Pediatric Eye Examination
| Site: | EHC | Egyptian Health Council |
| Course: | Ophthalmology Guidelines |
| Book: | Pediatric Eye Examination |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 8:22 PM |
Description
"last update: 22 February 2024"
- ACKNOWLEDGEMENTS
The Ophthalmology
Committee of National Egyptian Guidelines, Ministry of Health and
Ophthalmology
Chair of the committee: Hany Nasr.
Committee members: Mohamed Salah, Essam Eltokhi, Rania Gamal, Weam Obaid, Karim Rizk, Maged Maher, Ayman Elghonemy.
Contributors from outside the committee: Mustafa Azab.
➡️ABBREVIATIONS
NICU: neonatal intensive care unit
RAPD: relative afferent pupillary defect
IOP: intra-ocular pressure
ROP: retinopathy of Prematurity
➡️GLOSSARY
Myopia: a condition in which the visual images come to a focus in front of the retina of the eye resulting in defective vision of distant objects.
Hyperopia: a condition in which visual images come to a focus behind the retina of the eye and vision is better for distant than for near objects.
Stereopsis: is the perception of depth. It arises when objects behind and in front of the point of fixation (but within Panum fusional space) simultaneously stimulate horizontally disparate retinal elements. The fusion of these disparate images results in a single visual impression perceived in depth. A solid object is seen stereoscopically (in 3D) because each eye sees a slightly different aspect of the object.
Vergences: are binocular, simultaneous, disconjugated movements (in opposite directions, so that the angle between the eyes changes.
Convergence: is simultaneous adduction (inward turning) and divergence is outwards movement from a convergent position.
Fusional vergences: are motor responses that eliminate horizontal, vertical, and to a limited degree torsional image disparity.
Amblyopia: is diminution of vision occurring during the years of visual development secondary to abnormal visual stimulation or abnormal binocular interaction. It is usually unilateral but it can be bilateral. The diminished vision is beyond the level expected from the ocular pathology present.
Tropia: manifest deviation in which the visual axes do not intersect at the point of fixation.
Esotropia means inward eye deviation, an Exotropia means outward eye deviation, a hyper-tropia means upward eye deviation, and a hypo-tropia means downward eye deviation.
Nystagmus: is rhythmic, abnormal eye movements with a "slow" eye movement driving the eye off the target followed by a second movement that brings the eye back to the target.
Duction: an eye movement involving only one eye. It may be adduction, abduction elevation, depression, intorsion, extorsion.
Anisocoria: is when the pupils are not the same size.
Coloboma: ocular defects of the eyelids, iris, lens, ciliary body, zonules, choroid, retina or optic nerve. It is typically located in the inferonasal quadrant of the involved structure. It can affect one eye or both eyes.
Ptosis: is when the upper eyelid droops over the eye. The eyelid may droop just a little, or so much that it covers the pupil. Ptosis can limit or even completely block normal vision.
Proptosis: is the protrusion of the eyeball from the orbit.
Hypoglobus: is the downward displacement of the globe in the orbit.
Hyperglobus: is the upward displacement of the globe in the orbit.
Diplopia: is the simultaneous perception of two images of a single object that may be displaced horizontally or vertically in relation to each other. It is also called double vision.
Accommodation: is the mechanism by which the eye changes the refractive power by altering the shape of the lens in order to focus objects in various directions.
Keratoconus: is an uncommon corneal disorder where the central or paracentral cornea undergoes progressive thinning and steepening causing irregular astigmatism.
- EXECUTIVE SUMMARY
These guidelines describe the cornerstones of eye examination in the pediatric age group
♦️ A comprehensive pediatric eye and vision examination should include but is not limited to
- Review of the nature and history of the presenting problem, patient and family eye and medical histories and school performance history of the child.
- Examination should include assessment of visual acuity with a method suitable for age, determination of refractive status, ocular motility assessment and evaluation of pupillary response,
- Assessment of binocular vision, accommodation and evaluation of color vision can be indicated in selected cases.
- Assessment of peripheral retina, measurement of intraocular pressure, and visual field testing can be indicated in selected cases.
- Good practice statement
♦️ Cycloplegic retinoscopy is the preferred procedure for the evaluation of refraction in children, both for preschool and school age.
- Good practice statement
♦️ Infants should receive an in-person comprehensive eye and vision assessment between 6 and 12 months of age for the prevention and/or early diagnosis and treatment of sight-threatening eye conditions and to evaluate visual development.
- Strong Recommendation
♦️ Preterm infants with a history of ROP should be closely monitored for the development of high myopia, astigmatism, and anisometropia
- Strong Recommendation
♦️ Early visual examination in infants for amblyopia and amblyopic risk factors can lower the prevalence and severity of amblyopia in children.
- Strong Recommendation
♦️ Preschool children should receive an in-person comprehensive eye and vision examination at least once between the ages of 3 and 5 to prevent and/ or diagnose and treat any eye or vision conditions that may affect visual development.
- Strong Recommendation
♦️ School-age children should receive an in-person comprehensive eye and vision examination before beginning school to diagnose, treat, and manage any eye or vision conditions.
- Strong Recommendation
♦️ Children with myopia should have an in-person comprehensive eye and vision examination at least annually.
- Strong recommendation
- Introduction
About 19 million children ,all over the world, under the age of 15 years are visually impaired and 1.4 million children have irreversible blindness It was predicted that half of the blindness cases were preventable (1). According to statistics in 2022, there are more than 35.24 million children under the age of 15 living in Egypt (2). Comprehensive detailed eye examination in selected cases could prevent severe complications of eye diseases.
➡️Purpose of the guidelines:
▪️ Identify risk factors for ocular disease
▪️ Identify systemic disease based on associated ocular findings
▪️ Identify factors that may predispose to visual loss early in a child's life
▪️ Determine the health status of the eye and the visual system, and assess refractive errors
▪️ Discuss the findings of the examination and their implications with the parent/caregiver and the patient when appropriate
▪️ Initiate an appropriate management plan
➡️Scope of the guidelines
▪️ Proper evaluation of the eyes and visual functions of infants and children under the age of 18
➡️Target audience:
Ophthalmologists - Pediatricians – Family doctors - High nurses.
- Methods
A comprehensive search for guidelines was undertaken to identify the most relevant guidelines to consider for adaptation.
