Dysarthria (ECPG)
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Dysarthria (ECPG) |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:18 PM |
Description
"last update: 19 May 2024"
- Acknowledgements
Chief Editor: Reda Kamel1
General Secretary: Ahmed Ragab2
General Coordinator: Baliegh Hamdy3
Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdel Aziz,6 Tarek Ghanoum,7 Mahmoud Yousef8
Phoniatrics Chief Manager: Mahmoud Youssef8
Phoniatrics Executive Manager: Dalia Mostafa 9
Assembly board: Nirvana Gamal El Din Hafez Helmy 8, Ayman Shawky10
Grading Board (In alphabetical order): Azza Abdelaziz,11 Essam Aref,12 Ahlam A. N. El-Adawy,13 Safaa El Sady,8 Dalia Mostafa,9 Asmaa El-Dessouky Rashad,14 Yossra Abdel
Reviewing Board (In alphabetical order: Ahlam A. N. El-Adawy,13 Sabah Hassan8, Nahla Refai8
External reviewer: Taha Kamel Alloush 16
1Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 2Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 3Otorhinolaryngology Department, Faculty of Medicine/ Minia University, 4Otorhinolaryngology Department, Faculty of Medicine/ Beni-Suef University, 5Otorhinolaryngology Department, Faculty of Medicine/ Tanta University, 6Otorhinolaryngology Department, Faculty of Medicine/ Mansoura University, 7Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 9Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Cairo University, 10Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Military Armed Forced15, 11Phoniatrics Unit, Otorhinolaryngology Department/ Hearing and Speech Institute, 12Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 13Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Sohag University, 14Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Menoufia University, 15Phoniatrics Unit, Otorhinolaryngology Department, Faculty of Medicine/ Al-Azhar University.16 Neurology Department, Faculty of medicine, Ain Shams University
- Abbreviations
SMA: Smith Accent Voice therapy
APA: Auditory Perceptual Assessment
CPG: clinical Practice guidelines
AAC: augmentative and Alternative Communication mode- Executive Summary
The scope of the guidelines in the diagnosis and management of Dysarthria
1. Any subject with speech difficulty should undergo:
a). History taking ( strong recommendation)
b). Auditory perceptual assessment (APA) (strong recommendation)
c). Examination that includes both neurological examination and ENT examination ( strong recommendation)
2. By the end of this assessment battery, dysarthria by its type and severity should be diagnosed with exclusion of other speech disorders. ( conditional recommendation )
3. Rehabilitation will start tailoring a therapeutic plan that may include all the aspects (in blue rectangles) or some of them according to the most prominent speech parameters affecting the speech intelligibility of the patient.(strong recommendation)
4. For every aspect, your therapeutic trials may succeed or fail, and accordingly measurement of the outcome is of value every three months. Work with the patient in more than one aspect at the same time and not one of them at a time.( conditional recommendation)
5. Resonance therapy through training ,however, if failed shift to obturator.( conditional recommendation)
6. Articulation, respiration, phonation and prosody have many techniques to correct them.(conditional recommendation)
7. Prognosis and therapy termination is determined when patient’s satisfaction is reached and when the Auditory perceptual assessment showed correction and elimination of difficulties. (conditional recommendation)
8. Augmentative and alternative communication methods should be considered in case achieved progress is unsatisfactory, particularly in patients having severe difficulties. (strong recommendation )
- Introduction, scope and audience
➡️Introduction and definition
Dysarthria is a heterogeneous group of neurological speech disorders whose characteristics reflect abnormalities in the strength, speed, range, timing, or accuracy of speech movements as a result of pathophysiologic conditions such as weakness, spasticity, ataxia, rigidity and a variety of involuntary movements (e.g., dystonia and choreoasthetosis). Dysarthrias can affect the respirators, laryngeal, velopharyngeal, and oral articulatory subsystems, singly or in combination. The impact of dysarthria ranges from a barely appreciable speech disorder to a reduction in the intelligibility of speech to an inability to speak. This group of disorders varies along a number of dimensions, including age of onset (Congenital or acquired at any age), cause (vascular, traumatic, neoplastic, and so on), natural course (Developmental, recovering, stable, degenerative, and so on), site of lesion (Many sites in the central or peripheral nervous system or both), neurologic diagnosis Parkinson’s disease, traumatic. In addition, dysarthria is a speech disorder due to disturbed muscular control of the speech mechanism resulting from impaired motor control involved in the execution of speech. It has a neurogenic origin.
