Tinnitus (ORL) ECPG
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Tinnitus (ORL) ECPG |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:36 PM |
Description
"last update: 10 June 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled4, Mohamed Ghonaim5, Mahmoud Abdelaziz6, Tarek Ghannoum7, Mahmoud Youssef8
Otology Chief Manager: Ali Mahrous9
Otology Executive Managers: Yasser Shewel10, Mohamed Abdelbadie Salem5
Assembly board: Saad Elzayat11, Mohamed Modather12, Ayman Fouad6, Nabila El Niklawy9, Doaa Abd Elhalem9, Haitham Hassan Elfarargy11, Islam Soltan11
Grading Board (In alphabetical order)
Gamal Abdelfatah13, Ahmed Elkhateeb14, Fathi Erfan6, Ahmed Galal10, Amr Galal15, Sherif Safwat Guindi16, Hisham Hamad6, Adel Khalifa6, Ashraf Lotfy14, Ali Mahrous9, Mahmoud Mandour6, Amir Gorguy Mina10, Ihab Nada13, Mohamed Qotb16, Ashraf Salah13, Yasser Shewel10.
Reviewing Board: Ismail Zohdi1, Ahmed Aboul Wafa12, Ahmed S. Alhamshary17, Wesam Elesawy18.
1-Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2-Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 3-Otorhinolaryngology Department, Faculty of Medicine/ Minia University, 4-Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University, 5-Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 6-Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 7-Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8-Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9-Otorhinolaryngology Department, Faculty of Medicine/ Al Azhar University, 10-Otorhinolaryngology Department, Faculty of Medicine/ Alexandria University, 11-Otorhinolaryngology Department, Faculty of Medicine/ Kafr Elshiekh University, 12-Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 13-Otorhinolaryngology Department, Faculty of Medicine/ Misr University for Science and Technology,
14-Otorhinolaryngology Department, Faculty of Medicine/ Military Medical Academy, 15-Otorhinolaryngology Department/ Hearing and Speech Institute, 16-Otorhinolaryngology Department, Faculty of Medicine/ Fayoum University, 17-Otorhinolaryngology Department, Faculty of Medicine/ Banha University, 18Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Tanta University.- Abbreviations
Qol Quality of life
VS Vestibular schwannoma
CPG Clinical Practice Guideline
GRADE Grading of Recommendations Assessment, Development and Evaluation
MRI Magnetic Resonance Imaging
CT Computed tomography
NR Not Reported
RCT Randomized controlled trial
- Executive Summary
Tinnitus is described as ringing, buzzing, clicking, or pulsating noise perceived only by the patient (subjective) or the examiner and the patient's objective. It may be without aberrant cause (Primary) or due to a specific cause (Secondary) (Strong Recommendation).
Clinicians should perform a targeted history and physical examination at the initial evaluation of a patient with presumed primary tinnitus (Strong Recommendation).
Clinicians must distinguish patients with bothersome tinnitus from patients with no bothersome tinnitus (Strong Recommendation).
Clinicians should distinguish patients with bothersome tinnitus of recent onset from those with persistent symptoms (≥ 6 months) (Strong Recommendation).
Clinicians should obtain a prompt, comprehensive audiological examination in patients with tinnitus that is unilateral, persistent (≥ six months), or associated with hearing difficulties (Strong Recommendation).
Clinicians may obtain an initial comprehensive audiological examination in patients who present with tinnitus (regardless of laterality, duration, or perceived hearing status) (Conditional recommendation).
Clinicians should obtain imaging studies of the head and neck in patients with tinnitus, especially if they have one or more of the following: tinnitus that localises to 1 ear, pulsatile tinnitus, focal neurological abnormalities, or asymmetric hearing loss (Strong Recommendation).
Clinicians should educate patients with persistent, bothersome tinnitus about management strategies (Strong Recommendation).
Clinicians should recommend a hearing aid evaluation for patients with hearing loss and persistent, bothersome tinnitus (Strong Recommendation).
