Otology
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Otology |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 9:58 PM |
Description
"last update: 28 April 2024"
- Committee
|
|
Chief Editor: Reda Kamel1 General Secretary: Ahmed Ragab2 General Coordinator: Baliegh Hamdy3 Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdel Aziz,6 Tarek Ghanoum,7 Mahmoud Yousef8 Otology Chief Manager: Ali Mahrous12 Assembly board: Sherif Guindi,9 Yasser Shewel,10 Mahmoud Mandour,6 Usama Kamal,11 Ahmed Hesham Galal10 Grading Board (In alphabetical order): Mohamed Abdel Badie,5 Gamal Abdel Fattah,1 Doaa Abdel Halim,12 Ashraf Alhamshary,13 Mahmoud Badr El-Dine,10 Aziz Belal,10 Ezz Eldine Elshikh,14 Fathi Erfan,6 Ayman Fouad,6 Amr Galal,15 Mahmoud Ahmad Hamed,16 Haytham Hassan,10 Nabila Ibrahim,12 Ashraf Lotfy,17 Osama Metwaly,1 Amir Gorguy Mina,10 Waleed Monir,5 Ihab Nada,18 Mahmoud Qotb,9 Mohamed Refaat,19 Ashraf Salah el Dine,17 Yousef Shabana6 Reviewing Board (In alphabetical order): Hani Garem,10 Hisham Hamad,6 Saad El Zayat15 Hesham Taha20 Iman Iskandar21 Lydia Youssef22 Ministry of health ECPG steering committee: Reda Kamel1, Ahmed Ragab2, Mahmoud Abdelaziz6, Mohamed Elsheikh6, Sherif Guindi9, Ali Mahrous12, Louay Sharkawy1, Saad Elzayat15, Ahmed Abu Elwafa23, Iman Sadek20, Mahmoud Yousef8, Samir Halim24, Ahmed Mustafa25, Ehab Seifein 25, Ashraf Lotfy26, Mohamed Eltokhy27, Tamer Azzam27 1Otorhinolaryngology Dep. Faculty of Medicine/Cairo University, 2Otorhinolaryngology Dep. Faculty of Medicine/Menoufia University, 3Otorhinolaryngology Dep. Faculty of Medicine/Minia University, 4Otorhinolaryngology Dep. Faculty of Medicine/Beni-Suef University, 5Otorhinolaryngology Dep. Faculty of Medicine/Mansoura University, 6Otorhinolaryngology Dep. Faculty of Medicine/Tanta University, 7Audiovestibular Unit, Otorhinolaryngology Dep. Faculty of Medicine/Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Dep. Faculty of Medicine/Ain Shams University, 9Otorhinolaryngology Dep. Faculty of Medicine/Fayoum University, 10Otorhinolaryngology Dep. Faculty of Medicine/Alexandria University, 11Otorhinolaryngology Dep. Faculty of Medicine/South Valley University, 12Otorhinolaryngology Dep. Faculty of Medicine/Al Azhar University, 13Otorhinolaryngology Dep. Faculty of Medicine/Banha University, 14Otorhinolaryngology Dep. Faculty of Medicine/Zagazig University, 15Otorhinolaryngology