Second part
| Site: | EHC | Egyptian Health Council |
| Course: | Procedural work guide for the burns unit |
| Book: | Second part |
| Printed by: | Guest user |
| Date: | Monday, 23 December 2024, 5:08 PM |
- General Policies
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- A brief overview of the policies
The policies that will be presented are just a model, and the hospital has the right to make the policy in accordance with its work system.
The policy is reviewed every three years unless there is any change in it during those three years.
At the beginning of each policy, fill out the table as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
At the end of each policy, fill out the table as follows:
|
|
|
|
|
|
|
|
|
|
Evaluation policies
Evaluation areas and content policy according to each department
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
The hospital is committed to clarifying the areas and contents of the evaluation according to each department.
The Purpose :
Clarifying the areas and contents of the evaluation according to each section, which helps provide appropriate medical care to the patient, reach an accurate diagnosis, and develop a treatment plan.
Working procedures:
First: The treating physician:
1- The initial patient evaluation must include identifying the personal history, the patient’s complaints, and the patient’s family history.
2- The initial patient evaluation must clarify the patient’s medical history and medical examination, which includes (vital signs - examination of body systems according to specialty and condition).
3- Review the results of any evaluation performed on the patient outside the hospital (medical report) before admitting the patient for treatment inside the hospital.
4- Identify the patient’s previous treatments and the extent of his response to them in order to:
· Determine the initial diagnosis.
· Determine the research required for the patient.
· Develop an appropriate treatment plan.
· Identify the patient’s medical care needs and choose the best care for him.
5- The doctor re-examines the patient clinically after reviewing the patient’s complete medical history, within 24 hours of the patient’s admission to the hospital, according to the medical history and medical examination form.
6- Each of the departments determines the content of the medical evaluation according to the specialty and clinical work guides (heart, women, dialysis, premature infants).
7- The doctor records the diagnosis, examination results, and medical history in the patient’s file and signs it with the date and time.
8- The doctor re-evaluates the patient based on the results of the tests and examinations and the progress of his health condition. He registers and signs, writing the date and time in the patient’s file.
Secondly, nursing:-
· The nurse evaluates the patient upon admission to the hospital using the nurse evaluation form.
· The initial information and data are recorded when the patient enters the department on the nurse’s patient evaluation form:
- Vital signs (pressure - pulse - respiratory rate - temperature).
- Weight and height.
- Having an allergy.
- Pain assessment
- Evaluation of skin condition
- Assess the patient regarding the possibility of a fall
- Nutritional assessment.
- Evaluation of motor activity.
- The patient’s need for restraint or isolation.
- Informing the patient of his rights, responsibilities, and hospital policy within 24 hours of admission.
Third, anesthesia:
The anesthesiologist evaluates the patient's condition:
1- Before administering anesthesia according to a pre anesthesia sheet form showing the type of anesthesia planned.
2- Observing and evaluating the patient during anesthesia according to the form prepared for this purpose.
3- Evaluate the patient before leaving the recovery room according to the recovery model.
Fourth: Physiotherapist (evaluation of motor, functional, and rehabilitative activity in case the patient needs it).
Fifth: The treating physician evaluates the nutritional needs of patients, especially the cases that are sorted according to the nursing evaluation upon admission.
Sixth: The social worker, according to his job description (he verifies patients’ satisfaction, and conducts social research when the patient needs financial, material, educational, or social support).
Responsible:
Doctor - Nurse - Social Worker.
Forms:
(medical report - patient ticket - emergency form - nursing evaluation - anesthesia sheet - physical therapy form - patient satisfaction questionnaire).
References:
Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
Timeframe policy for completing the assessment
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
· The hospital is committed to evaluating the patient and determining his complete needs within 24 hours of his admission to the hospital.
The Purpose :
· Determine sufficient and permissible time to complete the patient’s assessment and determine his needs.
Working procedures:
1. The resident doctor evaluates the patient’s condition upon admission to the hospital.
2. Emergency surgery patient. The treating physician evaluates his condition immediately before performing the operation.
3. The nurse completes the nursing assessment when the patient is admitted to the hospital.
4. The patient is evaluated for physical therapy when he needs it, and this is decided by the treating physician.
5. The consultant evaluates the patient whose presentation is scheduled within a period not exceeding 24 hours for stable cases / anesthesia presentations in the internal department.