Clinicians may recommend sound therapy to patients with persistent, bothersome tinnitus (Strong Recommendation).
Clinicians should recommend cognitive behavioural therapy to patients with persistent, bothersome tinnitus (Strong Recommendation).
Clinicians can recommend antidepressants, anticonvulsants, or anxiolytics for a primary indication of treating persistent, bothersome tinnitus (Neramexane, Vestipitant alone or in combination with paroxetine, acamprosate, and dietary zinc supplements) (Conditional recommendation).
Clinicians can recommend Ginkgo biloba, melatonin, zinc, or other dietary supplements for treating patients with persistent, bothersome tinnitus (Conditional recommendation).
Clinicians should not prescribe for patients with persistent bothersome tinnitus (Strong Recommendation).
Intratympanic steroids should be used in acute tinnitus, cases with sudden SNHL and cases with SNHL not more than 30 dB, while Intratympanic lidocaine should be tried only for chronic tinnitus (Conditional recommendation).
Surgical treatment is offered for specific causes of tinnitus (e.g. glomus, vestibular schwannoma) (Strong Recommendation).
- Introduction, purpose, scope and audience
➡️Introduction
Tinnitus can occur on one or both sides of the head and can be perceived as coming from within or outside the head. Tinnitus most often occurs in the setting of concomitant sensorineural hearing loss (SNHL), particularly among patients with bothersome tinnitus and no obvious ear pathology. The quality of tinnitus can also vary, with ringing, buzzing, clicking, pulsations, and other noises described by tinnitus patients. In addition, the effects of tinnitus on health-related quality of life (QOL) vary widely, with most patients less severely affected but some experiencing anxiety, depression, and extreme life changes. Patients who have tinnitus accompanied by severe anxiety or depression require prompt identification and intervention, as suicide has been reported in tinnitus patients7 who have coexisting psychiatric illnesses. Most tinnitus is subjective, perceived only by the patient. In contrast, others can perceive objective tinnitus as rare and is not the focus of this guideline.
➡️Scope: The scope of the guideline is the diagnosis and management of bothersome and persistent (lasting 6 months or longer), often with a negative effect on the patient’s QOL.
➡️Target audience: The target audience is any clinician, including non-physicians, involved in managing these patients. Patients with tinnitus will often be evaluated by various healthcare providers, including primary care clinicians, speciality physicians, and non-physician providers such as audiologists and mental health professionals. The target patient population is limited to adults (18 years and older) with primary tinnitus that is persistent and bothersome.
- Methods
➡️Methods of development
Stakeholder Involvement: Individuals who were involved in the development process. Included are the above-mentioned otology chief manager, otology executive manager, assembly board, grading board, and reviewing board.
Information about the target population's experiences was not applicable to this topic.
The adaptation cycle passed over the set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase, including revision and external reviewing.
➡️Search Method
Electronic database searched: PubMed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, and Google Scholar.
➡️Keywords
amplification, hearing aids, hearing loss, quality of life, sound therapy, tinnitus
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Time period searched: from 2014 to 2020.
