Part Two
| Site: | EHC | Egyptian Health Council |
| Course: | Procedural work guide for the renal unit |
| Book: | Part Two |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 5:01 PM |
Table of contents
- - Public Policies
- - Nursing Plan Policy
- - Medical Files
- - Expected Events Policy
- - Policies for unexpected events
- - Patient Rights Policy
- - Patient complaints and suggestions policy
- - Patient safety and security policy
- - Policy for dealing with high-risk medications (including concentrated solutions)
- - Private policies
- - Patient reception policy
- - Machine care policy
- Public Policies
· A brief overview of the policies
· Evaluation policies
· Policy on assessment areas and content
· Timeframe policy for completing the assessment
· Minimum frequency and re-evaluation content policy
· Pain assessment, re-evaluation and management policy
· Nursing plan policy
· Nursing registration policy
· Policy for assessing patients for abuse or neglect
· Minimum medical history and clinical examination policy
· The policy of identifying the categories of hospital patients most at risk
· Medical files
· Policy for uniform and consistent content of the patient’s medical file
· The policy of who has the authority to write in the patient’s medical file
· The policy of who has the right to view the patient’s medical file to ensure the confidentiality of the information
· The policy of protecting medical records and information from loss, damage, tampering, and unauthorized use or access
· Medical files disposal policy and the duration of keeping records and files
· Screening process policy to determine patients' medical and nursing care needs
· Policy of information given to the patient and family upon admission to the hospital
· Patient management policy in the event that there is no available space for the requested medical service
· The policy of coordination and cooperation between all departments (including doctors and nursing staff) through the internal departments
· Policy for terminally ill patients
· Patient transfer, referral and discharge policy
· The hospital’s medical emergency response policy
· Health education policy for patients and their families
· Unforeseen events policies
· Incident reporting policy
· Policy for intensive analysis when unexpected events occur
· A list of facts that can be reported
· Patient rights policy
· Patient responsibilities policy towards the hospital
· The policy of refusing or not continuing treatment for the patient
· Patient complaints and suggestions policy
· Policy for obtaining informed written consent
· The policy of informing the patient of the outcome and expected costs
· Patient property preservation policy
· Patient safety and security policies
· General standards
· Correct patient identification policy
· Patient delivery and receipt policy
· Policy to avoid incorrect connection of catheters and tubes
· The policy of preventing patient falls and taking the necessary measures to avoid falls
· Policy for the safe use of restraint and seclusion
· Critical Consequences and Critical Warnings Policy
· Medication-specific standards
· Policy for handling high-risk medications (including concentrated solutions).
· A list of high-risk medications
· The policy of obtaining a list of the treatment that the patient takes when entering the hospital and upon discharge
· Policy on medicines that are similar in form and pronunciation
· A list of medications that are similar in appearance and pronunciation
· Policy for labeling medicines and their containers
· A list of abbreviations that should not be used in writing medications
A brief overview of the policies
The policies that will be presented are just a model, and the hospital has the right to make the policy in accordance with its work system.
The policy is reviewed every three years unless there is any change in it during those three years.
At the beginning of each policy, fill out the table as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
At the end of each policy, fill out the table as follows:
|
|
|
|
|
|
|
|
|
|
Evaluation areas and content policy according to each department
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital is committed to clarifying the areas and contents of the evaluation according to the Artificial Kidney Unit section.
Purpose: To clarify the areas and contents of the assessment according to each section, which helps to provide appropriate medical care to the patient, reach an accurate diagnosis, and develop a treatment plan.
Working procedures:
First: The treating physician:
1- The initial patient evaluation must include identifying the patient’s personal history, complaints, and family history.
2- Initial patient evaluation must clarify the patient’s medical history and medical examination, which includes (vital signs - examination of body systems according to specialty and condition).
3- Reviewing the results of any evaluation conducted on the patient outside the hospital (medical report) before admitting the patient for treatment inside the hospital.
4- Identifying the patient’s previous treatments and the extent of his response to them in order to:
· Determine the initial diagnosis.
· Determine the research required for the patient.
· Develop an appropriate treatment plan.
· Identifying the patient’s medical care needs and choosing the best care for him.
5- The doctor re-examines the patient clinically after reviewing the patient’s complete medical history, within 24 hours of the patient’s admission to the hospital, in accordance with the medical history and medical examination form.
6- Each of the departments determines the content of the medical evaluation according to the specialty and clinical work guides (heart, women, dialysis, premature infants).
7- The doctor records the diagnosis, examination results, and medical history in the patient’s file and signs it with the date and time.
8- The doctor re-evaluates the patient based on the results of the tests and examinations and the progress of his health condition. He registers and signs, writing the date and time in the patient’s file.
Secondly, nursing:-
· The nursing staff evaluates the patient upon admission to the hospital using the nursing evaluation form.
· Initial information and data are recorded when the patient enters the department on the patient’s nursing evaluation form:
- Vital signs (pressure - pulse - respiratory rate - temperature).
- Weight and height.
- The presence of allergies.
- Pain assessment
- Evaluation of skin condition
- Assess the patient regarding the possibility of a fall
- Nutritional assessment.
- Evaluation of motor activity.
- The patient’s need for restraint or isolation.
- Informing the patient of his rights, responsibilities, and hospital policy within 24 hours of admission.
Third, anesthesia:
The anesthesiologist assesses the patient's condition:
Before administering anesthesia according to a pre anesthesia sheet form showing the type of anesthesia planned.
Observing and evaluating the patient during anesthesia according to the form prepared for this purpose.
Evaluating the patient before leaving the recovery room according to the recovery model.
Fourth: Physiotherapist
(Assessing motor, functional, and rehabilitative activity if the patient needs it).
Fifth: The treating physician
Assessing the nutritional needs of patients, especially cases that are sorted according to the evaluation
Nursing upon admission.
Sixth: The social worker
According to his job description (he verifies patient satisfaction, and conducts social research when the patient needs financial, material, educational, or social support).
Responsible: the doctor - the nursing staff - the social worker.
Forms: (medical report - patient ticket - emergency form - nursing evaluation - anesthesia sheet - physical therapy form - patient satisfaction questionnaire).
References: Egyptian accreditation standards.
|
Preparation |
Review |
Confidence |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
Re-evaluating patients in critical and non-critical cases that require long-term (chronic) treatment.
The Purpose :
Ensure proper follow-up and continuity of patient care and evaluation
Working procedures :
First: In acute cases (care - premature infants):
The treating physicians in the departments evaluate and determine the following
Degree of awareness and awareness.
Vital Signs .
Complications occur.
Results of tests and treatment or (surgical interventions).
The extent of response to treatment
The nursing evaluation rate is continuous, and the doctor on duty is called to the department for a critical result (physiological - laboratory - x-ray) and when there is pain, and the doctor re-evaluates.
The re-evaluation of the patient is documented and a follow-up note is recorded at least once per shift (every 24 hours), and any procedures resulting from a call or emergency or important events for the patient are recorded by date and hour.
Second: In non-acute cases:-
Treating doctors evaluate patients in non-acute cases and ensure...
Vital Signs .
Complications occur
Test results and treatment
Patient compliance with treatment and medical instructions.
This is done every 12 hours for the internal department by the specialist or doctor on duty, unless the clinical evidence requires less than that and this is documented in the patient’s file.
Third: Conditions that require long-term treatment (chronic diseases)
The doctors treating the departments that care for patients who need long-term or (chronic) treatment ensure that:
Vital Signs .
Complications occur
Results of tests and treatment
How advanced the disease is
The frequency of re-evaluation shall be once a day by the doctor on duty or as required by clinical evidence and documented in the patient’s file.
The specialist doctor re-evaluates the patient from various specialties while the patient is in the hospital to determine the extent of the response to the treatment and its effectiveness.
The nursing staff on duty re-evaluates the patient each shift to determine the patient's needs
Fourth: Cases that need to be re-evaluated
The treatment plan developed for the patient Individualized care plan
Change in patient condition
Diagnosis: Patient diagnosis
Expected outcome of care, treatment or service
The extent of the patient's response to previous treatment
The re-evaluation is documented in the patient's file
The patient should be re-evaluated immediately before anesthesia is administered
Fifth: Content of re-evaluation for nursing
Vital signs: every 6 hours in inpatient departments, every 2 hours in care and premature care, after blood transfusion, before surgical operations, during recovery, and when the patient complains that requires re-measurement, or according to the doctor’s instructions.
The Pain:
Probability of patient falling: every shift.
Skin condition: all skin color during recovery.
Nutritional assessment: when the patient needs it, according to the doctor’s orders.
Measuring blood sugar: according to the doctor’s instructions.
The patient's need for restraint or isolation: according to the doctor's orders
Models:
Medical follow-up form.
the reviewer :
Egyptian accreditation standards.
|
Preparation |
Review |
Confidence |
|
|
|
|
Pain assessment, re-evaluation and management policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital is committed to a process of assessment, re-evaluation and pain management
Purpose: To clarify the process of assessment, re-evaluation, and treatment of pain.
procedures :
1- The responsible nursing staff assesses the pain (according to the following table), determines its severity, describes the pain, and its frequency by asking the patient and looking at the patient’s facial expression (in the event that he is unable to speak or in the event that he is a child), and this is recorded in the pain assessment form and kept in the patient’s file. When the patient enters the hospital.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Policy for assessing patients for abuse or neglect
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy : The hospital is committed to preventing harm or neglect to patients while they are in the hospital and dealing with such cases as soon as they occur to eliminate harm or neglect to patients while dealing with them.
Purpose: Develop methods for dealing with patients in cases of abuse or neglect.
Mistreatment: The patient while he is in the hospital, which leads to him being exposed to physical or psychological harm/injury, or both. There are types
Different types of mistreatment can be divided into:
Mental ill-treatment : by affecting the mental state.
Manifestations of mental abuse:
- Verbal assault
- To threaten
- Intimidation
- Isolation
- Insult
- Humiliation
- Deprivation
Physical mistreatment: by affecting the patient’s physical condition by exposing the patient to (beating, slapping, kicking)
Manifestations of physical abuse:
· The patient falls
· The appearance of bed sores in the patient
· The presence of wounds that are not well cared for
· Unexplained injuries
· Physical pain when touched
· The presence of marks resulting from bites, scratches, abrasions or bruises
· Unexplained signs of dehydration and malnutrition, sickness, sunken eyes, or eye injuries
· The presence of blood stains in the underwear
Sexual mistreatment: The patient is exposed to any form of sexual assault/harassment
Physical abuse:
Manifestations of physical abuse:
· theft
· Misuse of money and property
· blackmail
· scam
· There are abnormal actions in the patient’s bank account
· Indifference to spending money
Negligence:
It is any negligence [negligence in treatment] harming a patient in need without an acceptable medical reason from a responsible person while the patient is in the hospital.
· People in need: A person who needs the help of another due to (mental disability, age, or brain atrophy/functional dysfunction) which hinders the person’s ability to protect himself or provide his own care.
· Types of negligence to which the patient may be exposed:-
· - Negligence in medical and nursing care - Neglecting to administer treatment doses
· - Neglect of social and psychological needs - Lack of food/water
· - Placing the patient in an unsafe or unsupervised place
procedures :
· The doctor and nursing staff evaluate the patient’s condition and determine his treatment needs.
· The doctor and nursing staff inform the patient of the treatment plan and how to implement it.
· The nursing staff teaches the patient how to call her when needed
· The social worker visits patients in all departments daily to monitor patients’ complaints in order to report them to management and those responsible for resolving their complaints.
· In the event that a case of neglect or abuse is discovered, the patient’s treating physician shall be informed:
· - The doctor evaluates the patient’s condition and identifies manifestations of abuse or neglect, and a report is written with a commitment to physical and psychological treatment of the cases.
· - The doctor asks the patient to write down his complaint (for the damages he suffered), if he so desires, with or without a signature.
· - The head of the medical board assigns whomever he deems appropriate to investigate and follow up on the complaint, then the results are presented to him for necessary action.
Responsible: - Doctor - Nursing staff - Social worker.
Forms:- Patient Rights and Duties Form - Form for acknowledging the existence of trusts
|
Preparation |
Review |
Confidence |
|
|
|
|
- Nursing Plan Policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The purpose :
Understand the patient's needs and meet them.
Providing high-quality nursing care.
Politics :
The Services Department is committed to providing nursing care according to the patient’s needs and documenting it in the nursing care plan for each patient.
Steps:
The nursing team does:
Conduct a nursing assessment of the patient upon admission and determine the patient's problems.
Recording the patient's nursing problems in the nursing plan, which includes: (problems/needs - nursing intervention - evaluation - signature).
Writing the necessary procedures to help solve nursing problems.
Re-evaluation to determine the extent of the patient’s response to nursing interventions.
The department supervisor follows up the plan and implements its procedures.
Administrator :
Department Supervisor - Nursing staff members in the department.
Models:
Nursing care plan template.
The Reviewer :
Comprehensive hospital accreditation guides.
|
|
|
|
|
|
|
|
Nursing registration policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The purpose:
1. Record all patient data.
2. Teaching health team members to register on nursing forms in a correct, accurate and legible manner.
Politics:
The Nursing Services Department is committed to accurate nursing registration 24 hours a day in a correct, accurate and legible manner
Steps:
The nursing team members do:
1. Recording every activity performed by the patient from the moment he enters his form.
2. The team begins by assessing the patient using the prepared form.
3. The patient’s main complaint is identified and needs are determined.
4. Planning the care that will be provided to the patient.
5. Implement the plan carefully to get the desired results.
6. Evaluate the plan each shift to identify the development of the situation.
7. Repeat any of the steps in the plan that did not improve the patient’s condition.
8. Monitor vital signs and notify the doctor when there is any change from normal levels.
9. The necessity of working and submitting a report on any emergency incident during the work period, such as (patient falling - patient escaping - error in administering treatment).
10. The health team members must pay attention to recording the nursing progress, which includes (the patient’s condition - the doctor’s recommendations - all medical procedures, tests, and rumors - and surgical interventions - the nursing intervention - the patient’s evaluation of no new signs and symptoms).
Administrator :
Members of the nursing staff in the department - the department supervisor.
Model:
Nursing notes - nursing assessment - vital signs - nursing care plan - treatment charts
The reviewer:
Operational guide for nursing staff services at the Ministry of Health.
|
|
|
|
|
|
|
|
Minimum medical history and clinical examination policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital is committed to setting the minimum requirements for a patient’s medical examination upon admission.
Purpose: To determine the minimum medical examination and medical history necessary to evaluate the patient upon admission to the hospital.
Working procedures:-
1. The department doctor takes a medical history and examines the patient upon admission according to the medical history and medical examination form, which includes:
· The patient’s personal history, which explains (full name - gender - age - profession - marital status according to the national ID card - special habits such as smoking and drinking alcohol).
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. The doctor conducts a clinical examination of the patient, which includes:
Measuring vital signs (pressure, pulse, temperature).
A comprehensive examination of all parts of the patient’s body.
Local examination of the patient's complaint using various manual examination methods.
The doctor records the examination result and results from the date of admission and the clinical examination in the patient’s file (initial diagnosis).
The doctor records the initial treatment plan
3. The doctor, based on his findings and according to the patient’s need, orders in writing on the doctor’s order form to perform the necessary tests and x-rays for the patient and determines the notes of vital signs that will be taken and the dates for their recording by the department’s nurses.
4. The doctor writes the drug treatment accurately in the treatment description and implementation form.
5. The doctor determines the type of nutrition appropriate for the patient on the doctor’s order form.
6. The nursing staff records the patient’s data on the food form to bring meals to the patient.
7. The treating physician informs the patient and his family of the initial diagnosis, treatment or surgery plan, potential results, expected complications, and nutritional regimen.
Responsible: the specialist doctor
Forms: Medical History and Medical Examination Form - Food Form - Doctor's Orders Form.
References: Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy for identifying categories of hospital patients most at risk
|
|
Identifying the categories of hospital patients most at risk |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Patients in critical condition who are most at risk must be identified and followed up. Then the medical team begins the evaluation process and the plan is coordinated and implemented with the patient and family.
The purpose:
Identifying patients most at risk, such as children, individuals with special needs, the elderly, and psychiatric patients in the hospital, and the special evaluation required for each of them.