The main source was the Pediatric Ophthalmology/Strabismus Preferred Practice Pattern published by the American Academy of Ophthalmology, last edition of 2022 (3) and Comprehensive Pediatric Eye and Vision Examination by the American Optometric Association 2017 (4)
The inclusion/exclusion criteria followed in the search and retrieval of guidelines to be adapted:
- Selecting only evidence-based guidelines (guideline must include a report on systematic literature searches and explicit links between individual recommendations and their supporting evidence)
- Selecting peer reviewed publications only
- Selecting guidelines written in English language
- Excluding guidelines written by a single author not on behalf of an organization in order to be valid and comprehensive, a guideline ideally requires multidisciplinary input
- Excluding guidelines published without references as the panel needs to know whether a thorough literature review was conducted and whether current evidence was used in the preparation of the recommendations
The following characteristics of the retrieved guidelines were summarized in a table:
- Developing organization/authors
- Date of publication, posting, and release
- Country/language of publication
- Date of posting and/or release
- Dates of the search used by the source guideline developers
- Evidence assessment
According to WHO handbook for Guidelines (5) we used the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach to assess the quality of a body of evidence, develop and report recommendations. GRADE methods are used by WHO because they represent internationally agreed standards for making transparent recommendations. Detailed information on GRADE is available on the following sites:
■ GRADE working group: http://www.gradeworkingroup.org
■ GRADE online training modules: http://cebgrade.mcmaster.ca/
■ GRADE profile software: http://ims.cochrane.org/revman/gradepro
Table 1 Quality of evidence in GRADE
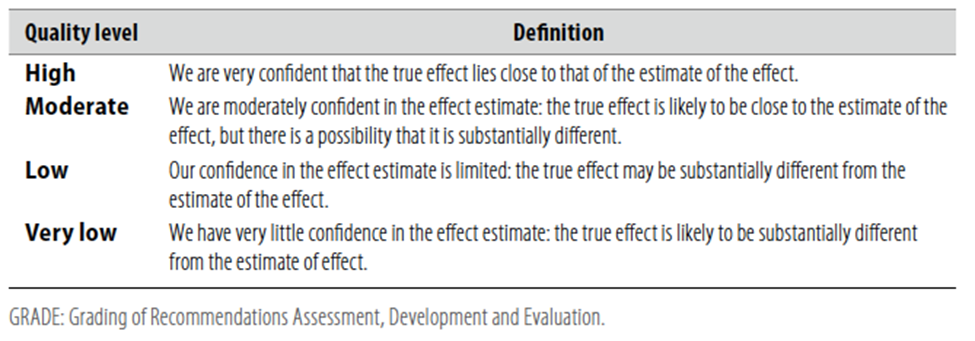
WHO guideline reporting tool - V1.5, December 2021
Table 2 Significance of the four levels of evidence
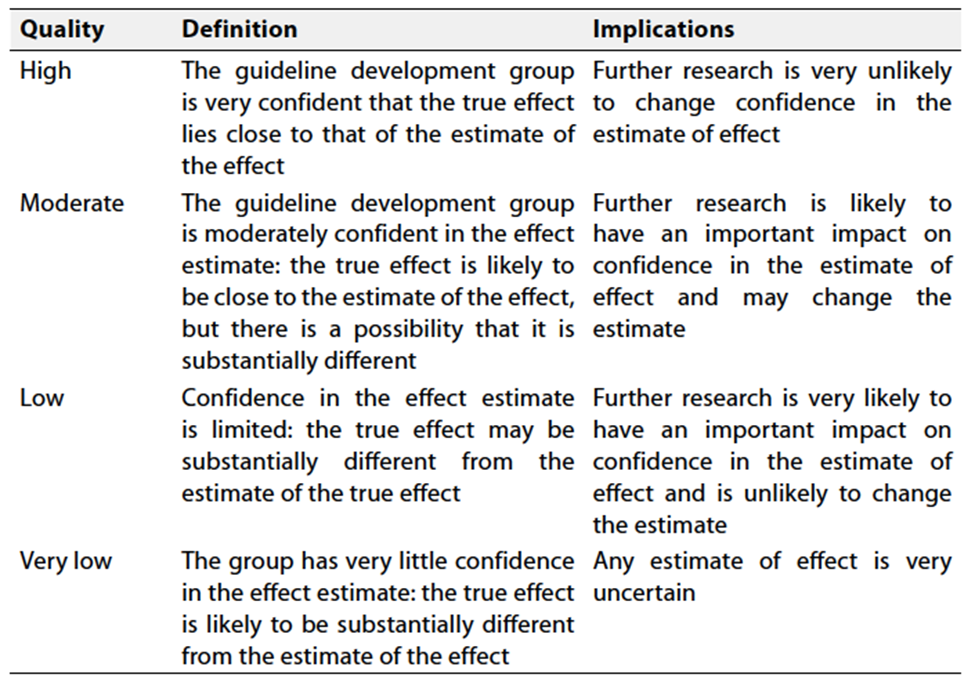
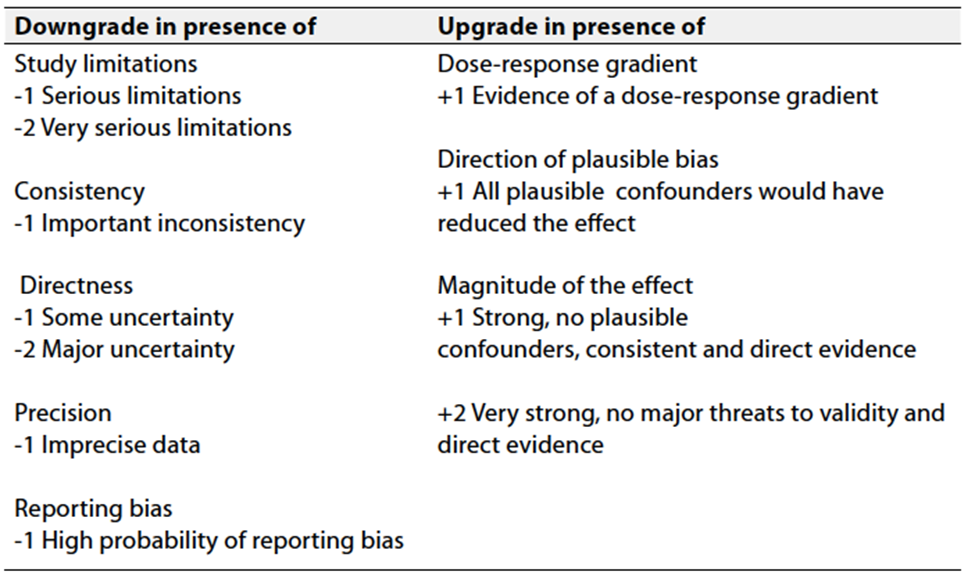
Table 3 Factors that determine how to upgrade or downgrade the quality of evidence
WHO guideline reporting tool - V1.5, December 2021
The strength of the recommendation
The strength of a recommendation communicates the importance of adherence to this recommendation.