Dep. Faculty of Medicine/Kafr El Shiekh University, 16Otorhinolaryngology Dep. Faculty of Medicine/Sohag University, 17Otorhinolaryngology Dep. Faculty of Medicine/Military Medical Academy, 18Otorhinolaryngology Dep. Faculty of Medicine/Misr University for Science and Technology, 19Otorhinolaryngology Dep. Faculty of Medicine/Suez Canal University Faculty of Medicine/Al Azhar University, 20Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 21Paediatric Dep. Faculty of Medicine/Cairo University, 22Head nurse, Out-patient Clinic, Hayat Medical Center (HMC), 23 Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 24Otorhinolaryngology Department Mataria Teaching Hospital, 25Otorhinolaryngology Department, Faculty of Medicine/ Hearing and Speech Institute, 26Otorhinolaryngology Department Secretariat of the Ministry of Defense, 27Otorhinolaryngology Department Ministry of Interior Medical Services Sector. - Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah |
Abbreviations
|
|
AAP American academy of pediatricians AAFP American academy of family practitioners AOM Acute otitis media CPG Clinical Practice Guideline GRADE Grading of Recommendations Assessment, Development and evaluation MEE Middle ear effusion MRI Magnetic Resonance Imaging OME Otitis media with effusion RCT Randomized controlled trial TM Tympanic membrane |
- Executive Summary
|
|
Chief Editor: Reda Kamel1 General Secretary: Ahmed Ragab2 General Coordinator: Baliegh Hamdy3 Scientific Board: Ashraf Khaled,4 Mohamed Ghonaim,5 Mahmoud Abdel Aziz,6 Tarek Ghanoum,7 Mahmoud Yousef8 Otology Chief Manager: Ali Mahrous12 Assembly board: Sherif Guindi,9 Yasser Shewel,10 Mahmoud Mandour,6 Usama Kamal,11 Ahmed Hesham Galal10 Grading Board (In alphabetical order): Mohamed Abdel Badie,5 Gamal Abdel Fattah,1 Doaa Abdel Halim,12 Ashraf Alhamshary,13 Mahmoud Badr El-Dine,10 Aziz Belal,10 Ezz Eldine Elshikh,14 Fathi Erfan,6 Ayman Fouad,6 Amr Galal,15 Mahmoud Ahmad Hamed,16 Haytham Hassan,10 Nabila Ibrahim,12 Ashraf Lotfy,17 Osama Metwaly,1 Amir Gorguy Mina,10 Waleed Monir,5 Ihab Nada,18 Mahmoud Qotb,9 Mohamed Refaat,19 Ashraf Salah el Dine,17 Yousef Shabana6 Reviewing Board (In alphabetical order): Hani Garem,10 Hisham Hamad,6 Saad El Zayat15 Hesham Taha20 Iman Iskandar21 Lydia Youssef22 Ministry of health ECPG steering committee: Reda Kamel1, Ahmed Ragab2, Mahmoud Abdelaziz6, Mohamed