Medical cases that require special services regarding hospital care:
Age 75 years or older
Altered state of consciousness or related disorders (mental disorders).
Traumas, multiple fractures, fractures of major joints.
Malnutrition, dehydration, microbial poisoning.
Patients with late cases.
children.
Victims of abuse, neglect or injury.
Dialysis patients.
Intensive care patients.
Chronic disease patients.
Patients at risk of falling.
Patients prone to bed sores.
Patients taking sedative medications and diuretics.
Procedures:
The medical team matches the at-risk cases to each patient within 24 hours of his admission to the hospital, and if the patient’s condition matches one of the following cases, the patient’s expected risk signs are determined.
Doctors and nurses record current and anticipated problems and major and alternative solutions in care plans.
Doctors and nurses follow up the cases and re-evaluate them according to the requirements of each case.
|
|
|
|
|
|
|
|
- Medical Files
Policy for uniform and consistent content of the patient's medical file
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The Purpose:
Familiarity of staff with the consistent composition of the patient’s medical record.
Politics:
· Having a medical record for every patient examined and treated.
· The fixed composition of the patient’s medical record contains sufficient information such as:
◾ Identify the patient by name - address - file number
◾ Allows for continuity of care
◾ Confirm the diagnosis
◾ Justification for treatment
◾ Documentation of treatment steps and results
· The components of medical records for patients in the hospital are standardized and have a specific format, and doctors and nurses are committed to using the forms in optimal use and they contain:
◾ Writing treatment orders in a unified manner and in the same place.
· Department nurses are obligated to familiarize the patient with all patient record forms, which contain:
◾ Patient’s name is four-digit number
· Test reports, rumors, the medical report, and a copy of the discharge summary are included in the patient’s file.
· The medical team corrects or amends one of the data recorded in the medical record by placing parentheses around the inaccurate data, taking into account ensuring that it is still possible to read it, sign in front of it, and record the date and time of making the correction, as it is not permissible to erase or delete incorrect data.
· The availability of data related to the consultations as evidence that the consulting physician reviewed the patient’s medical record and the results he reached when conducting the medical examination on him, as well as the consulting physician’s opinion and recommendations.
· Issuing verbal diagnostic and therapeutic orders to qualified nursing personnel. The orders must be signed within twenty-four (24) hours, and all orders must bear the date, time, signature, and procedures applied.
· The clinical data recorded in the medical record and any other data and signatures are clear and legible.
· Send a referral form with the patient when he is transferred to another hospital, while keeping a copy in the patient’s file.
· Giving the patient a discharge summary with complete information
Procedures:
· Nursing staff members ensure that the file contains the following data upon entry:
· Patient’s full name - uniform number - age
· Name, address and telephone number of a relative of the patient or someone who can be contacted in case of emergency.
· Nursing staff members do the following:
· Writing the patient’s full name and uniform number on all pages of the medical file.
· Recording the patient’s vital signs and medical condition in the vital signs register and the nursing staff’s observations register
· Modify the treatment implementation plan according to the doctor’s amendment on the doctor’s orders page.
· Doctors do the following:
· Complete the patient examination record and the record contains the following data:
· The type of allergy the patient suffers from, if any.
· Whether the patient suffers from any chronic infectious disease such as hepatitis C
· Diagnosis when the patient is admitted to the hospital
· The patient’s complete medical history: previous, current, and family medical history
· A detailed statement of the patient’s clinical examination, a statement of the results drawn, and the action plan
· Mention the results of laboratory tests and x-rays
· Clearly write the type of treatment applied on the doctor’s orders page.
· Request all required examinations or tests on the Clinical Progress page
· Record all types of routine and special follow-up, consultations and treatments appropriately on the appropriate forms.
· Take notes on the development of the condition at least daily for patients with serious conditions, as well as for patients whose conditions are difficult to diagnose or control their clinical problems. Notes of the development of the condition must also be recorded at the time of the observation to allow for continuity of care and the possibility of transferring the patient from one department to another. Also, as much as possible, it must be determined Each of the problems that the patient suffers from should be clearly stated in the case progress notes and linked to the orders issued regarding it, as well as the results of examinations and treatment. On the other hand, comprehensive notes about the development of the condition during the surgical procedure and immediately after the completion of the surgery must be recorded in the record. This is done for the purpose of providing correct information for use by any caregiver who subsequently assumes responsibility for caring for the patient
· Writing all operating reports immediately after the end of the surgical operation, provided that they include the patient’s full name, medical file number, date of the surgical operation, diagnosis before and after the surgical operation, the name of the surgeon and his assistant, the name of the surgical operation, and a detailed statement of the results and methods used during the operation and anesthesia. The samples taken, the amount of fluid secreted, complications, reasons for surgery, and the patient’s condition before the operation.
Writing a summary of discharge or death in all medical files of patients admitted to the hospital, which includes:
· Check-in and check-out dates
· Initial diagnosis - final diagnosis
· Analysis
· Actions taken
· Prescription drugs and other treatments
· Patient condition and next stop upon discharge
· Discharge instructions, including food, medication and follow-up instructions
· The name of the doctor who discharged the patient
· Fill out the referral form as follows:
· Reason for referral
· The required means of transportation and follow-up
· Description of the condition
· next station
· The emergency patient’s medical file contains:
· Patient arrival time and discharge time
· Final results at the end of treatment
· Patient’s condition upon discharge
· The patient’s destination upon discharge
· Medical care instructions for patient follow-up
· Documentation of the discharge order from the treating physician
Administrator:
· Nursing staff and medical staff.
Models:
· Patient records – content of the medical file for each department.
The reviewer :
· Medical records guide for the Ministry of Health.
|
|
|
|
|
|
|
|
The policy of who has the authority to write in the patient’s medical file
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The medical team, including nurses and treating doctors, is authorized to write in the patient’s medical file their names, clear and legible, and their job titles, provided that the information is clear and in legible handwriting, with the date and hour written.
The purpose:
Determine who has the authority to write in the medical file.
Procedures:
· When recording their performance in patient files, nursing staff members are obligated to write their names (first name) and record the date and hour.
· When registering in patient files, doctors are obligated to write their names (first name), use scribbles, and write the date and hour.
· All research, examinations and treatments requested for the patient must be signed by the treating physician, with his name written in three letters and his stamp.
· The person performing the medical tests and x-rays signs the results of the tests and x-ray reports with his or her full name or his own letter and writes the date and hour.
Administrator:
Nursing staff and medical staff.
|
|
|
|
|
|
|
|
The policy of who has the right to view the patient’s medical file to ensure the confidentiality of the information.
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The medical record is considered a legal document and therefore its confidentiality must be maintained, and this confidentiality is the basis of the legal aspect of the medical record.
· Establish controls to maintain the confidentiality of information and determine who has the right to view the medical record and what data they are permitted to view.
Purpose: Maintaining and protecting the confidentiality of patient information and data.
Procedures:
· All hospital employees sign a declaration of confidentiality of patient information.
Circumstances in which access to information in the medical file is permitted:
· If the file is requested from the medical team to view the patient’s examinations or information of clinical value, the doctor writes a request to extract the previous file in the current file, the doctor signs it clearly and with the date, then submits the file to the medical records official to extract the medical file.
· In the event that the sick applicant is himself, his legal representative, or external parties such as (the Administrative Prosecution - the Public Prosecution - Inspection Bodies - the Ministry of Health), the hospital director or medical director shall review the request and provide the information in one of the following ways:
◾ Orally.
◾ An exact copy of the file.
◾ Summary of the case.
◾ The original file. In this case, a representative from the hospital will refer the file and return it after the decision on it is completed.
· In the event that the patient is transferred to another hospital, the specialist doctor fills out the transfer form, which includes a summary of the case
(Diagnosis - reason for transfer)
· In the event of requesting a medical report on a case, the patient or his legal representative submits a verbal request to the official of the Medical Records Office to contact the treating physician to write the report on the case. This is done on the same day and delivered to the applicant.
· The hospital has the right to withhold some medical information about the patient in the event that the information represents harm to the patient, for example
(The patient’s knowledge of the nature of the patient’s medical condition may affect his psychological state and lead to a deterioration in his condition).
· List of persons authorized to view the hospital’s medical file:
◾ The doctor responsible for the case
◾ Doctors from other departments who are consulted about the patient’s condition.
◾ The nursing staff responsible for the case
◾ The patient or his legal representative with the authorization of the patient
◾ Hospital director
◾ Medical Director
◾ Quality and performance improvement coordinator
◾ Judicial and supervisory authorities and the Ministry of Health when necessary.
◾ Medical Statistics Officer
◾ Accounts Officer
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Responsible: All hospital employees.
Forms: Declaration of confidentiality of information
|
|
|
|
|
|
|
|
Policy for protecting medical records and information from loss, damage, tampering, and unauthorized use or access
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Protecting medical records and information from loss, damage, tampering and unauthorized use
The Purpose:
Ensuring that the medical file is preserved from loss or damage and ensuring that the patient’s medical information is preserved so that it can be retrieved when needed.
Procedures:
The hospital’s medical records room meets the following specifications:
Ventilation is adequate
Lighting is adequate
Fire protection
Intact storage shelves
Offices for workers
Access to the file storage area is not permitted to anyone other than authorized persons (patient affairs employees only).
The medical records office official keeps the patient's medical records on the shelf in the order of the month for each department.
The Medical Records Office official shall repair all records with loose papers or torn covers immediately before the important information recorded in them is exposed to further loss or damage.
The official in the medical records office keeps all reports related to diagnosis, examinations, etc., such as medical reports, laboratory results, etc., in the medical file, except for radiology, which is kept in the radiology department.
There is a record of requests in the place where files are kept, which includes the borrowed files and the person borrowing the file from the people authorized to view the file.
The medical records clerks assigned to work in the filing area are responsible for maintaining the cleanliness of the area and the neat order of files on the shelves.
Administrator:
Medical records office
|
|
|
|
|
|
|
|
Policy for disposing of medical files and the duration of keeping records and files
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The purpose:
Disposing of medical files through legal means and clarifying the legal period for keeping records and files.
Politics:
· Dispose of records within the specified period in accordance with regulations and laws.
· Dispose of records completely to prevent anyone from viewing them or extracting identical copies of them.
· Records may not be disposed of except based on an administrative order issued by the hospital director general.
Procedures:
· Inactive medical records may be disposed of after a certain period of time determined by the Ministry of Health guidelines.
· Records scheduled for disposal should be registered according to the patient's name, medical file number, and last date of activity.
· The records must be completely destroyed to prevent anyone from viewing them or extracting duplicate copies of them.
· The medical records official and clerk, on the first of December of each year, review the medical records to extract what has expired and is worthy of being permanently disposed of, in accordance with the guiding policies of the Egyptian Ministry of Health website.
· The medical records officer shall keep all records related to lawsuits or other investigations of a confidential or serious nature and shall not dispose of them until after the lawsuits are completed.
· On the first of January of each year, the medical records official examines the dispensed documents and after verifying the authenticity of the dispensed documents, they are packed into bags by the department’s workers to be delivered to the Health Affairs Directorate for disposal in accordance with the ‘archives regulations’.
· The following is the schedule for maintaining medical files and records.
· Below is the schedule for maintaining medical files and records.
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Administrator:
· Medical Records Department
· the reviewer:
· Ministry of Health Medical Records Guide
· Guiding policies for the Egyptian Ministry of Health website.
|
|
|
|
|
|
|
|
- Expected Events Policy
Screening process policy to determine patients' needs for medical and nursing care
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
The hospital is committed to conducting a priority assessment of patients' needs for therapeutic and nursing services when admitting the patient to the hospital and the appropriate department for the patient's condition
The purpose :
Providing medical care to the patient appropriate to his condition and in accordance with priorities and clinical work guides (therapeutic, diagnostic, palliative) when the patient is admitted to the inpatient department of the hospital.
Working procedures:
The department's nursing staff members are responsible for conducting the initial nursing assessment of the patient's condition, using the nursing staff evaluation form.
The responsible department nursing staff performs the pain assessment according to the pain assessment form
The nursing staff responsible for the case develops a nursing care plan according to the nursing assessment and documents it in the nursing plan form.
The responsible nursing staff members in the department contact the specialist doctor and inform him of the patient’s condition
The specialist doctor reviews the medical history, completes the medical examination, and determines the patient’s needs for medical care
The specialist doctor develops a treatment plan for the patient according to the priorities and treatment protocol for the case, which includes:
Necessary tests - Required tests
Treatment is according to the treatment description form
Required follow-up and observation - Any other instructions
The responsible nursing staff implements the treatment plan in the examination and research form, specifying the timing of the request and the hour of implementation.
Administrator :
· The treating physician - members of the nursing staff in the department
Models:
|
|
|
|
|
|
|
|
|
The Reviewer :
Approved Egyptian accreditation standards.
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital is committed to informing and informing the patient and his family upon admission of the necessary information to make the appropriate decision to treat the patient
Purpose: To determine the information that is given to the patient and his family upon admission to the hospital, which helps in making the appropriate decision to treat the patient, ensures the preservation of patients’ rights, facilitates the period of stay and obtaining the required medical care, and informs patients of their responsibilities towards the hospital, which achieves the satisfaction of patients and their families.
Working procedures:
1. When the patient enters the hospital, the receptionist or admission office employee introduces the patient and his family:
· Patients’ Bill of Rights - Patients’ Duties and Responsibilities Document
· Hospital instructions regarding visits, food and/and no smoking
2. The receptionist/admission office informs the patient of the cost of accommodation and treatment and reviews the price list, in accordance with Ministerial Resolution No. 186 of 2001.
3. The treating physician acquaints the patient/his family with the necessary information that will help them make an informed decision, which includes:
· Nature of the disease and diagnosis - Suggested treatment steps
· Expected outcome of treatment - Planned date of discharge from hospital
Responsible: The attending physician - members of the nursing staff in the department
References: Approved Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy for dealing with patients in the event that there is no available place for the required medical service
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital is committed to finding an alternative solution for the patient in the event that there is no place for the required service in the hospital
Purpose: To know how to act in the event that there is no room for the required service in the hospital
Working procedures:
1. When a case is discovered for which there is no available place to provide the required medical service in the hospital, the treating physician provides
Provides first aid to the patient and writes a report on the condition
2. The hospital helps the patient and his family to find an alternative place, through the emergency department and the directorate, and provides a report to the patient’s family about the situation.
3. After confirming the approval of the hospital to which the transfer will be made, the doctor responsible for completing the transfer procedures
Providing an equipped means of transportation suitable for the patient’s condition
4. The treating physician writes the specific data in the referral form and keeps a copy of it and attaches it to the report
The patient’s condition and providing an appropriate companion for the patient
5. The treating physician provides medical instructions to the patient and those accompanying him during transportation
Administrator :
· The attending physician - Nursing staff members
Models:
Conversion form
The reviewer :
· Approved Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Coordination and cooperation policy between all departments (including doctors and nurses)
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
The hospital is committed to providing means of coordination and cooperation between all departments
The purpose:
Know how to coordinate the provision of medical care to all patients
Working procedures:
1-Coordination between doctors and nurses
Nursing staff implement doctor's orders in a timely manner
Recording the delivery and receipt for each category and implementing the required follow-up and orders
Medical consultation
2-Coordination between departments during transportation or requesting diagnostic services:
Use policies that determine the appropriateness of transferring a patient within a hospital between:
Surgical and non-surgical treatment services after medical consultation and acceptance of the case
Diagnostic services and therapeutic services S1-DS18
Emergency services and internal department.
Administrator :
The attending physician - the department’s nursing staff members
The director, his deputy or the administrative representative
Models:
Conversion form
The reviewer :
Approved Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy for terminally ill patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Purpose: To provide medical services of a special nature to a terminally ill and near-death patient that keeps him free from pain while providing psychological, social and spiritual support to the patient and his family.
Procedures:
· The treating physician signs a thorough medical examination and carefully reviews the patient’s file, including analyses, x-rays, and examinations, to determine the patient’s final condition.
· The treating physician presents the results of the clinical examinations and analyzes to the consultants in the appropriate specialties to determine the patient’s health condition and ensure the futility of any progressive treatment provided to him.
