Vestibular Rehabilitation for Peripheral Vestibular Hypofunction
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Vestibular Rehabilitation for Peripheral Vestibular Hypofunction |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:07 PM |
Description
"last update: 9 June 2024"
Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdel Aziz,6 Tarek Ghanoum,7 Mahmoud Yousef8
Assembly Board: Soha Mekki,9 Abir Omara,10 Sara Fawzan11
Grading Board (In alphabetical order): Abeir Dabbous,7 Enass Sayed,12 Enaas Kolkaila,13 Eman Mostafa Basiouny,14 Mona Elakkad,15Mona Mourad,11 Mohamed Salama,12 Mostafa Youssif,16 Naema Ismail,17 Nashwa Nada,13 Reham Rafei,15 Rabab Koura,14 Radwa Mahmoud,16Salwa Mahmoud,10 Tarek El Dessouky,14 Trandil ElMehallawi13, Magdy ElHossieny Ebrahim Elewa18
Reviewing Board: Alaa Abousetta,19 Mohamed El-Badry,20 Nagwa Hazzaa21
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/ Menofia University, 3Otorhinolaryngology Department, Faculty of Medicine/ Menia University, 4Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/Mansoura University, 6Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 7Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Zagazig University, 10 Audiovestibular Medicine Unit, Otorhinolaryngology Department/ Hearing and Speech Institute, 11Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/Alexandria University,
12Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Asuit University, 13Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 14Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Bani-suif University, 15Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Fayoum University, 16Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ Suhag University,
17Audiovestibular Medicine Unit, Otorhinolaryngology Department, Faculty of Medicine/ AlAzhar University, 18Physiotherapy and rehabilitation department, Zagazig University 19Audiovestibular Medicine,Unit, Otorhinolaryngology Department, Faculty of Medicine/ Suez canal University. 20Audiovestibular Medicine, Unit, Otorhinolaryngology Department, Faculty of Medicine/ Menia University. 21Audiovestibular Medicine, Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain shams University.
Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah
Abbreviations
AECPG: Adapted Egyptian Clinical practice guideline.
APTA: American physical therapy association.
VRT: Vestibular rehabilitation therapy.
BSA: British society of audiology
BVH: Bilateral vestibular hypofunction.
CBT: Cognitive behavioral therapy.
GSE: Gaze stabilizing exercises.
IGE: international guidelines for education
VR: Visual reality
VOR: Vestibulo-ocular reflex.
UVH: Unilateral vestibular hypofunction.
Executive Summary
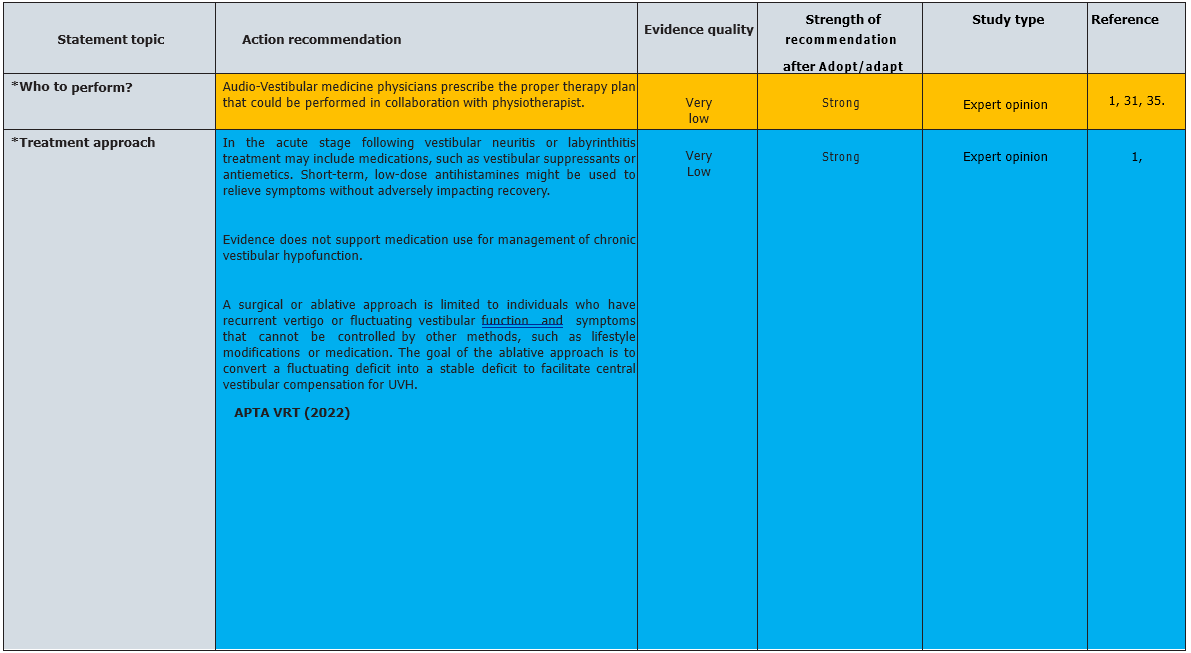
Audio-Vestibular medicine physicians prescribe
the proper therapy plan that could be performed in collaboration with physiotherapist,
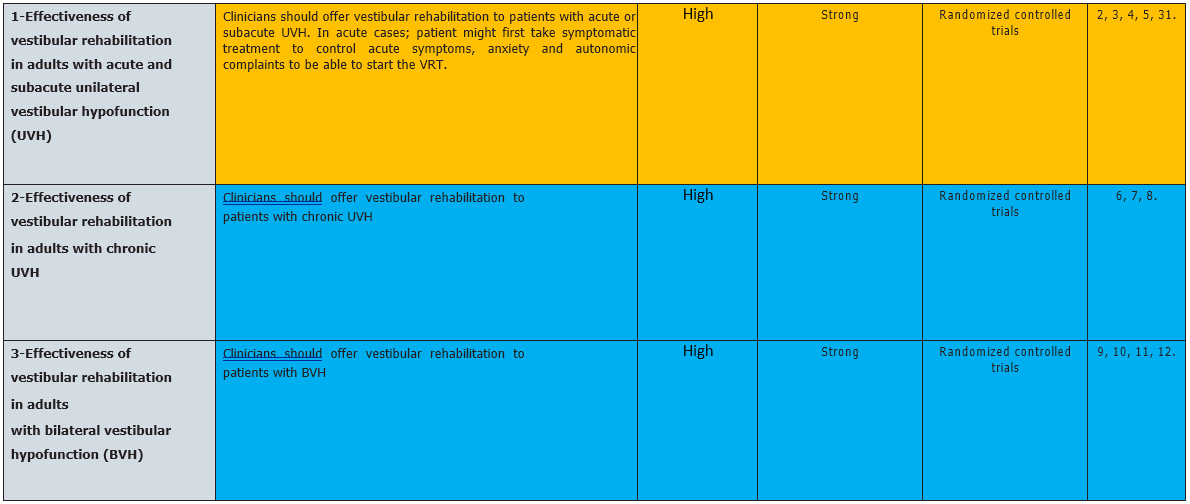
Clinicians should offer vestibular rehabilitation to patients with acute or
subacute UVH. (Strong recommendation), In acute cases; patient might
first take symptomatic treatment to control acute symptoms, anxiety and
autonomic complaints to be able to start the VRT. Also Clinicians are (strongly
recommended) to offer vestibular rehabilitation to patients with chronic
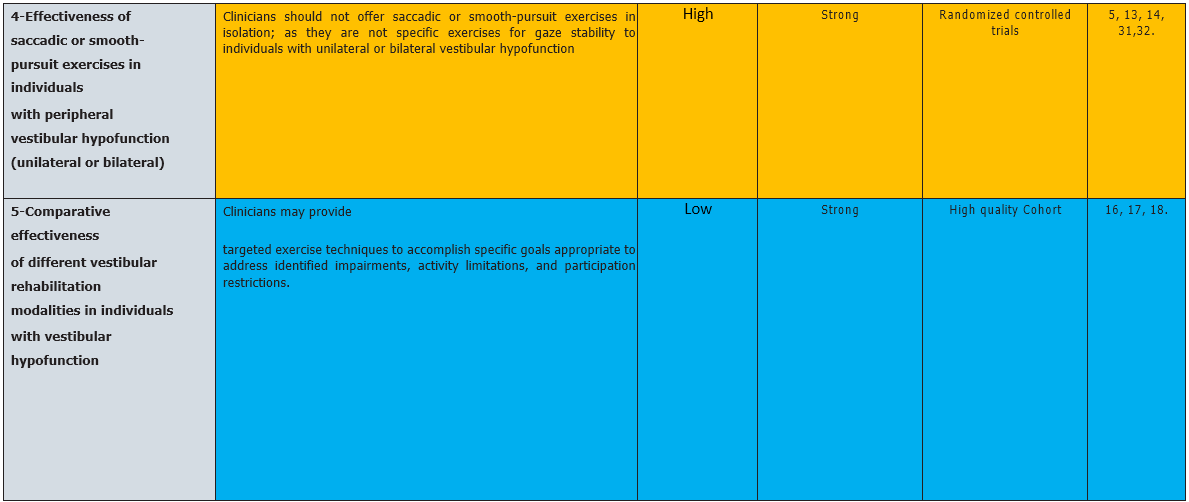
UVH and BVH. Clinicians should not offer
saccadic or smooth-pursuit exercises in isolation; as they are not specific
exercises for gaze stability to individuals with unilateral or bilateral
vestibular hypofunction (strong recommendation). Clinicians may provide targeted
exercise techniques to accomplish specific goals appropriate to address
identified impairments, activity limitations, and participation restrictions (strong
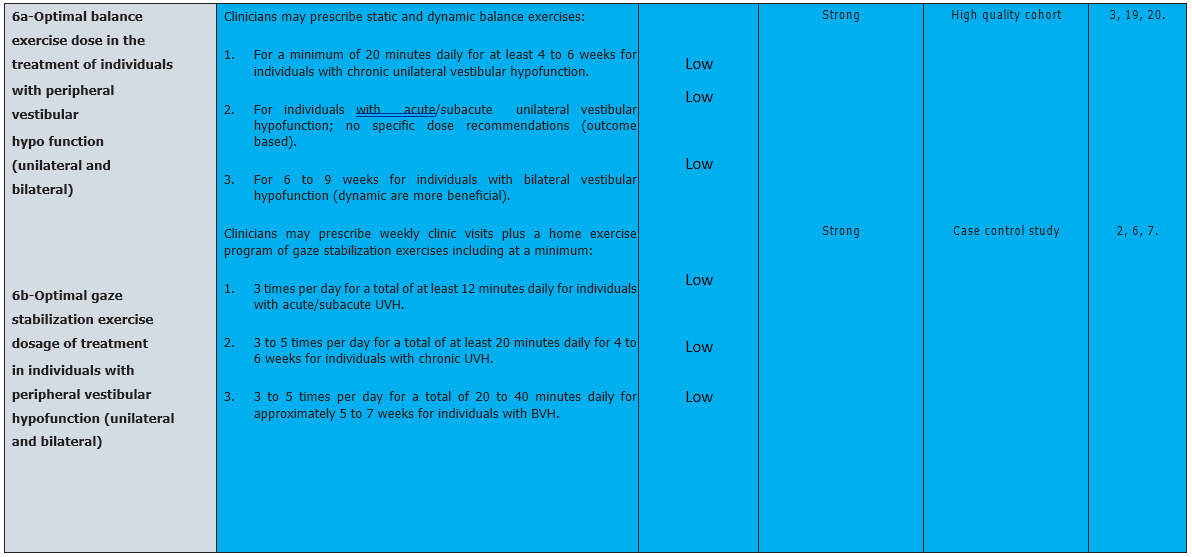
recommendation). Clinicians may prescribe static and dynamic balance
exercises and prescribe weekly clinic visits plus a home exercise program of
gaze stabilization exercises (strong recommendation). Clinicians should
offer supervised vestibular physical therapy in individuals with peripheral UVH