Elsheikh6, Sherif Guindi9, Ali Mahrous12, Louay Sharkawy1, Saad Elzayat15, Ahmed Abu Elwafa23, Iman Sadek20, Mahmoud Yousef8, Samir Halim24, Ahmed Mustafa25, Ehab Seifein 25, Ashraf Lotfy26, Mohamed Eltokhy27, Tamer Azzam27 1Otorhinolaryngology Dep. Faculty of Medicine/Cairo University, 2Otorhinolaryngology Dep. Faculty of Medicine/Menoufia University, 3Otorhinolaryngology Dep. Faculty of Medicine/Minia University, 4Otorhinolaryngology Dep. Faculty of Medicine/Beni-Suef University, 5Otorhinolaryngology Dep. Faculty of Medicine/Mansoura University, 6Otorhinolaryngology Dep. Faculty of Medicine/Tanta University, 7Audiovestibular Unit, Otorhinolaryngology Dep. Faculty of Medicine/Cairo University, 8Phoniatrics Unit, Otorhinolaryngology Dep. Faculty of Medicine/Ain Shams University, 9Otorhinolaryngology Dep. Faculty of Medicine/Fayoum University, 10Otorhinolaryngology Dep. Faculty of Medicine/Alexandria University, 11Otorhinolaryngology Dep. Faculty of Medicine/South Valley University, 12Otorhinolaryngology Dep. Faculty of Medicine/Al Azhar University, 13Otorhinolaryngology Dep. Faculty of Medicine/Banha University, 14Otorhinolaryngology Dep. Faculty of Medicine/Zagazig University, 15Otorhinolaryngology Dep. Faculty of Medicine/Kafr El Shiekh University, 16Otorhinolaryngology Dep. Faculty of Medicine/Sohag University, 17Otorhinolaryngology Dep. Faculty of Medicine/Military Medical Academy, 18Otorhinolaryngology Dep. Faculty of Medicine/Misr University for Science and Technology, 19Otorhinolaryngology Dep. Faculty of Medicine/Suez Canal University Faculty of Medicine/Al Azhar University, 20Audiovestibular Unit, Otorhinolaryngology Department, Faculty of Medicine/ Ain Shams University, 21Paediatric Dep. Faculty of Medicine/Cairo University, 22Head nurse, Out-patient Clinic, Hayat Medical Center (HMC), 23 Otorhinolaryngology Department, Faculty of Medicine/ Assiut University, 24Otorhinolaryngology Department Mataria Teaching Hospital, 25Otorhinolaryngology Department, Faculty of Medicine/ Hearing and Speech Institute, 26Otorhinolaryngology Department Secretariat of the Ministry of Defense, 27Otorhinolaryngology Department Ministry of Interior Medical Services Sector. - Sincere thanks extend to the secretaries: Samar Hussein and Eman Ragab, as well as the editor: Mohamed Salah |
Abbreviations
|
|