6. The anesthesiologist evaluates the patient in cases of emergency operations immediately before performing the operation.
7. The department supervisor calls the patient’s social worker when he needs him.
References:
Egyptian Accreditation Standards 2013
|
|
|
|
|
|
|
|
Minimum frequency policy and re-evaluation content
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Re-evaluation of patients in critical and non-critical cases that require long-term (chronic) treatment.
Purpose:
To ensure that patient care and assessment are properly monitored and continued
Working procedures :
First: In acute cases (critical units):
The treating physicians in the departments evaluate and determine the following
1- Degree of awareness and awareness.
2- Vital signs.
3- The occurrence of complications.
4- The results of the tests and treatment or (surgical interventions).
5- The extent of response to treatment.
o The nursing evaluation rate is continuous, and the alternate doctor is called when a critical result is issued (physiological - laboratory - x-ray) and when there is pain, and the doctor re-evaluates.
o The re-evaluation of the patient is documented and a follow-up note is recorded at least once per shift (every 24 hours), and any procedures resulting from a call or emergency or important events for the patient are recorded with the date and hour.
Second: In non-acute cases:-
Treating doctors evaluate patients in non-acute cases and ensure...
· Vital Signs .
· Complications occur
· The results of the tests and treatment
· Patient compliance with treatment and medical instructions.
This is done every 12 hours for the internal department by the specialist or doctor on duty, unless the clinical evidence requires less than that and this is documented in the patient’s file.
Third: Conditions that require long-term treatment (chronic diseases)
The doctors treating the departments that care for patients who need long-term or (chronic) treatment ensure that:
· Vital Signs .
· Complications occur.
· Results of tests and treatment.
· The extent of the disease.
The frequency of re-evaluation shall be once a day by the doctor on duty or as required by clinical evidence and documented in the patient’s file.
1. The specialist doctor re-evaluates the patient from various specialties while the patient is in the hospital to determine the extent of the response to the treatment and its effectiveness.
2. The on-duty nurse re-evaluates the patient each shift to determine the patient’s needs.
Fourth: Cases that need to be re-evaluated
· The treatment plan developed for the patient Individualized care plan
· Change in patient condition
· Diagnosis Patient diagnosis
· Expected outcome of care, treatment or service
· The extent of the patient’s response to previous treatment
3. The re-evaluation is documented in the patient’s file
The patient should be re-evaluated immediately before anesthesia is administered
Fifth: Content of re-evaluation for nursing
1- Vital signs: every 6 hours in inpatient departments, every 2 hours in care and premature care, after blood transfusion, before surgical operations, during recovery, and when the patient complains that requires re-measurement, or according to the doctor’s instructions.
2- Pain:
3- The possibility of the patient falling: every shift.
4- Skin condition: all skin color during recovery.
5- Nutritional evaluation: when the patient needs it according to the doctor’s orders.
6- Measuring blood sugar: according to the doctor’s instructions.
7- The patient’s need for restraint or isolation: according to the doctor’s orders.
Forms: Medical follow-up form.
References: Egyptian Accreditation Standards 2013
|
|
|
|
|
|
|
|
Pain assessment, re-evaluation and management policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
The hospital is committed to a process of assessment, re-evaluation and pain management.
Purpose:
To explain the process of assessing, re-evaluating, and treating pain.
Procedures :
1- The responsible nurse assesses the pain (according to the following table), determines its severity, describes the pain and its frequency by asking the patient and looking at the patient’s facial expression (in the event that he is unable to speak or in the event that he is a child), and this is recorded in the pain assessment form and kept in the patient’s file when Admission of the patient to the hospital.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 |
 |
 |
 |
 |
 |
|
2- The treating physician develops a pain treatment plan and records this in the patient’s medical file.
3- The responsible nurse implements the treatment and follow-up plan according to the pain model and the doctor’s instructions.
4- The responsible nurse re-evaluates the pain and records it in the previous form and completes it with each nursing shift. It is possible to re-evaluate more than that depending on the patient’s condition:
1. The charge nurse reassesses pain once before surgical operations, after surgical operations, once every hour for 3 hours, then every shift, or according to the doctor’s orders.
