Cerebrospinal fluid rhinorrhea (ECPG)
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Cerebrospinal fluid rhinorrhea (ECPG) |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:40 PM |
Description
"last update: 10 June 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdelaziz,6 Tarek Ghannoum,7 Mahmoud Youssef8
Rhinology Chief Manager: Ashraf Khaled4
Rhinology Executive Manager: Ahmed Elfarouk,1 Alaa Ghita,9 Mohamed Elsharnouby,10 Hossam Elsherif6
Assembly Board: Ismail Elnashar11, Mostafa A. El Taher12, Ashraf Elhosini11, Tamer Orabi11
Grading Board: (In alphabetical order)
Ibrahim Abd-elshafy2, Sameh Amin13, Diaa Elhennawi14, Mohamed Fawwaz,4 Mohamed Gamea15, Amr Gouda10, Baliegh Hamdy3,
Islam R. Herzalla11, Sayed Kaddah16, Ashraf Khaled,4 Mohamed Qotb13, Ahmad Ragab2, Ramez Reda4, Mohamed Osama Tamoum6, Hasan Abaza18, Hazem Tantawy19
Reviewing Board: Yaser khafagy5, Alaa Ghita9, Ahmed Ali Ibrahim17
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 3Otorhinolaryngology Department, Faculty of Medicine/ Minia University, 4Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 6Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Otorhinolaryngology Department, Faculty of Medicine/ Military Medical Academy, 10Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 11Otorhinolaryngology Department, Faculty of Medicine/ Zagazig University, 12Otorhinolaryngology Department, Faculty of Medicine/ Sohag University, 13Otorhinolaryngology Department, Faculty of Medicine/ Fayoum University, 14Otorhinolaryngology Department, Faculty of Medicine/ Suez Canal University, 15Otorhinolaryngology Department, Faculty of Medicine/ Misr University for Science and Technology, 16Otorhinolaryngology Department, Faculty of Medicine/ Al Azhar University, 17Otorhinolaryngology Department, Faculty of Medicine/Alexandria University, 18Neurosurgery department, Faculty of Medicine, Zagazig University, 19Radiology department, Zagazig University.