Strong recommendations
With strong recommendations, the guideline communicates the message that the
desirable effects of adherence to the recommendation outweigh the undesirable
effects. This means that in most situations the recommendation can be adopted
as policy.
Conditional recommendations
These are made when there is greater uncertainty about the four factors mentioned
in table 3 or if local adaptation has to account for a greater variety in
values and preferences, or when resource use makes the intervention suitable
for some, but not for other locations. This means that there is a need for
substantial debate and involvement of stakeholders before this recommendation
can be adopted as policy.
When not to make recommendations
When there is lack of evidence on the effectiveness of an intervention, it may
be appropriate not to make a recommendation.
- Recommendations
♦️ A comprehensive pediatric eye and
vision examination should include but is not limited to
- review of the nature and history of the presenting problem, patient and family eye and medical histories and school performance history of the child.
- Examination should include assessment of visual acuity with a method suitable to age, determination of refractive status, ocular motility assessment, evaluation of pupillary response,
- Assessment of binocular vision, accommodation, evaluation of color vision can be indicated in selected cases.
- Assessment of peripheral retina, measurement of intraocular pressure, and visual field testing can be indicated in selected cases.
- Good practice statement
- Level of evidence: very low (lack of published research to support or refute the use of all of the tests and/or assessments included in this recommendation).
♦️ Cycloplegic retinoscopy is the preferred procedure for the evaluation of refraction in children, both for preschool and school age
- Good practice statement
- Level of evidence: very low (lack of published research to support or refute the use of all of the tests and/or assessments included in this recommendation).
♦️ Infants should receive an in-person comprehensive eye and vision assessment between 6 and 12 months of age for the prevention and/or early diagnosis and treatment of sight-threatening eye conditions and to evaluate visual development.
- Strong Recommendation
- Level of evidence: Medium (Prospective cohort studies, Diagnostic study) (6-8)
♦️ Preterm infants with a history of ROP should be closely monitored for the development of high myopia, astigmatism, and anisometropia
- Strong Recommendation
- Level of evidence: Medium (Prospective cohort studies, Diagnostic study) (6)
♦️ Early visual examination in infants for amblyopia and amblyopic risk factors can lower the prevalence and severity of amblyopia in children.
- Strong Recommendation
- Level of evidence: Medium (Prospective cohort studies, Diagnostic study) (7)
♦️ Preschool age children should receive an in-person comprehensive eye and vision examination at least once between the ages of 3 and 5 to prevent and/ or diagnose and treat any eye or vision conditions that may affect visual development.
- Strong Recommendation
- Level of evidence: Medium (Systematic Review, Case series, Cross-sectional study) (9-12)
♦️ School-age children should receive an in-person comprehensive eye and vision examination before beginning school to diagnose, treat, and manage any eye or vision conditions.
- Strong Recommendation
- Level of evidence: Medium (Systematic Review, Case series, Cross-sectional study) (13-16)
♦️ Children with myopia should have an in-person comprehensive eye and vision examination at least annually.
- Strong recommendation
- Level of evidence: Medium (Randomized clinical trial, Prospective cohort study) (17-18)
➡️Clinical Indicators:
- Pediatric Eye evaluation included: assessment of visual acuity, determination of refractive status, ocular motility assessment, evaluation of pupillary response and cycloplegic refraction.
- Children were scheduled to be seen at least once at age of 6 months to 1 year, then between age 3 and 5 years, then before starting school.
➡️Updates:
To keep these recommendations up to date and ensure its validity it will be periodically updated. This will be done whenever new strong evidence is available and necessitates updating.
➡️Research Gaps:
It is recommended to have high quality randomised controlled trials on the frequency of visits needed for hypermetropic and astigmatic children
- Appendix 1
(Points of history taking and examinations)
➡️History Taking:
Thorough history taking is mandatory and should include the following:
▪️ Demographic data: including sex and date of birth
▪️ The chief complaint
▪️ Perinatal history: including maternal drug intake during pregnancy and/or lactation, gestational age at time of delivery, birth weight, history of NICU admission or any other neonatal intervention. This is important in infants and in special cases in older children.
▪️ Ocular history: including prior eye problems, diseases, diagnoses, treatment and surgeries
▪️ Systemic history: including history of hospitalization, surgeries and general health.
▪️ Current medications and allergies.
▪️ Family history of any related ocular or systemic conditions
➡️Examination
Documentation of the child’s level of cooperation in the examination can be useful in interpreting the results. The order of the examination may vary depending on the child’s level of cooperation. Testing of sensory function should be performed before using any dissociating examination techniques, such as covering an eye to check visual acuity or alignment. Binocular alignment testing should be done prior to cycloplegia. The examination should include the following elements:
▪️ Binocular red reflex (Brückner) test
▪️ Binocularity/stereo-acuity testing
▪️ Assessment of fixation pattern and/or visual acuity
▪️ Binocular alignment and ocular motility
▪️ Pupillary examination
▪️ External examination
▪️ Anterior segment examination
▪️ Cycloplegic retinoscopy/refraction
▪️ Funduscopic examination
➡️Binocular Red Reflex (Brückner) Test
To perform this test, the room is darkened, and the examiner sets the ophthalmoscope lens power at “0” and directs the ophthalmoscope light toward both eyes of the child simultaneously from approximately 50 to 75 centimeters. The Brückner test should be performed prior to pupillary dilation, because subtle differences in the red reflex are difficult to detect once the pupils are dilated (19). To be considered normal, a symmetric red reflex should be observed from both eyes. Opacities within the red reflex, a markedly diminished reflex, the presence of a white or dull reflex, or asymmetry of the red reflexes are all considered abnormal. The appearance of the red reflex varies based on retinal pigmentation and, thus, varies by race/ethnicity; therefore, the emphasis is on symmetry rather than the color of the reflex. Significant hyperopia will present as an inferiorly placed brighter crescent in the red reflex. Significant myopia presents as a superiorly placed brighter crescent (20).