and BVH (strong recommendation). Clinicians may use achievement of
primary goals, resolution of symptoms, normalized balance and vestibular
function, or plateau in progress as reasons for stopping therapy; objective and
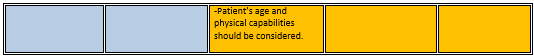
subjective outcome measures could be used, also Patient’s age and physical capabilities should
be considered. (Strong recommendation). Clinicians may evaluate factors
that could modify rehabilitation outcomes (strong recommendation). Clinicians
should offer vestibular rehabilitation therapy to persons with peripheral
vestibular hypofunction with the intention of improving quality of life (Strong
recommendation).
Introduction, scope and audience
➡️Introduction
Vestibular rehabilitation therapy (VRT) is a specialized form of physical therapy used to treat vestibular disorders or symptoms characterized by dizziness, vertigo and trouble with balance, posture and vision.
➡️Scope:
Providing evidence-based recommendations regarding appropriate VRT protocol to use in the treatment of individuals with acute, sub-acute, and chronic unilateral and bilateral peripheral vestibular hypofunction.
➡️Target audience:
Audio vestibular medicine physician are those who prescribe the proper therapy plan, ENT for appropriate referral and physiotherapist could perform physiotherapy under supervision of audio vestibular medicine physician.
Methods
➡️Methods of development
➡️Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Audio vestibular medicine Chief Manager, Audio vestibular medicine Executive Manager, Assembly Board, Grading Board and Reviewing Board.
➡️Search method
Electronic database searched:
Pubmed, Medline, Medscape, WebMD, Google Scholar
➡️Keywords:
Vestibular rehabilitation therapy, peripheral vestibular disorders, adults.
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Time period searched: from 2009 t0 2022
➡️Results
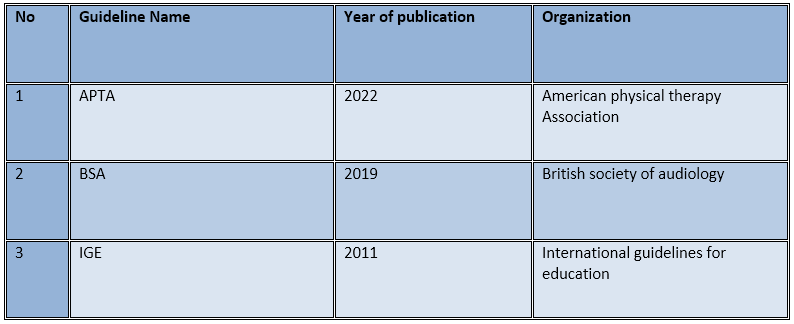
Three national Audio Vestibular Medicine consultants reviewed the guidelines available.