➡️Scope:
The scope of the guideline provides a brief overview of the context (eg: current policy and practice ) as well as the key issues that will be considered in the guideline, why the guideline is needed or where it will add value
➡️Target audience:
Phoniatricians and pediatricians.
- Methods
Methods of development
➡️Stakeholder Involvement: Individuals who were involved in the development process. Included the above-mentioned Phoniatrics Chief Manager, Phoniatrics Executive Manager, Assembly Board, Grading Board and Reviewing Board.
Information about target population experiences were not applicable for this topic.
➡️Search Method:
➡️Electronic database searched:
Pubmed, Medscape, ASHA, ANCDS Bulletin board, Google scholar
➡️Keywords
Dysarthria, neurological speech disorders, motor speech disorders, prosody
The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing.
➡️Time period searched: from January 2005 to December 2019.
➡️Results
Two national Phoniatricians reviewed the guidelines available. Guidelines from Royal college of speech and language therapists and ASHA summary of the clinical practice guidelines and ANCDS evidence for effectiveness of treatment gained the highest scores as regards currency, contents and quality.
It was graded GRADE by7 experts and reviewed by three expert reviewers to improve quality, gather feedback on draft recommendations.
The external review was done through a rating scale as well as open-ended questions.
➡️Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties.
Interpretation of strong and conditional recommendations for an intervention
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
WHO handbook for guideline development – 2nd ed.
Chapter 10, page 129
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
The following statements and flowchart were adapted from the Guidelines from the Academy of neurologic Communication disorders and sciences (ANCDS) and Royal college of speech and language therapists
which received the highest scores as regards the currency, contents, and quality.Recommendations Statements
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Assessment of VP Function
|
History Taking This phase of the assessment involves gathering pertinent information from the patient, the medical records and the referral source. Information should be gathered on areas such as the following: • The onset of symptoms and medical/ dental history. • the nature, duration, and natural course of velopharyngeal (VP) impairment. • Reports of previous treatment. • The level of concern about the problem. • The patient’s motivation relative to treatment. |
High |
Strong recommendation |
Systematic Review |
5 |
|
Assessment of VP Function
|
Search for etiological factors |
Very low |
Strong recommendation |
Expert opinion |
4 |
|
The perceptual assessment of speech
|
Determining the severity of the velopharyngeal impairment and the degree to which the velopharyngeal impairment disrupts speech production is critical to establishing the need for intervention and for accurate therapeutic intervention. |
High |
Strong recommendation |
Systematic Review |
5 |
Clinical questions | Action recommendation | Evidence Quality | Strength of Recommendation | Study type | Reference |
Examination
| Physical Examination This involves an assessment of the structure and function of the oral mechanism, including the velopharynx at rest and during movement. |
High |
Strong recommendation | Systematic Review | 5 |
Instrumental examination of the velopharyngeal mechanism
| It is necessary to directly observe and measure velopharyngeal activity. Instrumentation may include videoflouroscopy, nasoendoscopy, aerodynamic (pressure-flow). assessments, and acoustic assessment. This instrumentation allows for the evaluation of • Intraoral air pressure and nasal airflow during production of pressure consonants. • Palatal movement. • Lateral pharyngeal wall movement. • Sphincteric activity during speech. • Nasal airflow and intraoral air pressure. • The timing of velopharygeal movements. |
High |
Conditional recommendation | Systematic Review |
5 |
Instrumental examination of the velopharyngeal mechanism
| It is necessary to directly observe and measure velopharyngeal activity. Instrumentation may include videoflouroscopy, nasoendoscopy, aerodynamic (pressure-flow). assessments, and acoustic assessment. This instrumentation allows for the evaluation of • Intraoral air pressure and nasal airflow during production of pressure consonants. •Palatal movement. • Lateral pharyngeal wall movement. • Sphincteric activity during speech. • Nasal airflow and intraoral air pressure. • The timing of velopharygeal movements. |
High |
Conditional recommendation | Systematic Review | 5 |
Documentation by audiorecording and nasofibroscopic examination
| *Audio recording of speech sample to compare between before and after therapy. *Nasofibroscopic examination determine degree of palatal mobility and lateral pharyngeal wall mobility. |
Very low |
Conditional recommendation
| Expert opinion | 2 |
Resonance Intervention goal
| Enhancement of speech and communication function is a fundamental target of intervention. | High | Strong recommendation | Systematic Review | 5 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Prosthetic intervention