AAP American academy of pediatricians AAFP American academy of family practitioners AOM Acute otitis media CPG Clinical Practice Guideline GRADE Grading of Recommendations Assessment, Development and evaluation MEE Middle ear effusion MRI Magnetic Resonance Imaging OME Otitis media with effusion RCT Randomized controlled trial TM Tympanic membrane |
- Introduction
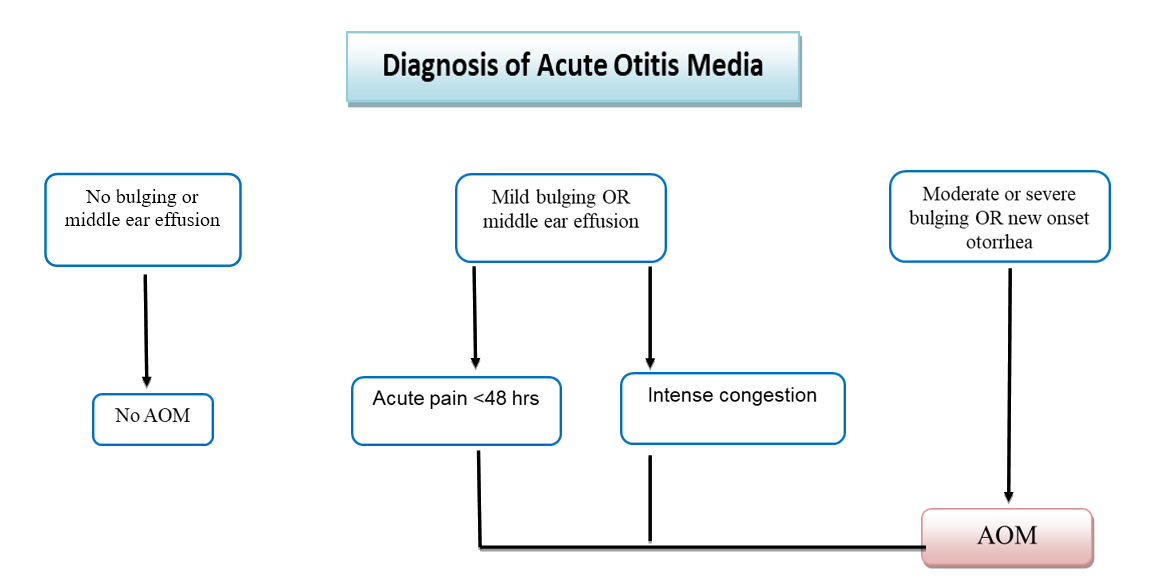
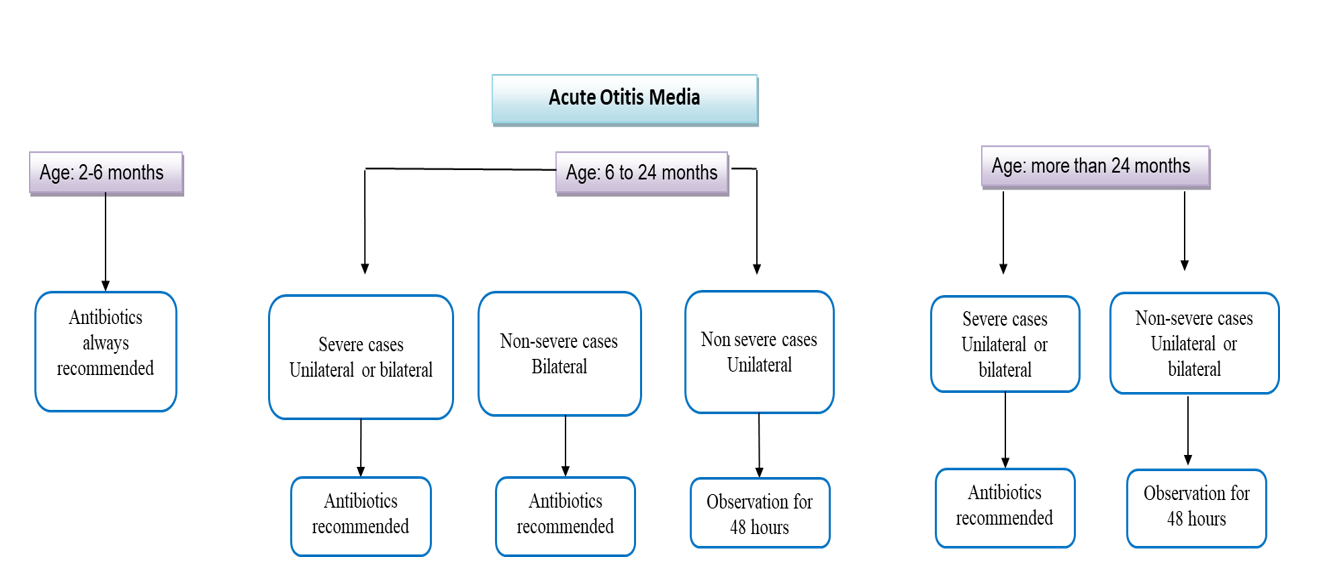
➡️Introduction and definitionsAcute otitis media (AOM) is defined as the presence of inflammation in the middle ear cleft with an effusion. The onset of symptoms and signs is rapid. It should be differentiated from otitis media with effusion (OME) 1 Otitis media with effusion OME; inflammation of the middle ear with fluid collected in the middle ear and absence of signs and symptoms of acute infection. 2 Middle ear effusion MEE; liquid in the middle ear without reference to etiology, pathogenesis, pathology, or duration 2 Persistent otitis; Persistence or worsening of symptoms after the initial management 3 Recurrent otitis media; three or more documented and separate episodes of AOM within 6 months or four or more episodes within 12 months with at least one episode in the past 6 months. 4 Uncomplicated AOM; AOM without otorrhoea 5 Non-severe AOM; AOM with the presence of mild otalgia and a temperature below 39°C 6 Severe AOM; AOM with the presence of moderate to severe otalgia or fever equal to or higher than 39°C 6 Tympanometry; measuring acoustic immittance (transfer of acoustic energy) of the ear as a function of ear canal air pressure 7 Initial antibiotic therapy; treatment of AOM with antibiotics that are prescribed at the time of diagnosis with the intent of starting antibiotic therapy as soon as possible after the encounter 8 Initial observation; initial management of AOM limited to symptomatic relief, with commencement of antibiotic therapy only if the child’s condition worsens at any time or does not show clinical improvement within 48 to 72 hours of diagnosis. 9 ➡️PurposeThe main goal of this guideline is to establish uniformity in the assessment and management of children with acute otitis media. To reach a proper diagnosis of AOM and exclude other causes of pain and hearing loss in children. Direct to proper management, and advise when to prescribe the proper antibiotic if and when needed, to improve the quality of life of our patients. The primary outcome of interest