PALPABLE BREAST MASSES
| Site: | EHC | Egyptian Health Council |
| Course: | Radiology Guidelines |
| Book: | PALPABLE BREAST MASSES |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:45 PM |
Description
"last update: 13 May 2024"
- Acknowledgement
We would like to acknowledge the Egyptian Health Council, Committee of National Egyptian Guidelines, and Radiology Scientific Committee for adapting this Guidelines.
Chair of the Panel:
Tarek El-Diasty
Scientific Group Members:
Anan Atef, Dalia Ahmed, Ekram Hamed, Heba El-Kassas, Ihab Reda, Khaled Matrawy, Maha Hussein Helal, Mohamed Fawzi, Mohamed Shaker, Ragab Hani, Rasha Kamal, Sahar Mansour, Samar El-Maadawy, Rana Hussein, Wael Elshawaf, Wahid Tantawy.
- Abbreviations
BIRADS: Breast imaging reporting and data system
CEM: Contrast enhanced mammography
DM: Digital mammography
DBT: Digital breast tomosynthesis
FNAB: Fine needle aspiration biopsy
MRI: Magnetic Resonance Imaging
US: Ultrasound.
- Glossary
Breast mass: a growth or a lump which develops in the breast that can be felt by the patient or healthcare provider. The mass can be “caused by an abnormal growth of cells , a cyst, hormonal changes, or an immune reaction. A mass may be benign (not cancer) or malignant (cancer)” [2].
Contrast-enhanced mammography: Contrast-enhanced mammography (CEM) is an emerging imaging diagnostic tool that uses iodinated contrast media for the visualization of breast neovascularity in a fashion similar to magnetic resonance imaging (MRI). [3]
Core biopsy: a biopsy in which a cylindrical sample of tissue is obtained (as from a kidney or breast) by a hollow needle.
Digital breast tomosynthesis: Tomosynthesis or “3D” mammography is a new type of digital x-ray mammogram which creates 2D and 3D-like pictures of the breasts. This tool improves the ability of mammography to detect early breast cancers and decreases the number of women “called back” for additional tests for findings that are not cancers. [4]
Fine needle aspiration biopsy: the process of obtaining a sample of cells and bits of tissue for examination by applying suction through a fine needle attached to a syringe.
Magnetic resonance imaging (MRI): a technique that produces computerized images of internal body tissues using a powerful magnetic field and pulses of radio waves.
Mammography: X-ray examination of the breasts
Ultrasound: the diagnostic or therapeutic use of ultrasound and especially a noninvasive technique involving the formation of a two-dimensional image used for the examination and measurement of internal body structures and the detection of bodily abnormalities
- Executive Summary
This guideline is concerned with imaging of female patients in the adult age group >18 years presenting with palpable breast mass. The recommendations according to the age group are as follows:
ADULT FEMALE, 40 YEARS OF AGE OR OLDER, PALPABLE BREAST MASS:
Variant 1: Initial imaging.
1. Mammography diagnostic:
In women 40 years of age or older with palpable breast mass, mammography is the initial diagnostic imaging modality of choice. Both breasts should be imaged in two views; craniocaudal and mediolateral oblique views enabling the entire breast to be completely screened for any additional lesions. The exam should be done under the supervision of a radiologist and a small radiopaque marker can be placed at the site of the palpable abnormality to assess in localizing the lesion.
Strong recommendation
2. Digital breast tomosynthesis diagnostic:
Diagnostic digital breast tomosynthesis (DBT) is recommended as an initial diagnostic tool. A radio-opaque marker can be applied to the skin to indicate its location.
Strong recommendation
3. Ultrasound breast:
Ultrasound of the breast is used following DBT or DM in this age group particularly if the patient has had a negative DM or DBT in the previous six months.
Strong recommendation
Variant 2: Mammography findings are suspicious or highly suggestive of malignancy (BI-RADS 4 or 5). Next imaging study.
1. Ultrasound breast:
Breast ultrasound is the next imaging modality of choice to characterize suspicious findings detected by DM or DBT. The ultrasound should be performed using a high-resolution linear transducer with a minimum frequency of 12 MHz and an adjustable focal zone. Examination of the remainder of the breast and the contralateral breast is recommended to search for any additional suspicious findings.
Strong recommendation
2. Contrast studies (contrast enhanced mammography/contrast MRI):
In women with dense breasts, contrast mammography (CEM) or contrast MRI are recommended for proper staging and to exclude multicentricity/bilaterality.