· After the consultants decide that this condition is incurable, a list of the symptoms accompanying the patient and how to treat them is written so that the patient is in a healthy state free of pain, even if this requires general anesthesia for the patient (see AP.15)
· The patient’s family is interviewed and the case is explained in detail by the consultants and the director of the unit caring for them, and moral support is provided to them conduct health education for them on how to deal with the condition
· The hospital is committed to providing and facilitating social support by consulting the citizen service office employee and providing the opportunity for the patient, if he requests, to have a clergyman attend for religious and spiritual support for the patient or his family.
Administrator :
· The treating physician and the treating consultant
· Citizen Service Office employee
The Reviewer :
· Egyptian quality standards
· Joint Commission International standards
|
|
|
|
|
|
|
|
Patient transfer, referral and discharge policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The Purpose :
Definition of what is meant and the cases in which the patient is transferred/transferred/discharged.
Establishing the foundations that ensure maintaining the patient’s security and safety and identifying those responsible for transferring, referring and discharging the patient inside and outside the hospital.
The Definition :
Patient transfer is the formal transfer of responsibility for patient care from:
One care unit to another.
One medical service to another
One specialist doctor for another
One institution to another
· Patient transfer
The person is sent from:
One doctor to another or one specialist
One department or service to another or different resources either for advice or care that is not provided by the referring entity or because it is not qualified to provide this service.
· Patient discharge
The hospital is committed to maintaining the patient’s security and safety and identifying those responsible during the process of his transfer, referral, or discharge from the hospital.
The patient is discharged to home
Working procedures:
First: Planning for transfer or transfer of the patient and discharge when developing a treatment and care plan for the patient
The treating doctor develops a medical care plan for the patient upon his admission to the hospital, completes the medical examination and the required tests, diagnoses the condition, and provides first aid to the patient.
The patient's need for transfer or referral is determined when developing a medical care plan for the patient according to his condition and to ensure continuity and continuity of medical care.
The patient's medical care plan must include the patient's planned discharge date
Second: Discuss the reason for the referral/transfer/discharge of the patient with the patient and his family
The treating physician explains the reasons for making the transfer/referral/discharge decision to the patient and his family
This is done when a decision is made, when a treatment plan begins to be developed, or when clinical and diagnostic results appear that are not available in the hospital
The doctor records the reason for transferring or transferring the patient inside or outside the hospital in the medical file
Third: Follow the correct and safe methods when transporting or referring a patient
The doctor records the required procedure within the patient’s medical file and ensures that all file data is completed, mentioning the reason for referral/transfer/or the patient’s condition upon discharge.
In the case of referral, the referral form is completed explaining the patient’s condition/reason for referral/required procedure
In the case of consultation, the consultation form is completed in accordance with the Medical Consultation Policy PA 6
The method of transporting/referring the patient is determined according to his health condition
When transporting/transferring a patient using a wheelchair or bed, the following measures must be taken:
Check the bed/chair and ensure its safety
Make sure the sides of the bed are in place
The department supervisor contacts the referral/transfer location to ensure the availability of the required service for the patient, and the time and result of the call are documented in the nursing status book in the case of internal referral/transfer.
The responsible nursing staff notifies the admission office and hospital accounts to take the necessary measures for the transfer/transfer/discharge process
Nursing staff members review the patient's complete data and ensure that the recorded data is correct.
Fourth: Transferring a patient to another facility, cases of referring a patient to another facility:
In the event that the service is not available in the hospital.
Patient's request for transfer to another facility
The specialist doctor provides first aid to stabilize the patient's condition, if necessary.
The specialist doctor determines the patient's condition.
The specialist doctor notifies the patient or his companions that the necessary service is not available for the patient in the hospital.
The treating physician ensures that there is a suitable place for the patient’s condition before transferring him by contacting the place receiving the patient and explaining the patient’s condition.
The treating physician notifies an ambulance to transport the patient, accompanied by the ambulance doctor and ambulance nurse, or transport the patient according to his desire after writing an acknowledgment from him or his family.
The treating physician completes the patient referral form
The nursing staff and the ancillary services worker transport the patient in a safe manner as mentioned previously.
The nursing staff ensures that a copy of the patient’s examination, procedures performed, research results, diagnoses, and treatment are sent with him to the place he is transferred to.
Fifth: Discharge of a patient:
When the patient's medical condition improves and stabilizes, the consultant/specialist determines the patient's discharge date, the treatment plan at home, the type of nutrition, and the follow-up date in the outpatient clinic.
The doctor completes the discharge form for the patient and completes all data in clear writing, and the patient is given the original discharge form and keeps a copy in the file.
The specialist doctor explains the instructions that will be implemented during the recovery period to the patient and his family, including how to take medications, how to deal with the medical condition, ways to obtain rehabilitative services, methods of proper therapeutic nutrition, and follow-up appointments in the outpatient clinic.
The nursing staff gives the patient his discharge form
The department supervisor ensures that the financial settlement is completed.
The nursing staff removes the cannulae from the patient's hand, if any, before leaving the department.
The nursing staff reviews the patient's discharge plan to determine his method of discharge
The assistive services worker transports the patient from the department using a wheelchair or a trolley according to the patient’s need until the patient is discharged.
Responsible for implementation:
the doctor
Nursing staff members in the department
Service worker
Models:
Checkout form
Conversion form
The Reviewer :
· Approved Egyptian accreditation standards
· Regulations and laws
|
|
|
|
|
|
|
|
Hospital medical emergency response policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The Purpose:
Preparing departments to deal with emergency situations that require emergency dealing, and developing a system to respond to emergency calls.
procedures:
The nursing supervisor of each department prepares an emergency vehicle with life-saving medications and tools according to the attached list that specifies the components and arrangement of the emergency vehicle, provided that the vehicle is close and available for use 24 hours a day.
The supervisor of each department reviews these carts daily
The hospital's pharmacists' department assigns a pharmacist to visit the emergency vehicle and verify its contents and suitability on a daily basis.
The medications used from the emergency vehicle are replaced immediately after they are used from the emergency cabinet of the department that used them. If these medications are not available in the emergency cabinet of any department, they are replaced from the intensive care emergency cabinet until they are dispensed from the hospital pharmacy.
The hospital (training officer) is committed to providing training sessions on cardiorespiratory resuscitation for all employees (doctors and nurses) in the hospital on a one-day basis every two years. Those who have obtained the training certificate are given a certificate stating this, and their direct supervisor is responsible for monitoring the workers’ obtaining the training courses.
Any hospital employee who suspects a case of cardiac arrest calls the cardiorespiratory resuscitation team by telephone to the intensive care unit and members of the nursing staff in the department or by using the switch to make a call and mention the department/department and the number of the room to which you want to move.
The department's nursing staff calls the rest of the team if the switch is not available.
In cases of cardiac arrest that occur in intensive care, the care physician is called and the cardiorespiratory resuscitation team is not requested unless the care physician requests it, and his responsibility is to supervise the patient’s resuscitation.
In cases of cardiac arrest that occur in operating rooms and units where the patient is supervised by an anesthesiologist, the cardiorespiratory resuscitation team is not called unless the anesthesiologist requests it, and he is responsible for supervising the patient’s resuscitation.
The first person to reach the patient performs cardiac resuscitation.
The case doctor is responsible for explaining the medical condition, reviewing the patient’s files, and informing the team leader of any information he needs. He also participates in performing cardiac resuscitation. He is responsible for communicating with the patient’s family, informing them of developments in the patient’s condition, and involving them in any medical decision that requires their participation.
Intensive care nursing staff members are responsible for giving medications and taking samples requested by the team leader and assisting the rest of the team members according to the team leader’s instructions.
The department's nursing staff members are responsible for recording the events of cardiac arrest, the dates for administering medications, the shape of the heartbeat, and the time the heart returns to beating on the form designated for that purpose. They are also responsible for giving breathing to the patient in the manner determined by the team leader.
The security personnel provides the appropriate atmosphere for the team's work and is present when informing the patient's family of any developments in his condition.
Work must be done to provide care facilities on an ongoing basis to receive post-cardiac arrest cases that may occur in hospital floors, after first aid has been provided in the internal department and his condition has been stabilized.
The medical team in the care is trained to respond quickly and immediately when called upon, and all members of the medical team must be present in the room where the emergency is and deal with the case in accordance with the cardiorespiratory resuscitation policy.
The call system is tested unexpectedly by the unit manager/hospital quality coordinator to ensure that doctors and nurses respond to the call, and the time between call and response is calculated as a form of performance evaluation within the unit, with the results reported to the hospital quality coordinator.
Cardiopulmonary resuscitation is performed according to the attached protocol.
All hospital employees are trained to deal with cardiac arrest cases (basic level), while care and anesthesia doctors are trained at the advanced level.
Administrator:
· All hospital employees
· CPR team
Models:
· Table of contents and arrangement of the emergency vehicle
· Monthly CPR team schedule
· Cardiorespiratory resuscitation protocol
The Reviewer:
· Egyptian quality standards.
· Cardiorespiratory resuscitation protocol
|
|
|
|
|
|
|
|
Health education policy for patients and their families
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Providing health education to patients visiting the hospital and their families ensures that patients are provided with important information that will help them recover and protect them from diseases when they enter the hospital, during their stay in the hospital, and after discharge. This is evident in the hospital’s commitment to educating the patient and his or her family related to the following:
Pathological diagnosis of the patient
Tests, diagnostic examinations and treatment
Use of medications and possible side effects
nutrition
Interactions between food and medicine
Physical therapy and rehabilitation
Special information on how to reduce the risk of diseases through nutrition
The harms of smoking and the need to avoid active and passive smoking
Exercise and health-related behaviors
The relationship between the patient and society
Exit and follow-up instructions
The Purpose:
Improving health care outcomes by educating the patient and his family to assist in recovery and raising the value of healthy behavior by providing health information about the various medical specialties necessary for the patient.
Procedures:
· According to Professional Ethics Regulation No. 238 of 2003, health education for patients and their families is considered one of the duties and responsibilities of the doctor and the medical team.
· The treating physician and the responsible nursing staff use a special record/form to educate patients and their families.
· The treating physician and the nursing staff responsible for the patient’s medical service evaluate the patient’s educational level and determine the educational needs upon admission of the patient.
· Any department participating in the educational seminars records its own seminar with its signature and date in the patient educational record
· If abbreviations are used, an explanation is provided for each abbreviation to clarify the information.
· The treating physician and the responsible nursing staff ensure that the patients’ educational record contains the type of information provided to the patient, to whom the information was provided, the extent of the response of the patient or his family, and a summary of the educational session that was conducted for the patient.
· The treating physician and the responsible nursing staff ensure that the forms for the departments participating in the educational seminars are placed in the patients’ educational record.
· The treating physician and responsible nursing staff ensure that the patient’s questions are given the opportunity.
· The treating physician and the responsible nursing staff ensure that the patient understands the discharge instructions and follow-up steps, and this is recorded in the patient’s file.
· The hospital provides a special place for patients in the internal departments and outpatient clinics to receive educational seminars.
· The hospital is committed to developing a unified educational material for chronic diseases/dialysis patients.
Administrator:
· Physician
· Members of the department’s nursing staff
· Medical provider from any department involved in patient education
Models:
· Patient and family education model
The Reviewer :
· Regulations of professional ethics
· Egyptian quality standards.
Preparation Review The Trust
- Policies for unexpected events
Incident reporting policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
A policy that explains the system for reporting near misses/incidents that enable employees to report them in order to help in continuous improvement of performance.
Purpose:
To provide an organized mechanism in the hospital to identify problems that lead to negative outcomes for patients, visitors, or employees in order to detect them early and prevent them from occurring.
Definitions:
· Near miss: An unplanned event with the potential to cause harm that was intercepted in time or by chance resulting in no harm to the person.
· Incident/accident: Any incident that occurs in the hospital (that does not represent routine patient care) that negatively affects or has the potential to affect the health or lives of patients, visitors, or hospital workers.
procedures
General procedures:
· The report must be written and completed by the person who discovered the accident or the person involved in this accident.
· The report must be written immediately after discovering the incident and submitted to the Quality Coordinator no later than 48 hours.
· The quality coordinator presents the report to the head of the relevant department and the hospital director to take corrective measures.
· Confidentiality must be observed in dealing with or maintaining these reports, while limiting access to them to persons with authority to do so.
· Do not use the information in this report as a means of taking disciplinary action against anyone.
· These reports should generally be discussed at Quality Committee and Medical Board meetings for educational purposes or to establish regulations limiting their occurrence.
· Items that make up the report
· Information about the infected person and the department he is in.
· The type of incident/unexpected event that has significance.
· Information about the near miss/accident/unexpected event that has significance.
· Description of the incident, indicating any action taken immediately after the discovery and the factors that led to this incident.
· Corrective actions taken.
· Data of the person who discovered the incident/unexpected event that has significance. Filling out this part is not mandatory.
· The department head verified the report.
· Instructions from the hospital director.
People responsible for writing the report
· All hospital employees, including doctors, nurses, pharmacists, chemists, radiology technicians, and non-medical service personnel.
· Corrective action plan and assigned responsibilities in the event of unforeseen accidents:
· After the report reaches the hospital’s quality coordinator (within 48 hours of the incident), he reviews it and returns to the head of the department in which the incident occurred and the person or persons who discovered the incident to find out the reasons that led to the incident. This is done within 48 hours of the report reaching the quality coordinator.
· The quality coordinator (or his designee from the quality team) classifies this incident as (specific to environmental safety - specific to medications - specific to patient safety and security)
· The Quality Coordinator (or his designee from the Quality Team) refers to (the Environmental Safety Officer - the Pharmacy Manager - the Patient Safety and Security Officer) according to the classification of the incident to make recommendations with the Quality Coordinator (or his designee from the Quality Team) to prevent this incident from recurring again. Other.
· After setting the necessary recommendations to avoid the occurrence of this incident, a corrective plan will be developed to implement these recommendations by the quality coordinator, the responsible person according to the classification of the incident, and the head of the department in which the incident occurred.
· The corrective plan includes recommendations, who is responsible for implementing each recommendation, the time frame for implementation, and the resources required.
· The quality coordinator (or his designated member of the quality team) follows up on the implementation of the established corrective plan and submits a report on it for discussion at the quality committee meeting.
Responsibilities
· The employee who discovered the accident
· Rapid intervention to protect or support the patient’s health condition.
· Immediately inform the existing doctor
· Writing the report before the end of the shift.
· The doctor who was informed of the accident
· Recording the result of the medical examination and the required medical care.
Hospital manager
· Review the condition and ensure that corrective actions have been implemented and provide any assistance required.
Quality coordinator
· Monitor all reports and ensure that all important steps to resolve the issue have been completed.
· Writing a monthly summary of all reports.
· Writing a quarterly report to the Quality Committee for discussion.
· Maintain a file of all reports for three years.
Occupational safety and health officer
· Examine all occupational safety and health reports to review safety-related incidents.
· Form a team from the Occupational Safety and Health Committee to review safety-related incidents.
· Recording the inspection results and corrective actions taken in the report.
· Return the completed report to the Quality Coordinator.
· Writing a monthly summary and presenting it to the Occupational Safety and Health Committee.
Responsible for implementation:
· The employee who discovered the accident
· The physician who has been notified
· Head of Department
· hospital manager
· Quality Coordinator
· Occupational safety and health officer
The Reviewer
· Egyptian accreditation standards.
· Regulating laws and regulations
Models
· Incident report form
Attachments
· Accidents and near misses that must be reported to the hospital.
|
Preparation |
Review |
The trust |
|
|
|
|
A list of facts that can be reported
|
ا |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Patient escapes
The patient's suicide, suicide attempt, and violence.
Unexpected mortality and complications including those resulting from institution-acquired infections.
Confirmed blood transfusion reactions (except for routine adverse reactions such as chills and fever).
Significant events in anesthesia and analgesia that caused harm to the patient.
Significant differences between preoperative diagnosis and postoperative diagnosis including surgical pathology findings.
Significant adverse drug reactions that cause patient harm.
Significant medication errors that caused harm to the patient, such as:
Giving the wrong medication.
Giving the wrong dose.