|
Palatal lift fitting has a long history associated with improved speech function in selected cases of dysarthria. |
High |
Strong recommendation |
Systematic Review |
5 |
|
Surgical intervention
|
It is not considered unless all other interventions have failed. |
High |
Strong recommendation |
Systematic Review |
5 |
|
Measurement of Outcomes
|
It is increasingly important to document the outcomes of intervention. A variety of outcome measures may be obtained and can be categorized. |
High |
Strong recommendation |
Systematic Review |
5 |
|
Respiratory and phonatory disorders in dysarthria
|
Respiratory/phonatory impairment is a common manifestation of dysarthria and can have a major impact on the adequacy of speech production. Treatment of the respiratory and phonatory subsystems. It is often given priority because improvements at this level generate improvements in other aspects of speech as well. |
High |
Strong recommendation |
Metanalysis |
2 |
|
Assessment of respiration and phonation
|
History of the problem 1. Onset and medical history. 2. Nature, duration and course of dysfunction. 3.Report of previous treatment. 4.Level of patient’s concern about the impairment and social limitations. 5. Patient’s motivation relative to treatment. Specific attention should be paid to the patient’s presenting complaints as they may provide the initial evidence of respiratory or phonatory involvement. |
low |
Strong recommendation |
Observational study |
4 |
|
Assessment of phonation and respiration
|
Speech characteristics can provide a window into the nature and existence of respiratory and/or phonatory subsystem involvement. perceptual evaluation of loudness and breath patterning. Inadequate loudness and improper control of loudness, as well as abnormal patterning of inhalation and exhalation during speech, may serve as indicators of impaired respiratory and function. |
Moderate |
Strong recommendation |
Metaanalysis |
2 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Assessment of respiration and phonation
|
Loudness • Overall loudness level. • Inconsistent loudness level. • Sudden, uncontrolled alterations in loudness. • The patient is unable to increase loudness. • The patient is unable to speak quietly. • The patient is unable to emphasize words in a sentence by increasing loudness. Breath Patterning • The patient does not demonstrate the normal pattern of quick inhalation followed by prolonged exhalation and • Does not inhale to appropriate lung volume levels (Chenery, 1998) • Speech is interrupted by sudden, forced inspiratory/expiratory • The patient runs out of air before inhaling • The patient produces few words/syllables on one breath. • Breaths occur at syntactically inappropriate locations in the utterance. |
high |
Strong recommendation |
Metaanalysis |
2 |
|
Assessment of respiration and phonation
|
Determination of Overall grade of dysphonia (Breathy, rough, asthenic or strained) Determination of pitch and associated vocal fry. |
Very low |
Strong recommendation |
Expert opinion |
5 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Physical Examination
|
Physical Examination A physical examination of the structure and function of the speech mechanism should be conducted, particularly if there are concerns of respiratory involvement. * The body position of the patient during evaluation (and treatment) should be con- sidered. Audible breathy inspiration, inhalatory stri- dor, or an audible grunt at the end of ex- piration. * Observation of these symptoms may pro- vide insight into the presence of respirato- ry/phonatory impairment, and whether the dysfunction stems from weakness, incoordi- nation, involuntary movements, and/or mal- adaptive strategies. |
Very low |
Strong recommendation |
Observational study |
2, 4 |
|
Clinical screening
|
Clinical Screening • A simple water glass manometer. • A hand-held respirometer is an economical device for gathering data on vital capacity. • Contrasting the sharpness of the patient’s cough with the glottal coup. • Sustained phonation time is also used as a very general estimate of respiratory/ phonatory capacity. • Sustained phonation with changes in loudness may also be implemented to estimate respiratory drive. |
Very low |
Conditional recommendation |
Observational study |
2,1,3 |
|
Instrumental Measures
|
A number of valuable respiratory/airflow measures (e.g., vital capacity, forced expiratory volume, functional residual capacity, inspiratory capacity, and expiratory/inspiratory reserve volumes) and subsequently compare them to predicted values based on the patient’s age, height and sex. Additionally, kinematic assessment allows the SLP to infer the airflow volume. |
Very low |
Strong recommendation |
Observational study |
1,2,3 |
|
Instrumental Measures
|
*Maximum phonation time is often used as a global assessment of phonatory capacity. *laryngeal adduction can be inferred from the sharpness of a patient’s cough and glottal coup. |
Very low |
Strong recommendation |
Observational study |
1,2,3 |
|
Phonatory assessment
|
Phonatory Function/ laryngeal assessment.