Conditional recommendation
3. Image guided core biopsy:
Core biopsy should be done for assessment and histological evaluation of suspicious palpable breast abnormalities allowing for tumor receptor status. If a suspicious finding seen by mammography of DBT correlates with the palpable abnormality, biopsy is warranted even with a negative ultrasound. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Strong recommendation
4. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done for the assessment and histological evaluation of suspicious palpable breast abnormalities allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Conditional recommendation
Variant 3: Diagnostic mammography, DBT, and US findings are probably benign (BI-RADS 3). Next imaging study.
1. Mammography:
Breast masses with mammographic features of BIRADS III morphology should undergo 6-, 12- and 24-month surveillance provided that the benign feature of the mass is persistent and there is no upgraded to BIRADS IV or V. Following a 24-month stabilization, the patient will be categorized as definitively benign BIRADS II and resume her normal screening.
Strong recommendation
2. Ultrasound breast:
Breast masses with ultrasound features of BIRADS III morphology should undergo 6-, 12- and 24-month surveillance provided that the benign feature of the mass is persistent and there is no upgraded to BIRADS IV or V. Following a 24-month stabilization, the patient will resume her normal screening. If the mass reduces in size or disappear during the 24-month surveillance, it can be downgraded to BIRADS II
Strong recommendation
3. Image guided core biopsy:
Core biopsy is recommended if the mass is newly developed or has shown a 20% increase in volume or single diameter size. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Strong recommendation
4. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done if the mass is newly developed or has shown a 20% increase in volume or single diameter size allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Conditional recommendation
Variant 4: Mammography findings are benign (BI-RADS 2) at the site of palpable mass. Next imaging study.
1. Ultrasound breast:
When the mammogram shows a benign finding, ultrasound is not necessary considering that there is a certain correlation between the mammographic finding and the clinically palpable abnormality.
If the correlation is uncertain, a targeted ultrasound examination is recommended.
Strong recommendation
2. Image guided core biopsy:
If a suspicious finding is detected by ultrasound, biopsy is recommended. A suspicious clinical examination should warrant biopsy irrespective of the imaging findings.
Strong recommendation
Variant 5: Mammography findings are negative (BI-RADS 1). Next imaging study.
1. Ultrasound breast:
Ultrasound breast should be done in women with a palpable abnormality and a negative mammogram.
Strong recommendation
2. Image guided core biopsy:
If a suspicious finding is detected by ultrasound, biopsy is recommended, A suspicious clinical examination should warrant biopsy irrespective of the imaging findings.
Strong recommendation
ADULT FEMALE, 30 YEARS OF AGE OR YOUNGER, PALPABLE BREAST MASS:
Variant 1: Initial imaging.
1. Ultrasound breast:
Ultrasound is the initial imaging modality of choice preferably targeted to the palpable abnormality.
Strong recommendation
Variant 2: US findings are suspicious or highly suggestive of malignancy (BI-RADS 4 or 5). Next imaging study.
1. Mammography diagnostic:
Mammography is indicated if the suspicious ultrasound finding correlates with the clinically palpable abnormality.
Strong recommendation
2. Digital breast tomosynthesis diagnostic:
DBT is indicated if the suspicious ultrasound finding correlates with the clinically palpable abnormality. DBT demonstrates the true extent of the lesion and exclude contralateral abnormalities particularly in young women with dense breasts.
Strong recommendation
3. Contrast studies (contrast mammography/contrast MRI):
In women with dense breasts, contrast mammography (CEM) or contrast MRI should be recommended for proper staging and to exclude multicentricity/bilaterality.
Conditional recommendation
4. Image guided core biopsy:
Core biopsy should be done for assessment and histological evaluation of suspicious palpable breast abnormalities allowing for tumor receptor status. If a suspicious finding seen by mammography of DBT correlates with the palpable abnormality, biopsy is warranted even with a negative ultrasound. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Strong recommendation
5. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done for the assessment and histological evaluation of suspicious palpable breast abnormalities allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Conditional recommendation
Variant 3: US findings probably benign (BI-RADS 3). Next imaging study.
1. Ultrasound breast:
Breast masses with ultrasound features of BIRADS III morphology should undergo 6-, 12- and 24-month surveillance provided that the benign feature of the mass is persistent and there is no upgraded to BIRADS IV or V. If the mass reduces in size or disappear during the 24-month surveillance, it can be downgraded to BIRADS II
Strong recommendation
2. Image guided core biopsy:
Core biopsy is recommended if the mass is newly developed or has shown a 20% increase in volume or single diameter size. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Strong recommendation
3. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done if the mass is newly developed or has shown a 20% increase in volume or single diameter size allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Conditional recommendation
Variant 4: US findings benign (BI-RADS 2). Next imaging study.