Giving medication incorrectly.
Giving medication to a wrong patient.
Related to operations:
Cancel the operation
Unexpected removal of any organ
Wrong patient
Incorrect counting of tools
Cases of error in the operation (patient - operating party - procedure)
Leaving a foreign body in the patient.
· Related to the laboratory:
Incorrect sample data
His eye is wrong
Improper storage
Incorrect laboratory results
Related to the hospital:
Visitor injured
Bed sores
Incorrect needle injury
· Security neutrality:
Theft or loss of personal property
Fight with a visitor or patient
Failure to follow hospital policies
attempt to suicide
· Fire and safety:
a fire
Chemical spill
One of the emergency exits is blocked
Expired fire extinguisher
Gas leak
Water leak
Unsafe electrical wires
Serious physical or psychological harm to a patient, employee, or visitor (nerve damage - loss of a limb or organ - death)
|
Preparation |
Review |
The trust |
|
|
|
|
Significant Error/Accident/Unexpected Event Report Form
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Intensive analysis policy when unexpected events occur
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The existence of standards and processes for intensive analysis of significant and undesirable unexpected events.
Purpose: To increase public knowledge about events, their causes, and strategies to prevent them, and focus the hospital's attention on understanding the reasons behind this event and changing hospital systems and processes in order to reduce the possibility of such an event occurring in the future.
Definitions:
· A significant unanticipated event is any unexpected event in health care that results in death or serious physical or psychological injury to a patient.
Procedures:
· A report on the occurrence of the event is written as per policy.
· The quality coordinator selects a team consisting of people close to this event and a member of the hospital’s quality team to analyze the reasons and determine the basic factors behind the occurrence of this event, provided that this is done within a month of forming the team.
· The analysis identifies changes that could be made in systems and processes (either through redesign or development of new systems or processes) that would reduce the risk of such events in the future.
· The analysis must be accurate, documented, and comprehensive, including the following:
· Identify the human factors and other things that are directly related to the event and the processes and systems relevant to its occurrence.
· Analyze basic systems and processes through a series of questions.
· Identify risks and their potential contributions to this type of event.
· Identify potential improvement in processes or systems that would lead to a reduction in the likelihood of such events occurring in the future.
· After identifying the root causes, the team will develop a corrective plan to avoid these causes in the future, provided that the time frame for implementing this plan does not exceed three months.
· time frame :
· The root causes must be analyzed and a corrective plan must be developed within a month of the event occurring.
· The corrective plan must be implemented within a period not exceeding three months.
· The root cause analysis and corrective plan implementation are reviewed by the hospital’s Quality Committee.
Responsible for implementation:
· Quality Committee
· work team
· People responsible for implementing the plan
The Reviewer:
· Egyptian accreditation standards.
· Regulating laws and regulations.
Models:
· Incident report form
|
Preparation |
Review |
The trust |
|
|
|
|
- Patient Rights Policy
Patient rights policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The hospital provides multiple medical services, and the hospital administration, doctors, and staff are committed to performance that preserves patients’ rights, while informing them of them from the time they enter and while performing the various services until they leave, in compliance with the hospital’s mission and fulfilling the patient’s health care needs.
The Purpose:
Preserving the rights of patients and their families.
Working procedures:
The hospital is committed to all regulations and laws issued by the Ministry of Health and the Federation of Medical Professions Syndicates with regard to the rights of patients and their families, as stated in the Professional Ethics Regulations issued by Minister of Health Resolution No. 238 of 2003, as well as Ministerial Resolution No. 186 of 2001. Accordingly, the hospital
It takes the following policies:
- The right to receive care if it is available in the hospital.
- The right to know the name of the treating physician, supervising physician and/or responsible physician
- The right to receive care that respects the patient’s values and personal beliefs.
- The right to know about and participate in making decisions regarding their care.
- The right to refuse treatment or not continue it: The doctor must do the following:
- The right to security, personal privacy, confidentiality and dignity. The patient has the right to have the following.
- The right to receive appropriate treatment for pain
- The right to file a complaint or suggestion without fear of persecution
- The right to know the prices of services and procedures.
The presence of a professional ethics regulation, Resolution No. 238 of 2003, in the hospital administration and with the quality coordinator as a reference in training on patients’ rights. The regulation includes the following points:
Chapter One: Doctors’ Section
Chapter Two: The doctor’s duties towards
the society
Occupation
The patients
Colleagues
· Part Three: Medical interventions of a special nature
Gender correction procedure
Assisted fertilization operations
Removal and transfer of human organs and tissues
· Chapter Four: Conducting medical experiments and research on human beings
A- A copy of Resolution No. 186 of 2001 from the hospital’s emergency director, which includes the following:
Informing the patient about the cost of surgical operations at all stages
It is prohibited to detain an inmate's body or exploit a death to gain material benefits
A copy of Prime Minister’s Decision No. 1063 of 2014 at the hospital’s emergency director, which includes the following:
All medical facilities are committed to providing treatment services for emergency and accident cases free of charge for 48 hours, after which the patient has the choice of staying at his own expense or being treated in the hospital’s free department, provided that the state bears the costs from the treatment budget at the state’s expense.
The right to receive care if it is available in the hospital:
This is to ensure the hospital’s ability to provide the necessary medical care to the patient. This depends on obtaining information about the patient’s needs and condition through a screening and selection process by the medical team, which is carried out by:
Evaluate the patient's medical history
Physical examination
Previous evaluations and examinations with the patient...etc
The medical team provides medical care to the patient after obtaining the results of the medical examination and necessary tests as long as the service the patient needs is available and a bed is available for this patient in the hospital.
This is usually done at the first point of contact:
When the patient arrives at the hospital
During ambulance transport
Before transferring from another location
The right to know the name of the treating physician, supervising physician and/or responsible physician:
This is done by the doctor introducing himself to the patient before dealing with him
An identification card placed by the doctor containing the name, specialty, personal photo, and hospital name
Doctors wear a white coat, blue or green suit.
Place the names of doctors and their specialties on the door of each clinic
The right to receive care that respects the patient’s personal values and beliefs:
Hospital staff must respect the patient's personal religious and cultural beliefs and the freedom to exercise them
Hospital workers must not prevent the patient's family from seeking help from a clergyman in cases that require spiritual support, such as patients on the verge of death
Hospital staff must respect Coptic patients’ wishes to specify the type of food on fasting days as long as this food does not conflict with the patient’s care plan.
Hospital workers must ensure that the patient receives the highest possible level of health care without discrimination based on age, sex, religion, race, nationality, origin, opinion, social or economic status, disability, special needs, or any other type.
The right to know about the decisions related to their care and to participate in making them, and this is done through the following:
Obtaining the patient’s consent (by the doctor) by signing a declaration of consent before the following procedures: surgery and surgical interventions.
Sedation: moderate or deep
Use of blood
Gastrointestinal endoscopy
A- He also has the right to know the treatment plan and participate in choosing it through the following:
The treating physician explains the patient's medical condition, the various proposals for treatment, and the various medical examinations required.
The doctor must also participate with the patient/his family when developing the treatment plan.
The right to refuse treatment or not continue it:
The doctor must do the following:
Explaining the health consequences to the patient/his family of refusing treatment.
Clarifying that the patient or whoever has the legal right to do so bears full responsibility in the event of insistence on refusal.
Informing patients about available care and treatment alternatives/discharge on demand despite doctors' advice
The physician supervising the treatment records the refusal of treatment
The right to security, personal privacy, confidentiality and dignity.
The patient has the right to have the following:
Security :
Security personnel and the medical team are responsible for protecting patients from harm, theft, destruction, tampering, or entering an unauthorized place or using something. This is done according to the security plan within the environmental safety plans
Privacy: The hospital administration is responsible for providing curtains, barriers, or sheets that ensure the patient’s privacy during:
Medical Examination
Conducting examinations
Care and treatment
Transport
Confidentiality:
Members of the hospital's medical team sign a declaration to maintain the confidentiality of patient data and information.
The medical team is responsible for not posting confidential information on the patient's door or at the nursing station.
The medical team is responsible for not discussing the patient's condition in public places.
The medical team asks patients to give permission in order to release information that is not covered by laws and regulations.
The right to view the patient's file.
While the file is in the internal departments of the hospital:
The doctor (therapist, radiologist, laboratory doctor), the head of the department, the nursing staff, and the pharmacist have the right to view the patient’s file.
After saving the file, the file can be viewed by:
Workers in the Medical Registration Department to complete entry and exit data.
Judicial bodies or the prosecution in the event of an attempt to obtain some information about the patient.
The patient or his first-degree relatives (after submitting an official request and approval by the hospital administration, provided that the request explains the reason for the patient or his relatives requesting to view the file).
Those conducting scientific studies (whether from inside or outside the hospital), and this also happens after submitting an official request and approving it from the hospital administration (according to the type of study and its compatibility with the cases in the hospital), provided that no personal data related to the patient is accessed ( such as name and address).
A- Dignity:
The medical team must treat the patient in an appropriate, ethical manner that preserves his dignity and prevents the loss of any of his moral rights (without insult, humiliation, or deprivation).
2. The right to receive appropriate treatment for pain: (see AP.15)
The patient has the right to receive appropriate treatment for pain at the appropriate time according to his condition, as the nursing staff evaluates the severity of the pain and informs the doctor of it to review the evaluation and prescribe the appropriate treatment for the patient. This is done through a special form that contains details about the patient, his medical condition, the degree of pain, Appropriate treatment and its dosage (pain assessment and treatment model)
3. The right to submit a complaint or suggestion without fear of persecution
The patient has the right to submit a complaint regarding any deficiencies he sees, as well as his suggestions for improving the service, provided that it is clarified how patients and their families can submit a complaint or suggestion in accordance with the provisions of the complaints policy established by the hospital.
- The right to know the prices of services and procedures:
The patient has the right to know the prices and prices of the various services provided by the hospital in the various departments. This is done by the administration announcing the prices of some services via signs in public places in the hospital, such as the reception, provided that a person responsible for inquiries clarifies.
The admission office clerk informs patients or their families of the estimated cost of the required health care and the patient signs a general declaration of admission that includes the patient’s knowledge of the cost of the service after being shown the price list.
Second:
Informing patients and their families of their rights through the following:
The hospital administration posts the terms of patient rights and duties on boards in patient waiting areas and departments.
The entry or reception employee takes the patient's signature on a patient rights and responsibilities form after informing him of them.
The department supervisor makes sure that the patient understands these rights, and in the event that the patient does not fully understand them for any reason (ignorance of reading, forgetfulness, lack of ability to comprehend or understand,...) the supervisor re-clarifies these rights.
A list of patients' rights is posted on the door/wall of all patient rooms.
The person responsible for the Citizen Service Office collects data on patient complaints daily, delivers it to the person responsible for the solution, and analyzes it monthly to identify weak points for taking corrective measures.
Administrator:
4. - All hospital employees. – Members of the nursing staff of the department or unit.
5. - Entry desk employee. – Citizen Service Officer
Models:
6. Patients’ Bill of Rights.
7. Unified emergency form.
8. Approval declarations form.
9. Pain assessment form.
10. Price lists for hospital services.
The Reviewer:
11. Professional Ethics Regulations 238 of 2003.
12. Ministerial Resolution 186 of 2001.
13. Egyptian accreditation standards.
14. Prime Minister’s Decision 1063 of 2014.
|
|
|
|
|
|
|
|
Patient responsibilities policy towards the hospital
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The hospital is committed to informing patients of their responsibilities and following up on the implementation of these responsibilities. In the event of a violation, the necessary measures will be taken in accordance with the hospital system.
The Purpose:
Informing the patient of his responsibilities while in the hospital.
Working procedures:
1- The patient’s duties include, at a minimum, the following:
A - Follow hospital policies and regulations, which include:
Maintaining hospital property.
Do not keep any personal belongings.
Commitment to the specified visit times.
It is forbidden to bring any food from outside the hospital, as the hospital provides appropriate food for each patient.
Maintain calm and follow order while visiting patients.
Commitment to the non-smoking policy.
The possibility of having a companion for the patient if the patient is a child under 6 years old, provided that the hospital takes a copy of the companion’s ID card.
The companion shall be paid, except in some special cases in which free companionship is permitted after obtaining the approval of the hospital director.
Financial commitment in accordance with the law, regulations and hospital policy.
B - Providing information:
The patient is obligated to provide correct, accurate and complete information about his current illness, treatment methods and frequency of treatment in any hospital.
The patient is obligated to submit the legal documents required of him.
C - Show respect for other patients and health care workers, help not make noise, and adhere to visiting instructions.
D - Financial commitment in accordance with the law, regulations and hospital policy.
E - Follow the proposed treatment plan.
- The patient is obligated to follow his own treatment plan, which was developed for him by the doctors. In the event of non-compliance, the responsible nursing staff members inform the doctor responsible for the treatment, writing this down immediately.
2- The patient is informed of his responsibilities through the following means:
- The patient signs a general declaration upon admission by the admission office employee or the receptionist, stating his commitment to hospital policy, respect for others, financial obligations, and his commitment to the treatment plan.
- The responsible nursing staff members in the internal departments read the patient’s responsibilities to him and inform him of them, with him knowingly signing them in the event that he is unable to realize or sign his duties during his admission.
- A list of patient responsibilities is posted on the door/wall of all patient rooms.
Administrator:
receptionist.
Responsible nursing staff members.
Citizen Service Office employee.
Models:
Patient duties document.
The Reviewer:
Professional Ethics Regulations No. 238 of 2003.
|
|
|
|
|
|
|
|
The policy of refusing or not continuing treatment for the patient
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The hospital is committed to guaranteeing the right of the patient, his family, or his legal representative to refuse or continue treatment, after ensuring that he or his legal representative is informed of the consequences related to refusing or not continuing treatment, and the responsibilities related to that.
The Purpose:
Respecting the patient’s right to refuse treatment or not continuing treatment, informing him of the consequences resulting from that, and holding the patient fully responsible if he insists on refusal.
Action Steps:
1- The specialist doctor informs the patient about his medical condition in a clear and appropriate way and informs him of the types of treatment used for him, whether medication or surgery.
2- The refusal of the patient or anyone who has the legal right to do so to receive treatment or to continue treatment is proven through the following:
· The nursing staff supervising the treatment for the patient records the refusal in the patient’s file.
· The nursing staff supervising the implementation of treatment for the patient informs the doctor of the patient’s refusal or continuation of treatment.
· The doctor supervising the treatment explains the impact of refusing or not continuing treatment and the resulting health consequences to the patient or to those who have the legal right to do so.
· The doctor will change or continue treatment, if possible.
· The doctor supervising the treatment makes it clear that the patient or whoever has the legal right to do so bears full responsibility in the event of insistence on refusal.
· The doctor supervising the treatment records the refusal or continuation of treatment in the patient’s file in the event that the patient or whoever has the right to do so continues to refuse, along with recording a summary of the patient’s conversation.
· The doctor records the patient’s refusal of treatment with documentation from him and the nursing staff present.
· The doctor supervising the treatment ensures that the following steps are taken:-
- Accommodating the patient or whoever has the right to do so to describe the patient’s general condition.
- The patient, or whoever has the right to do so, understands the expected outcome of the refusal and its consequences.
- The patient, or whoever has the right to do so, understands the seriousness of refusing treatment.
- Accommodating the patient or whoever has the right to bear full responsibility when refusing treatment.
- Writing a statement that the patient refuses treatment despite the advice of the doctor (the name of the treating doctor), and the patient signs this refusal.
- The patient’s signature on the refusal of treatment is in the file. If the patient refuses to sign, the treating physician and the responsible nursing staff members sign this refusal as witnesses.
3- The nursing staff responsible for implementing the treatment will record that the patient refused treatment and left the place before the doctor arrived in case the patient left without permission.
4- The specialist doctor confirms the patient’s desire to leave the hospital despite the advice of the team treating him in the patient’s file and proves that the risks of this procedure have been explained to the patient or whoever has the legal right to do so.
5- The patient, or whoever has the legal right to do so, signs his desire to leave, against the advice of the treating medical team, and records the date and time.
6- The patient, or whoever has the legal right to do so, undertakes to be seen by a specialist doctor outside the hospital as soon as possible.