A formal laryngeal assessment should be conducted when structural lesions or lesions of the vagus nerve are a possibility or prior to intensive voice therapy, such as the Lee Silverman Voice Treatment program. |
Very low |
Strong recommendation |
Observational study |
1,2,3 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Instrumental assessment of phonatory dysfunction
|
• Endoscopy. • Videostroboscoopy. • High-speech photography. • Optically precise rigid laryngoscopes. • Flexible fiberoptic laryngoscopy. • Aerodynamic measures have demonstrated utility in documenting perceptual voice characteristics and differentiating speakers with hypokinetic dysarthria. • Photoglottography. • Electroglottography. • Spectrographic/acoustic analyses. • Laryngeal aerodynamics. • Indirect mirror laryngoscopy. |
high |
Strong recommendation |
Systematic review |
6 |
|
Individual Intervention
|
Interventions vary as a type of dysarthria, severity of dysarthria, and co-existing factors. Therefore, individual intervention plans must be developed. |
High |
Strong recommendation |
Systematic review |
6 |
|
Individual Intervention
|
Staging of Intervention. Dysarthria often is not a stable condition. For example, children with developmental dysarthria may experience physiologic changes affecting speech production as they mature. Adults with acquired dysarthria may experience phases of recovery; as in dysarthria associated with traumatic brain injury; or phases of degeneration. (i.e., the timing of treatment) is critical for successful outcomes. |
High |
Strong recommendation |
Systematic review |
6 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Management of Reduced Function
|
The symptoms of respiratory/phonatory impairment may be categorized as reductions in: 1. Respiratory support. 2.Respiratory/phonatory coordination and control. 3. Phonatory functioning. |
High |
Strong recommendation |
Systematic review |
|
|
Improving the respiratory support
|
The following techniques have demonstrated clinical utility for improving respiratory support: • Controlled exhalation tasks. • Maximum inhalation and exhalation tasks. • Pushing and pulling techniques. • Breathing against resistance. • Using an air pressure transducer with feedback from an oscilloscope or computer screen. • Sustaining phonation with feedback from Visipitch or the VU meter on a tape recorder. |
High |
Strong recommendation |
Systematic review |
6 |
|
Prosthetic Assistance
|
Expiratory boards or paddles provide a stationary object for the patient to lean into while speaking, thus increasing expiratory force. |
high |
Conditional recommendation |
Systematic review |
6 |
|
Speech Tasks
|
Manipulations of breathing patterns during speech production can provide a means of improving respiratory support |
high |
Conditional recommendation |
Systematic review |
6 |
|
Improving Coordination/Control
|
Nonspeech Tasks Rehearsing a speech-like breathing pattern (i.e., quick inspirations and slow, controlled expirations) • Implementing “inspiratory checking” without accompanying speech (if it is problematic for the patient to speak on controlled exhalations). • Facilitating inspiratory coordination and speed through sniffing, or exhalatory coordination through blowing. • Practicing switching between inspiration and expiration; the speed of the task can eventually be increased. |
high |
Strong recommendation |
Systematic review |
6 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
|
Speech Tasks Initiate speech at variable points in the respiratory cycle and need more consistent inspiratory control. • Initiate speech at inappropriate lung volume levels and need to vary the depth of consecutive inhalations. • Terminate speech late in the expiratory cycle with resultant diminished loud- ness. • Exhibit abnormal or maladaptive respiratory patterns, such as speaking on inhalation and forced expiration, often seen in patients with hyperkinetic dysarthria or patients with a concomitant cognitive impairment. • Adopt a fatiguing pattern of breathing, such as excessive shoulder elevation. The speaker can then practice read ing paragraphs in which the respira tory patterns or breath group boundaries have been marked. • Cued conversational scripts. Conver- sational scripts for two speakers are prepared. The patient can practice modifying inhalations according to the marked respiratory patterns while speaking with another person. • Un cued reading/conversation. The patient reads aloud or speaks conver- sationally without the aid of respiratory pattern markings. |
High |
Strong recommendation |
Systematic review |
6 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Improving Phonatory Function
|