The American physical therapy association (APTA) guidelines gained the highest scores as regards currency, contents and quality and were thus adopted then adapted
It was graded by seventeen experts and reviewed by three expert reviewers to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
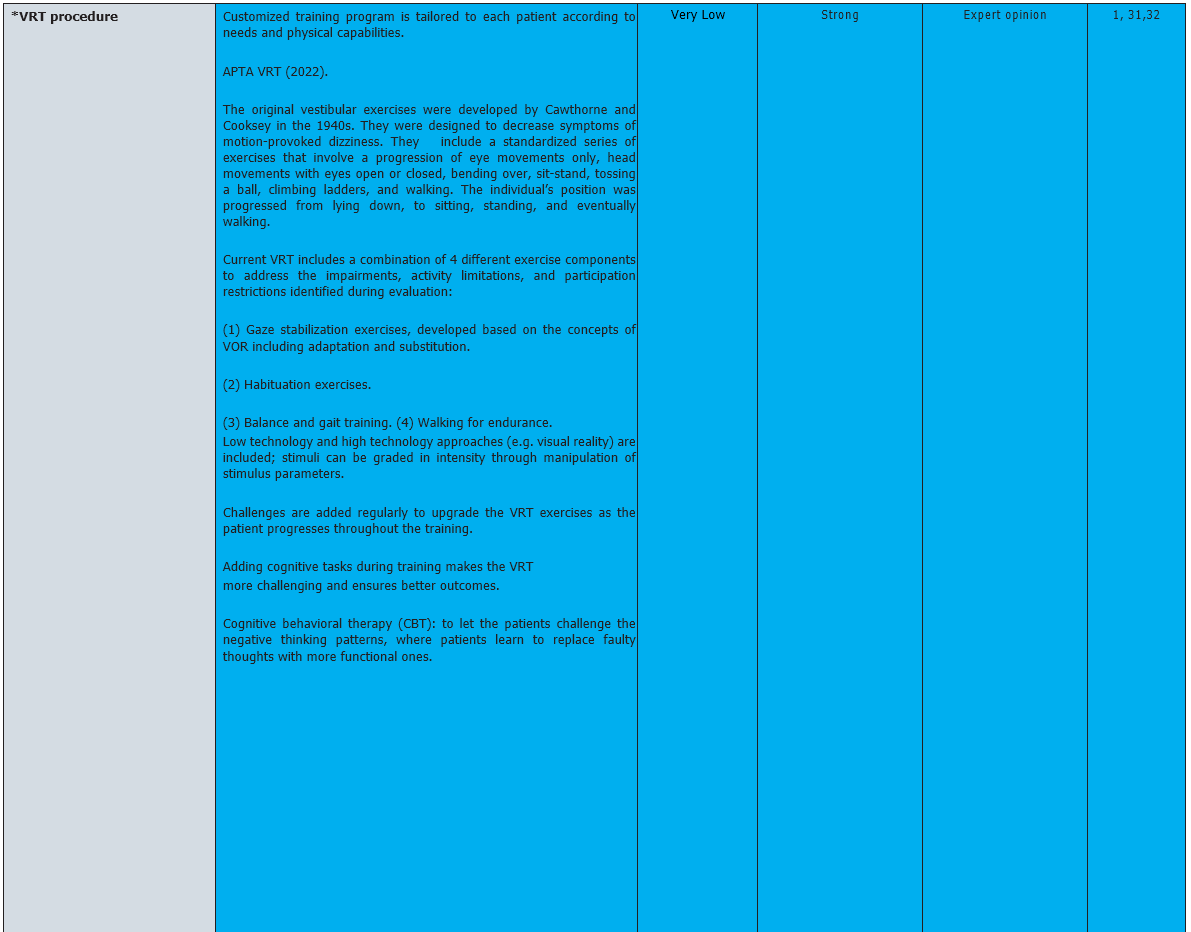
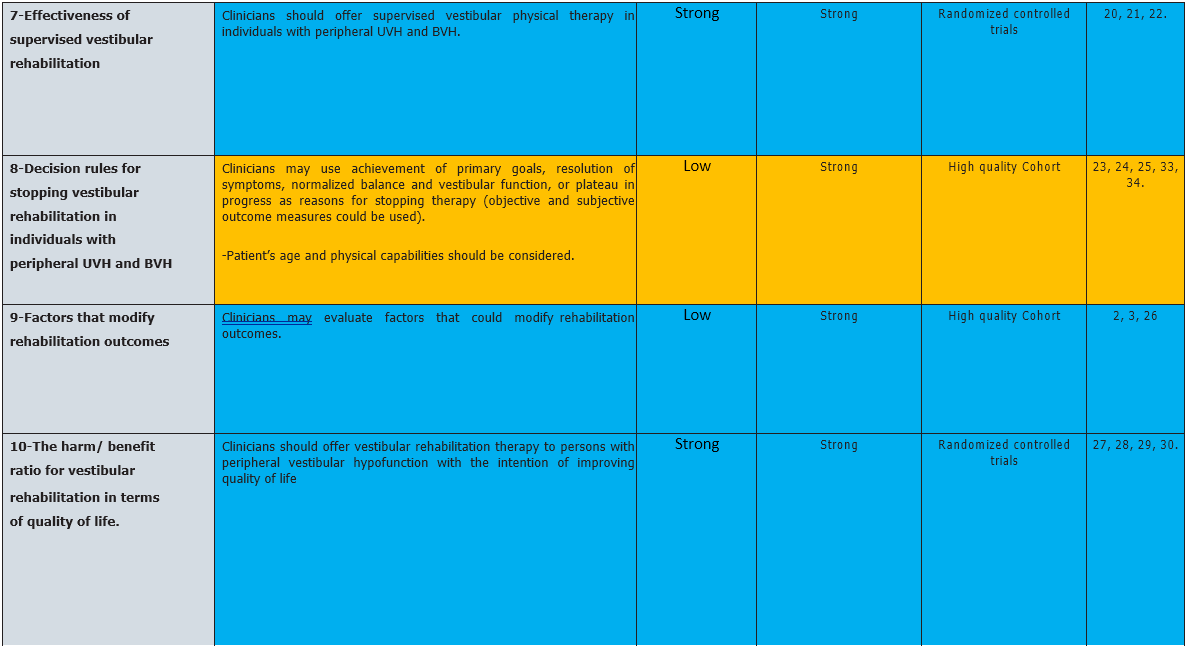
Recommendations
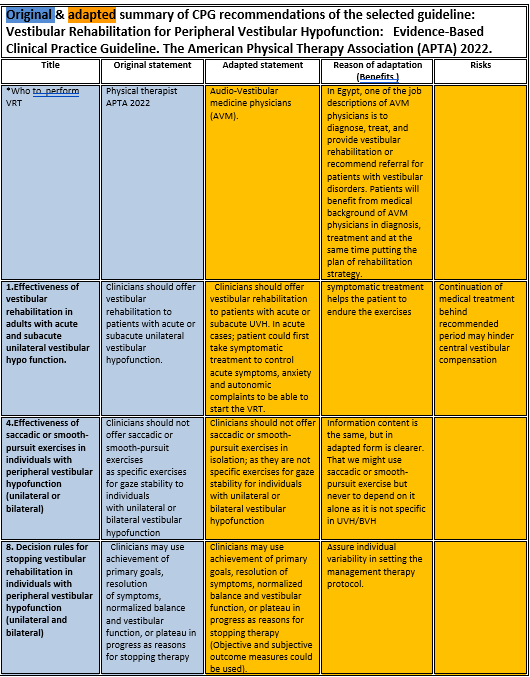
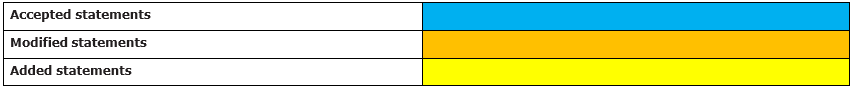
The following statements and flowchart were adapted from the Guidelines from Vestibular Rehabilitation for Peripheral Vestibular hypofunction: An updated clinical practice guideline from the academy of neurologic physical therapy of the American physical therapy association (APTA) 2022. which received the highest scores as regards the currency, contents, and quality.
Recommendations statements
Research needs
1-Researchers should explore delivery of VPT using technology, telehealth, or self-teaching methods as an alternative for some individuals and identify individual-level factors that impact the use of technology on rehabilitation outcomes and patient satisfaction.
2-There is a paucity of research on the effectiveness of vestibular rehabilitation in children. Randomized controlled studies are needed to determine the effect of GSE on gaze stability, gross motor abilities, and postural control in children with UVH and BVH.
3- Researchers need to investigate whether there is critical dosage or time points for person versus telehealth/remote supervision.
4-Researchers need to investigate added value of high technology methods (VR) to traditional methods of VRT.
5- Researchers should examine the concept of return to work. Areas for study include job requirements that may be difficult for individuals with vestibular hypofunction, job modification or assistive technology to allow return to work, criteria for return to work or disability assignment, and indicators for return to safe driving.
Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria
Audio vestibular physician should be able to:
· Acquire patient full medical history.
· Differentiate between UVH and BVH.
· Differentiate between peripheral and central causes of imbalance
· Apply customized VRT.
· Counseling the patient and/or family member.
· Periodic assessment for VRT effectiveness.
Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
References
1. Vestibular Rehabilitation for Peripheral Vestibular hypofunction: An updated clinical practice guideline from the academy of neurologic physical therapy of the American physical therapy association (APTA). Courtney D Hall et al. J. neurol. Phys. ther. 2022.