7- The Citizen Service Office employee fills out the patient’s opinion form about the medical service and clarifies any complaints to them.
8- In the event that the patient leaves the hospital and refuses treatment despite advice, the nursing staff will report the patient’s escape from the hospital.
Administrator:
◾ The treating physician.
◾ Responsible department nursing staff members.
◾ Citizen Service Office employee.
Models:
◾ Customized exit declaration form.
◾ Patient opinion questionnaire form.
The Reviewer:
◾ Egyptian accreditation standards.
|
|
|
|
|
|
|
|
- Patient complaints and suggestions policy
Patient complaints and suggestions policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The hospital is committed to establishing a system or procedure to ensure that patients know how to submit their complaints and suggestions, to work on examining and eliminating the causes of complaints, and to study the suggestions submitted by patients and their families.
The Purpose:
Clarifying how patients and their families can submit a complaint or suggestion, ensuring that the complaint is examined, its causes removed, and the proposals submitted to continue the hospital’s performance improvement process.
Methods for submitting complaints and suggestions:-
- First: Complaints received from outside the hospital.
- Second: Complaints issued from within the hospital.
Procedures:
First: Complaints received from outside the hospital.
1. The secretarial employee receives complaints received by the hospital from abroad by phone and reports them to the Citizens Service Office.
2. The secretarial employee directs the complainant to the Citizens Service Office.
3. The Chairman of the Complaints Committee reviews the complaint and identifies the department or persons responsible to verify and respond to it.
4. The person responsible (Citizens Service) for verifying the complaint writes an appropriate response to present to the Chairman of the Complaints Committee.
5. The Chairman of the Complaints Committee determines the necessary action to be taken regarding the complaint.
6. The Chairman of the Complaints Committee determines who will send the response to the party concerned with the complaint or contact the complainant by telephone/telegraph to set an appointment to meet him and inform him of what has been taken regarding the complaint.
Second: Complaints issued from within the hospital.
1 - Complaints submitted through complaint boxes:
The hospital administration sets up boxes to collect complaints from customers by distributing them in different areas of the hospital (administration building - reception).
· The Complaints Committee opens complaint boxes, classifies them, and delivers them to the Chairman of the Committee.
· The Chairman of the Complaints Committee examines the complaint and writes a summary of it in the event that the name of its submitter is not mentioned to present it to the director to discuss what was reported in it. In the event that the name of its submitter is mentioned, the Chairman of the Committee assigns someone to respond to what was stated in the complaint.
The results of complaints are submitted to the manager on a weekly basis.
· The hospital director takes the necessary action according to the result received.
2- Complaints submitted by telephone:
· The patient or his representative calls the extension number announced at the hospital.
· The Director’s Secretariat will listen to the complaint and record it in the relevant register, provided that at the end of the working day it informs the Chairman of the Complaints Committee of all complaints in the register.
· Complaints are received by telephone during morning working hours (8:00 a.m. to 2:00 p.m.)
3- Receiving patients’ complaints during personal interviews with them:
First: The patient or his representative submits a complaint:
The patient or his representative submits his complaint to the citizen service official.
· Second: Citizen Service Office employee passing through the internal departments:-
v Complaints Committee to discuss the problems and what has been done regarding them.
Third: Passing by the Patient Rights Coordinator:
v The citizen service office employee visits patients, listens to their complaints, records them in the special form, and works to resolve them by contacting the official. In the event of inability to do so, he submits them to the head of the complaints committee.
· The Citizen Service Office employee presents the complaint form daily to the supervisor
1. The Patient Rights Coordinator visits a random sample of patients to hear their complaints and suggestions, ensures that the Citizen Service Office employee visits them, and records those complaints, if any, in his visit record.
2. The citizen service official examines the complaints he finds.
3. The Citizen Service Officer fills out the patient satisfaction form in the section relevant to the complaint if the complaint or proposal needs follow-up.
Actions taken with complaints
· The Chairman of the Complaints Committee addresses the departments relevant to the complaint or proposal, either orally or in writing.
· The department concerned with the problem or proposal is committed to researching it and responding to it within a specific period of time determined by the committee chairman.
· Upon the expiration of the specified period of time, if an appropriate decision has not been taken in the relevant department, the matter shall be presented to the director for a decision to be made with the hospital administration.
· The hospital director’s recommendations for a solution are followed up by the citizen service official and the complainant is informed of the outcome.
· The confidentiality of the person reporting the complaint is maintained without attacking him or attempting to harm him.
Administrator:
- Director’s secretarial officer.
- Complaints Committee.
- Citizen Service Officer
Models:
- Patient Complaints Passing Form
- Inpatient complaint form.
- Patient opinion survey form.
Documentation:
- Complaints register.
The Reviewer:
Egyptian accreditation standards from 2013.
|
|
|
|
|
|
|
|
Policy for obtaining informed written consent
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The hospital follows a policy of obtaining patient consent in accordance with regulations and laws.
The Purpose:
Preserving the patient’s rights and obtaining the patient’s consent before providing health services to him in accordance with regulations and laws.
A - The patient’s attendance at the hospital is considered implicit consent to conduct medical examination and treatment in accordance with the text of Article No. 28 of the Regulations on Ethics and Honor of the Human Medicine Profession issued by Minister of Health and Population Resolution No. 238 of 2003.
B - The patient or whoever has the legal right to sign must sign the general declaration of consent to enter the hospital and receive treatment when the patient enters the hospital (general declaration form for hospital admission).
C - Physicians and hospital nursing staff must obtain informed written consent from the patient or his legal representative in all of the following cases (except for life-saving reasons):
- Surgical intervention.
- Hemodialysis.
- General anesthesia, sedation, or deep sleep.
- Transfusion of blood and blood products.
- Surgical and diagnostic endoscopy
Action Steps:
1. The acknowledgment of approval for the therapeutic procedure is deposited in the relevant section of the patient’s file after the signature of the patient or whoever has the legal right to do so.
2. The treating physician explains the reasons, advantages and risks of the procedure to be performed, along with explaining the consequences and alternatives resulting from it to the patient or whoever has the legal right to do so.
3. Doctors are obligated not to carry out this procedure before confirming the existence of the declaration signed by the patient or who has the legal right to do so.
4. The doctor must commit to explaining the procedure and its details, mentioning (the reasons - advantages - risks) to the patient or his family.
5. The patient, or whoever has the legal right to do so, signs the aforementioned declaration and records the date and time of signing.
6. The surgeon and anesthesiologist sign their commitment to the procedure mentioned in the declaration.
7. Determine the validity period for the approval of the therapeutic procedure to be thirty days from the date of the patient’s signature or whoever has the right to do so legally. If the patient’s condition requires emergency circumstances or based on the instructions of the treating physician based on the patient’s condition follow-up forms, the implementation of another procedure in addition to the first procedure or To change the type of procedure, a new approval must be obtained from the patient or whoever has the legal right to do so.
8. The declaration required to be signed by the patient must contain:-
- Patient name
- Name of the process/procedure.
- Type of planned anesthesia.
- Name/signature of the anesthesiologist.
- Name/signature of the surgeon.
- The date of the declaration must be prior to the date of the transaction.
- Signature of the patient/guardian/guardian
9. In the event that the patient is unable or qualified to sign the declaration (a minor, incapacitated person, or unconscious person), the following order shall be followed, with documents proving this to be submitted:
- The guardian, guardian, or guardian by law (provided that he submits proof of this).
- Husband/wife.
- One of the parents.
- One of the adult children.
- A grandparent or adult grandchild.
- An adult third-degree relative, provided that the degree of kinship is proven
10. In the event that the patient is unable to read and write or is unable to understand the information explained by the doctor, the patient’s fingerprint or stamp must be taken on the declaration, provided that one of the relatives indicated in the previous clause signs as a witness to the consent declaration and proves this before the doctor.
Due to the nature of the hospital’s work and the frequency of dealing with serious and critical cases, the approval must include permission for the transfusion of blood and its derivatives.
11. In cases of loss of consciousness and critical cases that affect the patient’s life, the medical team can perform some surgical interventions to save the patient’s life before obtaining the patient’s consent or it is not possible to obtain consent from his family, provided that the hospital director or his representative forms a committee of the treating physician, another physician, and a physician. anesthesia by signing that the procedure to be performed is life-saving and the reasons for its speedy procedure before obtaining the declaration referred to in the previous clause.
Administrator:
- Physician.
- Responsible department nursing staff members.
- The hospital director or his representative (department head - shift consultant - hospital alternate director - administrative deputy - head of the medical staff)
Models:
- Consent acknowledgment form
The Reviewer:
- Professional Ethics Regulations No. 238 of 2003.
- Ministerial recommendations to maintain patient safety during anesthesia.
- Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
The policy of informing the patient of the outcome and expected costs
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
- The medical service provider’s commitment to informing patients and their families of the results of the treatment and medical care provided to them and the expected costs.
The Purpose:
- Creating a system to inform patients and their families of the outcome of the medical care or treatment provided to them and the expected costs.
Procedures:
1. Doctors and medical service providers who have the right to evaluate the patient perform the required examinations and analyses.
2. The patient’s diagnosis is verified by the treating physicians or other groups.
3. Doctors develop the treatment or care plan required for the patient.
4. Doctors and medical service providers inform the patient of the treatment plan, alternative plans, complications and side effects, if any, and the expected result of each plan.
5. According to Article 21 of the Professional Ethics Regulations, it is permissible for humanitarian reasons not to inform the patient of the serious consequences of the disease. In this case, he must inform the patient’s family in a humane and appropriate manner of the seriousness of the disease and its serious consequences unless the patient expresses his desire not to inform anyone about his condition or specifies Certain people to inform them of it without risk to those around him.
6. Doctors and medical service providers inform the patient and his family of the expected costs of service and treatment. (See PR.2.10)
Administrator:
- Physician.
The Reviewer:
- Clinical evidence.
- Regulations of professional ethics.
- Egyptian quality standards approved from 2013.
|
|
|
|
|
|
|
|
Patient property preservation policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The hospital administration is committed to preserving patients’ belongings and working to encourage patients to send all their belongings to their homes or friends.
- Determine the hospital department and its responsibilities for patients’ property.
- The patient’s possessions (money, jewelry, watch, check book, wallet, etc.) are examined, recorded, and kept as safe deposit boxes in the hospital in the event that the patient’s identity is unknown or unconscious.
The Purpose:
- Preserving the patient’s property and specifying the hospital department to preserve it to ensure that the hospital is not exposed to accountability.
Working procedures:
· Patients should not keep any private property during their stay in the hospital.
· The patient, or whoever is legally entitled to do so, signs a declaration stating that he does not have any property if he does not have any property with him.
In the case of an unidentified patient (inability to determine the patient’s identity):
1. The responsible employee (hospital assistant) collects the patient’s belongings in a folder in the presence of the emergency nursing supervisor.
2. The assistant writes the contents of the portfolio (if the property is jewelry that is not described as gold or silver, but rather as a yellow ring with a white bezel, or silver jewelry... etc.) on the patient’s safe list form.
3. The person in charge of the emergency safe deposits, along with the nursing supervisor in charge of the emergency or her representative, sign the contents of the safe deposit list.
4. The person in charge of emergency safekeeping writes the patient’s name, date, and patient entry permit information on the clipboard in which the patient’s belongings are kept.
5. The person in charge of emergency safe deposits records the patient’s data in the relevant safe deposit register and places the number for the patient’s safe deposit list in the designated place in the safe deposit register.
6. The person in charge of emergency safe deposit boxes shall keep and secure the wallet in a designated safe deposit box and keep it tightly closed until requested by the patient himself or by someone who has the legal right to do so upon request.
7. The contents of the wallet are delivered to the patient according to the list available when he requests it, with his signature of receipt and his fingerprint being taken in the secretariat register.
· When the patient is discharged from the hospital.
1. The nursing staff supervising the patient’s treatment will notify the person in charge of safekeeping to bring the portfolio after ensuring that the numbers and contents match the receipt list available with the patient or whoever is legally entitled to receive it.
2. The employee responsible for safekeeping opens the wallet in front of the patient or whoever is legally entitled to do so, and the contents in the wallet are counted separately (money, jewelry, etc.).
3. The patient, or whoever is legally entitled to do so, retrieves the entire contents of the wallet and signs this in the safe deposit register, recording the date and hour of the retrieval, and the responsible employee signs as a witness to this.
4. A copy of the patient’s safe list is placed in his file.
Determine the hospital department and its responsibilities for patient property
The employee responsible for the deposits informs the patient or his legal representative that the hospital is considered responsible for the property of the unconscious patient only upon his arrival and the official receives the patient’s deposits, registers them, and signs their receipt, until the patient or his legal representative hands over the deposits and signs their receipt.
Administrator:
- Hospital Assistant.
- Responsible department nursing staff members.
Models:
- Declaration of the absence of property.
The Reviewer:
- Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
- Patient safety and security policy
Correct patient identification policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
Identifying the patient using two means before giving him treatment: blood or one of its derivatives, taking samples from the patient, or any diagnostic or therapeutic procedure.
The Purpose:
Achieving patient safety and reducing the risks that the patient may be exposed to during any procedure within the hospital.
Working procedures:
1- Everyone from the health team who deals with the patient must include:
· Doctors.
· Nursing.
· Pharmacists.
· Lab. Technician.
· Ray technician.
· Physiotherapist.
Use at least two means of identification for the patient to verify his identity:
· The name is fourfold.
· File No.
2- The nursing staff ensures that the identification bracelet data is correct before placing it on the right arm by matching it with the patient’s data and ensuring that it is legible and clear. If it is not possible to place the bracelet on the right arm for any reason, such as the presence of a cast, it is placed on the left arm.
3- The responsible nursing staff will place a new bracelet if the original is lost or becomes illegible.
4- The nursing staff confirms the patient’s full name as in the patient’s medical file and does not depend on another name (such as a nickname) and confirms the file number even if they are sure they know the patient.
5- The patient’s identity is verified before every interaction with him, such as:
Ø Giving treatment.
Ø Transfusion of blood or one of its derivatives.
Ø Taking a blood sample or any other samples necessary for medical analysis and laboratory examination.
Ø Transfer of the patient.
Ø Conducting diagnostic tests.
Ø Or when taking any other actions.
Note: Do not apply an identification label before taking the sample or on the package when it is empty.
6- When taking any measures, the nursing staff asks the patient about his name and introduces the patient herself and the procedure that will be taken, taking into account the presence of the patient’s bracelet and the two means of identification clearly written on it, which are the patient’s name and the file number.
7- Then the nursing staff matches the patient’s data on the bracelet with that in the medical file to confirm the patient’s identity before any action will be taken.
8- When taking a sample, the laboratory technician or nursing staff places a sticker identifying the sample that includes the patient’s name and file number immediately after taking the sample and before leaving the place.
Note: The laboratory technician performs the same patient identification procedures before withdrawing any sample.
9- In the case of premature infants, a bracelet is placed on the child’s right leg.
10- In the case of patients who have disturbed consciousness or are in a coma and for whom there is no way to prove their identity, their identity is proven by the following (unknown/unknown - patient number - date and hour of admission)
· If it is an accident, a report is prepared to prove the accident.
11- For newborns, they are identified by a bracelet placed on the foot with the following recorded:
· Mother's name
· Male Female
· File No
12- Dialysis patients: They are identified by an enclosed badge with the patient’s name on it
13- Patients in the emergency room or recovery room with the patient’s name in three and the reception ticket number
14- Outpatient patients have their test tubes and x-rays identified by the patient’s full name and outpatient ticket number
15- The radiology technician marks the x-rays with the patient’s quadrant name, file number, date, and time
16- None of the hospital employees remove the bracelet of any deceased patient until he leaves the hospital
17- In the event of an error in the patient identification process, reference is made to the incident report requirements policy
Responsible:
Medical team
References:
- International standards for patient safety.
- Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
Patient delivery and receipt policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The hospital's medical team is committed to the process of handing over and receiving patients' conditions in the various departments, including:
• Determine the necessary duties that must be handled during the delivery and receipt process.
• Determine who is responsible for delivery and receipt.
• Determine how to document the delivery and receipt process.