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
- Abbreviations
ESBS Endoscopic skull base surgery
CSF Cerebrospinal fluid
CPG Clinical Practice Guideline
GRADE Grading of Recommendations Assessment, Development and Evaluation
CT Computerized tomography
HRCT High resolution CT
MRI Magnetic Resonance Imaging
NR Not Reported
ICP Intracranial pressure
IIH Idiopathic intracranial hypertension
RCT Randomized controlled trial
LD Lumber drain
VP Ventriculo-peritoneal
- Executive Summary
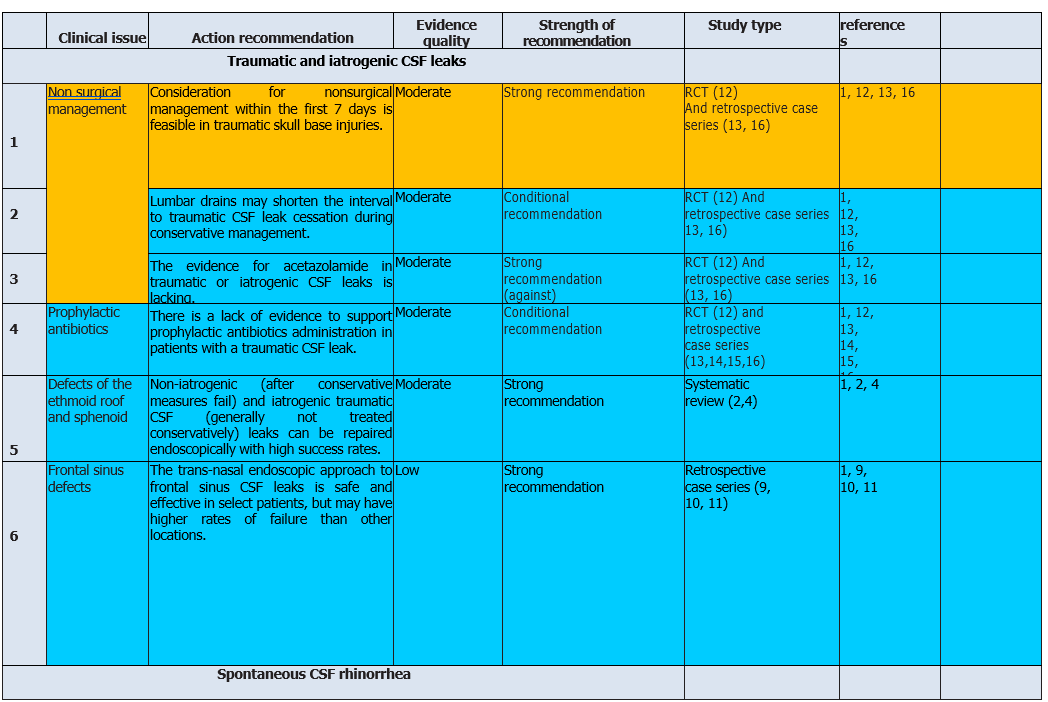
Traumatic and iatrogenic CSF leaks
Consideration for nonsurgical management within the first 7 days is feasible in traumatic skull base injuries (strong recommendation)
Lumbar drains may shorten the interval to traumatic CSF leak cessation during conservative management (conditional recommendation)
The evidence for acetazolamide in traumatic or iatrogenic CSF leaks is lacking (strong recommendation).
There is a lack of evidence to support prophylactic antibiotics administration in patients with a traumatic CSF leak (conditional recommendation).
For defects in the ethmoid roof and sphenoid, Non-iatrogenic (after conservative measures fail) and iatrogenic traumatic CSF (generally not treated conservatively) leaks can be repaired endoscopically with high success rates (strong recommendation)
For frontal sinus defects, the transnasal endoscopic approach to frontal sinus CSF leaks is safe and effective in select patients, but may have higher rates of failure than other locations (strong recommendation).
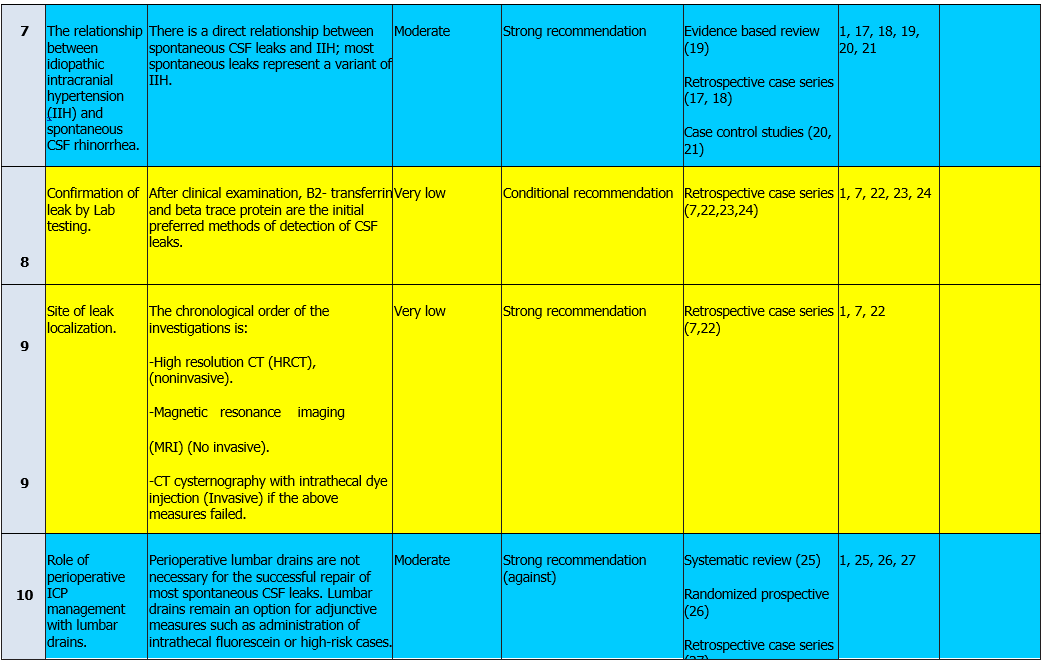
Spontaneous CSF rhinorrhea
There is a direct relationship between spontaneous CSF leaks and IIH; most spontaneous leaks represent a variant of IIH (strong recommendation).