➡️Binocularity/Stereoacuity Testing
Binocularity, or binocular vision, has several different components, including sensory fusion, stereopsis, fusional vergence (motor fusion), and other coordinated binocular eye movements. Sensorimotor fusion is sensitive to disruption by amblyopia, strabismus, refractive error, and deprivation. Binocular vision may be affected to different degrees depending on the underlying diagnosis, and tests to evaluate each of these components vary accordingly. The Worth 4-Dot Test is used to evaluate sensory fusion, the Randot Stereo Test is used to evaluate stereopsis, and a prism bar or rotary prism is used to evaluate fusional motor vergence (21,22) Assessment of stereoacuity is an important component of binocular alignment testing because high-grade stereoacuity is associated with normal alignment (23). Filter-free stereoacuity tests may be comparable to the Randot test and eliminate the need for polarizing lenses (24). Testing of sensory function should be performed before using any dissociating examination techniques (e.g., covering an eye to check monocular visual acuity or cover testing to assess alignment).
➡️Assessment of Fixation Pattern and Visual Acuity
Fixation:
Visual acuity measurement of the infant or toddler involves a qualitative assessment of fixation and tracking (following) eye movements. Fixation and following are assessed by drawing the child’s attention to the examiner or caregiver’s face or to a hand-held light, silent toy, or other fixation target and then slowly moving the target. Fixation behavior can be recorded for each eye as “fixes and follows” or “central, steady, and maintained through a smooth pursuit,” along with any qualifying findings, such as fixation that is eccentric, not central, not steady, or not maintained. Large differences in vision between the eyes can be detected by observing the vigor with which the child objects to occlusion of one eye relative to the other. Children resist covering an eye when the fellow eye has limited vision (25-27)
Grading schemes can be used to describe fixation preference. For strabismic patients, fixation pattern is graded binocularly by determining the length of time that the nonpreferred eye holds fixation. The eye will not hold fixation, holds momentarily, holds for a few seconds (or to or through a blink), or spontaneously alternates fixation.
For children with small-angle strabismus or no strabismus, the induced tropia test may be done by holding a base-down or base-in prism of 10 to 20 prism diopters over one eye and then over the other eye and noting fixation behavior (27-29) Studies have shown that these tests cannot stand alone as highly accurate screening tests for differentiating amblyopia from normal.(26, 30-32) However, when used in a clinical setting and interpreted in the context of other key findings, tests of fixation preference can be useful diagnostic tools to help determine whether there is amblyopia of sufficient severity to warrant treatment. Qualitative assessment of visual function should be replaced with a recognition visual acuity test based on optotypes (letters, numbers, or symbols) as soon as the child can perform this task reliably.
➡️Visual Acuity
Recognition visual acuity testing, which involves identifying optotypes and consisting of letters, numbers, or symbols, is preferred for assessment of visual acuity to detect amblyopia. The optotypes may be presented on a wall chart, computer screen, or hand-held card. Visual acuity is routinely tested at distance 3 to 6 meters and at near 35 to 40 centimeters. Visual acuity testing conditions should be standardized so that results obtained over a series of visits can be readily compared. High contrast charts with black optotypes on a white background should be used for standard visual acuity testing (33-34). A child’s performance on a visual acuity test will depend on the choice of chart and the examiner’s skills and rapport with the child, and on the child’s level of cooperation. To reduce errors, the environment should be quiet and free of distraction. Younger children may benefit from a pretest on optotypes presented at near, either at the start of testing or in a separate session.
Before monocular testing, the examiner should ensure that the child is able to perform the test reliably. Allowing children to match optotypes on the chart to those found on a hand-held card will enhance performance, especially in young, shy, or children with cognitive impairments. Visual acuity testing of children with special needs can provide quantitative information about visual impairment and reduce concerns of parents about the child’s vision (34). A shorter testing distance or flip chart can also facilitate testing in younger children (35).
Visual acuity testing should be performed monocularly and with best refractive correction in place. Ideally, the fellow eye should be covered with an adhesive patch or tape. If such occlusion is not available or not tolerated by the child, care must be taken to prevent the child from peeking and using the “covered” eye. Sometimes the child will not allow any monocular occlusion, in which case binocular visual acuity should be measured.
Monocular visual acuity testing for patients with nystagmus or latent nystagmus requires special techniques such as blurring the fellow eye with high plus lenses or using a translucent occluder rather than an opaque one. Binocular visual acuity testing can also be performed on these patients to gain additional information about typical visual performance.
An age-appropriate and consistent testing strategy on every examination is essential. The choice and arrangement of optotypes can significantly affect the visual acuity score obtained (36-37). Optotypes should be clear, standardized, and of similar characteristics, and they should not reflect a cultural bias (34).
LEA SYMBOLS® (Good-Lite Co., Elgin, IL, USA), a set of four symbols developed for use with young children, are useful because each optotype blurs similarly as the child is presented with smaller symbols, increasing the reliability of the test (36,39). Because they include only four possible responses, these acuity tests are easier for younger children. Children who cannot name them may match them using a hand-held card. Other charts like HOTV (36,40), Allen Figures, Lighthouse Chart, Kindergarten (Sailboat) Eye Chart can also be used (34,41)
For older cooperative children Landolt C chart or tumbling E chart can be used. The majority of optotypes must be correctly identified to “pass” a line. A similar number of optotypes on each line with equal spacing is preferred. In the setting of amblyopia, testing with single optotypes is likely to overestimate visual acuity(42,44) because of the crowding phenomenon; that is, it is easier to discriminate an isolated optotype than one presented in a line of optotypes. Therefore, a more accurate assessment of monocular visual acuity is obtained in amblyopia with a line of optotypes. In order to preserve the crowding effect of adjacent optotypes, optotypes should not be covered or masked as the examiner points to each successive optotype. If a single optotype must be used to facilitate visual acuity testing for some children, the single optotype should be surrounded (crowded) by bars placed above, below, and on either side of the optotype(45,47)
Forced choice preferential looking testing can provide an assessment of grating resolution visual acuity in some infants and preverbal children, and the patient’s acuity can be compared with normative data; this method overestimates recognition visual acuity in children with amblyopia(48,49)
➡️Binocular Alignment and Ocular Motility Assessment
The corneal light reflection, binocular red reflex (Brückner) test, and cover tests are commonly used to assess binocular alignment. Cover/uncover tests for tropias and alternate cover tests for the total deviation (latent component included) in primary gaze at distance and near should use accommodative targets. The cover test is performed by covering one eye and observing for a refixation movement of the fellow eye; if it occurs, then a tropia is present. Cover tests require sufficient visual acuity and cooperation to fixate on the desired target. Ocular versions and ductions, including into the oblique fields of gaze, should be tested in all infants and children. Eye movements may be tested using oculocephalic rotation (doll’s head maneuver) or assessed by observing spontaneous eye movements in the inattentive or uncooperative child. Binocular alignment testing should be done before cycloplegia, because alignment may change after cycloplegia.
