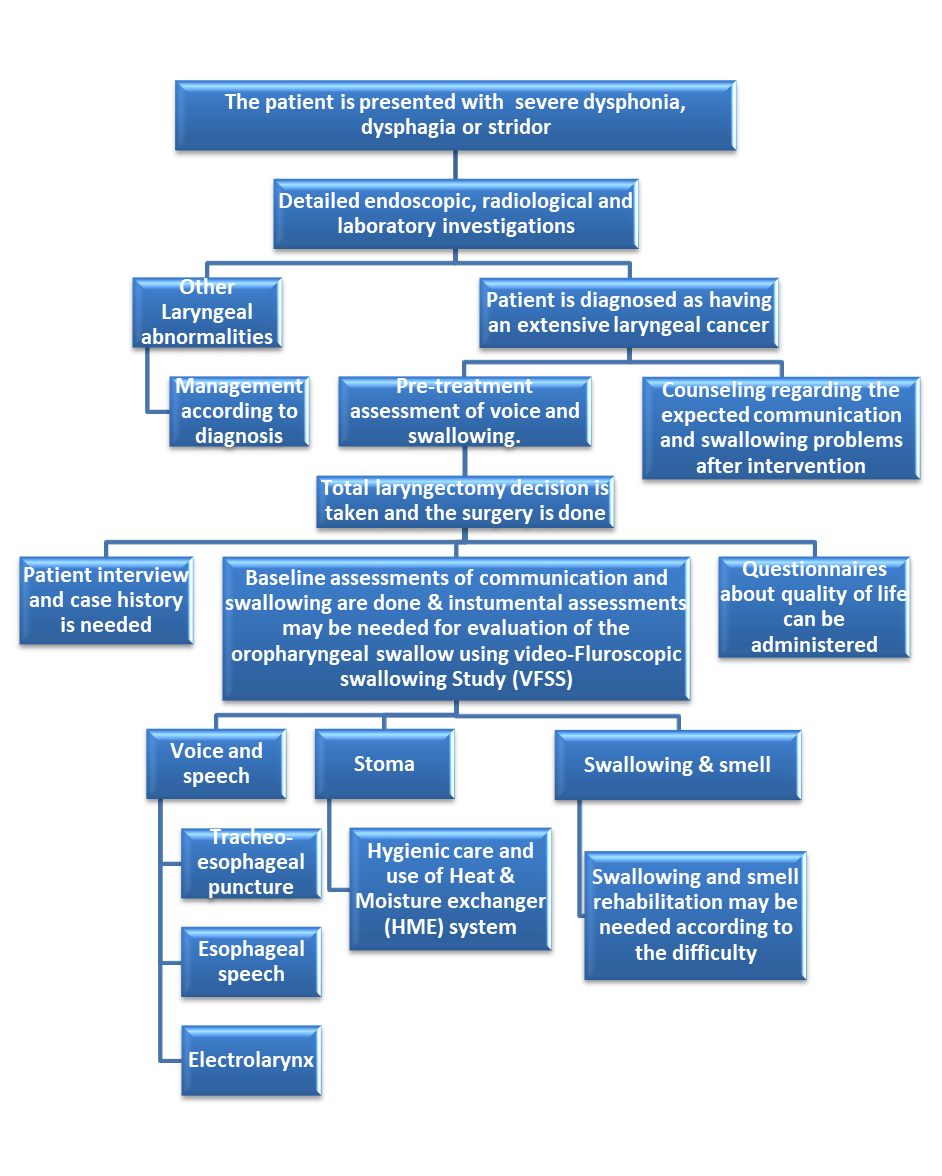
Annex 2:
Tables of appraisal of selected guidelines:
1- Currency (table 1)
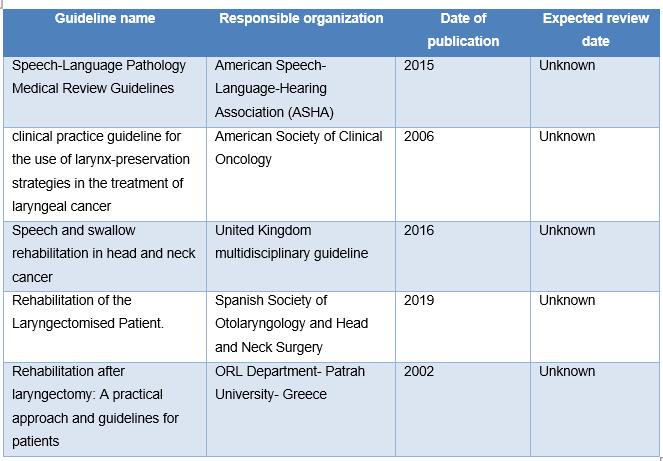
2- Content (table 2)
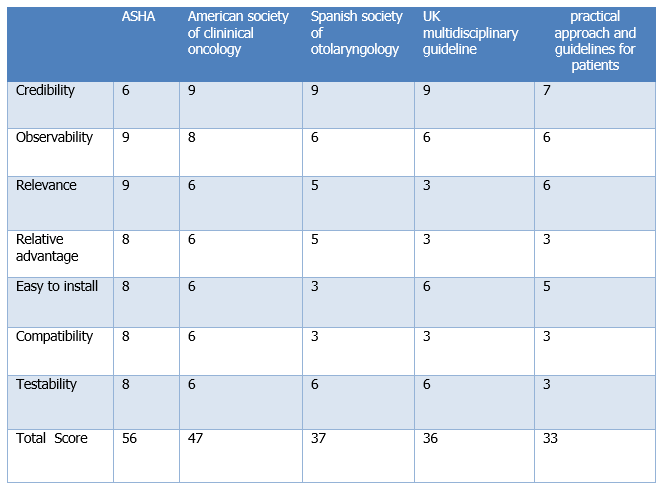
3- Quality (Table 3)

Annex 3: The risks and benefits of added and/or modified statements