After clinical examination, B2- transferrin and beta trace protein are the initial preferred methods of detection of CSF leaks (conditional recommendation).
For site of leak detection, High resolution CT (HRCT) and Magnetic resonance imaging (MRI) are the initial imaging modalities (non invasive). CT cysternography with intrathecal dye injection (Invasive) may be required if the previous measures failed to determine the site of leak (conditional recommendation).
Perioperative lumbar drains are not necessary for the successful repair of most spontaneous CSF leaks. Lumbar drains remain an option for adjunctive measures such as administration of intrathecal fluorescein or high-risk cases (strong recommendation) (Recommendation against except in high risk cases).
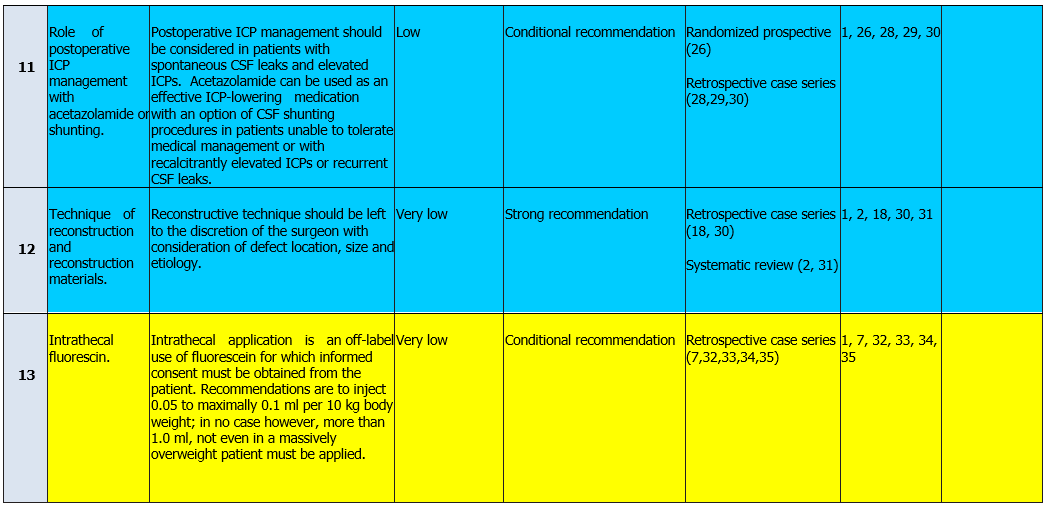
Postoperative ICP management should be considered in patients with spontaneous CSF leaks and elevated ICPs. Acetazolamide can be used as an effective ICP-lowering medication with an option of CSF shunting procedures in patients unable to tolerate medical management or with recalcitrantly elevated ICPs or recurrent CSF leaks (conditional recommendation).
Reconstructive technique should be left to the discretion of the surgeon with consideration of defect location, size and etiology (strong recommendation).
Intrathecal application is an off-label use of fluorescein for which informed consent must be obtained from the patient (conditional recommendation).- Introduction, scope and audience
➡️Introduction
➡️Scope: The scope of the guideline is the diagnosis and management of CSF rhinorrhea of various causes and locations of the skull base. The guidelines are intended to specify the recommended diagnostic tools and the recommended management options in different situation with the aim of raising the standard of care and unifying methods of management among practitioners.
➡️Target audience: ENT, neurosurgical and neurology physicians involved in the management of skull base pathologies.
- Methods
➡️Methods of development
Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Rhinology Chief Manager, Rhinology Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
➡️Search Method
Electronic database searched:
Pubmed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar
➡️Keywords
CSF rhinorrhea, Endoscopic skull base surgery, skull base repair
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
Time period searched: from 2009 to 2019.
➡️Results
The guidelines were chosen and formulated by the assembly team which consisted of four national otorhinolaryngologists. The International Consensus Statement on Allergy and Rhinology: Endoscopic Skull Base Surgery (ICAR: ESBS), 2019 gained the highest scores as regards currency, contents and quality.
It was graded (GRADE) by 17 experts and reviewed by three expert reviewers to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
➡️Setting: primary, secondary and tertiary care centers & hospitals and related specialties.