Physical Strategies to Enhance Adduction: Clasping hands together and squeezing palms together as hard as possible • Interlacing hands and pulling outward. • Pushing down on the speaker’s raised arms in a rapid, uninterrupted motion. • Sitting in a chair, grasping the bottom with both hands, and pulling upward. • Sitting in a chair and pushing down on the seat bottom with both hands. • Pushing against a lap board, the arms of a wheelchair, or against any other firm surface. • Pushing the head forward against resistance provided by the examiner’s hands placed on the forehead of the speaker. • Grunting and controlled coughing (To elicit phonatory behavior). Trigger Better Speech with Increased Loudness • High phonatory and physical effort • Intensive treatment: Daily practice opportunities are requisite; treatment is administered four times a week for 16 sessions in one month. • Sensory calibration/perception: Speaker learns to identify the appropriate amount of effort. • Quantification: Quantified feedback by the clinician is key to motivating speakers. |
high |
Strong recommendation |
Systematic review |
6 |
|
Measurement of Outcomes
|
Perceptual measures. Measure of activity. Measures of impairment. |
high |
Strong recommendation |
Systematic review |
6 |
|
Alternative and augmentative communication tools
|
If a speaker remains unable to communicate satisfactorily following intervention, AAC modes should be pursued. |
high |
Strong recommendation |
Systematic review |
6 |
|
Candidacy
|
The most common explanation for selecting a particular intervention for a speaker with dysarthria was based on physiologic features. Because the respiratory subsystem provides the energy source and the phonatory system provides the sound source, both are critical to speech production. |
high |
Strong recommendation |
Systematic review |
6 |
|
Articulation therapy
|
Working with articulatory deficits as an isolated error of articulation. |
Low |
Conditional recommendation |
Cross sectional study |
7 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
|
Prognostic indicators were provided for intervention. * In speakers with flaccid dysarthria, improved phonation with pushing exercises was used as a rationale for a complete program to enhance respiratory drive. * In persons with Parkinson disease, improved phonation with instructions to speak loudly was cited as a positive indicator of candidacy for treatment. |
high |
Strong recommendation |
Systematic review |
6 |
|
Clinical questions |
Action recommendation |
Evidence Quality |
Strength of Recommendation |
Study type |
Reference |
|
Improving phonatory Function
|
Smith accent voice therapy technique will improve function of respiration and phonation in the form of: • Increase loudness. • Better respiratory support. • Slowing the rate of speech. • Adjust onset of phonation and respiration. |
Very low |
Strong recommendation |
Cross sectional study |
6,7 |
|
Articulation therapy
|
Treatment of articulatory errors using: Consonant exaggeration. Syllable by syllable attack. Slowing the rate of speech. Oral muscular exercises are not mandatory for weak musculature as muscle tone needed for speech is different from muscle tone needed for the swallowing process. Restrict oral muscle exercises in drooling. |
Very low |
Conditional recommendation |
Cross sectional study |
6,7 |
|
Prosodic correction
|
Therapeutic intervention for: Pitch inflections, stress and tone units. |
Very low |
Strong recommendation |
Cross sectional study |
6,7 |
|
AAC
|
Augmentative and alternative communication in case of: *Failed traditional therapy. *Anarthria. |
Very low |
Strong recommendation |
Cross sectional study |
6,7 |
|
Prognosis
|
Good prognosis with: Young age. Early intervention. Intensive therapeutic strategies. |
Very low |
Conditional recommendation |
Cross sectional study |
6,7 |
- Research needs
There is a need to conduct randomized controlled trials (RCTs) to determine the efficacy of therapy in persistent prosodic affection
The factors influencing the outcome of rehabilitation using smith accent voice therapy
- Monitoring and evaluating
Monitoring/ Auditing Criteria: to assess guideline implementation or adherence to recommendations.
Acquire the a full history from the patient or parents
· Exclude other causes of speech difficulty
· Prescribe the proper assessment
· Consider managing the defective speech mechanism according to the patient’s needs
· Give advice on how to monitor improvement
All clinicians should be aware and informed to consider the following:
· Red Flags that need urgent referral for Assessment/ Management must be taken into consideration.
· For Assessment it is crucial to perform a detailed history/ clinical examination as a minimum patient assessment
· Management should be targeted towards treating the defective speech mechanism and to improve intelligibility of speech.
