Voice disorders
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Voice disorders |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:27 PM |
Description
"last update: 28 April 2024"
- Committee
➡️Chair of the Panel:
Usama Abdel Naseer
➡️Scientific Group Members:
Abdalla Anayet, Abdelrahman Eltahaan, Ahmed Mostafa, Alaa Gaafar, Amr Taha, Ashraf Lotfy, Athar Reda Ibrahim, Bahaa Eltoukhy, Haytham Elfarargy, Hazem Dewidar, Ihab Sifin, Loay Elsharkawy, Mai Mohammed Salama, Mina Esmat, Rania Abdou, Reda Sharkawy, Saad Elzayat, Samir Halim.
➡️Abbreviations
VD: voice disorders
➡️Glossary:
Dysphonia: Altered vocal quality, pitch, loudness, or vocal effort that impairs communication as assessed by a clinician and/or affects quality of life
Patient-reported outcome measures: subjective evaluation by patients with voice disorders, the Voice Handicap Index (VHI) and Voice-Related Quality of Life (V-RQOL) were developed from the viewpoint of the disorders’ effects on patient quality of life.
Stroboscope: Advanced laryngeal imaging designed to visualize vocal fold vibratory abnormalities that cannot be appreciated with continuous light laryngoscopy. It uses a synchronized flashing light that passes through a laryngoscope
The aerodynamic assessment : is defined as “individual or combined measurements of voice strength, pitch, expiratory flow in phonation and maximum phonation time (MPT)” . This method enables examiners to understand the pathological conditions related to vocal-fold vibration, and it is useful to compare the patient’s voice before and after treatment
Acoustic analysis is an objective evaluation of voice disorders that analyzes speech signals and provides quantitative evaluations.
Voice therapy: is provided for dysphonia with no morphological abnormality. Voice therapy is also applicable to motor diseases, such as vocal-fold paralysis, Parkinson’s disease, or psychogenic vocal disorders. Voice therapy has a long history both in direct and indirect therapy, and methodologies of the therapies based on various theoretical systems have been developed, but its classification or application has not been established adequately
➡️Scope
This Guideline is concerned with diagnosis and treatment decision of voice disorders affecting children and adults
- Executive Summary
· In the GRBAS Scales, four grades of scale are recommended because of their high reproduction rate and sufficient resolution
· Using the VHI and V-RQOL as patient-reported outcome measures They are, strongly recommended as subjective evaluation tools for voice disorders as they are highly reliable and validated
· Laryngoscopy is an essential tool for visualization of the larynx to diagnose the cause of dysphonia
· Laryngostroboscopy is useful for diagnosis of voice disorders. It is also useful for the diagnosis and monitoring. Laryngostroboscopy was useful for the diagnosis of patients with voice disorders in 27.2% of cases
· Acoustic analysis is useful in objective evaluation of voice disorders, especially for evaluating effectiveness of treatment.
· measurement of voice strength, measurement of pitch, measurement of expiratory flow in phonation, measurement of MPT, measured individually or combined
· clinicians should advocate voice therapy for patients with dysphonia from a cause amenable to voice therapy
· Clinicians should inform patients with dysphonia about control/preventive measures
· Clinicians should document resolution, improvement, or worsened symptoms of dysphonia or change in QOL among patients with dysphonia after treatment or observation.
➡️Purpose
Appraisal of the research evidence that exists to support the use of voice measures in the clinical assessment of patients with voice disorders. And outline the measures used in the management of Functional voice disorders.
Specifically, the goals are to improve diagnostic accuracy, identify cases who are most susceptible to voice disorders, and educate clinicians and patients regarding voice disorders
➡️The target audience
The guideline is intended for all clinicians who are likely to diagnose and manage voice disorders
- Methods
A comprehensive search for guidelines was undertaken to identify the most relevant guidelines to consider for adaptation.