➡️Pupillary Examination
The pupils should be assessed for size, symmetry, and shape; for their direct and consensual responses to light; and for presence of a relative afferent defect. Pupillary evaluation in infants and children may be difficult due to hippus, poorly maintained fixation, and/or rapid changes in accommodative status. Anisocoria greater than 1 millimeter may indicate a pathological process, such as Horner syndrome, Adie tonic pupil, or a pupil-involving third-cranial-nerve palsy. Irregular pupils may indicate the presence of traumatic sphincter damage, iritis, or a congenital abnormality (e.g., coloboma). A relative afferent pupillary defect (RAPD) of 0.3 or more log units (i.e., easily visible) is not typically seen in amblyopia. A subtle RAPD may be seen with dense amblyopia. The presence of a large RAPD should warrant a search for compressive optic neuropathy or other etiologies of visual impairment (e.g., retinal abnormality). (50)
➡️External Examination
The external examination involves assessment of the eyelids, eyelashes, lacrimal system, and orbit. The examination should include an assessment of ptosis, the amount of levator function, presence of eyelid retraction, and relative position of the globe within the orbit (e.g., proptosis or globe retraction, hypoglobus, or hyperglobus). Older children may tolerate measurement of globe position using an exophthalmometer. For uncooperative or younger children, proptosis of the globe may be estimated by comparing the position of the globes when viewing from above the head. The anatomy of the face (including the eyelids, interocular distance, and presence or absence of epicanthal folds), orbital rim, and presence of oculofacial anomalies should be noted. The position of the head and face (including head tilt, turn, or chin-up or chin-down head posture) should be recorded. Children who have prominent epicanthal folds and/or a wide, flat nasal bridge and normal binocular alignment often appear to have an esotropia (pseudoesotropia). Dysmorphic features need further evaluation.
➡️Anterior Segment Examination
The cornea, conjunctiva, anterior chamber, iris, and lens should be evaluated using slit-lamp biomicroscopy, if possible. For infants and young children, anterior segment examination using a direct ophthalmoscope, a magnifying lens such as that used for indirect ophthalmoscopy, or a hand-held slit-lamp biomicroscope may be helpful.
➡️Cycloplegic Refraction
Determination of refractive error is important in the diagnosis and treatment of amblyopia or strabismus. Patients should undergo cycloplegic refraction with retinoscopy, followed by subjective refinement of refraction when possible (51). Cycloplegic autorefraction has also been shown to be an accurate means of assessing the refractive error of children and can be used in conjunction with retinoscopy and subjective refinement (52). Care must be made to ensure that adequate time passes following installation of cycloplegia agents. Adequate cycloplegia is necessary for accurate retinoscopy in children because of their increased accommodative tone compared with adults. One study found that noncycloplegic refraction compared with cycloplegic refraction among school-aged children resulted in a measurement of 0.65 D more myopia on average (53). Uncommon short-term side effects of cycloplegic agents may include hypersensitivity reactions, fever, dry mouth, tachycardia, nausea, vomiting, flushing, somnolence, and, rarely, behavioral changes (i.e., delirium). Punctal occlusion may be useful to reduce these side effects. (54-56) If the reaction is severe, the child should be referred to an emergency care setting and physostigmine may be given. See appendix 2
➡️Funduscopic Examination
The optic disc, macula, retina, vessels, and the choroid should be examined, preferably using an indirect ophthalmoscope and condensing lens after adequate dilation is achieved. It may be impossible to examine the peripheral retina of the awake young child. If necessary, examination of the peripheral retina with an eyelid speculum and scleral depression may require swaddling, sedation, or general anesthesia.
➡️OTHER TESTS
Based on the patient's history and findings, additional tests or evaluations that are not part of the routine comprehensive ophthalmic evaluation may be indicated. Components that may be included if the child cooperates are the sensorimotor evaluation, assessment of accommodation and convergence, color-vision testing, measurement of intraocular pressure (IOP), and imaging. Photography of facial or ocular structural abnormalities may be helpful for documentation and follow-up.
➡️Sensorimotor Evaluation
A sensorimotor examination consists of measuring binocular alignment in more than one field of gaze with sensory testing of binocular function when appropriate, which includes testing of binocular sensory status (stereoacuity or Worth 4-Dot); assessing diplopia-free visual field; measuring ocular torsion (double Maddox rods); and/or assessing whether horizontal, vertical, and torsional components require correction in order to restore binocular alignment (using a prism or a synoptophore).
➡️Assessment of Accommodation and Convergence
Testing the near point of accommodation and convergence and determining accommodative and fusional convergence amplitudes can be helpful in children with reading concerns. In a recent study, convergence insufficiency was reported to be present in 2% to 6% of 5th and 6th grade children and accommodative insufficiency in 10% (57) Noncycloplegic retinoscopy provides a rapid assessment of accommodation and may be helpful in evaluating a child with asthenopia who has high hyperopia or a child at risk for accommodative dysfunction, such as cerebral palsy, Down syndrome, or other types of developmental delay. (58-59) Accurate accommodation when viewing a small target on or near the retinoscope is seen as a neutral retinoscopic reflex or small degree of “with” movement. In dynamic retinoscopy, the examiner evaluates the change in the retinoscopic reflex from a “with” motion toward neutrality when the patient shifts fixation from distance to the near target. (60-61)
➡️Color-Vision Deficiency Testing
Color-vision deficiency testing is usually performed with pseudoisochromatic plates, and children who cannot yet identify numbers can instead identify simple objects (62-63). Eight percent of males and less than 1% of females are color deficient. (64) Color-vision testing is not routinely performed in asymptomatic children but can be useful in symptomatic children or when there is a family history. When identified in a young child, it can be useful for their teachers to be aware that it may be difficult for them to accurately identify certain colors.