Interpretation of strong and conditional recommendation for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not. |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations,
The following statements were adapted from The International Consensus Statement on Allergy and Rhinology: Endoscopic Skull Base Surgery (ICAR: ESBS), 2019 which received the highest scores as regards the currency, contents, and quality.
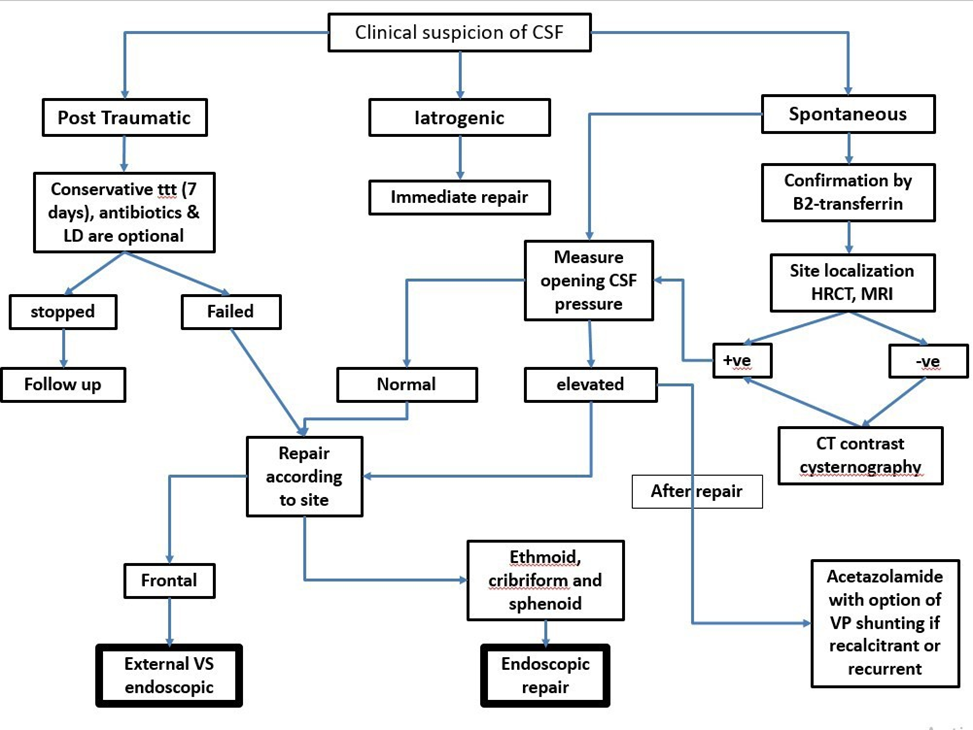
Recommendations statements
The flowchart was developed from the assembly board to simplify the statements and putting it in a practical way. The flowchart has the same information contained in the statements.
- Implementation considerations
Research needs
▪️ There is a need to conduct randomized controlled trials (RCTs) to determine the safety of using intrathecal fluorescein in localizing skull base defect.
▪️ There is a need to conduct RCTs to compare between grafts and vascularized flaps in repair of skull base defects.
▪️ There is a need to conduct RCTs to detect the safety and efficacy of repair of frontal sinus leaks using the endoscopic technique.
▪️ More studies are needed to determine the ideal duration of conservative Nonsurgical management options in traumatic and iatrogenic CSF leaks.
▪️ More studies are needed to evaluate the effect and optimal duration of medical management of idiopathic increase intracranial tension
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria:
Clinicians should be able to
- Take full history and perform clinical examination including endoscopic assessment
- Follow the order of investigation from starting by the non-invasive (CT and MRI) and resorting to the invasive (intrathecal contrast) only in case of need
- Be able to detect clinical and radiological criteria of increased intracranial pressure
- Make good consultation and referral if the setting and expertise are insufficient at his place of practice.
- Follow up and detect symptoms and signs of complications specifically meningitis and pneumocephalus
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. Wang E, Zanation A, Gardner P, et al. ICAR: endoscopic skull-base surgery. International Forum of Allergy & Rhinology. 2019; 9(S3).