No further imaging required.
Strong recommendation
Variant 5: US findings negative (BI-RADS 1). Next imaging study.
No further imaging required.
Strong recommendation
ADULT FEMALE, 30 to 39 YEARS OF AGE, PALPABLE BREAST MASS.
Same guidelines as adult female 40 years or older.
Strong recommendation
- Introduction
In Egypt, breast cancer is the most common malignancy among females representing 32 % of female cancers with a crude incidence rate of 35.8/1000,00 normal population and an age standardized incidence rate of 48.8/100,000 normal population [5]. Based on the first Egyptian population based national cancer registry published in 2014, the updated statistics according to the World Health Organization (WHO) in Egypt, 2020 for breast cancer is 22,038 new case each year among females with a crude incidence rate of 43.5/100,000 normal population and an age standardized incidence rate of 48.7/100,000 normal population [6].
The most prevalent sign of cancer is a palpable lump, and compared to malignancies found by screening, palpable cancers are typically more aggressive and have worse prognoses [7]. Palpable breast masses may show up in a number of situations, including: before a baseline mammogram; during routine breast self-examination or clinical breast examination; in between routine mammogram screenings; or following an extended absence from mammography due to advanced age or personal preference [8].
Following a comprehensive clinical breast examination, often conducted by the referring physician or a board-certified breast clinician, the radiologist must demonstrate concordance between the imaging findings and the clinically observed mass at that location [1].
When a palpable mass is present, the negative predictive value of mammography with ultrasonography varies from 97.4% to 100% [9-11]. Additionally, when a highly suspicious clinical finding is seen, a negative imaging evaluation shouldn't prevent a biopsy [1].
- Scope and purpose
The purpose of this multidisciplinary guideline is to assess healthcare providers to accurately diagnose and characterize palpable breast mass in female patients by a multimodality imaging approach in a timely manner and to differentiate between benign and suspicious masses that need to be further evaluated with core biopsy.
The target audience:
- General surgeons
- Breast surgeons
- Oncology surgeons
- Oncologists
- Obstetricians and gynecologists
- Methods
A comprehensive search for guidelines was undertaken to identify the most relevant guidelines to consider for adaptation.
inclusion/exclusion criteria followed in the search and retrieval of guidelines to be adapted :
• Selecting only evidence-based guidelines (guideline must include a report on systematic literature searches and explicit links between individual recommendations and their supporting evidence)
• Selecting only national and/or international guidelines
• Specific range of dates for publication (using Guidelines published or updated 2015 and later)
• Selecting peer reviewed publications only
• Selecting guidelines written in English language
• Excluding guidelines written by a single author not on behalf of an organization in order to be valid and comprehensive, a guideline ideally requires multidisciplinary input.
• Excluding guidelines published without references as the panel needs to know whether a thorough literature review was conducted and whether current evidence was used in the preparation of the recommendations.
The following characteristics of the retrieved guidelines were summarized in a table:
• Developing organisation/authors
• Date of publication, posting, and release
• Country/language of publication
• Date of posting and/or release