The Purpose:
• The delivery and receipt process is a vital process in order to maintain the safety and security of patients by codifying the exchange of patient information among the medical team while he is in the hospital for the continuity of providing medical care to patients.
Responsible for delivery and receipt:
• Between doctors of the same specialty by using the hand-over model.
• Between doctors with different specialties for patients whose condition requires consultation with doctors from more than one specialty, using the medical consultation form.
• Emergency doctors when transporting the patient to and from hospital departments (Patient Transport Form).
• Between nursing staff members with each shift change (situation book).
• Nursing staff members when transporting a patient to and from operations, care, or to another department (time out form)
Working procedures:
• When a new patient is admitted, the head nurse or her representative receives the patient from the paramedic and the admission or reception office worker, and records all the patient’s data and what the treating physician requested in the patient’s condition record.
• Nursing staff members record the patient’s conditions throughout the shift in the patient conditions record.
• After the shift ends and the nursing staff attends the next shift, the nursing staff delivers the conditions of all patients in terms of the development of their medical condition, especially critical cases, surgical cases, treatment given to the patient, any change that has occurred, and any requests such as bringing test results or rumors related to the patient, and preparing the patient for operations, if any. ............etc., with the delivery and receipt documented with the signature of the two nurses in the notebook.
• In cases of operations, the nursing staff prepares the patient for the operation according to the doctor’s instructions. The nursing staff hands over the patient and the patient’s pillow to the nursing staff for the operations and treatment for the patient if requested by the doctor in accordance with the patient preparation form for operations and the patient receipt portion of the time-out form.
• After completing the operation, the surgical nursing staff contacts the department nursing staff to come to receive the patient and the patient’s footbed.
• When there is a need to transfer the patient, the nursing staff transfers the patient and delivers the patient’s file after updating it to the nursing staff in the department to which the patient is transferred within the hospital.
• Resident doctors receive and pick up the patient at the start of the work shift according to the patient handover form that includes: ) Patient’s name - File number - Diagnosis - Positive medical examination results - Positive test results - Follow-up and notes).
• When the patient needs to be referred for consultation, the consultation form is used and the required data is recorded according to the form
Administrator:
• Nursing staff members.
• the doctors.
Models:
• Medical file.
• Record patients’ conditions.
• Consultation form.
• Delivery and receipt form for doctors.
• Operations time-out model.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy to avoid incorrect connection of catheters and tubes
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
· Specifies the necessary data that must be placed on the catheters, as well as those responsible for handling them, to avoid the connection or incorrect use of the catheters.
The Purpose:
· Achieving patient safety by avoiding incorrect connection of catheters and tubes in the artificial kidney unit.
Working procedures:
· Patients, their families, or hospital employees do not have the right to disconnect, install, or reinstall any type of tube or catheter, except:
Ø The doctor.
Ø Nursing staff members.
Ø Supervisor.
Informing the patient of this is the responsibility of the nursing staff responsible for the patient’s room.
· The department creates a policy for each type of tubes and catheters in the department, explaining:
o Responsible for installation.
o Installation and installation method.
o Ensure the integrity of the installation.
o Follow up and care for the connection.
· The following information is required to be shown on each catheter: the name of the installer, date and hour.
· Installation and verification of the correct installation of each type is carried out according to its policy.
· The doctor must specify the name and type of tube through which the medicine will be administered.
· Nursing staff must verify all connections before giving any medication and before and after performing any procedure in accordance with the policy for each type.
Administrator:
• Members of the nursing staff.
• the doctors.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Safe use of restraint and seclusion policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
· The patient’s safety and security are maintained and his right not to be restricted unless there is harm to the patient or those around him
· The patient is restrained for the shortest possible time after evaluating the patient and ensuring the necessity of restraint using the least means
· The patient is restricted based on the order of the qualified treating physician
Purpose: To preserve the patient’s rights and dignity and prevent him from harming himself or others.
Restraint: is a means that reduces or prevents the patient's movement. There are two types:
Either physical: This is a method of restraining the patient by the hands, feet, and torso of the body.
Or medicinal: It is a medication given with the aim of reducing the patient’s movement and calming his behavior.
Isolation: This is the restriction of the patient’s residence in a special room or area in cases of violence and aggressive behavior by the patient towards himself or those around him, including workers, patients, and others.
Reasons for restriction:
1. A patient who suffers from psychological disorders that make him capable of harming himself or those around him.
2. A neurological patient who suffers from a cerebral shock and in the event of agitation makes him unable to move unconsciously and capable of harming himself and others.
3. The post-operative patient is agitated, leading to harm to himself and others.
4. A liver patient who suffers from a state before hepatic coma and is in a state of agitation.
5. The patient is conscious but has a history of hurting himself before or removing the devices installed on him, such as the monitor - the central vein - or injection and pumping devices.
Reasons for isolation: The patient with behavioral diseases is isolated in a room alone until he is transferred to another hospital and the patient’s family is informed.
Procedures :
First: Patient evaluation:
· The responsible nursing staff determines the patient’s need for registration based on his behavior
The treating physician records the restriction order in the patient’s medical file, explaining the following:
The reason for the restriction
The type of restriction required
The time the restraining order was given/the specific duration of the restriction
Restriction started:
· Registration is performed using the fastest available method, whether pharmaceutical or physical, except after consulting a consultant, but in some cases it is prohibited to use the pharmaceutical method.
Restriction method:
· Nursing personnel use leather belts, gauze and cotton ties, or other means to restrain parts of the body. The four limbs are often used for restraint, except in cases such as meal times and personal hygiene.
· Female: The responsible nursing staff wraps the legs together and then ties them to the foot of the bed.
· Male: The responsible nursing staff restrains each leg of the patient individually at the foot of the bed.
· The treating physician shall sign the verbal registration order within 24 hours from the time he is notified of the case.
· The nursing staff takes care not to harm the patient psychologically or physically during the restraint.
· The nursing staff takes care to maintain the patient’s privacy.
· Patients whose freedom is legally restricted. The doctor is prohibited from participating in restricting them except when there is a strict medical necessity (Article 35 of Professional Ethics - Resolution 238 of 2003)
Second: Patient follow-up:
· The nursing staff records the patient’s follow-up using the relevant form, which includes the following data:
- Patient’s behaviour
- Vital Signs
- Blood division
- Skin condition
· Responsible nursing staff members follow up on the patient under restraint and for medical and surgical reasons at least every two hours, and this is documented in the patient’s medical file.
· Nursing staff members follow up on the patient under restraint for psychological reasons at least every half hour, and observations are recorded in the patient’s medical file on the patient restraint form.
Third: Renewal of the restriction order:
· Restraining orders made for medical and surgical reasons, the treating physician must renew the order at least every 24 hours based on continued need.
· Restraining orders made for psychological reasons, the treating physician must renew the order at least every 6 hours based on continued need.
Fourth: Ending the restriction:
· Specifications for ending the restraint: It either completely improves the patient’s state of consciousness or deteriorates and leads to a coma.
· Trained nursing personnel terminate the patient’s restraint in accordance with the doctor’s orders, according to the patient’s condition and in accordance with medical evidence, provided that the time and date of ending the restraint are recorded.
Fifth: Training:
· The person responsible for the hospital's patient care policies provides practical training to the doctors and nurses in the internal care department on how to implement the policy.
Sixth: Health education for the patient and his family:
The doctor/responsible nursing staff informs the patient and his family of the following:
- The extent of the need to restrain the patient
- Restriction period
- Rating rate during restriction
Responsible:
Nursing staff members
· Physician
Forms:
Restraint and follow-up order form
The Reviewer:
· Egyptian Quality Standards 2013
· JCI Standards 2014
|
|
|
|
|
|
|
|
Critical outcomes policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The policy explains the following:
· Definition of critically significant results.
· When to report critically significant results.
· How to report critically significant results.
· Who reports critically significant findings.
· Who receives the communication of critically significant findings.
· Document reporting of critically significant findings.
Purpose:
To maintain the safety and security of the patient and take appropriate action when there are critically significant results that require rapid intervention by the treating physician or any member of the medical team.
Definition:
Panic Values: These are results that may indicate the presence of a life-threatening situation for the patient that requires an urgent response or rapid intervention by the treating physician.
Working procedures:
1- Each department develops a list of its critical results, which includes the following:
· Results of critical laboratory tests (laboratory).
· Results of critical diagnostic examinations (Radiology Department).
· Critical medical examination results (internal departments / care / dialysis......).
2- In the event of any result of critical significance according to the previous lists, the person in charge (laboratory physician/radiologist/resident physician/department nursing staff members/laboratory or radiology technician) shall immediately inform the treating physician or department nursing staff members.
3- The informant must verify the full name of the person who was notified.
4- The recipient of the report (the treating physician) - (the nursing staff) shall do the following:
· Record the critical result immediately in the critical results log.
· The recipient of the report re-reads the patient’s data and test results to the informant in order to ensure that everything that was received and recorded in the patient’s file is correct and accurate.
· The treating physician has the right to accept or reject the result in light of its suitability to the patient’s condition, which may require a re-examination or procedure from the informant.
5- Document the reporting process through the following:
· The recipient (the treating physician) – (the responsible nursing staff members) shall document in the critical findings record the following data immediately upon receiving the report:
(Today's date - Reporting time (hour and minute) - Test result).
The action taken in terms of accepting or rejecting the result or requesting a re-examination.
(The full name of the laboratory/radiology official who reported - the full name of the recipient of the report (the doctor - the nursing staff))
Administrator:
• Laboratory and radiology doctors.
• Resident doctors.
• Nursing staff.
• Physician..
Models:
• List of critical results for each section.
• Critical Results Model.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Model of findings with serious clinical implications
|
|
|||
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
||||||
- Policy for dealing with high-risk medications (including concentrated solutions)
Policy for dealing with high-risk medications (including concentrated solutions)
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
· Identifying high-risk medications by scientific names, collecting them in a separate list and distributing them to all medical service providers, and dealing with the medications included in the aforementioned list in the correct manner in accordance with the instructions for each preparation to ensure that the patient is not exposed to any therapeutic risks as a result of the incorrect use of concentrated solutions without diluting them.
The Purpose:
· Ensuring that high-risk medications are handled with due care in order to ensure that the patient’s health is not exposed to any therapeutic risks.
Identification:
· Dangerous medicines are medicines that cause serious danger to the patient when used incorrectly. Therefore, a list is prepared for them that explains what these dangerous medicines are that must be handled with care to avoid any error in their use.
Working procedures:
· The pharmacy director, with the help of hospital pharmacists, prepares a list of dangerous drugs and solutions with high concentrations, specifying the scientific name and instructions for dilution, administration, and observation.
· The pharmacy director distributes the list to all therapeutic departments and units in the hospital.
· These medications are not placed in regular departments, and their presence is limited to critical hot areas such as (care, operations, emergency, and kidney departments), and their presence is limited to departments inside the emergency vehicle.
· When using these medications, check with the doctor first and then do a double review by two nurses before giving them.
· When preparing these medications, it should be in a place with good lighting and away from any noise or interruptions.
When storing these medicines, a red sticker is placed on the box containing these medicines, and it is in a separate place from the regular medicines, provided that this sticker contains the following information:
- The scientific name of the drug
- The focus
- Pharmaceutical form
- Expiration date
· When dispensing these medications, the pharmacist places a red mark on each ampoule or bottle. In the event that the pharmacist dispenses large quantities, the nursing staff can be instructed to place this mark on each unit.
· When placing medications that are similar in pronunciation, shape, or both, the containers should be separated and not placed next to each other, in addition to writing clear addresses on the containers.
· A medication reference is placed in each section that includes (use of each medication - method of administration - doses - side effects - standards that must be followed regarding use and preparation).
When giving anticoagulants, the treating physician does the following:
o Use protocols that explain the initiation and continuation of anticoagulant therapy and the tests required for follow-up.
o Documentation of pre-treatment and current INR in the medical record.
o When anticoagulants are given, doses are linked to laboratory results.
o Use a pump if heparin is given continuously intravenously.
o Health education for the medical team, the patient and his family regarding:
(The importance of follow-up - adherence - drug and food interactions - negative reactions).
· When giving narcotic medications, the pain is evaluated by the doctor and the necessary measures are taken in the event of severe pain.
Administrator :
· Pharmacists
· The doctors
· Nursing staff
Models:
· List of high-risk medications
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards 2013.
|
|
|
|
|
|
|
|
List of high-risk medications
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
|
High Risk Medications |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
The policy of obtaining a list of the treatment that the patient takes upon admission to the hospital and upon discharge
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
· Obtaining a list of the patient’s current treatment so that it is complete and documented when the patient begins entering the hospital.
· Giving the patient a list of his entire treatment, explaining how to use it, upon his discharge from the hospital.
The Purpose:
· Achieving patient safety while in the hospital by ensuring that the patient receives a current treatment list so that the patient does not stop taking the medication, which may lead to his health condition being affected or the surgical operation for which he was admitted to the hospital being postponed.
· Ensuring the safety of the patient when he is discharged from the hospital or transferred to another place by giving the patient a list of his treatment so that he does not stop and his health condition is not affected.
The Definition:
· The doctor checks the patient’s current treatment upon admission.
Work procedures upon entry:
· The doctor evaluates the patient upon admission, asks him about the medications he is taking at home, and records this on the patient’s medical history form.
· The doctor performs a medical evaluation of the patient based on the results of x-rays, medical tests, and the patient’s current treatment.
Based on the doctor’s findings from the aforementioned examination and evaluation, he develops a treatment plan, taking into account the patient’s current medications to ensure continuity of health care, taking into account writing in Arabic and not using unknown or known abbreviations.
· The Pharmacy Department publishes a list of abbreviations that should not be used in writing medications, provided that it is reviewed every two years to add or delete any abbreviation.
Work procedures upon exit:
· The doctor provides a comprehensive explanation to the patient about the health condition upon discharge in a clear, simple and understandable manner.
· The doctor writes the patient’s discharge treatment in the medical record, follow-up card, and discharge summary, along with an explanation of the treatment to the patient.
· The department’s nursing staff delivers a follow-up card and a discharge summary to the patient.
· When a patient is transferred/transferred to another hospital, the treatment carried out in the hospital is written in the external transfer/referral form and the discharge summary.
Administrator :
· The doctors.
· Nursing staff.
· Pharmacy.
Models:
- A list of abbreviations that should not be used in writing medicines
- Discharge summary.
- External transfer/referral model.
The Reviewer:
· International standards for patient safety.
· Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy on drugs that are similar in form and pronunciation
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: Separate medications that are similar in appearance and pronunciation to reduce risks.
Purpose: To achieve patient safety while in the hospital by adhering to the system of separating medications that are similar in form and pronunciation.
Working procedures:
· The pharmacy prepares a list of medications that are similar in appearance and pronunciation, and it is responsible for renewing and updating this list every 6-12 months.
· The pharmacy manager distributes the list to all therapeutic departments and units in the hospital.
· The pharmacist separates them and writes clear addresses on the containers containing each one in storage areas.
· Medicines that are similar in appearance and pronunciation are highlighted in green.
· When dispensing medications that are similar in appearance and pronunciation, the pharmacist alerts those who will receive the medication from the pharmacy of the need to separate them for the safety of the patient.
· Nursing supervisors in departments and roles separate and write clear addresses on the containers containing each of them in storage areas.
Administrator:
· Pharmacists.
· Nursing staff.
Models:
· A list of medications that are similar in name and pronunciation.
The Reviewer:
· International standards for patient safety.