2. Lacour M, Laurent T, Alain T. Rehabilitation of dynamic visual acuity in patients with unilateral vestibular hypofunction: earlier is better. Eur Arch Otorhinolaryngol. 2020;277(1):103-113. doi:10.1007/s00405-019-05690-4.
3.Ismail EI, Morgan AE, Abdel Rahman AM. Corticosteroids versus vestibular rehabilitation in long-term outcomes in vestibular neuritis. J Vestib Res. 2018;28(5/6):417-424. doi:10.3233/VES-180645.
4. Tokle G, Mørkved S, Bråthen G, et al. Efficacy of vestibular rehabilitation following acute vestibular neuritis: a randomized controlled trial. Otol Neurotol. 2020;41(1):78-85. doi:10.1097/
MAO.0000000000002443.
5. Scheltinga A, Honegger F, Timmermans DP, Allum JH. The effect of age on improvements in vestibulo-ocular reflexes and balance control after acute unilateral peripheral vestibular loss. Front Neu-
rol. 2016;7:18. doi:10.3389/fneur.2016.00018.
6. Herdman SJ, Hall CD, Maloney B, Knight S, Ebert M, Lowe J. Variables associated with outcome in patients with bilateral vestibular hypofunction: preliminary study. J Vestib Res. 2015;25(3/4):185-194. doi:10.3233/VES-150556.
7. Lehnen N, Kellerer S, Knorr AG, et al. Head-movement-emphasized rehabilitation in bilateral vestibulopathy. Front Neurol. 2018;9:562. doi:10.3389/fneur.00562
8. Strupp M, Kim JS, Murofushi T, et al. Bilateral vestibulopathy: diagnostic criteria consensus document of the classification committee of the Bárány Society. J Vestib Res. 2017;27(4):177-189. doi:10.3233/VES-170619 .
9. Ricci NA, Aratani MC, Caovilla HH, Ganança FF. Effects of vestibular rehabilitation on balance control in older people with chronic dizziness: a randomized clinical trial. Am J Phys Med Rehabil. 2016;95(4):256-269.
10. Patarapak S, Jarusripan P, Isipradit P. Chulalongkorn vestibular balance exercise for rehabilitation in persons with various types of vestibular disorders. J Med Assoc Thai. 2015;98(suppl 1):S77-S84.
11. Itani M, Koaik Y, Sabri A. The value of close monitoring in vestibular rehabilitation therapy. J Laryngol Otol. 2017;131(3):227-231. doi:10.1017/S0022215116009750.
12. Szturm T, Reimer KM, Hochman J. Home-based computer gaming in vestibular rehabilitation of gaze and balance impairment. Games Health J. 2015;4(3):211-220. doi:10.1089/g4h.2014.0093
13. Herdman SJ, Schubert MC, Das VE, Tusa RJ. Recovery of dynamic visual acuity in unilateral vestibular hypofunction. ArchOtolaryngol Head Neck Surg. 2003;129(8):819-824. doi:10.1001/archotol.129.8.819.
14. Krebs DE, Gill-Body KM, Parker SW, Ramirez JV, Wernick Robinson M. Vestibular rehabilitation: useful but not universally so. Otolaryngol Head Neck Surg. 2003;128(2):240-250. doi:10.1067/mhn.2003.72.
15. Meldrum D, Herdman S, Vance R, et al. Effectiveness of conventional versus virtual reality-based balance exercises in vestibular rehabilitation for unilateral peripheral vestibular loss: results of a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(7):1319-1328.e1. doi:10.1016/j.apmr.2015.02.032. 16. Jáuregui-Renaud K, Villanueva Padrón LA, Cruz Gómez NS. The effect of vestibular rehabilitation supplemented by training of the breathing rhythm or proprioception exercises, in patients with chron- ic peripheral vestibular disease. J Vestib Res. 2007;17(1):63-72.
16. Jáuregui-Renaud K, Villanueva Padrón LA, Cruz Gómez NS. The effect of vestibular rehabilitation supplemented by training of the breathing rhythm or proprioception exercises, in patients with chronic peripheral vestibular disease. J Vestib Res. 2007;17(1):63-72.
17. Brugnera C, Bittar RS, Greters ME, Basta D. Effects of vibrotactile vestibular substitution on vestibular rehabilitation—preliminary study. Braz J Otorhinolaryngol. 2015;81(6):616-621. doi:10.1016/j.bjorl.2015.08.013.
18. Marioni G, Fermo S, Zanon D, Broi N, Staffieri A. Early rehabilitation for unilateral peripheral vestibular disorders: a prospective, randomized investigation using computerized posturography. Eur Arch Otorhinolaryngol. 2013;270(2):425-435. doi:10.1007/s00405-012-1944-4.