• Dates of the search used by the source guideline developers
All retrieved Guidelines were screened and appraised using AGREE II instrument (www.agreetrust.org) by at least two members. the panel decided a cut-off point or rank the guidelines (any guideline scoring above 50% on the rigour dimension was retained). These guidelines were adapted mainly from American College of Radiology ACR Appropriateness Criteria®, Palpable Breast Masses update in 2022 with partial incorporation of insights from reputable sources to enhance its comprehensiveness and applicability [1]
Evidence assessment:
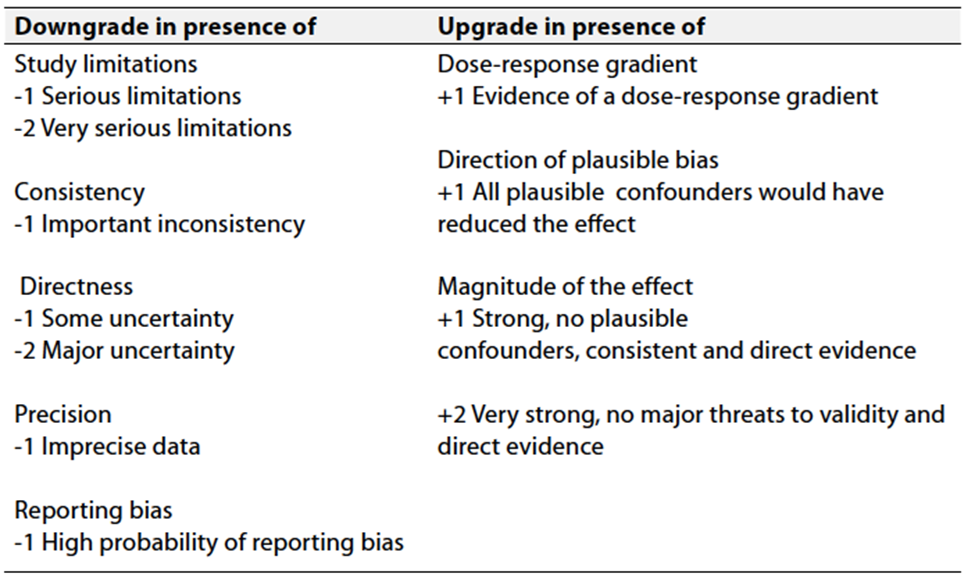
According to WHO handbook for Guidelines we used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess the quality of a body of evidence, develop and report recommendations. GRADE methods are used by WHO because these represent internationally agreed standards for making transparent recommendations. Detailed information on GRADE is available on the following sites:
■ GRADE working group: http://www.gradeworkingroup.org
■ GRADE online training modules: http://cebgrade.mcmaster.ca/
■ GRADE profile software: http://ims.cochrane.org/revman/gradepro
Table 1 Quality of evidence in GRADE
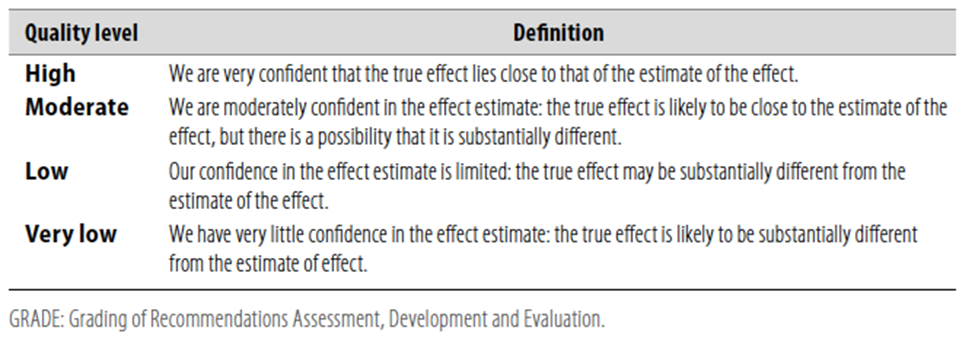
Table 2 Significance of the four levels of evidence

Table 3 Factors that determine How to upgrade or downgrade the quality of evidence.
The strength of the recommendation
The strength of a recommendation communicates the importance of adherence to the recommendation.
Strong recommendations
With strong recommendations, the guideline communicates the message that the desirable effects of adherence to the recommendation outweigh the undesirable effects. This means that in most situations the recommendation can be adopted as policy.
Conditional recommendations
These are made when there is greater uncertainty about the four factors above or if local adaptation has to account for a greater variety in values and preferences, or when resource use makes the intervention suitable for some, but not for other locations. This means that there is a need for substantial debate and involvement of stakeholders before this recommendation can be adopted as policy.
When not to make recommendations
When there is lack of evidence on the effectiveness of an intervention, it may be appropriate not to make a recommendation.
- RECOMMENDATIONS
ADULT FEMALE, 40 YEARS OF AGE OR OLDER, PALPABLE BREAST MASS:
Variant 1: Initial imaging.
1. Mammography diagnostic:
In women 40 years of age or older with palpable breast mass, mammography is the initial diagnostic imaging modality of choice. Both breasts should be imaged in two views; craniocaudal and mediolateral oblique views enabling the entire breast to be completely screened for any additional lesions. The exam should be done under the supervision of a radiologist and a small radiopaque marker can be placed at the site of the palpable abnormality to assess in localizing the lesion.
Remarks: If the patient had a recent mammogram within the last six months, examination of the ipsilateral breast may be considered. Spot compression with or without magnification and supplementary views like exaggerated craniocaudal, cleavage and 90o medio-lateral views may be needed to clarify the nature or the location of the palpable abnormality.
Strong recommendation
High-Quality Evidence (systematic review of guidelines and cross-sectional studies with a consistent reference standard) [1, 12].
2. Digital breast tomosynthesis diagnostic:
Diagnostic digital breast tomosynthesis (DBT) is recommended as an initial diagnostic tool. A radio-opaque marker can be applied to the skin to indicate its location.