➡️Intraocular Pressure Measurement
Intraocular pressure measurement is not necessary for every child because glaucoma is rare in this age group and, when present, usually has additional manifestations (e.g., buphthalmos, epiphora, photosensitivity, and corneal clouding in infants; myopic progression in very young children; and enlarged optic cups). Intraocular pressure should be measured whenever a child has or is at risk for glaucoma. Because IOP measurement can be difficult in some children, a separate examination with the patient sedated or anesthetized may be required. The introduction of more compact instruments such as the Tono-Pen (Reichert, Inc., Depew, NY, USA), Perkins tonometer (Haag-Streit UK Ltd., Harlow, United Kingdom), and iCare rebound tonometer (iCare Finland Oy, Helsinki, Finland) have facilitated testing (65-66). One advantage of the iCare is that topical anesthetic drops are not required; however, overestimation of IOP sometimes occurs (67) Central corneal thickness measurement may be helpful in interpreting IOP because thicker corneas may cause artificially high IOP readings and vice versa. (68-70)
➡️Imaging
Photography or imaging in conjunction with the comprehensive pediatric eye examination may be appropriate to document and follow changes of facial or ocular structural abnormalities. Examples of indications to image include external photography for orbital or adnexal masses, strabismus, ptosis, or facial structure abnormalities; photography and optical coherence tomography to document cataract and other anterior segment anomalies; corneal topography to detect early changes related to keratoconus; ultrasound for vitreous and/or retinal pathology; and autofluorescence for optic nerve head assessment. Optical coherence tomography of the retinal nerve fiber layer/ganglion cell layer and of the retina may be considered in young children for conditions such as unexplained visual loss, risk of ocular toxicity from medication, glaucoma suspect, optic neuropathy, retinal dystrophies, and ROP.
Appendix 2
Recommended cycloplegic agents
Table 1:
|
Age |
Recommended Agent |
Dosage |
Duration of Cycloplegia + Mydriasis |
Side Effect Profile |
|
Preterm to 3 months |
Cyclomydril (cyclopentolate 0.2% and phenylephrine 1%) |
Two sets of one drop separated by 5 minutes |
6 – 48 hours |
Minimal |
|
3 months to 1 year |
Cyclopentolate 0.5% |
Two sets of one drop separated by 5 minutes |
6-–48 hours+ |
Moderate |
|
1 year to 12 years |
Cyclopentolate 1% |
Two sets of one drop separated by 5 minutes |
6–48 hours+ |
Moderate |
|
Atropine 1% drops or ointment |
One drop twice a day for 3 days |
1–2 weeks+ |
High |
|
|
12 years and older |
Tropicamide 1% (may be used for younger children if cyclopentolate unavailable) |
Two sets of one drop separated by 5 minutes |
2–6+ hours |
Low |
At present, there is no ideal cycloplegic agent that has rapid onset and recovery, provides sufficient cycloplegia, and has no local or systemic side effects (54). Cyclopentolate hydrochloride 1% is useful because it produces rapid cycloplegia that approximates the effect of topical ophthalmic atropine 1% solution but with a shorter duration of action (55). Cyclopentolate 1% solution is typically used in term infants over 12 months old. The dose of cyclopentolate should be determined based on the child's weight, iris color, and dilation history. In eyes with heavily pigmented irides, repeating the cycloplegic eyedrops or using adjunctive agents, such as phenylephrine hydrochloride 2.5% (which has no cycloplegic effect) or tropicamide 1.0%, may be helpful to achieve adequate cycloplegia and dilation to facilitate retinoscopy and ophthalmoscopy. (54). Tropicamide (0.5%) and phenylephrine hydrochloride (2.5%) may also be used in combination to produce adequate dilation and cycloplegia. For children younger than 6 months, an eyedrop combination of cyclopentolate 0.2% and phenylephrine 1% is often used. (56). Some studies showed than low dose or very low dose phenylephrine and cyclopentolate microdrops for retinopathy of prematurity eye examinations may be sufficient (The Little Eye Drop Study): A randomised controlled non-inferiority trial. (71)
In some children, higher concentrations may be necessary, but should be with care of higher incidence of complications.
In rare cases, topical ophthalmic atropine sulphate 1% solution may be necessary to achieve maximal cycloplegia (55). The use of topical anesthetic prior to the cycloplegic reduces the stinging of subsequent eyedrops and promotes penetration of subsequent eyedrops. (57)
Appendix 3
Diagnosis and management points
When the eye examination is normal or indicates only a refractive error, and the child does not have risk factors for the development of eye disease, the ophthalmologist should establish an appropriate interval for re-examination. If re-examination has been determined to be unnecessary, patients should return for a comprehensive eye evaluation if new ocular symptoms, signs, or risk factors for ocular disease develop. Periodic vision screening should be continued. An evaluation every 6 months may be needed to evaluate progression.
When the history reveals risk factors for developing ocular disease or the examination shows potential signs of an abnormal condition, the ophthalmologist should determine an appropriate treatment and management plan for each child based on the findings and the age of the child.
When ocular disease is present, a treatment and management plan should be established, which may involve observation, eyeglasses, topical or systemic medications, occlusion therapy, eye exercises, and/or surgical procedures. The ophthalmologist should communicate the examination findings and the need for further evaluation, testing, treatment, or follow-up to parents/caregivers and the patient and the patient’s primary care physician or other specialists, as appropriate. Further evaluation or referral to other medical specialists may be advised.
Refractive correction is prescribed for children to improve visual acuity, alignment, and binocularity and to reduce asthenopia. Refractive correction plays an important role in the treatment of amblyopia and strabismus. Table 2 provides guidelines for refractive correction in infants and young children. Smaller amounts of refractive error may also warrant correction depending on the clinical situation. (SEE THE GUIDELINES ON MANAGEMENT OF REFRACTIVE ERRORS IN CHILDREN FOR MORE DETAILS)
Factors that help children to wear eyeglasses successfully include a correct prescription, frames that fit well, and positive reinforcement. Children require updates in eyeglasses much more frequently than adults owing to eye growth and associated changes in refraction. Infants and children with cerebral visual impairment or Down syndrome, and children on prescribed seizure medication may have poor accommodation and, therefore, require correction for smaller amounts of hyperopia compared with typically developing infants and toddlers.
For the youngest children, an evaluation every 6 months may be needed to evaluate progression.
- REFERENCES
1. Yekta, A., Hooshmand, E., Saatchi, M., Ostadimoghaddam, H., Asharlous, A., Taheri, A. and Khabazkhoob, M., 2022. Global prevalence and causes of visual impairment and blindness in children: A systematic review and meta-analysis. Journal of Current Ophthalmology, 34(1), p.1.