19. Cakrt O, Chovanec M, Funda T, Kalitová P, Betka J, Zverina E, KolárP, Jerábek J. Exercise with visual feedback improves postural stability after vestibular schwannoma surgery. Eur Arch Otorhinolaryngol. 2010;267(9):1355-1360. doi:10.1007/s00405-010-1227-x.
20. Pavlou M, Bronstein AM, Davies RA. Randomized trial of supervised versus unsupervised optokinetic exercise in persons with peripheral vestibular disorders. Neurorehabil Neural Repair. 2013;27(3):208-218. doi:10.1177/1545968312461715.
21. Varriano B, Sulway S, Wetmore C, et al. Vestibular exercises as a fall prevention strategy in patients with cognitive impairment. Can J Neurol Sci. 2020;47(1):126-130. doi:10.1017/cjn.2019.309.
22. van Vugt VA, van der Wouden JC, Essery R, et al. Internet based vestibular rehabilitation with and without physiotherapy support for adults aged 50 and older with a chronic vestibular syndrome in general practice: three armed randomised controlled trial. BMJ. 2019;367:l5922. doi:10.1136/bmj.l5922.
23. Telian S, Shepard N, Smith-Wheelock M, Kemink J. Habituation therapy for chronic vestibular dysfunction: preliminary results. Otolaryngol Head Neck Surg. 1990;103(1):89-95. doi:10.1177/019459989010300113.
24. Shepard NT, Smith-Wheelock M, Telian SA, Raj A. Vestibular and balance rehabilitation therapy. Ann Otol Rhinol Laryngol. 1993;102(3, pt 1):198-205. doi:10.1177/000348949310200306.
25. Topuz O, Topuz B, Ardiç FN, Sarhus M, Ögmen G, Ardiç F. Efficacy of vestibular rehabilitation on chronic unilateral vestibular dysfunction. Clin Rehabil. 2004;18(1):76-83. doi:10.1191/0269215504cr704oa.
26. Horak FB, Jones-Rycewicz C, Black FO, Shumway-Cook A. Effects of vestibular rehabilitation on dizziness and imbalance. Oto-laryngol Head Neck Surg. 1992;106(2):175-180.
27. Enticott JC, O’Leary SJ, Briggs RJ. Effects of vestibulo-ocular reflex exercises on vestibular compensation after vestibular schwannoma surgery. Otol Neurotol. 2005;26(2):265-269. doi:10.1097/00129492-200503000-00024.
28. Rossi-Izquierdo M, Santos-Pérez S, Soto-Varela A. What is the most effective vestibular rehabilitation technique in patients with unilateral peripheral vestibular disorders? Eur Arch Otorhinolaryngol. 2011;268(11):1569-1574. doi:10.1007/s00405-011-1532-z.
29.Tee LH, Chee NWC, Zhu M, Jin J. Functional outcomes after customized vestibular rehabilitation in subjects with chronic vestibular dysfunction. Physiother Sing. 2010;13(2):4-7.
30. Bittar RSM, Pedalini MEB, Lorenzi MC, Formigoni LG. Treating vertigo with vestibular rehabilitation: results in 155 patients. Rev Laryngol Otol Rhinol. 2002;123(1):61-65.
31.Practice guidance Vestibular Rehabilitation British society of audiology (BSA). 2019.
32.International Guidelines for Education in Vestibular Rehabilitation Therapy (IGE/VRT). Journal of Vestibular Research October 2011.
33.Hall CD, Herdman SJ, Whitney SL, et al. Vestibular rehabilitation for peripheral vestibular hypofunction: an evidence-based clinical practice guideline: From the American Physical Therapy Association Neurology.
34.Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines, Graham R, Mancher M, Miller Wolman D, et al. eds. Clinical practice guidelines we can trust. Washington, DC: National Academies Press (US). 2011. doi:10.17226/13058.
35. Phillips B, Ball C, Sackett D, et al. Oxford Centre for Evidencebased Medicine—Levels of Evidence. https:// www. cebm.net/ 2009/06/oxford-centre-evidence- based-medicine-levels-evidencemarch- 2009. apta. Published 2009.
Annexes
Editorial Independence:
· This guideline was developed without any external funding.
· All the guideline development group members have declared that they do not have any competing interests.