inclusion/exclusion criteria followed in the search and retrieval of guidelines to be adapted:
· Selecting only evidence-based guidelines (guideline must include a report on systematic literature searches and explicit links between individual recommendations and their supporting evidence)
· Selecting only national and/or international guidelines
· Specific range of dates for publication (using Guidelines published or updated 2013 and later)
· Selecting peer reviewed publications only
· Selecting guidelines written in English language
· Excluding guidelines written by a single author not on behalf of an organization in order to be valid and comprehensive, a guideline ideally requires multidisciplinary input
· Excluding guidelines published without references as the panel needs to know whether a thorough literature review was conducted and whether current evidence was used in the preparation of the recommendations
The following characteristics of the retrieved guidelines were summarized in a table:
• Developing organisation/authors
• Date of publication, posting, and release
• Country/language of publication
• Date of posting and/or release
• Dates of the search used by the source guideline developers
All retrieved Guidelines were screened and appraised using AGREE II instrument (www.agreetrust.org) by at least two members. the panel decided a cut-off point or rank the guidelines (any guideline scoring above 50% on the rigour dimension was retained)
Evidence assessment
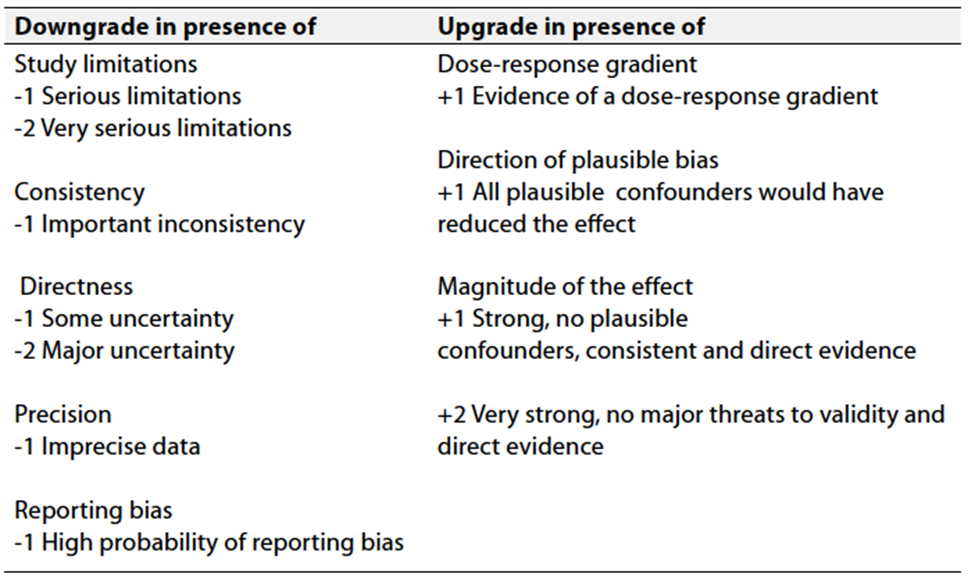
According to WHO handbook for Guidelines we used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess the quality of a body of evidence, develop and report recommendations. GRADE methods are used by WHO because these represent internationally agreed standards for making transparent recommendations. Detailed information on GRADE is available on the following sites:
■ GRADE working group: http://www.gradeworkingroup.org
■ GRADE online training modules: http://cebgrade.mcmaster.ca/