2. https://www.statista.com/statistics/1230371/total-population-of-egypt-by-age-group/
3. https://www.aaojournal.org/article/S0161-6420(22)00866-1/pdf#:~:text=Pediatric%20Eye%20Evaluations%20PPP,-P229&text=A%20more%20accurate%20assessment%20of,crowd)%20the%20optotype%20being%20identified.
4. https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf
5. https://iris.who.int/bitstream/handle/10665/145714/9789241548960_eng.pdf?sequence=1
6. Wang J, Ren X, Shen L, et al. Development of refractive error in individual children with regressed retinopathy of prematurity. Invest Ophthalmol Vis Sci 2013; 54:6018-24.
7. Eibschitz-Tsimhoni M, Friedman T, Naor J, et al. Early screening for amblyogenic risk factors lowers the prevalence and severity of amblyopia. J AAPOS 2000; 4:194-99.
8. Atkinson J, Braddick O, Nardini M, Anker S. Infant hyperopia: detection, distribution, changes and correlates-outcomes from the Cambridge infant screening programs. Optom Vis Sci 2007; 84:84-96.
9. Holmes JM, Lazar EL, Melia BM, et al. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol 2011; 129:1451-57.
10. U.S. Preventive Services Task Force. Vision screening for children 1 to 5 years of age: US Preventive Services Task Force Recommendation statement. Pediatrics 2011; 127:340-46.
11. Dobson V, Clifford-Donaldson CE, Green TK, et al. Optical treatment reduces amblyopia in astigmatic children who receive spectacles before kindergarten. Ophthalmology 2009; 116:1002-8.
12. Kemper AR, Wallace DK, Patel N, Crews JE. Preschool vision testing by health providers in the United States: findings from the 2006-2007 Medical Expenditure Panel Survey. J AAPOS 2011; 15:480-83.
13. Jones-Jordan LA, Sinnott LT, Manny RE, et al. Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci 2010; 51:115-21.
14. Kulp MT, Ciner E, Maguire M, et al. Uncorrected hyperopia and preschool early literacy: results of the Vision in Preschoolers-Hyperopia in Preschoolers (VIP-HIP) study. Ophthalmology 2016;123:681-89.
15. Shankar S, Evans MA, Bobier WR. Hyperopia and emergent literacy of young children: pilot study. Optom Vis Sci 2007; 84:1031-38.
16. van Rijn LJ, Krijnen JS, Nefkens-Molster AE, et al. Spectacles may improve reading speed in children with hyperopia. Optom Vis Sci 2014; 91:397-403.
17. Gwiazda J, Deng L, Manny R, Norton TT. Seasonal variations in the progression of myopia in children enrolled in the Correction of Myopia Evaluation Trial. Invest Ophthalmol Vis Sci 2014; 55:752-58.
18. Comet Group. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci 2013; 54:7871-84.
19. Tongue, A.C. and Cibis, G.W., 1981. Brückner test. Ophthalmology, 88(10), pp.1041-1044
20. Rajalakshmi AR, Rajeshwari M. Efficacy of Bruckner's test for screening of refractive errors by nonophthalmologist versus ophthalmologist: A comparative study. Middle East Afr J Ophthalmol. 2019;26:185-188.
21. American Academy of Ophthalmology Basic and Clinical Science Course Subcommittee. Basic and clinical science course. Pediatric ophthalmology and strabismus: Section 6, 2022-2023. San Francisco, CA: American Academy of Ophthalmology; 2022.
22. American Association for Pediatric Ophthalmology and Strabismus. Policy Statement. Refractions in children. San Francisco, CA: American Association for Pediatric Ophthalmology and Strabismus; 2012. https://aapos.org/HigherLogic/System/DownloadDocumentFile.ashx?DocumentFileKey=99eb2c55-1e37-f226-0a58-34dca1cc1165. Accessed August 25, 2022.
23. Lanca CC, Rowe FJ. Measurement of fusional vergence: A systematic review. Strabismus. 2019;27:88-113.
24. Lagstein O, Hecht I, Anteby I. Comparison of a new, filter-free stereopsis test (BEST) with the RandotStereotest in a pediatric cohort. J Pediatr Ophthalmol Strabismus. 2020;57:129-135.
25. Procianoy L, Procianoy E. The accuracy of binocular fixation preference for the diagnosis of strabismic amblyopia. J AAPOS. 2010;14:205-210.
26. Sener EC, Mocan MC, Gedik S, et al. The reliability of grading the fixation preference test for the assessment of interocular visual acuity differences in patients with strabismus. J AAPOS. 2002;6:191-194.
27. Wright KW, Walonker F, Edelman P. 10-diopter fixation test for amblyopia. Arch Ophthalmol.
28. 1981;99:1242-1246.
29. Frank JW. The clinical usefulness of the induced tropia test for amblyopia. Am Orthopt J. 1983;33:60-69.
30. Wallace DK. Tests of fixation preference for amblyopia. Am Orthopt J. 2005;55:76-81.
31. Friedman DS, Katz J, Repka MX, et al. Lack of concordance between fixation preference and HOTV optotype visual acuity in preschool children: The Baltimore Pediatric Eye Disease Study. Ophthalmology.2008;115:1796-1799.
32. Cotter SA, Tarczy-Hornoch K, Song E, et al. Fixation preference and visual acuity testing in a population-based cohort of preschool children with amblyopia risk factors. Ophthalmology. 2009;116:145-153. Hakim OM. Association between fixation preference testing and strabismic pseudoamblyopia. J Pediatr Ophthalmol Strabismus. 2007;44:174-177.
33. World Health Organization. Consultation on development of standards for characterization of vision loss and visual functioning. Geneva, 4-5 September 2003. Accessed August 25, 2022 https://apps.who.int/iris/handle/10665/68601. Accessed August 25, 2022.
34. Morale SE, Hughbanks-Wheaton DK, Cheng C, et al. Visual acuity assessment of children with special needs. Am Orthopt J. 2012;62:90-98.
35. Vision in Preschoolers Study Group. Preschool vision screening tests administered by nurse screeners compared with lay screeners in the vision in preschoolers study. Invest Ophthalmol Vis Sci. 2005;46:2639-2648.
36. Cyert L, Schmidt P, Maguire M, et al. Vision in Preschoolers (VIP) Study Group. Threshold visual acuity testing of preschool children using the crowded HOTV and Lea symbols acuity tests. J AAPOS. 2003;7:396-399.