- Updating
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
1. Royal college of speech and language therapists. Clinical guidelines. Speech mark publishing. 2005.
2. Yorkston KM, et al. Evidence for effectiveness of treatment of loudness, rate, or prosody in Dysarthria: A systematic review. Journal of Medical speech and language pathology. ANCDS Bulletin Board. Carl Coehlo. 2007;15(2).
3. ASHA Summary of the clinical practice guideline 2017, https://www.asha.org/articlesummary.dysarthria.
4. Clinical guidelines speech therapy e vi core healthcare. 2019.
5. Yorkston KM, Spencer KA, Duffy J, Beukelman, et al.: Evidence –Based Practice guidelines for dysarthria: Management of velopharyngeal function. Academy of Neurologic Communication Disorders and Science: Bulletin Board ANCDS, Journal of Medical Speech language pathology. 2001;9(4):257-274.
6. Spencer KA, Yorkston KM, etal.,: Practice guidelines for Dysarthria: Evidence of the behavioral management of the respiratory/phonatory system. Technical report (3). Academy of neurologic communication disorders and sciences, 1-51
7. Fujimura O and Hirano M : Voice quality in neurological disorders; pathophysiological correlates. in: Vocal fold physiology. Singular publishing 1995
- Annexes
Editorial Independence:
- This guideline was developed without any external funding.
- All the guideline development group members have declared that they do not have any competing interests.

Annex2 :
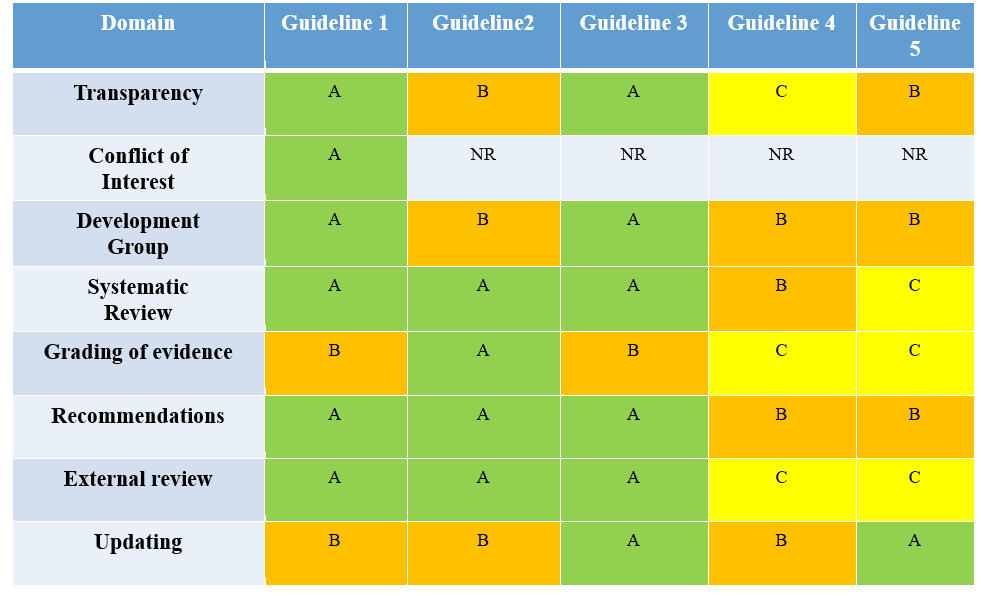
Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.