was the total antibiotic prescription incidence for AOM. Secondary outcomes included the type of antibiotic prescribed and the prescription of analgesics. ➡️Scope:The scope of the guideline is the diagnosis and management of AOM and recurrent AOM in children 6 months and older without any underlying conditions. The guideline also aims at recommending the different ways of preventing recurrence of AOM. ➡️Target audience:ENT, Pediatricians and family physicians, to be used for management and/or appropriate referral of children with acute otitis media. |
- Methods
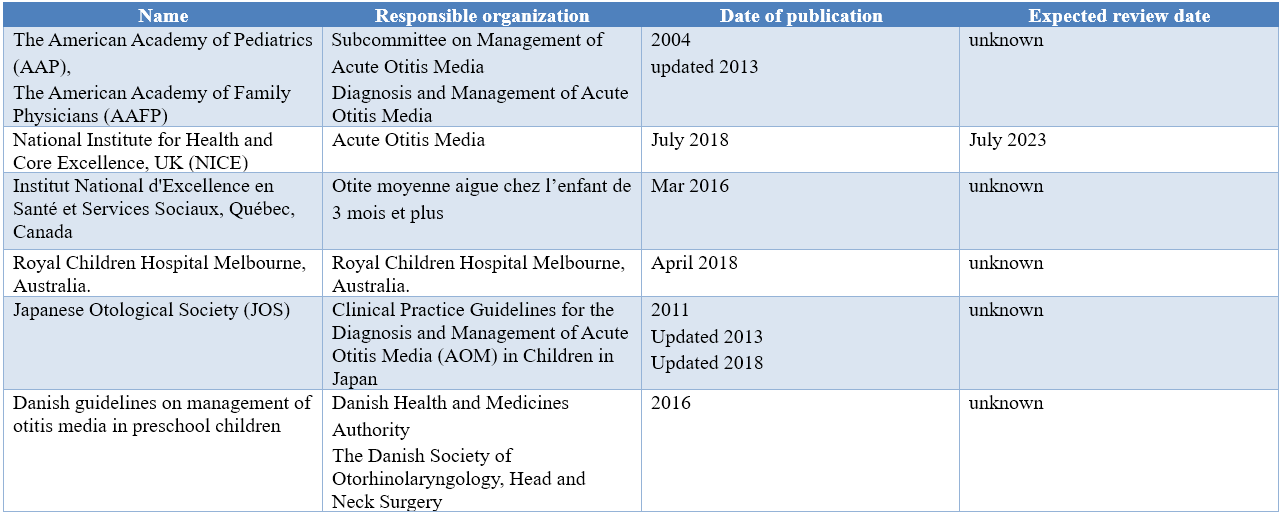
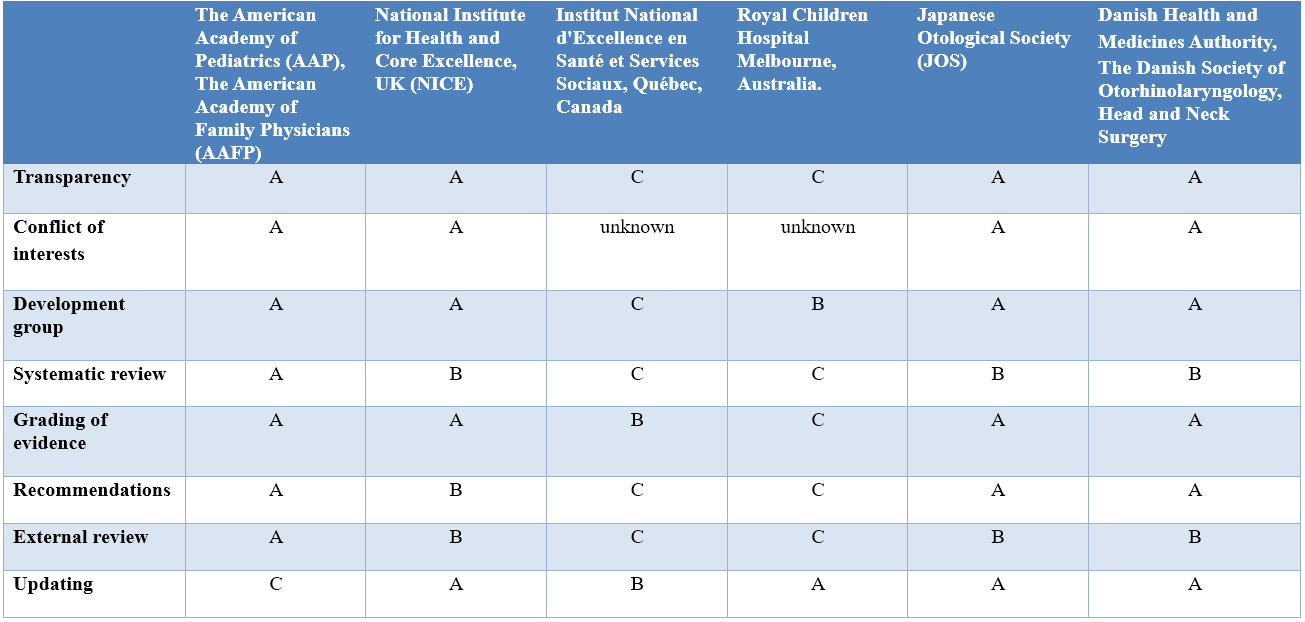
➡️Methods of development Stakeholder Involvement: Individuals who were involved in the development process. Including the above-mentioned Otology Chief Manager, Otology Executive Manager, Assembly Board, Grading Board and Reviewing Board. Information about target population experiences were not applicable for this topic. ➡️Search methodElectronic database searched: Pubmed, Medline, Egyptian Knowledge Bank, Medscape, WebMD, Google Scholar ➡️Keywords:Acute Otitis Media, Guidelines, Children The adaptation cycle passed over: set-up phase, adaptation phase (Search and screen, assessment: currency, content, quality & /decision/selection) and finalization phase that included revision and external reviewing. Time period searched: from January 2004 to December 2020. ➡️ResultsFive national otorhinolaryngologists reviewed the guidelines available. Guidelines from the American Academy of Pediatrics (AAP) and American Academy of Family Physicians gained the highest scores as regards currency, contents and quality. It was graded GRADE by twenty two experts and reviewed by six expert reviewers to improve quality, gather feedback on draft recommendations. The external review was done through a rating scale as well as open-ended questions. Setting: Primary, secondary and tertiary care centers & hospitals, and related specialties. |
Interpretation of strong and conditional recommendations for an intervention 10
|
Audience |
Strong recommendation |
Conditional recommendation |
|
Patients |
Most individuals in this situation would want the recommended course of action; only a small proportion would not. Formal decision aides are not likely to be needed to help individuals make decisions consistent with their values and preferences. |