37. Committee on Vision. Recommended standard procedures for the clinical measurement and specification of visual acuity. Report of Working Group 39. Assembly of Behavioral and Social Sciences, National Research Council, National Academy of Sciences, Washington, D.C. Adv Ophthalmol. 1980;41:103-148.
38. Candy TR, Mishoulam SR, Nosofsky RM, Dobson V. Adult discrimination performance for pediatric acuity test optotypes. Invest Ophthalmol Vis Sci. 2011;52:4307-4313.
39. Hyvarinen L, Nasanen R, Laurinen P. New visual acuity test for pre-school children. Acta Ophthalmol (Copenh). 1980;58:507-511.
40. Vision in Preschoolers (VIP) Study Group. Effect of age using Lea symbols or HOTV for preschool vision screening. Optom Vis Sci. 2010;87:87-95.
41. Chaplin PK, Bradford GE. A historical review of distance vision screening eye charts: What to toss, what to keep, and what to replace. NASN Sch Nurse. 2011;26:221-228.
42. Rentschler I, Hilz R, Brettel H. Spatial tuning properties in human amblyopia cannot explain the loss of optotype acuity. Behav Brain Res. 1980;1:433-443.
43. Stager DR, Everett ME, Birch EE. Comparison of crowding bar and linear optotype acuity in amblyopia. Am Orthopt J. 1990;40:51-56.
44. Youngson RM. Anomaly in visual acuity testing in children. Br J Ophthalmol. 1975;59:168-170.
45. Ying GS, Kulp MT, Maguire M, et al. Sensitivity of screening tests for detecting vision in preschoolerstargeted vision disorders when specificity is 94%. Optom Vis Sci. 2005;82:432-438.
46. Morad Y, Werker E, Nemet P. Visual acuity tests using chart, line, and single optotype in healthy and amblyopic children. J AAPOS. 1999;3:94-97.
47. Saarela TP, Westheimer G, Herzog MH. The effect of spacing regularity on visual crowding. J Vis. 2010;10:17.
48. Drover JR, Wyatt LM, Stager DR, Birch EE. The teller acuity cards are effective in detecting amblyopia. Optom Vis Sci. 2009;86:755-759.
49. Friendly DS, Jaafar MS, Morillo DL. A comparative study of grating and recognition visual acuity testing in children with anisometropic amblyopia without strabismus. Am J Ophthalmol. 1990;110:293-299.
50. Portnoy JZ, Thompson HS, Lennarson L, Corbett JJ. Pupillary defects in amblyopia. Am J Ophthalmol.1983;96:609-614.
51. Wilson LB, Melia M, Kraker RT, et al. Accuracy of autorefraction in children: A report by the American Academy of Ophthalmology. Ophthalmology. 2020;127:1259-1267.
52. Guo X, Shakarchi AF, Block SS, et al. Non-cycloplegic compared with cycloplegic refraction in a Chicago school-aged population. Ophthalmology. 2022.
53. Fan DS, Rao SK, Ng JS, et al. Comparative study on the safety and efficacy of different cycloplegic agents in children with darkly pigmented irides. Clin Experiment Ophthalmol. 2004;32:462-467.
54. Rosenbaum AL, Bateman JB, Bremer DL, Liu PY. Cycloplegic refraction in esotropic children. Cyclopentolate versus atropine. Ophthalmology. 1981;88:1031-1034.
55. Khoo BK, Koh A, Cheong P, Ho NK. Combination cyclopentolate and phenylephrine for mydriasis in premature infants with heavily pigmented irides. J Pediatr Ophthalmol Strabismus. 2000;37:15-20.
56. Apt L, Henrick A. Pupillary dilatation with single eyedrop mydriatic combinations. Am J Ophthalmol.1980;89:553-559.
57. Nunes AF, Monteiro PML, Ferreira FBP, Nunes AS. Convergence insufficiency and accommodative insufficiency in children. BMC Ophthalmol. 2019;19:58.
58. Satgunam P, Datta S, Sumalini R. Near vision in individuals with Down syndrome: A vision screening study. Eye (Lond). 2019;33:1254-1260.
59. Guyton DL, O'Connor GM. Dynamic retinoscopy. Curr Opin Ophthalmol. 1991;2:78-80.
60. McClelland JF, Parkes J, Hill N, et al. Accommodative dysfunction in children with cerebral palsy: A population-based study. Invest Ophthalmol Vis Sci. 2006;47:1824-1830.
61. Hunter DG. Dynamic retinoscopy: The missing data. Surv Ophthalmol. 2001;46:269-274.
62. Seshadri J, Lakshminarayanan V. Screening efficiency of the Hardy-Rand-Rittler (HRR) colour test (4thedn). J Mod Opt. 2007;54:1361-1365.
63. National Center for Health Statistics. Color vision deficiencies in youths 12-17 years of age. United States. Vital Health Stat, Ser 11, DHEW Publ no. (HRA) 74-1616, no. 134, 1974.
64. Gandhi NG, Prakalapakorn SG, El-Dairi MA, et al. Icare ONE rebound vs Goldmann applanation tonometry in children with known or suspected glaucoma. Am J Ophthalmol. 2012;154:843-849.
65. Lambert SR, Melia M, Buffenn AN, et al. Rebound tonometry in children: A report by the American Academy of Ophthalmology. Ophthalmology. 2013;120:e21-27.
66. Flemmons MS, Hsiao YC, Dzau J, et al. Icare rebound tonometry in children with known and suspected glaucoma. J AAPOS. 2011;15:153-157.
67. Lopes JE, Wilson RR, Alvim HS, et al. Central corneal thickness in pediatric glaucoma. J Pediatr Ophthalmol Strabismus. 2007;44:112-117.
68. Tai TY, Mills MD, Beck AD, et al. Central corneal thickness and corneal diameter in patients with childhood glaucoma. J Glaucoma. 2006;15:524-528.
69. Dai E, Gunderson CA. Pediatric central corneal thickness variation among major ethnic populations. JAAPOS. 2006;10:22-25.
70. Pediatric Eye Disease Investigator Group. Central corneal thickness in children. Arch Ophthalmol. 2011;129:1132-1138.
71. Lisa Jean Kremer, Natalie Medlicott , Mary Jane Sime et al. Low dose or very low dose phenylephrine and cyclopentolate microdrops for retinopathy of prematurity eye examinations (The Little Eye Drop Study): a randomised controlled non-inferiority trial. Arch Dis Child Fetal Neonatal Ed 2023 Jul;108(4):380-386.