· Egyptian accreditation standards
|
|
|
|
|
|
|
|
A list of medications that are similar in appearance and pronunciation
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
A list of medications that are similar in appearance and pronunciation
Sound alike drugs
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A list of abbreviations that should not be used in writing medications
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|||||
A list of abbreviations that should not be used in writing medications
· U/ UI
· Q.D, QD, q.d, qd
· Q.O.D, QOD, q.o.d, qod
· MS, MSO4
· Mg SO4
· Trailing zero
· No leading zero
· Dose x frequency x duration
· › greater than
· ‹ less than
· Abbreviation of drugs names
· cc
· µg
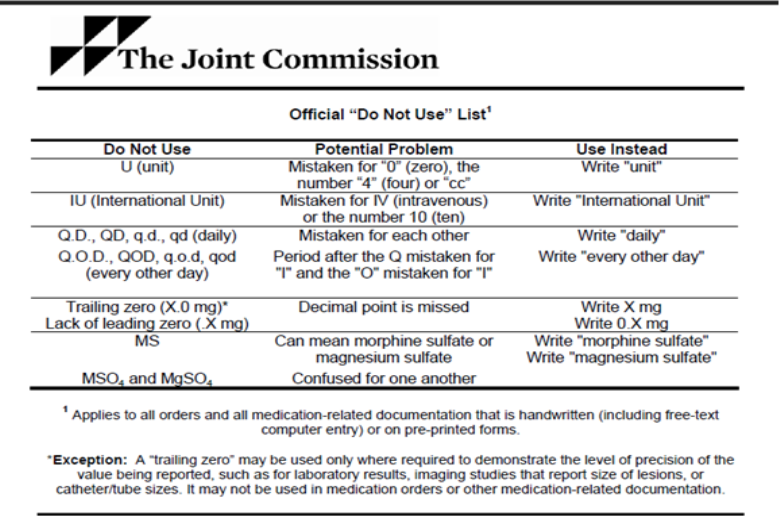
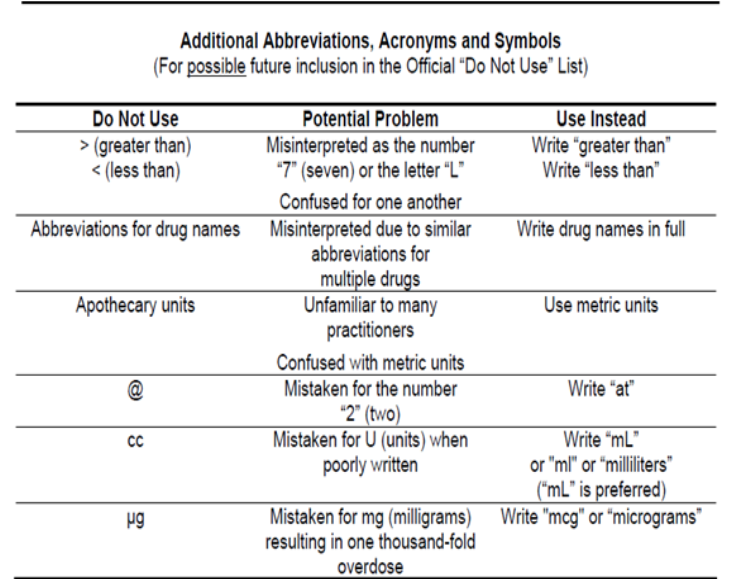
1. The nursing staff responsible for receiving the patient for operations receives the patient’s medical record and verifies the patient’s basic data.
- Private policies
· EKG policy
· Nursing care policy for angina patients
· Nursing care policy for heart attack patients
· Nursing care policy for patients with heart failure
· Nursing care policy for trauma patients
· Nursing care policy for patients with pulmonary infiltrates
· Policy for nursing care of an unconscious patient
· Nursing care policy for diabetic coma patients
· Electroshock device policy
· Central cannulation care policy
· Policy for receiving a patient for the first time
· Policy for receiving a regular patient in the unit
· A policy that assesses the dry weight of a patient with kidney failure
· Central venous catheter installation policy (MAHOCER)
· Policy for inserting a femoral venous catheter
· Policy for conducting serological examinations for patients
· Policy for starting a hemodialysis session
· Policy for completing the hemodialysis session
· Machine care policy
· Peritoneal dialysis policy
· Monthly analysis policy
· Monthly treatment disbursement policy
· Laundry unit accounts policy
· Employee health policy
Electrocardiogram policy
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Teaching nurses how to perform electrocardiograms for hospital patients in a quality manner and to protect the electrocardiogram device from damage as a result of misuse.
Tools and supplies:
The EKG device and its accessories, and ensuring that there are connections to the device
- Chart paper for the device - medical gel - cotton or tissue paper.
Steps:
Review the receipt of the patient’s application in terms of completing his data or not.
Hand washing (routine).
Preparing the necessary tools (EKG device and its accessories, ensuring the availability of the device’s connections - graph paper for the device - medical gel - cotton or tissue roll)
Help the patient to relax and lie on his back.
Explaining the procedure to the patient.
Help the patient to take off or lift his clothes from the places where the device’s electrical connections will be placed.
Ensure that there is no jewelry or metal on the patient before installing the extensions.
Placing the medical generation of electrodes.
Tie the electrodes around the wrists and around the legs in the correct manner.
The first connection for the chest (V1) is placed between the fourth and fifth ribs on the right side of the rib cage, (V2) the second connection is placed next to it on the left side of the chest, the third connection (V3) is placed under the nipple of the left breast, and the fourth, fifth and sixth connections are next to it on the left side.
Start operating the device.
Ensure that the feather traces its impact in the center of the device’s graph bar if the device is manual.
Complete the EKG by waiting until the readings are recorded.
Remove all connections from the patient and remove the medical gel using dry medical cotton or a tissue roll.
Help the patient cover himself and get out of bed.
Recording the patient’s data on the EKG (the patient’s name in four - date - hour - the signature of the person performing the work in three) after completing the EKG.
Record this in its own register to know the number of cases that have been completed daily.
Delivering the EKG to the nursing staff responsible for the patient.
Return the tools and arrange them in place until they are used.
Wash hands after finishing.
- Administrator :
Department nursing staff members.*
Department supervisor.
- The Reviewer :
Procedural work guide for the artificial kidney unit (Nursing Guide Line).
|
|
|
|
|
|
|
|
Policy for dealing with angina patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Dealing with angina patients.
The Definition:
It is chest pain resulting from a lack of blood ischemia of the heart muscle due to narrowing of the coronary arteries.
Steps:
Taking a medical history from the patient to confirm his condition and determine the location of the pain.
It calms the patient and puts him in a semi-sitting position.
Connecting the patient to the monitor to follow up on the situation.
Connecting the patient to oxygen.
Make an electrocardiogram and show it to the doctor.
Giving medications to the patient according to the doctor’s instructions (aspirin, heparin, nitroglycerin...).
Continuously assess pain according to the pain assessment map.
Conduct continuous follow-up of the patient through vital signs and electrocardiogram, and inform the doctor immediately.
The Reviewer :
Nursing Guide Line
|
|
|
|
|
|
|
|
Policy for dealing with heart attack patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Dealing with angina patients.
The Definition:
It is chest pain resulting from a lack of blood ischemia of the heart muscle due to narrowing of the coronary arteries.
Steps:
Taking a medical history from the patient to confirm his condition and determine the location of the pain.
It calms the patient and puts him in a semi-sitting position.
Connecting the patient to the monitor to follow up on the situation.
Connecting the patient to oxygen.
Make an electrocardiogram and show it to the doctor.
Giving medications to the patient according to the doctor’s instructions (aspirin, heparin, nitroglycerin...).
Continuously assess pain according to the pain assessment map.
Conduct continuous follow-up of the patient through vital signs and electrocardiogram, and inform the doctor immediately.
The Reviewer :
Nursing Guide Line
|
|
|
|
|
|
|
|
Policy for dealing with heart attack patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
Sudden chest pain resulting from the blockage of one of the coronary arteries, most often by a blood clot, which leads to part of the heart muscle being deprived of blood supply and thus dying.
Steps:
Taking a medical history from the patient to confirm his condition and determine the location of the pain.
Work to calm the patient and place him in a semi-sitting position.1
Connecting the patient to the monitor to follow up on the situation - Connecting the patient to oxygen.
Take an electrocardiogram and show it to the doctor.
Installation of 1-2 peripheral cannulae and taking a blood sample to perform complete laboratories including cardiac enzymes (troponin LDH - CPK).
Giving medications to the patient according to the doctor’s instructions (analgesics - tridylnitroglycerin - streptokinase...).
Nursing note when administering streptokinase:
Observe the patient's pressure and pulse, as well as note the patient's complaint of shortness of breath, vomiting, profuse sweating, and scratching. This occurs as a result of an allergy to it. In this case, streptokinase is stopped and a large dose of hydrocortisone is given.
The anti-streptokinase drug is cyclocaprone and is given in case of bleeding.
Performing an electrocardiogram for the patient before, during, and after administration.
Do not give intramuscular or subcutaneous injections to the patient during or immediately after administration.
Noticing bleeding from the nose or mouth.
Important notes: Nursing staff members must:
Continuously assess pain according to the pain assessment map. - Evaluate and record a complete description of the pain.
Complete rest for the patient to reduce oxygen consumption. - Do an EKG during pain.
Giving the patient oxygen if the patient feels short of breath and informing the doctor.
The Reviewer :
Procedural work guide (Nursing Guide Line).
|
|
|
|
|
|
|
|
Policy for dealing with heart attack patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
Sudden chest pain resulting from the blockage of one of the coronary arteries, most often by a blood clot, which leads to part of the heart muscle being deprived of blood supply and thus dying.
Steps:
Taking a medical history from the patient to confirm his condition and determine the location of the pain.
Work to calm the patient and place him in a semi-sitting position.
Connecting the patient to the monitor to follow up on the situation - Connecting the patient to oxygen.
Take an electrocardiogram and show it to the doctor.
Installation of 1-2 peripheral cannulae and taking a blood sample to perform complete laboratories including cardiac enzymes (troponin LDH - CPK).
Giving medications to the patient according to the doctor’s instructions (analgesics - tridylnitroglycerin - streptokinase...).
Nursing note when administering streptokinase:
Observe the patient's pressure and pulse, as well as note the patient's complaint of shortness of breath, vomiting, profuse sweating, and scratching. This occurs as a result of an allergy to it. In this case, streptokinase is stopped and a large dose of hydrocortisone is given.
The anti-streptokinase drug is cyclocaprone and is given in case of bleeding.
Performing an electrocardiogram for the patient before, during, and after administration.
Do not give intramuscular or subcutaneous injections to the patient during or immediately after administration.
Noticing bleeding from the nose or mouth.
Important notes: Nursing staff members must:
Continuously assess pain according to the pain assessment map. - Evaluate and record a complete description of the pain.
Complete rest for the patient to reduce oxygen consumption. - Do an EKG during pain.
Giving the patient oxygen if the patient feels short of breath and informing the doctor.
The Reviewer :
Procedural work guide (Nursing Guide Line).
|
|
|
|
|
|
|
|
Heart failure care policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Inability to pump an appropriate amount of blood to the rest of the body in order to reduce patient complications.
Tools and devices used:
EKG device.
Earphone .
Pressure device.
Normal range: 5 – 12 cm.
Steps:
Place the patient in a cool, quiet room to help him sleep.
Connect the patient to a monitor to monitor the number of heartbeats and perform an EKG.
Place all things within the patient's reach.
Keep the patient in a comfortable position constantly.
Reassure the patient about his health.
Conducting the necessary tests for the patient.
Educating the patient about the importance of rest when he returns home.
Introducing the patient to the symptoms of poisoning from Digitalis (nausea, vomiting, diarrhea, headache, depression, tension, dizziness, spasms, hallucinations, memory loss, increased or decreased heart rate, urticaria).
- Nursing staff must do the following before giving Digitalis (Lanoxin):
Taking the patient's pulse for a full minute with the stethoscope on the patient's chest.
Carefully observe the heart rate if it is regular or irregular and record it.
Stop the dose and inform the doctor if the patient's pulse is fast or less than 60 beats per minute.
Carefully observe the patient for any symptoms of anoxin poisoning.
Giving the patient meals rich in potassium.
Avoid giving the patient any food that contains sodium salts.
Weigh the patient every day at the same time on the same scale, usually before breakfast.
Taking care of the patient's skin because swollen skin is more susceptible to cracking.
Connecting the patient to oxygen in case of difficulty breathing.
Make a fluid chart for the patient.
The Reviewer :
Nursing Guide Line
|
|
|
|
|
|
|
|
Policy on how to deal with trauma patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
A decrease in the amount of blood that reaches the vital organs in the body, such as (the brain, heart, and kidneys), which leads to the tissues of these organs being deprived of a sufficient amount of oxygen and nutrients carried by the blood.
Steps:
Bringing the patient to the reception area and calming the patient down.
Connecting the patient to a monitor device and measuring vital signs in a regular manner to follow his condition moment by moment while monitoring the patient’s degree of consciousness.
Implementing the doctor’s instructions to treat the patient according to the type of shock and the factor causing it (in cases of bleeding, the patient’s blood is given - in cases of burns, plasma is given - in cases of vomiting and diarrhea, solutions are given to the patient) i.e. compensating the patient for the amount of fluids that were lost, whether through sweat Or bleeding.
Raise the patient's lower part so that the blood reaches the brain and this does not negatively affect the patient.
Put the patient on oxygen according to the doctor’s instructions.
Warm the patient naturally so that sweat secretion and loss of fluids from the body do not increase.
The Reviewer :
Procedural work guide (Nursing Guide Line).
|
|
|
|
|
|
|
|
Policy for dealing with the unconscious patient
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
It is a condition in which the patient loses his awareness and sense of what is happening around him. This is the result of disorders in the sensory nervous system, and these disorders are accompanied by a decline (decrease) in some brain cell functions.
Steps:
Assess the level of awareness and reporting.
Maintaining the integrity of the airways and breathing (setting an airway - adjusting the patient's position - applying oxygen according to the doctor's instructions)
Observe breathing and report. - Observing vital signs.
Observing the skin (its color - the areas of contact - the presence of dryness...).
Turn the patient over and create a turning pattern to maintain blood flow and skin integrity.
Continuously provide full care for the patient, especially (mouth, eyes, nose, skin folds...)
Maintaining the patient’s provision of appropriate nutrition for his condition via (intravenous or gastric tube (RIL) and recording the quantity on a fluid chart).
Place a urinary catheter and take appropriate care of it.
Maintaining the safety and security of the patient (such as raising bed barriers - taking care not to place sharp machines or supplies on the patient’s bed).
Recording, reporting, and restraining the patient according to the doctor’s orders, and following up on the restraint according to patient safety procedures.
Take notes for the comatose patient on the following points:
Description of level of activity or awareness:
- In full awareness (Alert) in danger - (Confused)
- Restless - Very sleepy - (Drowsy)
- In lethargic (Lethargic) in a complete coma (comatose)
Recording the data on a fluid balance map with the amounts taken in from treatment and fluids and out from urine and feces secretions...etc.
References:
Procedural Action Guide (Nursing Guide Line)
|
|
|
|
|
|
|
|
Policy for dealing with patients with pulmonary edema
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
It is lung congestion resulting from an increase in the amount of blood in the blood vessels in the respiratory system, which leads to great difficulty in breathing
Steps:
Help the patient to sleep at an angle of 90 or 45 degrees or sit in a chair because this position facilitates the breathing process.
Supply the patient with 8 liters of humidified oxygen or according to instructions.
Giving the patient medications according to instructions, such as:
Giving the patient a diuretic such as Lasix intravenously slowly.
Giving aminophylline to dilate the bronchi.
Suctioning the airways if secretions are present.
Installing a urinary catheter to calculate the amount of incoming and outgoing fluids, especially since these patients are given diuretics in large quantities.
Sometimes a patient needs a respirator to save his life.
The Reviewer :
Procedural work guide (Nursing Guide Line).
|
|
|
|
|
|
|
|
Central cannula care policy
|
|
ا |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The Definition :
◾ It is a measurement of blood pressure in the right atrium or vena cava through the installation of a catheter
Section: Nursing staff members before inserting the cannula:
◾ Explaining the steps to the patient and trying to reduce stress
◾ Hand washing (hygienic) – preparing tools
◾ Connect the patient to the monitor device
◾ Prepare the entire emergency vehicle next to the patient
Section: Nursing staff during cannula insertion:
◾ Place the patient in the appropriate position according to the doctor’s orders
◾ Open tools while maintaining sterilization steps
◾ Observe the monitor, discover any disorders, and inform the doctor
◾ Assisting the doctor in the installation steps
◾ Replacement of the cannula
◾ Take x-rays after installation to confirm its location
Section: Nursing staff after cannulation:
◾ Replace the catheter and follow infection control methods
◾ Observe the location of the catheter to detect any signs or infection
◾ Do not bend the catheter
◾ Measuring vital signs
◾ Keep the catheter open by dripping with a solution of saline + heparin, depending on the case
◾ Do not push the solutions forcefully in the event of a blockage of the catheter, but they must be drained by drawing blood
Method for measuring central venous pressure:
◾ Connect the CVP ruler to the patient.