2. Psaltis A, Schlosser R, Banks C, et al. A Systematic Review of the Endoscopic Repair of Cerebrospinal Fluid Leaks. Otolaryngology-Head and Neck Surgery. 2012;147(2): 96–203.
3. Bedrosian J, Anand V, Schwartz T. The Endoscopic Endonasal Approach to Repair of Iatrogenic and Noniatrogenic Cerebrospinal Fluid Leaks and Encephaloceles of the Anterior Cranial Fossa. World Neurosurgery. 2014;82[6S]:S86-S94.
4. Sharma S, Kumar G, Bal J, et al. Endoscopic repair of cerebrospinal fluid rhinorrhoea. European Annals of Otorhinolaryngology, Head and Neck diseases. 2016;133(3):187-90.
5. Konuthula N, Khan M, Del Signore A, et al. A systematic review of secondary cerebrospinal fluid leaks. Am J Rhinol Allergy. 2017;31(6):48-56.
6. Sumaily I. Current Approach to Cerebrospinal Fluid Rhinorrhea: Diagnosis and Management. J Otolaryngol ENT Res: 2017;7(1):00191.
7. Lund V, Stamberger H, NicolaI P, et al. European Position Paper on Endoscopic Management of Tumours of the Nose, Paranasal Sinuses and Skull Base. Rhinology, 2019: supplement 22.
8. American Academy of Pediatrics Steering Committee on Quality Improvement and Management. Classifying recommendations for clinical practice guidelines. Pediatrics. 2004; 114:874-877.
9. Woodworth BA, Schlosser RJ, Palmer JN. Endoscopic repair of frontal sinus cerebrospinal fluid leaks. J Laryngol Otol. 2005;119:709-713.
10. Chaaban MR, Conger B, Riley KO, Woodworth BA. Transnasal endoscopic repair of posterior table fractures. Otolaryngol Head Neck Surg. 2012; 147:1142-1147.
11. Jones V, Virgin F, Riley K, Woodworth BA. Changing paradigms in frontal sinus cerebrospinal fluid leak repair. Int Forum Allergy Rhinol. 2012; 2:227- 232.
12. Albu S, Florian IS, Bolboaca SD. The benefit of early lumbar drain insertion in reducing the length of CSF leak in traumatic rhinorrhea. Clin Neurol Neurosurg. 2016; 142:43-47.
13. Bell RB, Dierks EJ, Homer L, Potter BE. Management of cerebrospinal fluid leak associated with craniomaxillofacial trauma. J Oral Maxillofac Surg. 2004; 62:676-684.
14. Gosal JS, Gurmey T, Kursa GK, Salunke P, Gupta SK. Is acetazolamide really useful in the management of traumatic cerebrospinal fluid rhinorrhea? Neurol India. 2015;63:197-201.
15. Abrishamkar S, Khalighinejad N, Moein P. Analysing the effect of early acetazolamide administration on patients with a high risk of permanent cerebrospinal fluid leakage. Acta Med Iran. 2013; 51:467-471.
16. Yilmazlar S, Arslan E, Kocaeli H, et al. Cerebrospinal fluid leakage complicating skull base fractures: analysis of 81 cases. Neurosurg Rev. 2006; 29:64-71.
17. Schlosser RJ, Bolger WE. Management of multiple spontaneous nasal meningoencephaloceles. Laryngoscope. 2002; 112:980-985.
18. Banks CA, Palmer JN, Chiu AG, O’Malley BW Jr, Woodworth BA, Kennedy DW. Endoscopic closure of CSF rhinorrhea: 193 cases over 21 years. Otolaryngol Head Neck Surg. 2009; 140:826-833.
19. Wall M. Idiopathic intracranial hypertension. Neurol Clin. 2010; 28:593-617.
20. Aaron GP, Illing E, Lambertsen Z, et al. Enlargement of Meckel’s cave in patients with spontaneous cerebrospinal fluid leaks. Int Forum Allergy Rhinol. 2017; 7:421-424.
21. Psaltis AJ, Overton LJ, Thomas WW 3rd, Fox NF, Banks CA, Schlosser RJ. Differences in skull base thickness in patients with spontaneous cerebrospinal fluid leaks. Am J Rhinol Allergy. 2014; 28:e73-e79.