Most individuals in this situation would want the suggested course of action, but many would not |
|
Clinicians |
Most individuals should receive the intervention. Adherence to the recommendation could be used as a quality criterion or performance indicator. |
Different choices will be appropriate for individual patients, who will require assistance in arriving at a management decision consistent with his or her values and preferences. Decision aides may be useful in helping individuals make decisions consistent with their values and preferences. |
|
Policymakers |
The recommendation can be adopted as policy in most situations. |
Policy-making will require substantial debate and involvement of various stakeholders. |
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to Decision frameworks (GRADE Working Group 2013)
|
Grade |
Definition |
|
High
|
We are very confident that the true effect lies close to that of the estimate of the effect. |
|
Moderate
|
We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
|
Low
|
Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
|
Very Low
|
We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect |
- Recommendations
|
|
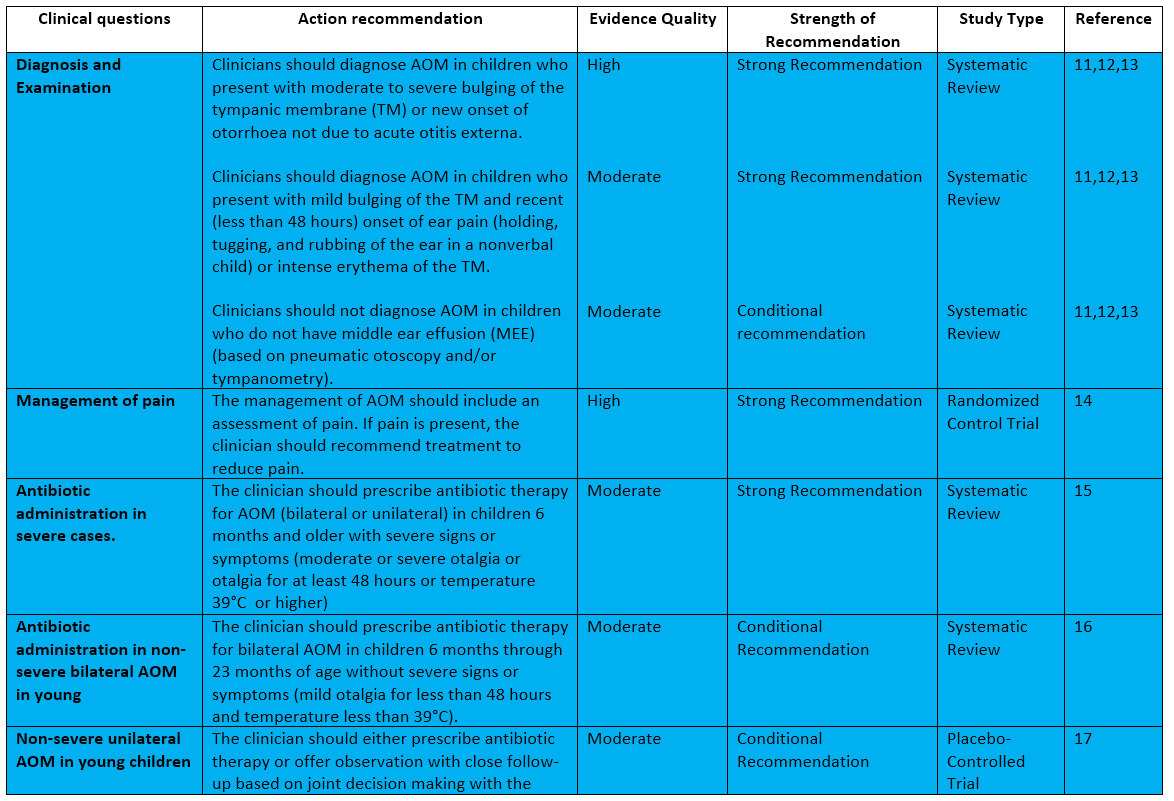
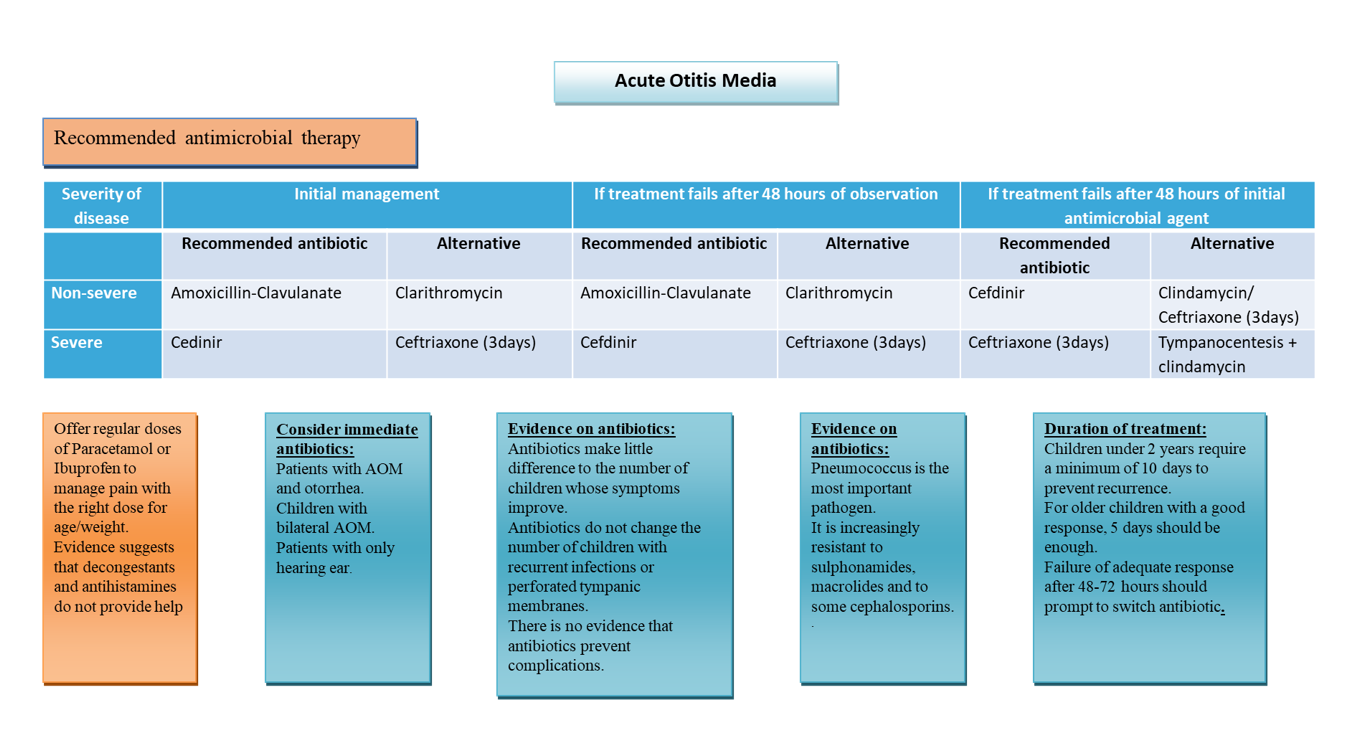
The following statements and flowchart were adapted from the Guidelines from the American Academy of Pediatrics (AAP) and American Academy of Family Physicians which received the highest scores as regards the currency, contents, and quality. |
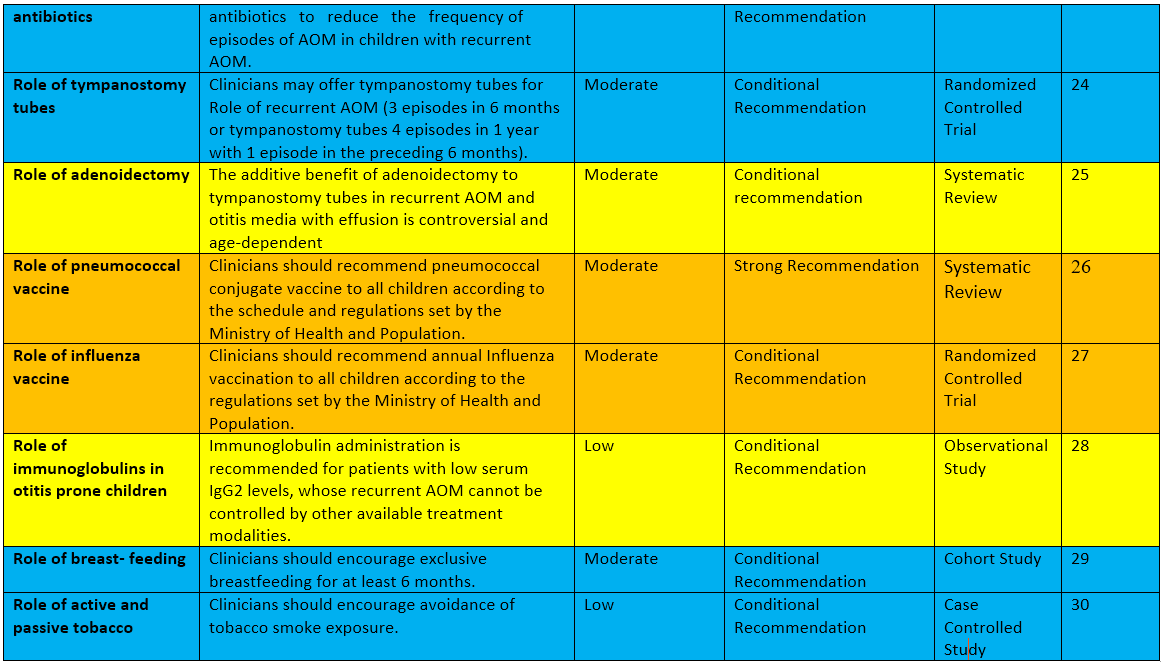
Recommendations statements
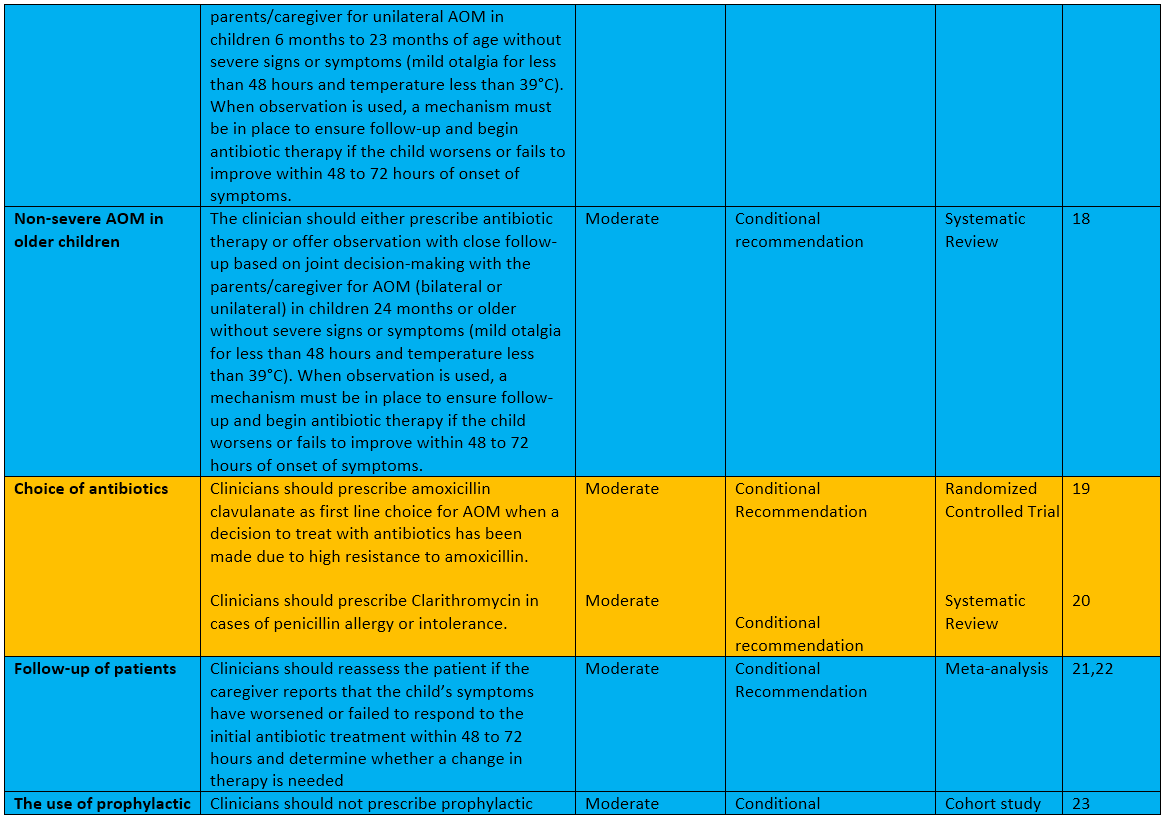
- Monitoring and evaluating the impact of the guideline
Monitoring/ Auditing Criteria:
· Management of pain with analgesics
· Administration of amoxicillin-clavulanate as the first choice antibiotic treatment when a decision to treat with antibiotics has been made
- Updating of the guideline
Updating Procedure:
Any recommendation of this guideline will be updated when new evidence that could potentially impact the current evidence base for this recommendation is identified. If no new reports or information are identified for a particular recommendation, the recommendation will be revalidated. The focus will be on recommendations supported by very-low- or low certainty evidence and where new recommendations or a change in the published recommendations may be needed.