◾ Close all solutions connected to the patient.
◾ Adjust the zero level with the ruler at the middle of the armpit.
◾ Close the valve towards the patient and open it towards the solution and the ruler until it is full, then close it towards the solution and open towards the patient.
◾ If the readings are below zero, they are negative, usually in a state of drought.
◾ The reading is unstable between two numbers if the patient is on a respirator and the second reading is taken.
Implementation Officer:
◾ The nursing team.
The Reviewer :
◾ Procedural work guide
|
|
|
|
|
|
|
|
- Patient reception policy
Receiving a new patient for the first time
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Receiving a new patient into the artificial kidney unit according to the standards of specialized medical centers and the standards of international quality organizations.
Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ The unit supervisor and the accounts employee interview the patient and present him to the unit director.
◾ The patient was presented to the unit doctor and examined.
◾ Determine the patient’s financial transaction by the accounting employee.
◾ Writing permission for virus tests for the patient by the doctor.
◾ Taking the sample from the patient by nursing staff.
◾ Virus results appear.
◾ Registering the patient in virus registries.
◾ The result is positive for viruses B, AIDS. The patient is referred because there is no positive machine.
◾ Create a personal data card by the accounts employee.
◾ Determine the timing of the sessions by the unit director and unit supervisor, and give an appointment card.
◾ Nursing staff weighs the patient before entering the session.
◾ The weight in excess of its normal weight is calculated in order to be withdrawn.
◾ Make a sheet for the patient by the doctor.
Responsible for implementation: unit supervisor, accounts officer, unit manager.
References:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Policy for receiving regular patients in the unit
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Regular patient reception at the artificial kidney unit according to the standards of specialized medical centers and the standards of international quality organizations.
Purpose:
International quality for all our customers in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ The accounting employee confirms the appointment through the appointment card.
◾ Recording the patient in the unit’s records.
◾ Nursing staff weighs the patient before entering the session.
◾ Recording the patient in the unit’s visitor book.
◾ Calculating the weight in excess of the normal weight in order to be withdrawn.
◾ Connecting the patient to the machine designated for him.
◾ Preparing the machine for a hemodialysis session.
◾ Testing of electricity and water connections.
◾ Prepare a jerry can of washing solution and place it next to the machine.
◾ Place the stick inside the jerry can according to the type of washing solution.
◾ Open the machine and perform a test of the machine.
◾ Place the artery and vein connections in their correct place.
◾ Place the artery connection in a bottle of salt solution to remove the air from the filter and line.
◾ After ensuring that the air has exited, he placed an ampoule of heparin in the intravenous connection and made a closed circuit.
◾ Pass the solution for 15 minutes in the machine.
Responsible for implementation: nursing staff members in the unit, accounts officer.
References:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Dry weight assessment policy for renal failure patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
It is the weight that the patient has after the session in the following case:
He does not have difficulty breathing.
No swelling of the feet and legs.
Normal pressure (not low or high).
The patient does not experience muscle tension.
To reach this weight, the patient is advised to do the following:
Do not consume salt in all its forms.
Reduce drinking fluids in general, not just water, so that the fluid intake rate is one liter per day.
The patient's dry weight must be reviewed as it is a value that is subject to change (at least every month).
|
|
|
|
|
|
|
Mahurker (Clavicular Catheter Set) Installation Policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Installation of a Mahurker (clavicle catheter set) according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
Preparing the necessary supplies and medications by the doctor and with the assistance of nursing staff.
Sterilize the installation site by a doctor.
Giving Xylocaine solution to the site of application by the doctor.
Installation of a clavicle catheter set by a doctor.
Transferring the patient to the radiology department for a chest x-ray by the worker in the presence of nursing staff.
Show the x-ray to the doctor to follow up on the location of the catheter.
The catheter is installed by a doctor and assisted by nursing staff.
Starting the session on the dialysis machine.
After the end of the session, a 10 cm ampoule of heparin is given into the arterial and venous connection.
A silk plaster is placed on the place of the hook.
Responsible for implementation:
Doctors and nursing staff in the unit.
References:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Femoral catheter installation policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Installation of a femoral catheter according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
◾ Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ Prepare the required supplies.
◾ Sterilize the catheter site (groin) with Betadine.
◾ Giving Xylocaine at the site of installation.
◾ Catheter installation by a doctor.
◾ The catheter is installed by the doctor and the assistance of nursing staff.
◾ Starting the session on the dialysis machine.
◾ After the session ends, the femoral catheter is removed.
◾ Pressure on the catheter site for 10 minutes while doing exercises with the leg where the catheter is.
◾ After the bleeding stops, a sterile pad is placed on the catheter site and a plaster is applied.
Responsible for implementation:
◾ Doctors and nursing staff in the unit.
References:
◾ Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Policy for serological examinations of patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Serological examinations for patients in the dialysis unit according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
◾ Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ Viral tests are performed for patients in sections every 3 months (HCV-HBV-HIV) and no dialysis is performed for any new patient before performing a pre-test using the ELISA method. In the event of an extreme emergency, a session is held for the patient in the emergency room and a sample is drawn for analysis using the ELISA method.
◾ Sectional serological examinations are performed using the ELISA method.
◾ If a patient’s result is positive for HIV using the ELISA method, in this case another sample is taken and sent to the central laboratories of the Ministry of Health and Population so that it can be analyzed using the Western Blot method. If it is confirmed that he is positive for the infection, the patient is transferred to undergo dialysis in a hospital. Fever.
Responsible for implementation:
◾ Unit director, unit nursing staff members
The Reviewer:
◾ Proposed specifications for the dialysis unit
◾ National Infection Control Guide.
|
|
|
|
|
|
|
|
Policy for starting a hemodialysis session
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
The start of the hemodialysis session in the artificial kidney unit according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
Nursing staff wash hands (routine washing) before starting work.
Nursing staff wear protective clothing.
The nursing staff measures the pressure, pulse, and temperature before the session, and the pressure is measured every hour during the session and whenever the patient’s condition requires.
Nursing staff wash hands (surgical washing) before transporting the patient.
Disinfecting the site of the venous and arterial connection in the patient’s hand with betadine.
The nursing staff, in the presence of the doctor, places two Festula catheters in the patient's arm. After ensuring that the catheter is fixed in the patient's arm, the nursing staff connects the patient to the device.
Connecting the closed artery connection to the closed artery needle.
Open the valve after ensuring that there is no air in the connections.
Open the blood pump slowly and give the amount of heparin agreed upon with the treating physician.
Close the intravenous connection valve when blood reaches it and close the blood pump.
Connect the end of the closed-cock intravenous line to the end of the closed intravenous needle.
Open the blood pump slowly with all closed valves open.
Ensure that the blood level in the air barrier rises and speed up the blood pump gradually.
Wrap the extensions around the patient's hand securely and secure them.
The nursing staff fills out the follow-up paper information during the session for each patient.
The excess weight, blood pump speed, vital signs, medications and solutions are recorded during the session, and any signs of low blood pressure are noted.
Give the heparin dose at the specified times.
Observe and monitor blood pressure every hour during the session.
Note any changes that occur in the patient during the hemodialysis session.
Responsible for implementation:
Unit nursing staff, doctors
The Reviewer:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Patient complications policy during dialysis session
(low blood pressure)
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Dealing with low blood pressure during a dialysis session according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and followers of occupational health and safety policies and infection control standards.
Procedures:
Stop drawing until we restore balance to the patient.
Position the patient (head down and feet up whenever possible).
0.9% natural salt solution gradually, starting from 100 cm3, and according to the doctor’s order, quickly and not by drip.
Reduce the washing machine temperature to 36.5 degrees Celsius.
Avoid using 2.7 trisalt solution to avoid the patient feeling thirsty and consuming large amounts of fluids that will lead to weight gain.
Reconsider the assessment of the patient's dry weight, and accordingly, the withdrawal rate and withdrawal rate must be adjusted by the specialist physician.
Important Notes:
Reducing the speed of the blood pump does not lead to improving the pressure, but rather reduces the efficiency of washing, and increasing its speed does not cause a drop in pressure.
Be careful in weighing the patient only with the knowledge of the nurses, not the attendants, workers, or the patient himself before and after the session, and write that down on the patient’s sheet.
Prepare an intravenous device and a bottle of 0.9% salt for rapid intervention when the pressure drops and to avoid dismissing the patient from the session.
Patients who suffer from significant weight gain between sessions, it is preferable to use the (Isolated UF) or ISO program, or what is called external traction bypass, according to the doctor’s order.
Ineffectiveness of using dexamethasone ampoules during hypotension.
Responsible for implementation:
◾ Doctors and nurses in the unit.
The Reviewer:
◾ Proposed specifications for the dialysis unit.
◾ National Infection Control Guide.
|
|
|
|
|
|
|
|
Policy for terminating a hemodialysis session
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Ending the hemodialysis session in the artificial kidney unit according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ Prepare the necessary supplies (plaster + sterile gauze).
◾ Wear protective clothing (apron - gloves).
◾ Measure blood pressure before ending the session.
◾ Close the blood pump and close the artery valve and artery needle.
◾ Place the artery connection in the solution bottle and open the blood pump.
◾ Activate the connections and filter to ensure that blood does not clot in the filter.
◾ Raise the vestula and the nursing staff gently presses it.
◾ After ensuring that there is no blood in the place of the vestula, disinfect the site of the vestula with betadine, sterile gauze and plaster.
◾ Dispose of the connections, filter, and all consumables related to the patient, and sterilize the machine from the outside with chlorine and alcohol.
◾ Weigh the patient and record this in the papers.
◾ Measure blood pressure before allowing the patient to leave the unit.
◾ Recording all supplies and medications and signing the department’s nursing staff.
◾ The patient signs the session and confirms the date of the next session.
◾ Allow the patient to leave the unit by the worker.
Responsible for implementation:
◾ Nursing staff members in the unit.
The Reviewer:
◾ Proposed specifications for the dialysis unit
|
|
|
|
|
|
|
|
- Machine care policy
Machine care policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Caring for the machine after the session according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
◾ Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ Wear protective clothing.
◾ Remove the solution stick from the jerry can and place it in the machine.
◾ Connecting dialysis tubes to the machine.
◾ Ensure that all doors (pump, blood tank) are closed.
◾ Enter the Rinse program first.
◾ Enter the machine into the Disinfection program.
◾ Apply the necessary solution to the machine: chlorine or citric solution.
◾ After the machine finishes the program, the machine shuts down.
◾ Wipe the machine from the outside with chlorine diluted at a ratio of 2:8.
◾ Wipe the parts of all operating keys with alcohol.
Responsible for implementation:
◾ Nursing staff members in the unit.
The Reviewer:
◾ Proposed specifications for the dialysis unit
|
|
|
|
|
|
|
|
Peroneal dialysis session policy (temporary)
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Conducting a peritoneal dialysis session (temporary) according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
Explain what will be done to the patient.
Wear protective clothing and sterile gloves for both the doctor and the nursing staff.
Abdominal skin sterilization.
Injection of local anesthetic (Xylocaine) into the selected area in the lower abdomen by the doctor.
Installing a peritoneal catheter and verifying its placement by the doctor.
The patient and the connections are handled sterilely (sterile gloves).
A bottle of washing solution, whether concentrated or diluted, depending on the patient's condition, is placed inside the peritoneal cavity over a period of a quarter of an hour.
Leave it for 15 to 20 minutes, then empty it over a quarter of an hour.
Heparin and the antibiotic are placed in the lubricants or solution used according to the doctor's instructions.
Responsible for implementation:
Doctors and nursing staff in the unit.
The Reviewer:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Policy for conducting monthly patient analysis
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Conducting a monthly analysis of patients in the dialysis unit according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
The doctor visits the patient and determines the type of tests required.
Writing the tests in a test permit by the doctor.
Preparing special tubes for the sample type by nursing staff.
Samples are collected while following infection control instructions by the nursing staff responsible for the patient.
Send the sample to the laboratory by the worker in the unit.
Bring the analysis results from the laboratory through the secretariat.
Informing the doctor of the results and recording them in his patient file and the analysis notebook.
Giving a copy of the test permit to the accounting employee to place in the patient’s file.
Presenting monthly analyzes to the unit manager.
Responsible for implementation:
The unit director, doctors, the unit's nursing staff, the accounting officer and the secretarial.
The Reviewer:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Policy for disbursing monthly treatment to Ministry of Health patients
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics
Disbursing monthly treatment to Ministry of Health patients according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
◾ Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
◾ The patient or companion brings the decision.
◾ The decision is delivered to the accounts.
◾ The accounts give a scan of the patient signed by the accounts official.
◾ The doctor writes the required medications for the patient.
◾ The patient goes to a state-funded pharmacy to dispense medications.
◾ The patient signs a permission to dispense medications at the pharmacy.
◾ The pharmacist delivers a copy of the disbursement authorization to the accounts official to place in the patient’s accounts.
Responsible for implementation:
Unit pharmacist.
Unit accounts.
The Reviewer:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Dialysis unit accounts policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
Dialysis unit calculations according to the standards of specialized medical centers and the standards of international quality organizations.
The Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
The patient is brought to the dialysis unit.
The doctor signs a medical examination and determines the required tests and investigations.
Sessions are conducted for the patient at his expense according to his need and the doctor is determined until a decision is made at the expense of the state or the approval of the company.
The accounts employee and the specialist doctor write the necessary medical report.
The report of the tripartite committee is written for patients undergoing treatment at state expense.
Writes a medical report for corporate patients to obtain approval for dialysis.
After issuing the decision for the patients of the Ministry of Health or approval from the companies, the accounts employee receives it after informing the doctor and saves it in a special file in the patient’s name.
An appropriate time is determined for the unit and for the patient to undergo dialysis sessions.
A clavicle catheter (Mahurker) is installed, and the patient is held accountable for its installation. If the patient has had an arteriovenous connection, dialysis is performed through it.
And it's done three sessions per week at the specified times.
The accounting clerk records all patients with hesitations or other cases in a special program for the dialysis unit on the computer.
He also records records in a notebook for verification with the program on the computer and also with another notebook for nursing.
Then write down the monthly sessions and treatment again in the hospital’s software to extract the bill.
At the end of the month, the accounts employee prepares an invoice for the total number of sessions and monthly treatment for each patient, and it is sent to the marketing department, which sends it by division to the ministry or companies for collection.
Responsible for implementation:
Doctors, accounts officer.
The Reviewer:
Proposed specifications for the dialysis unit.
|
|
|
|
|
|
|
|
Employee health policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
Maintaining the health of the two years in the dialysis unit according to the standards of specialized medical centers and the standards of international quality organizations.
Purpose:
Providing treatment services at a distinguished level according to the standards of specialized medical centers and the standards of international quality organizations to all our clients in order to satisfy them while preserving the environment according to the standards and objectives of environmental protection institutions and following occupational health and safety policies and infection control standards.
Procedures:
The necessary training and instructions must be provided to people who are exposed to infection by virtue of their work on a regular basis (for example, annually). The necessary training and instructions are also provided to new health staff before they take up work in dialysis units, and this training is documented in a designated record.
All workers in dialysis units must be vaccinated against hepatitis B virus, and this must be documented in a designated record.
The health team must wear special, leak-proof clothing to protect themselves from infection and protect their clothes from getting dirty when performing procedures during which they may be exposed to splashes or splashes of blood (such as when starting and finishing a patient’s delivery for dialysis, as well as when cleaning dialysis machines and During the apheresis process).
The health team should not eat, drink, or smoke in the area designated for dialysis.
It is not recommended to take any special measures or impose any work restrictions on anyone infected with a blood-borne disease (hepatitis B and C).
Responsible for implementation:
Unit director, unit nursing staff members
The Reviewer:
◾ Proposed specifications for the dialysis unit
◾ National Infection Control Guide.
|
|
|
|
|
|
|
|