22. Oakley GM, Alt JA, Schlosser RJ, Harvey RJ, Orlandi RR. Diagnosis of cerebrospinal fluid rhinorrhea: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2016 ;6:8-16.
23. Wise SK, Schlosser RJ. Evaluation of spontaneous nasal cerebrospinal fluid leaks. Curr Opin Otolaryngol Head Neck Surg. 2007; 15:28-34.
24. Arrer E, Meco C, Oberascher G, Piotrowski W, Albegger K, Patsch W. beta-Trace protein as a marker for cerebrospinal fluid rhinorrhea. Clin Chem. 2002; 48(6 Pt 1):939-941.
25. Ahmed OH, Marcus S, Tauber JR, Wang B, Fang Y, Lebowitz RA. Efficacy of perioperative lumbar drainage following endonasal endoscopic cerebrospinal fluid leak repair. Otolaryngol Head Neck Surg. 2017; 156:52-60.
26. Albu S, Emanuelli E, Trombitas V, Florian IS. Effectiveness of lumbar drains on recurrence rates in endoscopic surgery of cerebrospinal fluid leaks. Am J Rhinol Allergy. 2013; 27:e190-e194.
27. Meco C, Arrer E, Oberascher G. Efficacy of cerebrospinal fluid fistula repair: sensitive quality control using the beta-trace protein test. Am J Rhinol. 2007; 21:729-736.
28. Chaaban MR, Illing E, Riley KO, Woodworth BA. Acetazolamide for high intracranial pressure cerebrospinal fluid leaks. Int Forum Allergy Rhinol. 2013; 3:718-721.
29. Teachey W, Grayson J, Cho DY, Riley KO, Woodworth BA. Intervention for elevated intracranial pressure improves success rate after repair of spontaneous cerebrospinal fluid leaks. Laryngoscope. 2017; 127:2011-2016.
30. Campbell RG, Farquhar D, Zhao N, Chiu AG, Adappa ND, Palmer JN. Cerebrospinal fluid rhinorrhea secondary to idiopathic intracranial hypertension: long-term outcomes of endoscopic repairs. Am J Rhinol Allergy. 2016; 30:294-300.
31. Hegazy HM, Carrau RL, Snyderman CH, Kassam A, Zweig J. Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: a meta-analysis. Laryngoscope. 2000; 110:1166-1172.
32. Tahir MZ, Khan MB, Bashir MU, Akhtar S, Bari E. Cerebrospinal fluid rhinorrhea: an institutional perspective from Pakistan. Surg Neurol Int. 2011; 2:174.
33. Demarco RC, Tamashiro E, Valera FC, AnselmoLima WT. Use of a hypodense sodium fluorescein solution for the endoscopic repair of rhinogenic cerebrospinal fluid fistulae. Am J Rhinol. 2007; 21:184-186.
34. Lanza DC, O’Brien DA, Kennedy DW. Endoscopic repair of cerebrospinal fluid fistulae and encephaloceles. Laryngoscope. 1996; 106(9 Pt 1):1119-1125.
35. Placantonakis DG, Tabaee A, Anand VK, Hiltzik D, Schwartz TH. Safety of low-dose intrathecal fluorescein in endoscopic cranial base surgery. Neurosurgery. 2007;61(3 Suppl):161-165; discussion 165-166.
- Annexes
Editorial Independence:
▪️ This guideline was developed without any external funding.
▪️ All the guideline development group members have declared that they do not have any competing interests.