Table 1: Currency
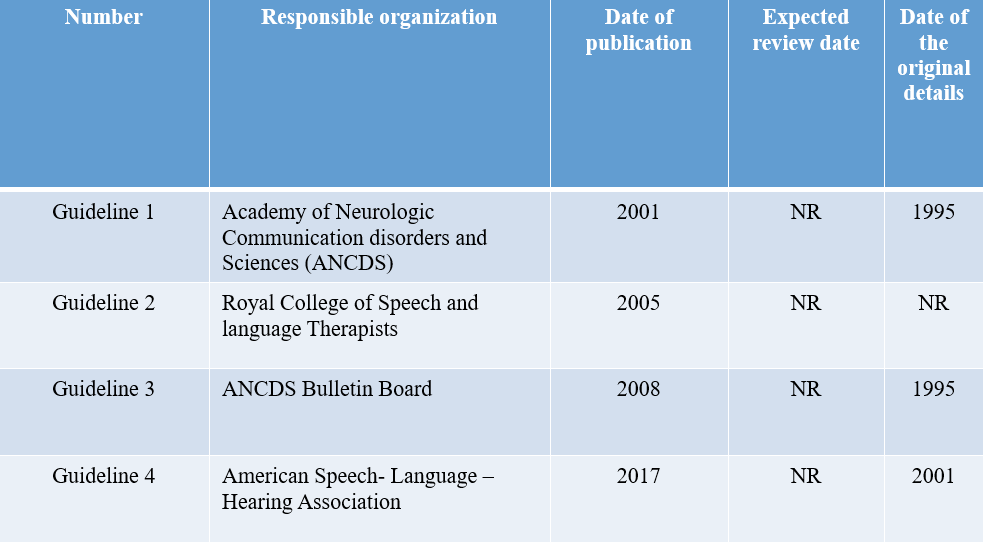
Table 2: Content
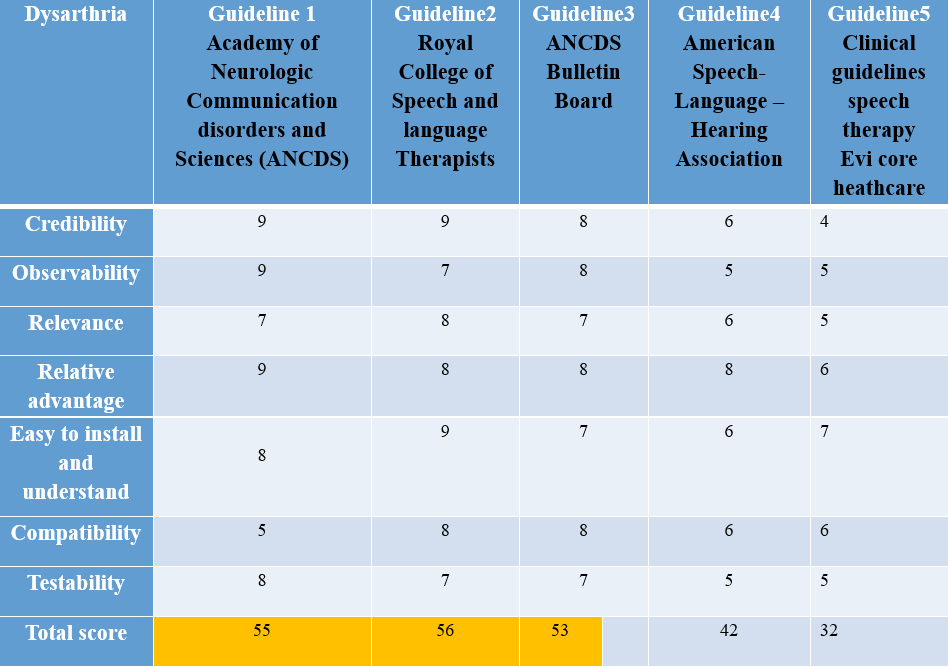
Table 3: Quality
Annex 3:
The risks and benefit from added or modified statements
|
Statement |
Risk |
benefit |
|
Smith accent voice therapy technique will improve function of respiration and phonation in the form of: § Increase loudness. § Better respiratory support. § Slowing the rate of speech. Adjust onset of phonation and respiration. |
May not applied by all physicians. It is usually known and applied by middle east physicians |
Mandatory in cases of dysarthria as it corrects the prosodic affection as well as loudness and respiratory incoordination and hence improve intelligibility |
|
Treatment of articulatory errors using: Consonant exaggeration. Syllable by syllable attack. Slowing the rate of speech. Oral muscular exercises are not mandatory for weak musculature as muscle tone needed for speech is different from muscle tone needed for the swallowing process.
|
Speech Intelligibility won’t improve |
Essential to improve speech intelligibility |
|
Therapeutic intervention for: Pitch inflections, stress and tone units |
The tone of speech as well as other prosody elements still affected with abnormal speech performance |
Prosodic correction |
|
Augmentative and alternative communication in case of: *Failed traditional therapy. *Anarthria. |
May stop trying to train verbal communication |
There is need to train patients using AAC to overcome loss of communication in cases of anarthria |
|
Good prognosis with: Young age. Early intervention. Intensive therapeutic strategies. |
Unrealistic expectations might stop commitment to therapy intervention |
Adding prognostic apects may motivate patients and caregivers to continue therapy even if slow improvement is seen |