- References
|
1. The diagnosis and management of acute otitis media. Lieberthal AS, Carroll AE, Chonmaitree T, et al. Pediatrics. 2013;131:0–99. 2. Bluestone CD. Definitions, terminology, and classification. In: Rosenfeld RM, Bluestone CD, eds. Evidence-Based Otitis Media. Hamilton, Canada: BC Decker; 2003:120–135 3. Schilder AG, Chonmaitree T, Cripps AW, Rosenfeld RM, Casselbrant ML, Haggard MP, Venekamp RP. Otitis media. Nat Rev Dis Primers. 2016 Sep 8;2(1):16063. doi: 10.1038/nrdp.2016.63. PMID: 27604644; PMCID: PMC7097351. 4. Jamal A, Alsabea A, Tarakmeh M, Safar A. Etiology, Diagnosis, Complications, and Management of Acute Otitis Media in Children. Cureus. 2022 Aug 15;14(8):e28019. doi: 10.7759/cureus.28019. PMID: 36134092; PMCID: PMC9471510. 5. American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113(5):1451–1465 6. Bluestone CD, Klein JO. Definitions, terminology, and classification. In: Bluestone CD, Klein JO, eds. Otitis Media in Infants and Children. 4th ed. Hamilton, Canada: BC Decker; 2007:1–19 7. Bluestone CD, Klein JO. Diagnosis. In: Otitis Media in Infants and Children. 4th ed. Hamilton, Canada: BC Decker; 2007:147–212 8. Stevanovic T, Komazec Z, Lemajic-Komazec S, Jovic R, Acute otitis media: To follow-up or treat?, International Journal of Pediatric Otorhinolaryngology, Volume 74, Issue 8, 2010, Pages 930-933, ISSN 0165-5876 9. Sakulchit T, Goldman RD. Antibiotic therapy for children with acute otitis media. Can Fam Physician. 2017 Sep;63(9):685-687. PMID: 28904032; PMCID: PMC5597011. 10. WHO handbook for guideline development – 2nd ed. (ISBN 978 92 4 154896 0) © World Health Organization 2014 11.The diagnosis and management of acute otitis media. Lieberthal AS, Carroll AE, Chonmaitree T, et al. Pediatrics. 2013;131:0–99. 12. Bluestone CD. Definitions, terminology, and classification. In: Rosenfeld RM, Bluestone CD, eds. Evidence-Based Otitis Media. Hamilton, Canada: BC Decker; 2003:120–135 13. Schilder AG, Chonmaitree T, Cripps AW, Rosenfeld RM, Casselbrant ML, Haggard MP, Venekamp RP. Otitis media. Nat Rev Dis Primers. 2016 Sep 8;2(1):16063. doi: 10.1038/nrdp.2016.63. PMID: 27604644; PMCID: PMC7097351. 14. Bertin L, Pons G, d’Athis P, et al. A randomized, double-blind, multicentre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam Clin Pharmacol. 1996;10(4):387–392 15. Coker TR, Chan LS, Newberry SJ, et al. Diagnosis, microbial epidemiology, and antibiotic treatment of acute otitis media in children: a systematic review. JAMA.2010;304(19):2161–2169 16. Sanders S, Glasziou PP, DelMar C, Rovers M. Antibiotics for acute otitis media in children [review]. Cochrane Database Syst Rev. 2009;(2):1–43 17. Tähtinen PA, Laine MK, Huovinen P, Jalava J, Ruuskanen O, Ruohola A. A placebo controlled trial of antimicrobial treatment for acute otitis media. N Engl J Med. 2011;364(2):116–126 18. Spurling GK, Del Mar CB, Dooley L, Foxlee R. Delayed antibiotics for respiratory infections. Cochrane Database Syst Rev. 2007;(3):CD004417 19. Hoberman et al. Treatment of Acute Otitis Media in Children under 2 Years of Age. N Engl J Med; 364:105-115 (2011) 20. Spoială EL, Stanciu GD, Bild V, Ababei DC, Gavrilovici C. From Evidence to Clinical Guidelines in Antibiotic Treatment in Acute Otitis Media in Children. Antibiotics (Basel). 2021 Jan 6;10(1):52. doi: 10.3390/antibiotics10010052. PMID: 33419114; PMCID: PMC7825459. 21. Nitsche MP, Carreño M. Antibiotics for acute otitis media in children. Medwave. 2015;15(Suppl 2):e6295. 22. Marcy M, Takata G, Shekelle P, et al. Management of Acute Otitis Media. Evidence Report/Technology Assessment No. 15. Rockville, MD: Agency for Healthcare Research and Quality; 2000 23.Teele DW, Klein JO, Word BM, et al; Greater Boston Otitis Media Study Group. Antimicrobial prophylaxis for infants at risk for recurrent acute otitis media. Vaccine. 2000;19(suppl 1):S140–S143 24. Gonzalez C, Arnold JE, Woody EA, et al. Prevention of recurrent acute otitis media: chemoprophylaxis versus tympanostomy tubes. Laryngoscope. 1986;96(12): 1330–1334 25. Schilder et al. Panel 7: Otitis Media: Treatment and Complications.Otolaryngol Head Neck Surg; Apr;156(4_suppl):S88-S105(2017) 26. Jansen AG, Hak E, Veenhoven RH, Damoiseaux RA, Schilder AG, Sanders EA. Pneumococcal conjugate vaccines for preventing otitis media. Cochrane Database Syst Rev. 2009;(2):CD001480 27. Heikkinen T, Ruuskanen O, Waris M, Ziegler T, Arola M, Halonen P. Influenza vaccination in the prevention of acute otitis media in children. Am J Dis Child. 