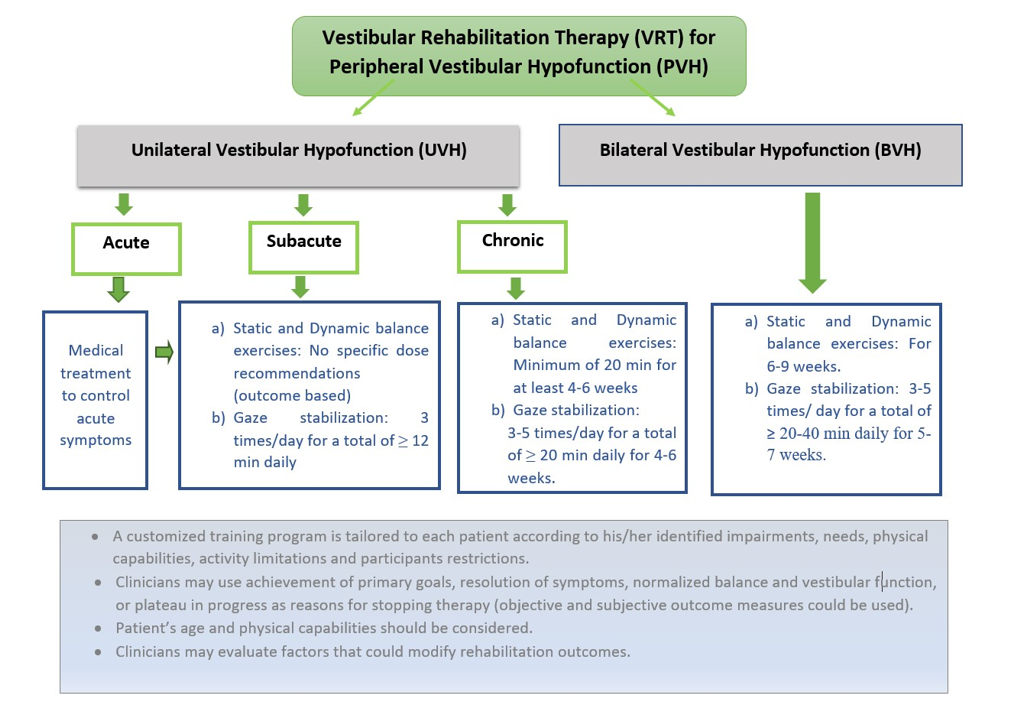
Annex 1: Guideline Flowchart
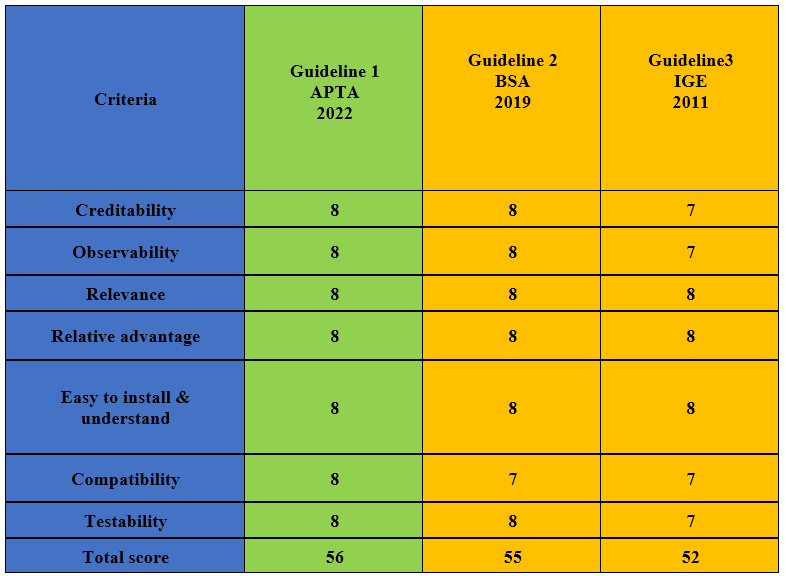
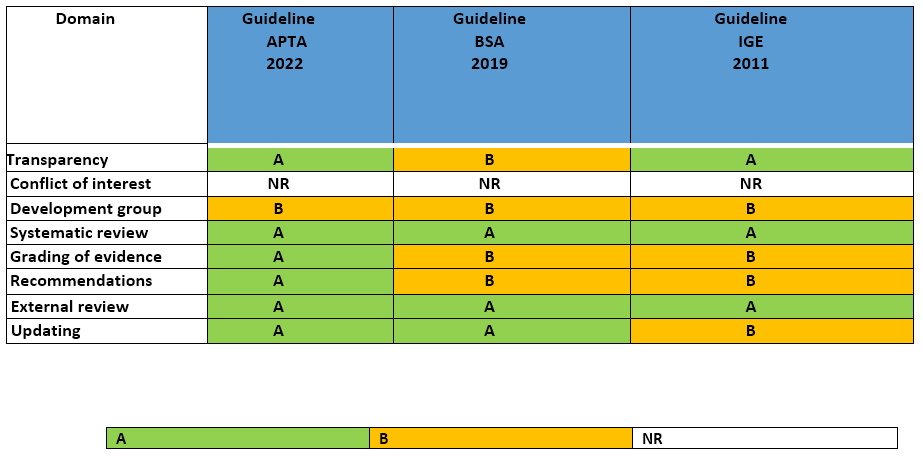
Annex 2: Tables of appraisal of selected guidelines: Content (table 1), Quality (table 2) and Currency (table 3) of the selected guidelines.
Assessment of Content
Assessment of Quality
Assessment of Currency of VRT for peripheral vestibular hypofunction
Annex 3: The risks and benefits of added and/or modified statements