Remarks: Previous studies have demonstrated that DBT is as accurate as digital mammography (DM) in the workup of women presenting with palpable breast lumps aided by its thin section multiplanar capabilities using combined DM and DBT or DM alone.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [13, 14].
3. Ultrasound breast:
Ultrasound of the breast is used following DBT or DM in this age group particularly if the patient has had a negative DM or DBT in the previous six months.
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [1, 15]
Variant 2: Mammography findings are suspicious or highly suggestive of malignancy (BI-RADS 4 or 5). Next imaging study.
1. Ultrasound breast:
Breast ultrasound is the next imaging modality of choice to characterize suspicious findings detected by DM or DBT. The ultrasound should be performed using a high-resolution linear transducer with a minimum frequency of 12 MHz and an adjustable focal zone. Examination of the remainder of the breast and the contralateral breast is recommended to search for any additional suspicious findings.
Remarks: A negative ultrasound examination necessitates stereotactic or tomosynthesis guided biopsy of the suspicious mammographic or DBT finding respectively.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [1, 15, 16]
2. Contrast studies (contrast enhanced mammography/contrast MRI):
In women with dense breasts, contrast mammography (CEM) or contrast MRI are recommended for proper staging and to exclude multicentricity/bilaterality.
Remarks: CEM provides superior imaging performance compared to standard mammography and is considered a relatively affordable accessible imaging tool with a sensitivity approaching MRI.
Conditional recommendation
Moderate-Quality Evidence (observational studies and guidelines) [17-22]
3. Image guided core biopsy:
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [1, 23]
4. Image guided fine needle aspiration:
Remarks: Core biopsy is considered a superior highly sensitive and specific diagnostic method compared to image guided FNAB allowing for tumor receptor status.
Conditional recommendation
Moderate-Quality Evidence (observational studies and guidelines) [1, 24]
Variant 3: Diagnostic mammography, DBT, and US findings are probably benign (BI-RADS 3). Next imaging study.
1. Mammography:
Breast masses with mammographic features of BIRADS III morphology should undergo 6-, 12- and 24-month surveillance provided that the benign feature of the mass is persistent and there is no upgraded to BIRADS IV or V. Following a 24-month stabilization, the patient will be categorized as definitively benign BIRADS II and resume her normal screening.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [25, 26]
2. Ultrasound breast:
Breast masses with ultrasound features of BIRADS III morphology should undergo 6-, 12- and 24-month surveillance provided that the benign feature of the mass is persistent and there is no upgraded to BIRADS IV or V. Following a 24-month stabilization, the patient will resume her normal screening. If the mass reduces in size or disappear during the 24-month surveillance, it can be downgraded to BIRADS II
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [25, 27]
3. Image guided core biopsy:
Core biopsy is recommended if the mass is newly developed or has shown a 20% increase in volume or single diameter size. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Remarks: In some situations, biopsy may be recommended even in probably benign lesions like high-risk patients, patients waiting for organ transplantation, individuals with known synchronous malignancies, or patients attempting to conceive. Moreover, circumstances where a biopsy could relieve a patient's acute anxiety could lead to tissue sampling.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [25, 28]
4. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done if the mass is newly developed or has shown a 20% increase in volume or single diameter size allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Remarks: Core biopsy is considered a superior highly sensitive and specific diagnostic method compared to image guided FNAB.
Conditional recommendation
Moderate-Quality Evidence (observational studies and guidelines) [1, 24]
Variant 4: Mammography findings are benign (BI-RADS 2) at the site of palpable mass. Next imaging study.
1. Ultrasound breast:
When the mammogram shows a benign finding, ultrasound is not necessary considering that there is a certain correlation between the mammographic finding and the clinically palpable abnormality.
If the correlation is uncertain, a targeted ultrasound examination is recommended.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [1, 29-31]
2. Image guided core biopsy:
If a suspicious finding is detected by ultrasound, biopsy is recommended. A suspicious clinical examination should warrant biopsy irrespective of the imaging findings.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [1, 31, 32]
Variant 5: Mammography findings are negative (BI-RADS 1). Next imaging study.
1. Ultrasound breast:
Ultrasound breast should be done in women with a palpable abnormality and a negative mammogram.
Remarks: Ultrasound increases the detection of both malignant and benign etiologies. In the assessment of a palpable breast mass, the negative predictive value is quite high—more than 97%—when both mammography and US are negative or benign.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [29, 33, 34]
2. Image guided core biopsy:
If a suspicious finding is detected by ultrasound, biopsy is recommended, A suspicious clinical examination should warrant biopsy irrespective of the imaging findings.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [31, 32, 34]
ADULT FEMALE, 30 YEARS OF AGE OR YOUNGER, PALPABLE BREAST MASS:
Variant 1: Initial imaging.