■ GRADE profile software: http://ims.cochrane.org/revman/gradepro
Table 1 Quality of evidence in GRADE
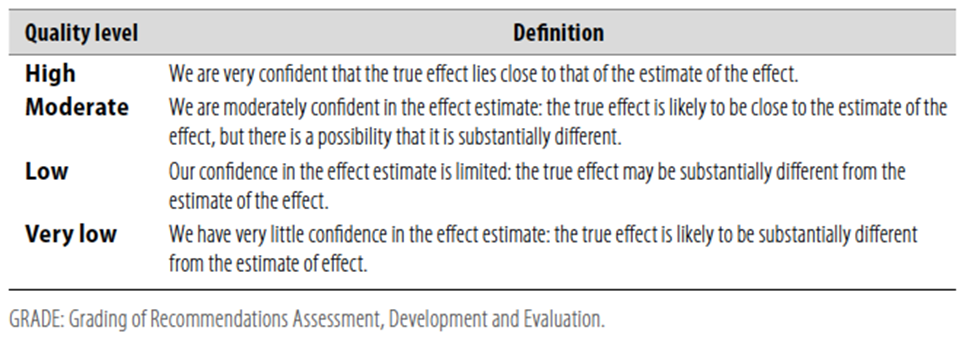
Table 2 Significance of the four levels of evidence
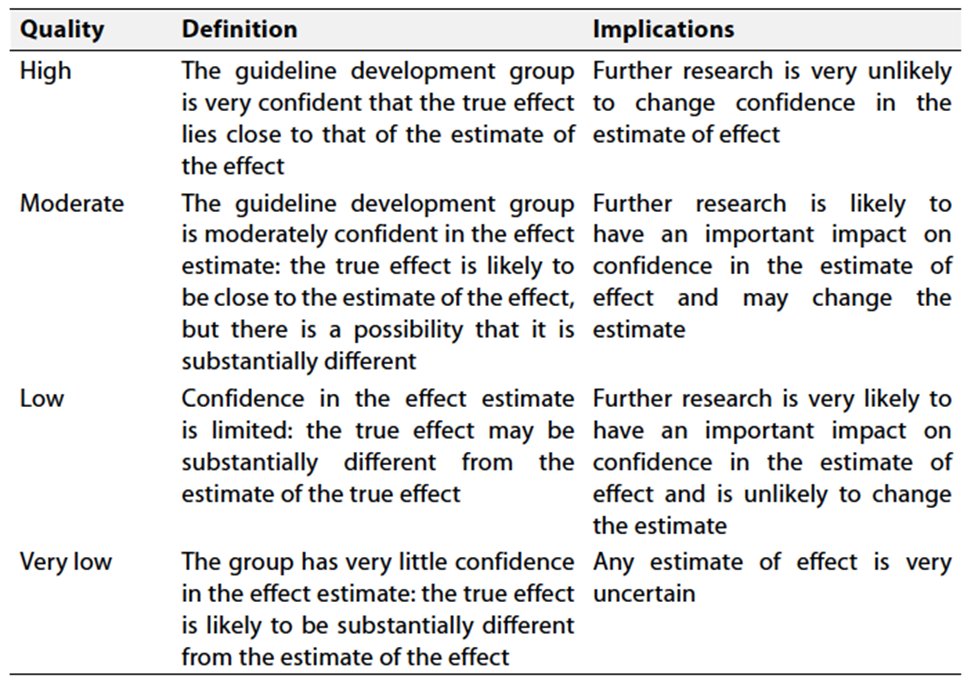
Table 3 Factors that determine How to upgrade or downgrade the quality of evidence
- The strength of the recommendation
The strength of a recommendation communicates the importance of adherence to the recommendation.
➡️Strong recommendations
With strong recommendations, the guideline communicates the message that the desirable effects of adherence to the recommendation outweigh the undesirable effects. This means that in most situations the recommendation can be adopted as policy.
➡️Conditional recommendations
These are made when there is greater uncertainty about the four factors above or if local adaptation has to account for a greater variety in values and preferences, or when resource use makes the intervention suitable for some, but not for other locations. This means that there is a need for substantial debate and involvement of stakeholders before this recommendation can be adopted as policy.
When not to make recommendations
When there is lack of evidence on the effectiveness of an intervention, it may be appropriate not to make a recommendation- Recommendations
|
|
|
Evidence-Based Statements (recommendation levels ) |
Grades / Levels of Evidence |
|
1.
The
use of GRBAS Scales for voice quality evaluation?
|
In the GRBAS Scales, four grades of scale are recommended because of their high reproduction rate and sufficient resolution |
Strong Recommendation |
A |
|
2. Using the VHI and V-RQOL as patient-reported outcome measures?
|
They are, strongly recommended as subjective evaluation tools for voice disorders as they are highly reliable and validated |
Strong Recommendation |
A |
|
3. Laryngoscopy use for the assessment of dysphonia?.
|
Laryngoscopy is an essential tool for visualization of the larynx to diagnose the cause of dysphonia |
