Post stroke Oropharyngeal dysphagia
| Site: | EHC | Egyptian Health Council |
| Course: | Otorhinolaryngology, Audiovestibular & Phoniatrics Guidelines |
| Book: | Post stroke Oropharyngeal dysphagia |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 10:09 PM |
Description
"last update: 28 April 2024"
- Committee
Chair
of the Panel:
Usama Abdel Naseer
Scientific Group Members:
Abdalla Anayet, Abdelrahman Eltahaan, Ahmed Mostafa, Alaa Gaafar, Amr Taha, Ashraf Lotfy, Athar Reda Ibrahim, Bahaa Eltoukhy, Haytham Elfarargy, Hazem Dewidar, Ihab Sifin, Loay Elsharkawy, Mai Mohammed Salama, Mina Esmat, Rania Abdou, Reda Sharkawy, Saad Elzayat, Samir Halim.
➡️Abbreviations
PSOPD: post-stroke oropharyngeal dysphagia
TDT: Traditional Dysphagia Therapies
NMES neuromuscular electrical stimulation
rTMS: Repetitive transcranial magnetic stimulation
tDCS transcranial direct current stimulation
TES : transcutaneous electrical stimulation .
PES :pharyngeal electrical stimulation .
➡️ Glossary
Oropharyngeal dysphagia: typically refers to difficulty in eating as a result of disruption in the swallowing process.
The Eating Assessment Tool-10 (EAT-10) is a dysphagia screening tool developed in 2008 by Belafsky et al. to identify people at high risk of swallowing disorders. It is a 10-item self-assessment scale that patients can complete in a short period of time. Each item corresponds to 5 levels of difficulty from “no problem” to “serious problem,”
The water-swallowing test (WST): is frequently used in clinical practice as a functional assessment to detect aspiration and prevent pneumonia. It is a standardized test used all over the world
traditional swallowing training, (TST) relies on behavioral training that focus on enhancing sensory feedback from the oropharynx to the central pattern generator, strengthening the disused or pharyngeal musculature, preventing atrophy and reduced motor output from the central pattern generator, and minimizing symptoms through the use of compensatory postural adjustments.
Repetitive transcranial magnetic stimulation and transcranial direct current stimulation, surface neuromuscular electrical stimulation (NMES): ,Are numerous adjunctive treatment options that may theoretically improve the recovery of dysphagia.
➡️Scope
This Guideline is concerned with diagnosis and treatment decision of: oropharyngeal dysphagia. This is targeting adults >18 years this guideline is not targeting pediatric population.
- Executive Summary
The Phoniatrician’s role is:
- Identifying signs and symptoms of dysphagia;
- Identifying normal and abnormal swallowing anatomy and physiology supported by imaging;
- Identifying indications and contraindications specific to each patient for various assessment procedures;
- Identifying signs of potential disorders in the upper aerodigestive and/or digestive tracts and making referrals to appropriate medical personnel;
- Assessing swallow function as well as analyzing and integrating information from such assessments collaboratively with medical professionals, as appropriate;
- Providing treatment for swallowing disorders, documenting progress, adapting and adjusting treatment plans based on patient performance
- Identifying and using appropriate functional outcome measures;
- Understanding a variety of medical diagnoses and their potential impact(s) on swallowing;
- Recognizing possible contraindications to clinical decisions and/or treatment;
- Being aware of typical age-related changes in swallow function;
- Providing education and counseling to individuals and caregivers;
- Respecting issues related to quality of life for individuals and/or caregivers;
- Practicing interprofessional collaboration;
- Advocating for services for individuals with swallowing and feeding disorders;
- Determining the effectiveness and possible impact of current diet on overall health (e.g., positioning, feeding dependency, environment, diet modification, compensations).
➡️Purpose
Appraisal of the research evidence that exists to support the use of instrumental measures in the clinical assessment of patients with PSOPD. And outline the measures used in its management.