1. Ultrasound breast
Ultrasound is the initial imaging modality of choice preferably targeted to the palpable abnormality.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference
Standard) [35, 36]
Variant 2: US findings are suspicious or highly suggestive of malignancy (BI-RADS 4 or 5). Next imaging study.
1. Mammography diagnostic:
Mammography is indicated if the suspicious ultrasound finding correlates with the clinically palpable abnormality.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [1, 31]
2. Digital breast tomosynthesis diagnostic:
DBT is indicated if the suspicious ultrasound finding correlates with the clinically palpable abnormality. DBT demonstrates the true extent of the lesion and exclude contralateral abnormalities particularly in young women with dense breasts.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [31, 37]
3. Contrast studies (contrast mammography/contrast MRI):
In women with dense breasts, contrast mammography (CEM) or contrast MRI should be recommended for proper staging and to exclude multicentricity/bilaterality.
Remarks: CEM provides superior imaging performance compared to standard mammography and is considered a relatively affordable accessible imaging tool with a sensitivity approaching MRI.
Conditional recommendation
Moderate-Quality Evidence (observational studies and guidelines) [17-22]
4. Image guided core biopsy:
Core biopsy should be done for assessment and histological evaluation of suspicious palpable breast abnormalities allowing for tumor receptor status. If a suspicious finding seen by mammography of DBT correlates with the palpable abnormality, biopsy is warranted even with a negative ultrasound. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [11, 24]
5. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done for the assessment and histological evaluation of suspicious palpable breast abnormalities allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Remarks: Core biopsy is considered a superior highly sensitive and specific diagnostic method compared to image guided FNAB allowing for tumor receptor status.
Conditional recommendation
Moderate-Quality Evidence (observational studies and guidelines) [11, 24, 25]
Variant 3: US findings probably benign (BI-RADS 3). Next imaging study.
1. Ultrasound breast:
Breast masses with ultrasound features of BIRADS III morphology should undergo 6-, 12- and 24-month surveillance provided that the benign feature of the mass is persistent and there is no upgraded to BIRADS IV or V. If the mass reduces in size or disappear during the 24-month surveillance, it can be downgraded to BIRADS II
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [25-27]
2. Image guided core biopsy:
Core biopsy is recommended if the mass is newly developed or has shown a 20% increase in volume or single diameter size. If the lesion is detected by ultrasound, ultrasound-guided biopsy is the preferred approach as it is and more tolerated by the patient as it avoids breast compression and may allow biopsy for difficult to reach locations by stereotactic biopsy. A radio-opaque clip is placed and a post-biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Remarks: In some situations, biopsy may be recommended even in probably benign lesions like high-risk patients, patients waiting for organ transplantation, individuals with known synchronous malignancies, or patients attempting to conceive. Moreover, circumstances where a biopsy could relieve a patient's acute anxiety could lead to tissue sampling.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference standard) [11, 25, 26, 38]
3. Image guided fine needle aspiration:
Fine needle aspiration biopsy (FNAB) can be done if the mass is newly developed or has shown a 20% increase in volume or single diameter size allowing for faster pathology results but with no difference in therapy timing. A radio-opaque clip is placed and a post aspiration biopsy mammogram or DBT is done to confirm its location and correlation between the ultrasound and mammography/DBT findings.
Remarks: Core biopsy is considered a superior highly sensitive and specific diagnostic method compared to image guided FNAB.
Conditional recommendation
Moderate-Quality Evidence (observational studies and guidelines) [11, 24, 25, 38]
Variant 4: US findings benign (BI-RADS 2). Next imaging study.
No further imaging required.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference
Standard) [1, 35, 36]
Variant 5: US findings negative (BI-RADS 1). Next imaging study.
No further imaging required.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference
Standard) [1, 35, 36]
ADULT FEMALE, 30 to 39 YEARS OF AGE, PALPABLE BREAST MASS.
Same guidelines as adult female 40 years or older.
Strong recommendation
High-Quality Evidence (systematic review of cross-sectional studies with a consistent reference
Standard) [1, 34]
Clinical indicators for monitoring:
Patient file review for the following:
· Proper imaging selection according to the age group.
· Timely initiation of core biopsy procedure in case of suspicious imaging or clinical findings.
· The physician should document follow-up of patients with BIRADS 3 lesions and educate the patient for the importance and the need for follow-up.