➡️Results
Seven national otorhinolaryngologists reviewed the guidelines available. Guidelines from the American Academy of Otorhinolaryngology-Head and Neck Surgery gained the highest scores as regards currency, contents and quality. It was graded GRADE by sixteen experts and reviewed by four expert reviewers to improve quality, gather feedback on draft recommendations. The external review was done through a rating scale and open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals and related specialtiesInterpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
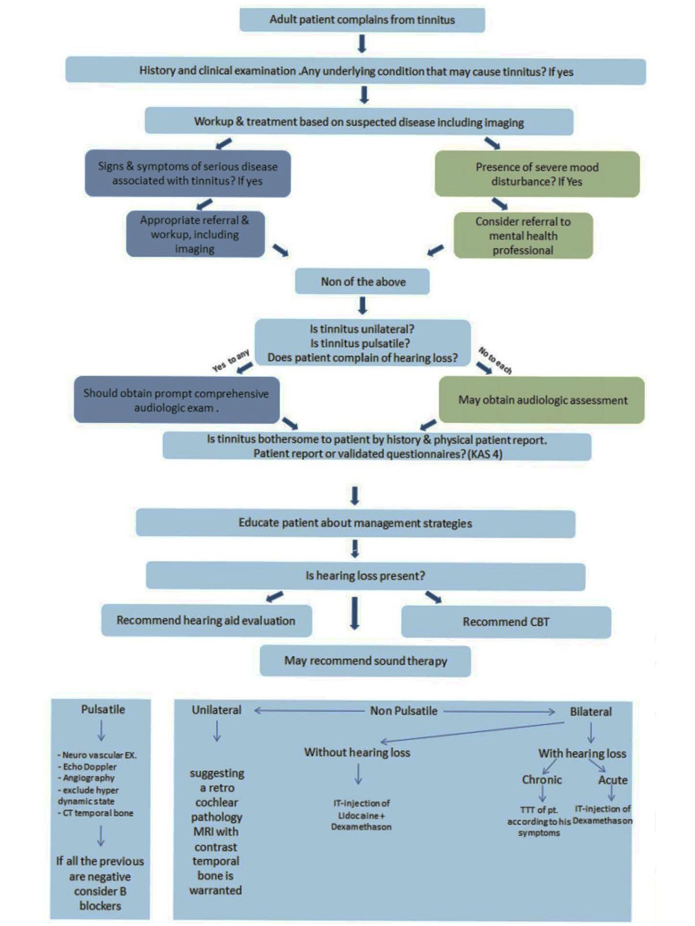
The following statements and flowchart were adapted from the Guidelines from the American Academy of Otorhinolaryngology-Head and Neck Surgery which received the highest scores as regards the currency, contents, and quality.
Recommendations statements
|
Clinical question |
Key action statement |
Strength of recommendation Recommendation |
Level of evidence |
Study typeRefernce |
|
Definition of Tinnitus
|
A condition described as ringing, buzzing, clicking or pulsating noise perceived only by the patient(subjective) or the examiner and the patient objective. it may be without an aberrant cause (Primary) or due to a specific cause (Secondary). |
Strong Recommendation |
Moderate |
RCT8 |
|
History and physical exam
|
Clinicians should perform a targeted history and physical examination at the initial evaluation of a patient with presumed primary tinnitus to identify conditions that if promptly identified and managed may relieve tinnitus. |
Strong Recommendation |
Moderate |
RCT9-11 |
|
Bothersome tinnitus
|
Clinicians must distinguish patients with bothersome tinnitus from patients with no bothersome tinnitus. |
Strong Recommendation |
Moderate |
RCT12,13 |
|
Persistent tinnitus
|
Clinicians should distinguish patients with bothersome tinnitus of recent onset from those with persistent symptoms (≥ 6 months) to prioritise intervention and facilitate discussions about natural history and follow-up care. |
Strong Recommendation |
Moderate |
RCT14 |
|
Prompt Audiologic Examination
|
Clinicians should obtain a prompt, comprehensive audiologic examination in patients with tinnitus that is unilateral, persistent (≥ 6 months), or associated with hearing difficulties. |
Strong Recommendation |
Moderate |
RCT15 |
|
Routine Audiologic Examination
|
Clinicians may obtain an initial comprehensive audiologic examination in patients who present with tinnitus (regardless of laterality, duration, or perceived hearing status). |
Conditional recommendation |
High |
Well-organized RCT16 |
|
Imaging studies
|
Clinicians should obtain imaging studies of the head and neck in patients with tinnitus especially if they have 1 or more of the following: tinnitus that localizes to 1 ear, pulsatile tinnitus, focal neurological abnormalities, or asymmetric hearing loss.( MRI temporal bone with contrast with special emphasis on IAC and CPA to exclude retrocochlear lesion, CT temporal bone to exclude dehiscent jugular vein, dehiscent carotid canal, glomus, or other causes and MRI with contrast and MRA to exclude vascular loop). |
Strong Recommendation |
High |
Systematic review17 |
|
Education and Counselling
|
Clinicians should educate patients with persistent, bothersome tinnitus about management strategies. |
Strong Recommendation |
High |
Systematic review18 |
|
Hearing aid evaluation
|
Clinicians should recommend a hearing aid evaluation for patients with hearing loss and persistent, bothersome tinnitus. |