1991;145(4):445–448 28. Veenhoven, R., et al. Immunoglobulins in Otitis-Prone Children. Pediatr Res 55, 159–162 (2004). 29. Scariati PD, Grummer-Strawn LM, Fein SB. A longitudinal analysis of infant morbidity and the extent of breastfeeding in the United States. Pediatrics. 1997;99(6). Available at: www.pediatrics.org/cgi/content/full/99/6/e5 30. Ilicali OC, Keles¸ N, Deger K, Savas¸ I. Relationship of passive cigarette smoking to otitis media. Arch Otolaryngol Head Neck Surg. 1999;125(7):758–762 Further Reading· Lieberthal AS, Carroll AE, Chonmaitree T, et al. Clinical Practice Guideline: The Diagnosis and Management of Acute Otitis Media. Pediatrics. 2013;131(3):e964– e999 · Sabella, Goldfarb J, Applying new guidelines on acute otitis media: from principles to practice. Cleveland Clinic Journal of Medicine, supplement 4 to volume 71, June 2004. · Marchisio P, Bellussi L, Di Mauro G, Doria M, Felisati G, Longhi R, Novelli A, Speciale A, Mansi N, Principi N. Acute otitis media: From diagnosis to prevention. Summary of the Italian guideline. Int J Pediatr Otorhinolaryngol. 2010;74(11):1209-16. · Kitamura K, Iino Y, Kamide Y, Kudo F, Nakayama T, Suzuki K, Taiji H, Takahashi H, Yamanaka N, Uno Y. Clinical practice guidelines for the diagnosis and management of acute otitis media (AOM) in children in Japan - 2013 update. Auris Nasus Larynx. 2015;42(2):99-106. · Heidemann CH, Lous J, Berg J, Christensen JJ, Håkonsen SJ, Jakobsen M, Johansen CJ, Nielsen LH, Hansen MP, Poulsen A, Schousboe LP, Skrubbeltrang C, Vind AB, Homøe P. Danish guidelines on management of otitis media in preschool children. Int J Pediatr Otorhinolaryngol. 2016;87:154-63. · Institut National d’Excellence en Santé et Services Sociaux (INESSS), Otite moyenne aigue chez l’enfant de 3 mois et plus, published date 2016, Québec, Canada, https://www.inesss.qc.ca/ fileadmin/doc/CDM/UsageOptimal/Guides-serieI/ Guide-Otite-Enfant.pdf. · Ovnat Tamir S, Shemesh S, Oron Y, Marom T. Acute otitis media guidelines in selected developed and developing countries: uniformity and diversity. Arch Dis Child. 2017;102(5):450-457. · Deniz Y, van Uum RT, de Hoog MLA, Schilder AGM, Damoiseaux RAMJ, Venekamp RP. Impact of acute otitis media clinical practice guidelines on antibiotic and analgesic prescriptions: a systematic review. Arch Dis Child. 2018;103(6):597-602. 10.1136. · National Institute for Health and Care Excellence; Otitis media (acute): antimicrobial prescribing NICE guideline [NG91] Published date: 28 March 2018, https://www.nice.org.uk/guidance/ng91. · Royal Children Hospital Melbourne, Australia; Acute Otitis media Guidelines, 2018, https://www.rch.org. au/clinicalguide/guideline_index/Acute_otitis_media. · Bourgeois T, Griffith C, Johnson EC, Leblanc B, Melancon B. Barriers to Current Guidelines in the Management of Pediatric Acute Otitis Media. J Pediatrics & Pediatr Med. 2019;3(3):7-24. · Hayashi T, Kitamura K, Hashimoto S, Hotomi M, Kojima H, Kudo F, Maruyama Y, Sawada S, Taiji H, Takahashi G, Takahashi H, Uno Y, Yano H. Clinical practice guidelines for the diagnosis and management of acute otitis media in children-2018 update. Auris Nasus Larynx. 2020;47(4):493-526. · Suzuki HG, Dewez JE, Nijman RG, Yeung S. Clinical practice guidelines for acute otitis media in children: a systematic review and appraisal of European national guidelines. BMJ Open. 2020;10(5). · Veenhoven, R., Rijkers, G., Schilder, A. et al. Immunoglobulins in Otitis-Prone Children. Pediatr Res. 2004;55:159–162. · Guidelines Review Committee, Quality Assurance of Norms and Standards. WHO handbook for guideline development, 2nd Editio, Chapter 10 page 129 · Schünemann, Brożek, Guyatt, Oxman GRADE Handbook, Chapter 5; Quality of evidence, 2013 |
- Annexes
Editorial Independence:
· This guideline was developed without any external funding.
All the guideline development group members have declared that they do not have any competing interests.Annex 1: Guideline Flowchart
Annex 2: Tables of appraisal of selected guidelines: Currency (table 1), Content (table 2) and Quality (table 3) of the selected guidelines.

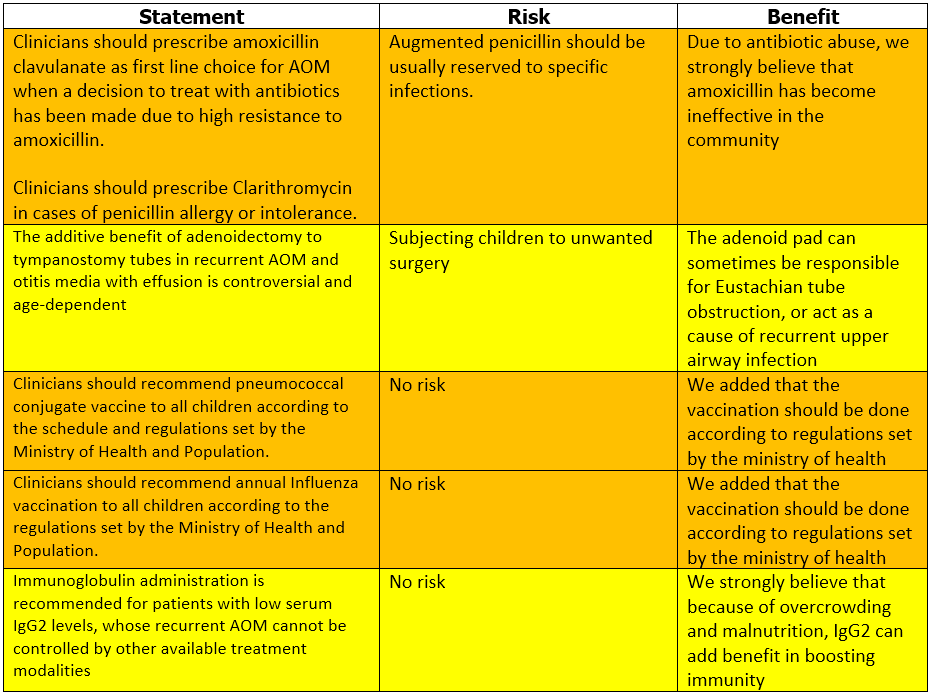
Annex 3: The risks and benefits of added and/or modified statements