Strong Recommendation |
A |
|
4. The use of laryngostroboscopy in dysphonia?
|
Laryngostroboscopy is useful for diagnosis of voice disorders. It is also useful for the diagnosis and monitoring. Laryngostroboscopy was useful for the diagnosis of patients with voice disorders in 27.2% of cases |
Recommendation |
C |
|
5. Using acoustic analysis of voice clinically
|
Acoustic analysis is useful in objective evaluation of voice disorders, especially for evaluating effectiveness of treatment. |
Recommendation |
C |
|
6. The use of aerodynamic assessment of voice disorders
|
measurement of voice strength, measurement of pitch, measurement of expiratory flow in phonation, measurement of MPT, measured individually or combined |
Recommendation |
C |
|
7. Antireflux medication |
Clinicians should notprescribe antireflux medications to treat isolated dysphonia based on symptoms alone attributed to suspected gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR), without visualization of the larynx |
Recommendation against |
C
|
|
8. Corticosteroid therapy |
Clinicians should notroutinely prescribe corticosteroids for patients with dysphonia prior to visualization of the larynx |
Recommendation against |
C
|
|
9. Antimicrobial therapy |
Clinicians should not routinely prescribe antibiotics to treat dysphonia.
|
Strong recommendation against |
A
|
|
10. Advocating for voice therapy |
clinicians should advocate voice therapy for patients with dysphonia from a cause amenable to voice therapy |
Strong recommendation |
A |
|
11. Imaging |
clinicians should not obtain computed tomography (CT) or magnetic resonance imaging (MRI) among patients with a primary voice complaint prior to visualization of the larynx |
Recommendation against |
c |
|
12. Education/prevention. |
Clinicians should inform patients with dysphonia about control/preventive measures |
Recommendation |
C |
|
13. Outcomes |
Clinicians should document resolution, improvement, or worsened symptoms of dysphonia or change in QOL among patients with dysphonia after treatment or observation. |
Recommendation |
C |
Research Needs
1. Evaluate the different modalities of voice therapy
Develop prognostic indicators to identify the benefits of voice analysis and its impact on selection of voice therapy modalities- References
1- Umeno H, Hyodo M, Haji T, Hara H, Imaizumi M,
Ishige M, Kumada M, Makiyama K, Nishizawa N, Saito K, Shiromoto O, Suehiro A,
Takahashi G, Tateya I, Tsunoda K, Shiotani A, Omori K. A summary of the
Clinical Practice Guideline for the Diagnosis and Management of Voice
Disorders, 2018 in Japan. Auris Nasus Larynx. 2020 Feb;47(1):7-17. doi:
10.1016/j.anl.2019.09.004. Epub 2019 Oct 4. PMID: 31587820.
2- Stachler RJ, Francis DO, Schwartz SR, Damask CC, Digoy GP, Krouse HJ, McCoy SJ, Ouellette DR, Patel RR, Reavis CC, Smith LJ. Clinical practice guideline: hoarseness (dysphonia)(update). Otolaryngology–Head and Neck Surgery. 2018 Mar;158(1_suppl):S1-42.
3- Verdolini K, Rosen CA, Branski RC, editors. Classification manual for voice disorders-I. Psychology Press; 2014 Apr 8.
4- Wuyts FL, De Bodt MS, Van de Heyning PH. Is the reliability of a visual analog scale higher than an ordinal scale? An experiment with the GRBAS scale for information. J Voice 1999;13:508–17.
5- Chang JI, Bevans SE, Schwartz SR. Otolaryngology clinic of North America: evidence-based practice: management of hoarseness/dysphonia. Otolaryngol Clin North Am 2012;45:1109–26.
6- Woo P, Colton R, Casper J, Brewer D. Diagnostic value of stroboscopic examination in hoarse patients. J Voice 1991;5:231–8.
7- Sataloff RT, Spiegel JR, Hawkshaw MJ. Strobovideolaryngoscopy: results and clinical value. Ann Otol Rhinol Laryngol 1991;100:725–7.
8- Petrovic-Lazic M, Jovanovic N, Kulic M, Babac S, Jurisic V. Acoustic and perceptual characteristics of the voice in patients with vocal polyps after surgery and voice therapy. J Voice 2015;29:241–6.
9- Burduk PK, Wierzchowska M, Orzechowska M, Kazmierczak W, Pawlak-Osinska K. Assessment of voice quality after carbon dioxide laser and microdebrider surgery for Reinke edema. J Voice 2015;29:256–9.