Strong Recommendation |
High |
Systematic review19 |
|
Sound therapy
|
Clinicians may recommend sound therapy to patients with persistent, bothersome tinnitus. |
Strong Recommendation |
Low |
Observational studies20,21 |
|
Cognitive behavioural therapy (CBT)
|
Clinicians should recommend cognitive behavioural therapy to patients with persistent, bothersome tinnitus. |
Strong Recommendation |
High |
Systematic review22 |
|
Medical therapy
|
Clinicians can recommend antidepressants, anticonvulsants, or anxiolytics for a primary indication of treating persistent, bothersome tinnitus (Neramexane, Vestipitant alone or in combination with paroxetine, acamprosate, and dietary zinc supplements). |
Conditional recommendation
|
Low |
Observational study23 |
|
Dietary supplements
|
Clinicians can recommend Ginkgo biloba, melatonin, zinc, or other dietary supplements for treating patients with persistent, bothersome tinnitus. |
Conditional recommendation |
High |
Well-organized RCT24 |
|
Acupuncture
|
No recommendation can be made regarding the effect of acupuncture in patients with persistent bothersome tinnitus. |
Strong Recommendation |
High |
Systematic review25 |
|
Intratympanic injection
A-Intratympanic steroids
B- Intratympanic lidocaine
C- combined Intratympanic steroids and lidocaine
|
Clinicians should have enough experience with Intratympanic injection. Intratympanic injection should be done once weekly for 3-5 times. Intratympanic steroids should be used in acute tinnitus, cases with sudden SNHL and cases with SNHL not more than 30 dB. Intratympanic lidocaine should be tried only for chronic tinnitus. The combination reduces the irritative effect of lidocaine. |
Conditional recommendation |
Moderate |
RCT26-28 |
|
Surgical treatment of tinnitus
|
Surgical treatment is offered for specific causes of tinnitus (e.g. glomus, vestibular schwannoma). |
Strong Recommendation |
Moderate |
RCT29 |
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria: to assess guideline implementation or adherence to recommendations. This is accomplished if the quality of life of children with AOM is improved with no increase in rate of complications.
Clinicians should be able to:
· Acquire a full history from the patient
· Do audiogram examination
· Exclude other causes of tinnitus
· Is the tinnitus unilateral or bilateral
· Is the tinnitus bothering or not
· Discuss the possible management plans
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1.Henry JA, Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 2005;48:1204-1235.
2. Hoffman HJ, Reed GW. Epidemiology of tinnitus. In: Snow JB, ed. Tinnitus: Theory and Management. Lewiston, NY: BC Decker; 2004:16-41.
3. Henry JA, Zaugg TL, Myers PJ, Schechter MA. The role of audiologic evaluation in progressive audiologic tinnitus management. Trends Amplif. 2008;12:170-187.
4. Vital and Health Statistics: Current Estimates from the National Health Interview Survey, 1994. Series 10: Data from the National Health Survey No. 193; US Department of Health and Human Services Public Health Service, CDC, National Center for Health Statistics, DHHS Publication No. (PHS) 96-1521.
5. Nondahl DM, Cruickshanks KJ, Huang GH, et al. Tinnitus and its risk factors in the Beaver Dam Offspring Study. Int J Audiol. 2011;50(5):313-320.
6. US Department of Veterans Affairs, ed. Annual Benefits Report: Fiscal Year 2012. Washington, DC: Department of Veterans Affairs; 2013.