Specifically, the goals are to improve diagnostic accuracy, identify post stroke cases who are most susceptible to OPD, and educate clinicians regarding assessment and rehabilitation
➡️The target audience
The guideline is intended for all clinicians who are likely to diagnose and manage OPD
- Methods
A comprehensive search for guidelines was undertaken to identify the most relevant guidelines to consider for adaptation.
inclusion/exclusion criteria followed in the search and retrieval of guidelines to be adapted:
· Selecting only evidence-based guidelines (guideline must include a report on systematic literature searches and explicit links between individual recommendations and their supporting evidence)
· Selecting only national and/or international guidelines
· Specific range of dates for publication (using Guidelines published or updated 2013 and later)
· Selecting peer reviewed publications only
· Selecting guidelines written in English language
· Excluding guidelines written by a single author not on behalf of an organization in order to be valid and comprehensive, a guideline ideally requires multidisciplinary input
· Excluding guidelines published without references as the panel needs to know whether a thorough literature review was conducted and whether current evidence was used in the preparation of the recommendations
The following characteristics of the retrieved guidelines were summarized in a table:
• Developing organisation/authors
• Date of publication, posting, and release
• Country/language of publication
• Date of posting and/or release
• Dates of the search used by the source guideline developers
All retrieved Guidelines were screened and appraised using AGREE II instrument (www.agreetrust.org) by at least two members. the panel decided a cut-off point or rank the guidelines (any guideline scoring above 50% on the rigour dimension was retained)