These indicators cover aspects such as documentation, diagnostic procedures, and patient education, providing a comprehensive approach to monitoring physician adherence to the clinical guidelines.
Updating the guideline
To keep these recommendations up to date and ensure its validity it will be periodically updated. This will be done whenever strong new evidence is available and necessitates updating.
- REFERENCES
1. Klein KA, Kocher M, Lourenco AP et al (2023) ACR appropriateness criteria® palpable breast masses: 2022 update. J Am Coll Radiol 20:S146-S163. Doi:10.1016/j.jacr.2023.02.013
2. Anonymous (2011) Definition of mass - NCI dictionary of cancer terms - NCI. 2024
3. Patel BK, Lobbes MBI, Lewin J (2018) Contrast enhanced spectral mammography: A review. Seminars in ultrasound, CT, and MRI 39:70-79. Doi:10.1053/j.sult.2017.08.005
4. Anonymous Tomosynthesis (3D mammography). 2024
5. Ibrahim AS, Khaled HM, Mikhail NN, Baraka H, Kamel H (2014) Cancer incidence in egypt: Results of the national population-based cancer registry program. Journal of Cancer Epidemiology 2014:437971-18. Doi:10.1155/2014/437971
6. Anonymous Homepage – IARC. 2024
7. Ma I, Dueck A, Gray R et al (2012) Clinical and self breast examination remain important in the era of modern screening. Ann Surg Oncol 19:1484-1490. Doi:10.1245/s10434-011-2162-9
8. Salzman B, Collins E, Hersh L (2019) Common breast problems. American family physician 99:505-514
9. DENNIS MA, PARKER SH, KLAUS AJ, STAVROS AT, KASKE TI, CLARK SB (2001) Breast biopsy avoidance: The value of normal mammograms and normal sonograms in the setting of a palpable lump. Radiology 219:186-191. Doi:10.1148/radiology.219.1.r01ap35186
10. MOY L, SLANETZ PJ, KOPANS DB et al (2002) Specificity of mammography and US in the evaluation of a palpable abnormality: Retrospective review. Radiology 225:176-181. Doi:10.1148/radiol.2251010999
11. Shetty MK, Shah YP (2002) Prospective evaluation of the value of negative sonographic and mammographic findings in patients with palpable abnormalities of the breast. Journal of ultrasound in medicine 21:1211-1220. Doi:10.7863/jum.2002.21.11.1211
12. Chan CHF, Coopey SB, Freer PE, Hughes KS (2015) False-negative rate of combined mammography and ultrasound for women with palpable breast masses. Breast Cancer Res Treat 153:699-702. Doi:10.1007/s10549-015-3557-2
13. Zuley ML, Guo B, Catullo VJ et al (2014) Comparison of two-dimensional synthesized mammograms versus original digital mammograms alone and in combination with tomosynthesis images. Radiology 271:664-671. Doi:10.1148/radiol.13131530
14. Hawley JR, Kang-Chapman JK, Bonnet SE, Kerger AL, Taylor CR, Erdal BS (2018) Diagnostic accuracy of digital breast tomosynthesis in the evaluation of palpable breast abnormalities. Academic radiology 25:297-304. Doi:10.1016/j.acra.2017.09.016
15. Leung SE, Ben-Nachum I, Kornecki A (2016) New palpable breast lump with recent negative mammogram: Is repeat mammography necessary? American journal of roentgenology (1976) 207:200-204. Doi:10.2214/AJR.15.14799
16. Anonymous (2019) ACR practice parameter for the performance of a breast ultrasound examination. Int Urogynecol J 30:1389-1400. Doi:10.1007/s00192-019-03954-5
17. Pötsch N, Vatteroni G, Clauser P, Helbich TH, Baltzer PAT (2022) Contrast-enhanced mammography versus contrast-enhanced breast MRI: A systematic review and meta-analysis. Radiology 305:94. Doi:10.1148/radiol.212530
18. WARNER E, MESSERSMITH H, CAUSER P, EISEN A, SHUMAK R, PLEWES D (2008) Systematic review: Using magnetic resonance imaging to screen women at high risk for breast cancer. Annals of internal medicine 148:671-679. Doi:10.7326/0003-4819-148-9-200805060-00007
19. Mann RM, Kuhl CK, Moy L (2019) Contrast‐enhanced MRI for breast cancer screening. Journal of magnetic resonance imaging 50:377-390. Doi:10.1002/jmri.26654