7. Lewis JE, Stephens SDG, McKenna L. Tinnitus and suicide. Clin Otolaryngol Allied Sci. 1994;19:50-54.
8-Zoger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics.
2006;47:282-288.
9-Roland PS, Smith TL, Schwartz SR, et al. Clinical practice guideline: cerumen impaction. Otolaryngol Head Neck Surg.
2008;139(suppl):S1-S21.
10-Bast F, Mazurek B, Schrom T. Effect of stapedotomy on preoperative tinnitus and its psychosomatic burden. Auris Nasus
Larynx. 2013;40:530-533.
11-Kim DK, Park SN, Kim MJ, Lee SY, Park KH, Yeo SW. Tinnitus in patients with chronic otitis media before and after middle ear surgery. Eur Arch Otorhinolaryngol. 2011;268:1443-1448.
12-Tyler RS, Baker LJ. Difficulties experienced by tinnitus sufferers. J Speech Hear Disord. 1983; 48:150-154.
13- Lasisi AO, Gureje O. Prevalence of insomnia and impact on quality of life among community elderly subjects with tinnitus. Ann Otol Rhinol Laryngol. 2011;120:226-230.
14- Shim HJ, Song SJ, Choi AY, Hyung Lee R, Yoon SW. Comparison of various treatment modalities for acute tinnitus. Laryngoscope.2011;121(12):2619-2625.
15- Stachler RJ, Chandrasekhar SS, Archer SM, et al. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146(3 suppl):S1-S35.
16- Coles RRA. Classification of causes, mechanisms of patient disturbance, and associated counselling. In: Vernon JA, Moller AR, eds. Mechanisms of Tinnitus. Boston, MA: Allyn & Bacon; 1995:11-19.
17- Fortnum H, O’Neill C, Taylor R, et al. The role of magnetic resonance imaging in identifying suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history. Health Technol Assess. 2009;13(18):iii-iv, ix-xi, 1-154.
18- Nyenhuis N, Zastrutzki S, Weise C, Jager B, Kroner-Herwig B. Efficacy of minimal contact interventions for acute tinnitus: a randomised controlled study. Cogn Behav Ther. 2013; 42:127- 138.
19- Trotter MI, Donaldson I. Hearing aids and tinnitus therapy: a 25-year experience. J Laryngol Otol. 2008;122:1052-1056.
20-Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. New York, NY: Cambridge University Press; 2004.
21-Jastreboff PJ, Jastreboff MM. Tinnitus retraining therapy. In: Snow JB, ed. Tinnitus: Theory and Management. Hamilton, London: BC Decker; 2004:310-313.
22- Hesser H, Weise C, Westin VZ, Andersson G. A systematic review and meta-analysis of randomised controlled trials of cognitive-behavioral therapy for tinnitus distress. Clin Psychol Rev. 2011;31:545-553.
23- Pichora-Fuller MK, Santaguida P, Hammill A, et al. Evaluation and treatment of tinnitus: comparative effectiveness. Comparative Effectiveness Review No. 122. (Prepared by the McMaster University Evidence-Based Practice Center under Contract No. 290-2007-10060-I.) AHRQ Publication No. 13-EHC110-EF. Rockville, MD: Agency for Healthcare Research and Quality; August 2013. www.effectivehealthcare.ahrq.gov/reports/final
24- Rejali D, Sivakumar A, Balaji N. Ginkgo biloba does not benefit patients with tinnitus: a randomized placebo-controlled double-blind trial and meta-analysis of randomized trials. Clin Otolaryngol Allied Sci. 2004;29:226-231.
25- Kim JI, Choi JY, Lee DH, Choi TY, Lee MS, Ernst E. Acupuncture for the treatment of tinnitus: a systematic review of randomized clinical trials. BMC Complement Altern Med. 2012;12:97.
26- Choi SJ, Lee JB, Lim HJ, et al. Intratympanic dexamethasone injection for refractory tinnitus: prospective placebo-controlled study. Laryngoscope. 2013;123:2817-2822.