➡️Evidence assessment
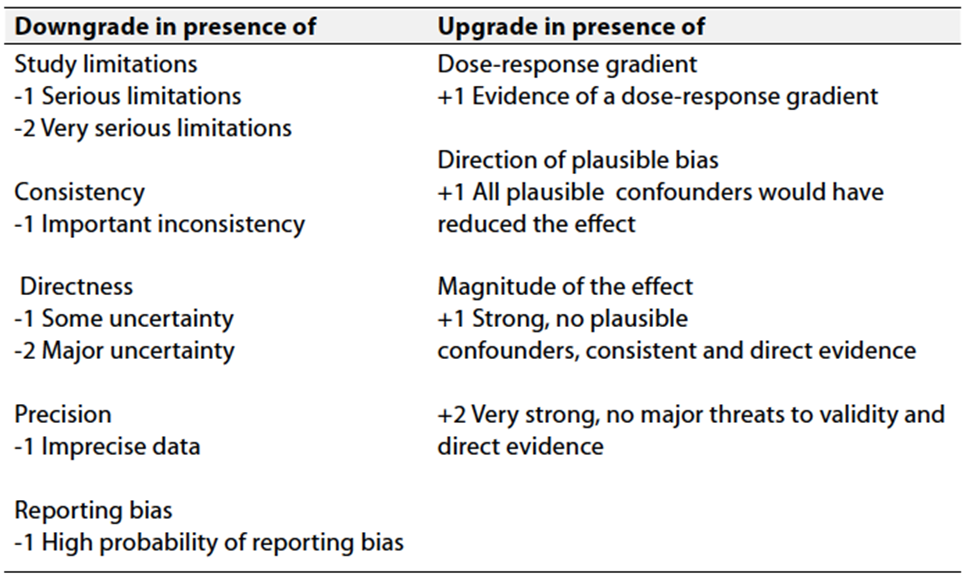
According to WHO handbook for Guidelines we used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess the quality of a body of evidence, develop and report recommendations. GRADE methods are used by WHO because these represent internationally agreed standards for making transparent recommendations. Detailed information on GRADE is available on the following sites:
■ GRADE working group: http://www.gradeworkingroup.org
■ GRADE online training modules: http://cebgrade.mcmaster.ca/
■ GRADE profile software: http://ims.cochrane.org/revman/gradepro
Table 1 Quality of evidence in GRADE
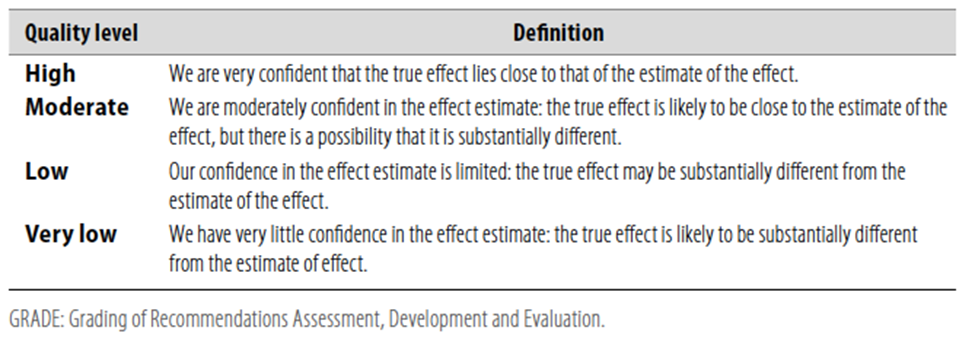
Table 2 Significance of the four levels of evidence
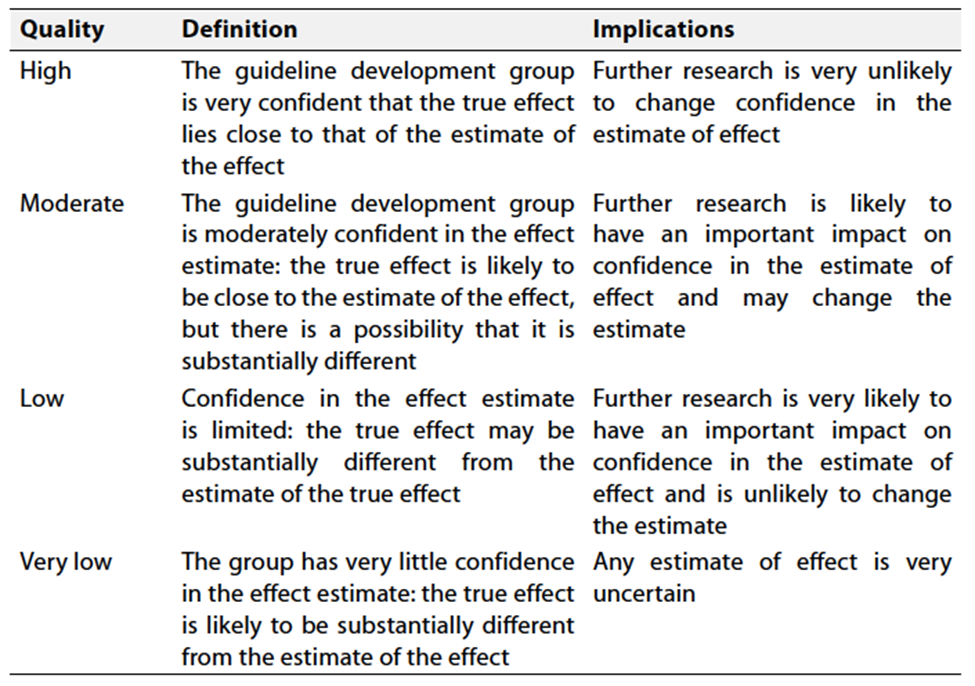
Table 3 Factors that determine How to upgrade or downgrade the quality of evidence
- The strength of the recommendation
The strength of a recommendation communicates the importance of adherence to the recommendation.
➡️Strong recommendations
With strong recommendations, the guideline communicates the message that the desirable effects of adherence to the recommendation outweigh the undesirable effects. This means that in most situations the recommendation can be adopted as policy.
➡️Conditional recommendations
These are made when there is greater uncertainty about the four factors above or if local adaptation has to account for a greater variety in values and preferences, or when resource use makes the intervention suitable for some, but not for other locations. This means that there is a need for substantial debate and involvement of stakeholders before this recommendation can be adopted as policy.
When not to make recommendations
When there is lack of evidence on the effectiveness of an intervention, it may be appropriate not to make a recommendation.