20. Jochelson MS, Lobbes MBI (2021) Contrast-enhanced mammography: State of the art. Radiology 299:36-48. Doi:10.1148/radiol.2021201948
21. Kim G, Phillips J, Cole E et al (2019) Comparison of contrast-enhanced mammography with conventional digital mammography in breast cancer screening: A pilot study. Journal of the American College of Radiology 16:1456-1463. Doi:10.1016/j.jacr.2019.04.007
22. Coffey K, Jochelson MS (2022) Contrast-enhanced mammography in breast cancer screening. European journal of radiology 156:110513. Doi:10.1016/j.ejrad.2022.110513
23. Garg S, Mohan H, Bal A, Attri AK, Kochhar S (2007) A comparative analysis of core needle biopsy and fine-needle aspiration cytology in the evaluation of palpable and mammographically detected suspicious breast lesions. Diagnostic cytopathology 35:681-689. Doi:10.1002/dc.20721
24. Ly A, Ono JC, Hughes KS, Pitman MB, Balassanian R (2016) Fine-needle aspiration biopsy of palpable breast masses: Patterns of clinical use and patient experience. Journal of the National Comprehensive Cancer Network 14:527-536. Doi:10.6004/jnccn.2016.0061
25. Polat DS, Merchant K, Hayes J, Omar L, Compton L, Dogan BE (2023) Outcome of imaging and biopsy of BI-RADS category 3 lesions: Follow-up compliance, biopsy, and malignancy rates in a large patient cohort. Journal of ultrasound in medicine 42:1285-1296. Doi:10.1002/jum.16142
26. Buch KA, Qureshi MM, Carpentier B et al (2015) Surveillance of probably benign (BI-RADS 3) lesions in mammography: What is the right follow-up protocol? The breast journal 21:168-174. Doi:10.1111/tbj.12387
27. Lee KA, Talati N, Oudsema R, Steinberger S, Margolies LR (2018) BI-RADS 3: Current and future use of probably benign. Curr Radiol Rep 6:5. Doi:10.1007/s40134-018-0266-8
28. Radiology ACo (2017) ACR practice parameter for the performance of ultrasound-guided percutaneous breast interventional procedures.
29. Durfee SM, Selland DG, Smith DN, Lester SC, Kaelin CM, Meyer JE (2000) Sonographic evaluation of clinically palpable breast cancers invisible on mammography. The breast journal 6:247-251. Doi:10.1046/j.1524-4741.2000.99111.x
30. Harvey JA (2006) Sonography of palpable breast masses. Seminars in ultrasound, CT, and MRI 27:284-297. Doi:10.1053/j.sult.2006.05.003
31. Lehman CD, Lee AY, Lee CI (2014) Imaging management of palpable breast abnormalities. American journal of roentgenology (1976) 203:1142-1153. Doi:10.2214/AJR.14.12725
32. Gumus H, Gumus M, Mills P et al (2012) Clinically palpable breast abnormalities with normal imaging: Is clinically guided biopsy still required? Clinical radiology 67:437-440. Doi:10.1016/j.crad.2011.10.010
33. Ciatto S, Houssami N (2007) Breast imaging and needle biopsy in women with clinically evident breast cancer: Does combined imaging change overall diagnostic sensitivity? Breast (Edinburgh) 16:382-386. Doi:10.1016/j.breast.2007.01.007
34. LEHMAN CD, LEE CI, LOVING VA, PORTILLO MS, PEACOCK S, DEMARTINI WB (2012) Accuracy and value of breast ultrasound for primary imaging evaluation of symptomatic women 30-39 years of age. American journal of roentgenology (1976) 199:1169-1177. Doi:10.2214/AJR.12.8842
35. Harvey JA (2006) Sonography of palpable breast masses. Seminars in ultrasound, CT, and MRI 27:284-297. Doi:10.1053/j.sult.2006.05.003
36. Gonzaga MA (2011) How accurate is ultrasound in evaluating palpable breast masses? The Pan African medical journal 7:1. Doi:10.4314/pamj.v7i1.69094
37. Lee WK, Chung J, Cha E, Lee JE, Kim JH (2016) Digital breast tomosynthesis and breast ultrasound: Additional roles in dense breasts with category 0 at conventional digital mammography. European journal of radiology 85:291-296. Doi:10.1016/j.ejrad.2015.09.026
38. Barr RG, Zhang Z, Cormack JB, Mendelson EB, Berg WA (2013) Probably benign lesions at screening breast US in a population with elevated risk: Prevalence and rate of malignancy in the ACRIN 6666 trial. Radiology 269:701-712. Doi:10.1148/radiol.13122829