27- Elzayat S, Ragab S, Eisa M, Amer M, Mandour MF, Mehraz M. Evaluation of Adding Lidocaine to Dexamethasone in the Intra-tympanic Injection for Management of Tinnitus: A Prospective, Randomized, Controlled Double-blinded Trial. Int Tinnitus J. 2018;22(1):54-59. Published 2018 Jun 1. doi:10.5935/0946-5448.20180009
28- Elzayat S, El-Sherif H, Hegazy H, Gabr T, El-Tahan AR. Tinnitus: Evaluation of Intratympanic Injection of Combined Lidocaine and Corticosteroids. ORL J Otorhinolaryngol Relat Spec. 2016;78(3):159-166. doi:10.1159/000445774
29- Van Gompel JJ, Patel J, Danner C, et al. Acoustic neuroma observation associated with an increase in symptomatic tinnitus: results of the 2007-2008 Acoustic Neuroma Association survey [published online June 21, 2013]. J Neurosurg.
- Annexes
Editorial Independence:
· This guideline was developed without any external funding.
· All the guideline development group members have declared that they do not have any competing interests.
Annex 1: A flow chart of the Tinnitus guideline.
Annex 2: Assessment of Currency Table
|
Number |
Name |
Responsible organization |
Date of Publication |
Expected Review Date |
Date of original details in the references |
|
1 |
Practice Guidance: Fitting of combination hearing aids for subjects with tinnitus |
British Society of Audiology |
2020 |
NR |
recent references |
|
2 |
NICE Guideline |
National Institute for Health and Care Excellence |
2020 |
NR |
recent references |
|
3 |
A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment |
European |
2019 |
NR |
recent references |
|
4 |
Clinical practice guideline: tinnitus |
AAO-HNSF |
2014 |
NR |
Not recent references |
|
5 |
Clinical practice guidelines for diagnosis and treatment of chronic tinnitus in Japan |
Oto-Rhino-Laryngological Society of Japan |
2019 |
NR |
recent references |
Annex 3: Assessment of Content Table
|
Score Items (each to be given score from (1-9) |
British Society Of Audiology (2020) |
NICE Guideline
|
European guideline |
AAO-HNSF |
Japanese guidelines |
|
Credibility |
9 |
9 |
9 |
9 |
9 |
|
Observability |
8 |
7 |
8 |
9 |
7 |
|
Relevance |
9 |
9 |
7 |
9 |
9 |
|
Relative advantage |
8 |
5 |
8 |
9 |
8 |
|
Easy to Install |
9 |
7 |
9 |
9 |
6 |
|
Compatibility |
8 |
7 |
7 |
8 |
7 |
|
Testability |
5 |
7 |
- |
9 |
7 |
|
Total score |
56 |
51 |
48 |
62 |
53 |
Annex 4: Assessment of Quality Table
|
Domain |
British Society Of Audiology (2020) |
NICE Guideline
|
European guideline |
AAO-HNSF |
Japanese guidelines |
|
Transparency |
A |
A |
A |
A |
A |
|
Conflict of interest |
A |
A |
A |
A |
A |
|
Development group |
A |
A |
A |
A |
A |
|
Systematic review |
A |
A |
A |
A |
A |
|
Grading of evidence |
A |
A |
A |
A |
A |
|
Recommendation |
A |
A |
A |
A |
A |
|
External review |
A |
A |
A |
A |
A |
|
Updating |
B |
B |
B |
C |
A |
Annex 5: The risks and benefits of added and/or modified statements
|
Statement |
Risk |
Benefit |
|
Imaging studies |
No risk |
We focused on the role of imaging studies to find the primary cause of tinnitus, which may improve the management outcomes. |
|
Medical therapy |
Side effects of the used medications. |
This may improve the outcomes, especially in specific situations such as the associated depression of somatosensory manifestations. |
|
Intratympanic injection |
Tympanic membrane residual perforation |
It may be helpful in severe and resistant cases. |


