- Recommendations
|
|
Evidence-Based Statements recommendation levels |
Grades / Levels of Evidence |
|
Eating assessment tool (EAT-10) can be used as a dysphagia screening tool (1) |
Strong Recommendation; |
Moderate Evidence |
|
All patients should receive a formal dysphagia screen by either water swallow test or multiple consistency test as fast as possible following admission secondary to acute stroke. Until such time that this screening can be conducted and swallowing has been judged to be safe, no administration of any food or liquid, including oral medication, is recommended (1)
|
Strong Recommendation, |
Moderate Evidence |
|
All stroke patients failing a dysphagia screen and/or showing other clinical predictors of post-stroke dysphagia (i.e., severe aphasia, severe dysarthria, severe facial palsy, and/or severe neurological deficit) should receive a dysphagia evaluation as soon as possible. In addition to clinical swallow examination, videofluoroscopic swallow study, or, preferably, fiberoptic endoscopic evaluation of swallowing should be available. Evaluation should routinely include swallowing of tablets, liquids, and different food consistencies and quantities (1)
|
Weak Recommendation, |
Low Evidence |
|
For individuals with dysphagia secondary to stroke, texture modification and/or thickened liquids may be utilized to reduce risk of pneumonia (1) |
Weak For Recommendation |
Low Evidence |
|
These modified textures and viscosities must only be prescribed based upon an appropriate assessment of swallowing. (1) |
Strong for Recommendation |
Low Evidence |
|
Additionally, these patients should be monitored for fluid balance and nutritional intake (1)
|
Strong Recommendation |
Moderate Evidence |
|
Behavioral swallowing exercises (defined as including exercises, maneuvers, postural changes, and expiratory muscle strength training within this guideline) to rehabilitate swallow function are recommended for individuals with dysphagia status post stroke, however the training program should be tailored to the specific swallowing impairment of the individual based upon assessment findings (1) |
Weak Recommendation |
Moderate Evidence |
|
Oral care interventions are recommended in patients with dysphagia secondary to stroke in order to reduced pneumonia risk (1) |
Weak Recommendation |
Low Evidence |
|
Swallowing fluoroscopy may also be appropriate in evaluating patients with globus pharyngeus, chronic cough, regurgitation, or recurrent pneumonia (2) |
recommendation |
Moderate Quality of Evidence |
|
Videofluoroscopic swallow studies (VFSS) are appropriate for patients with suspected swallowing impairments from the oral to the pharyngoesophageal phases of deglutition or patients with inconclusive or incongruent clinical swallow exam results (2) |
recommendation |
Low Quality of Evidence |
|
VFSS should be the assessment tool used for patients with known neurologic diseases or with liquid dysphagia complaints (2) |
recommendation |
High Quality of Evidence |
|
When conducting a videofluoroscopic swallow study (VFSS), clinicians should follow "a standardized and reproducible stepwise protocol including the lateral and anterior-posterior (AP) views" (2) |
recommendation |
Moderate Quality of Evidence |
|
As clinically appropriate, VFSS protocol should progress from the smallest bolus volume to larger volumes and multiple consistencies and solids should be used (2) |
recommendation |
Moderate Quality of Evidence |
|
In patients with post-stroke dysphagia and insufficient oral intake we suggest an early enteral nutrition via a nasogastric tube.(1)
|
Weak recommendation |
Quality of evidence: Moderate
|
|
In patients with post-stroke dysphagia, we suggest treatment with rTMS, TES, tDCS and PES as adjunct to conventional dysphagia treatments to improve swallowing function.(1)
|
Weak recommendation |
Moderat
|
- References:
1- European Stroke Organisation and European Society for Swallowing Disorders Guideline for the Diagnosis and Treatment of Post-Stroke Dysphagia . Dziewas, R., Michou, E., et al. (2021). European Stroke Journal, 6(3), LXXXIX-CXV.
2- The American
Broncho-Esophagological Association Position Statement on Swallowing
Fluoroscopy Dhar, S. I., Nativ-Zeltzer, N., et al. (2023). Laryngoscope,
133(2), 255-268.
3- Anne
Marie Beck, Annette Kjaersgaard, Tina Hansen, Ingrid Poulsen, Systematic review
and evidence based recommendations on texture modified foods and thickened
liquids for adults (above 17 years) with oropharyngeal dysphagia – An updated
clinical guideline, Clinical Nutrition,Volume 37, Issue 6, Part A,2018,Pages
1980-1991,ISSN 0261-5614, https://doi.org/10.1016/j.clnu.2017.09.002.
4- Comparative
Effectiveness of Combined and Single Neurostimulation and Traditional Dysphagia
Therapies for Post-Stroke Dysphagia: A Network Meta-Analysis. Banda, K. J., Wu,
K. C., et al. (2023). Neurorehabilitation and Neural Repair, 37(4), 194-204.
5- Clinical
Guidelines for Stroke Management Stroke Foundation. (2022).
Melbourne (Australia): Stroke Foundation,