Annex 1: Guideline Flowchart
Annex 2: Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
|
No |
Guidelines name |
year of pblication |
The Organizaion |
Age of Demography |
|
1 |
ICAR (international consensus statement allergy and rhinology)- ESBS |
2019 |
the American Rhinologic Society and the American Academy of Otolaryngic Allergy |
Adult and children |
|
2 |
Europian position paper on endoscopic management of tumors of the nose, PNS and skull base |
2015 |
European Rhinologic Society |
Adult and children |
|
3 |
A systematic review of secondery CSF rhinorrhea (2017) |
2017 |
Department of Otolaryngology—Head and Neck Surgery, Mount Sinai Medical Center, |
Adult and children |
|
4 |
The endoscopic endonasal repair for iatrogenic and non iatrigenic CSF leaks and encephaloceles of the anterior cranial fossa (2014 |
2014 |
Weill Cornell Medical College, New York Presbyterian Hospital, New York, New York, USA |
Adult and children |
(Table 1): assessment of currency table
|
Criteria |
Guideline A (ICAR-ESBS) |
Guideline B (EPOS) |
Guideline C A systematic review of secondery CSF rhinorrhea (2017), Mount Sinai Medical Center |
Guideline D The endoscopic endonasal repair for iatrogenic and non iatrigenic CSF leaks and encephaloceles of the anterior cranial fossa (2014) Weill Cornell Medical College, New York |
|
Credibility |
9 |
8 |
7 |
7 |
|
Observability |
9 |
8 |
7 |
7 |
|
Relevance |
9 |
9 |
7 |
6 |
|
Relative advantage |
9 |
6 |
6 |
7 |
|
Easy to install and understand |
9 |
8 |
8 |
7 |
|
Compatibility |
8 |
8 |
8 |
8 |
|
Testability |
8 |
8 |
8 |
8 |
|
Total Score |
61 |
55 |
51 |
52 |
(Table 2) assessment of content table
|
Guideline A (ICAR-ESBS) |
Guideline B (EPOS) |
Guideline C A systematic review of secondery CSF rhinorrhea (2017), Mount Sinai Medical Center |
Guideline D The endoscopic endonasal repair for iatrogenic and non iatrigenic CSF leaks and encephaloceles of the anterior cranial fossa (2014Weill Cornell Medical College, New York |
|
|
Transparency |
A |
A |
B |
B |
|
Conflict of interest |
B |
B |
B |
B |
|
Development group |
B |
C |
C |
c |
|
Systematic revie |
A |
A |
A |
B |
|
Grading of evidence |
A |
A |
B |
B |
|
recommendation |
A |
B |
C |
C |
|
External review |
B |
NR |
NR |
NR |
|
updating |
B |
B |
B |
B |
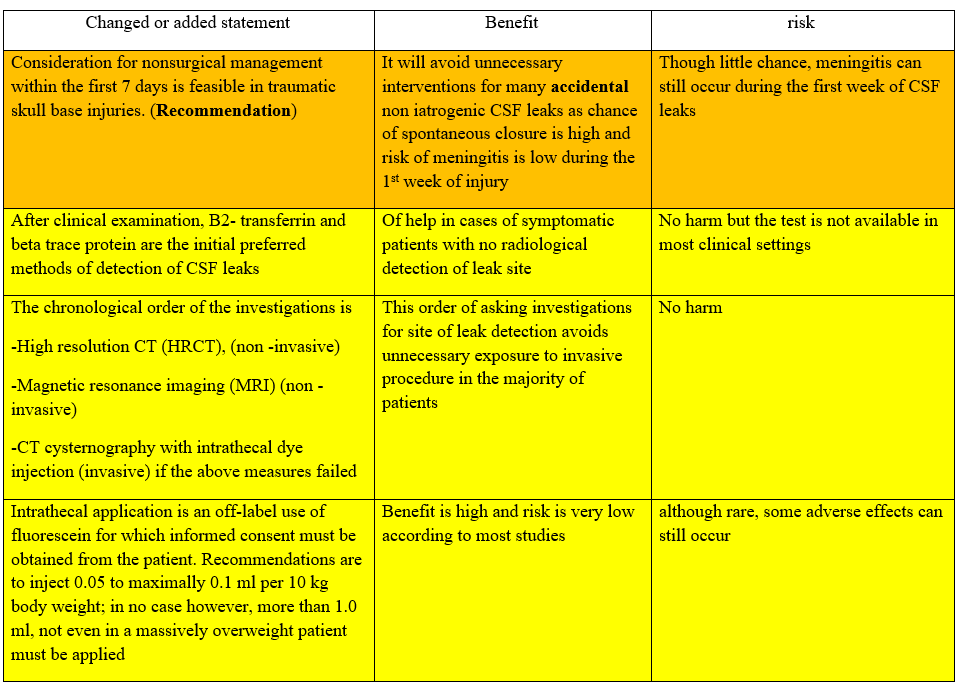
Annex 3: The risks and benefits of added and/or modified statements