2. The charge nurse reassesses pain if pain is present and one hour after pain medication is given.
Responsible: Nursing staff members - Doctor.
Forms : Pain Assessment Form .
References:- Approved Egyptian Accreditation Standards 2013
Attachments : Clinical evidence for the indications for medications used to treat pain
|
|
|
|
|
|
|
|
- Nursing plan policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
The Services Department is committed to providing nursing care according to the patient’s needs and documenting it in the nursing care plan for each patient.
The Purpose :
1. Understand the patient’s needs and meet them.
2. Provide high-quality nursing care.
Steps:
The nursing team does:
1. Conduct a nursing assessment of the patient upon admission and determine the patient’s problems.
2. Writing down the patient’s nursing problems in the nursing plan, which includes: (problems/needs - nursing intervention - evaluation - signature).
3. Write the necessary procedures to help solve nursing problems.
4. Re-evaluation to determine the extent of the patient’s response to nursing interventions.
5. The department supervisor follows up the plan and implements its procedures.
Administrator :
Department Supervisor - Charge Nurse.
Models:
Nursing care plan template.
The Reviewer :
Comprehensive hospital accreditation guides.
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
The Nursing Services Department is committed to accurate nursing registration 24 hours a day in a correct, accurate and legible manner
The Purpose:
Record all patient data.
Teaching health team members to register on nursing forms in a correct, accurate and legible manner.
Steps:
The nursing team members do:
1. Recording every activity performed by the patient from the moment he enters his form.
2. The team begins by evaluating the patient using the prepared form.
3. The patient’s main complaint is identified and needs are determined.
4. Planning the care that will be provided to the patient.
5. Implement the plan carefully to obtain the desired results.
6. Evaluate the plan each shift to identify the development of the situation.
7. Repeat any of the steps of the plan that did not improve the patient’s condition.
8. Monitor vital signs and notify the doctor when any change occurs from normal levels.
9. The necessity of working and submitting a report on any emergency incident during the work period, such as (patient falling - patient escaping - error in administering treatment).
10. The health team members must pay attention to recording the nursing progress, which includes (the patient’s condition - the doctor’s recommendations - all medical procedures, tests, rumors - and surgical interventions - nursing intervention - patient evaluation for no new signs and symptoms).
Administrator :
Nursing staff members
Models:
Nursing notes - nursing assessment - vital signs - nursing care plan - treatment charts
The Reviewer:
Operational guide for nursing services at the Ministry of Health.
|
|
|
|
|
|
|
|
Policy for assessing patients for abuse or neglect
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
The hospital is committed to preventing harm or neglect to patients while they are in the hospital and dealing with these cases as soon as they occur to eliminate harm or neglect to patients while dealing with them.
Purpose:
To develop methods for dealing with patients in the event of exposure to abuse or neglect.
Mistreatment:
the patient while he is in the hospital, which leads to him being exposed to physical or psychological harm/injury, or both. There are types
Different types of mistreatment can be divided into:
Mental abuse:
By affecting the mental state.
Manifestations of mental abuse:
· Verbal assault.
· To threaten .
· Intimidation .
· isolation .
· Insult.
· Humiliation.
· Deprivation .
Physical abuse:
By affecting the patient's physical condition by exposing the patient to (beating, slapping, kicking).
Manifestations of physical abuse:
· Patient falling.
· The appearance of bed sores in the patient.
· The presence of wounds that are not well cared for.
· The presence of unexplained injuries.
· Physical pain when touched.
· The presence of marks resulting from biting, scratching, abrasions or bruises.
· Unexplained signs of dehydration and malnutrition, sickness, sunken eyes, or eye injuries.
· The presence of blood stains in the underwear.
Sexual mistreatment:
The patient is exposed to any form of sexual assault/harassment.
Physical abuse:
Manifestations of physical abuse:
· theft .
· Misuse of money and property.
· blackmail .
· scam .
· There are abnormal actions in the patient’s bank account.
· Indifference to spending money.
Negligence:
It is any negligence [dereliction of treatment] that harms a patient in need without an acceptable medical reason from a responsible person while the patient is in the hospital.
Special need:
He is a person who needs the help of another due to (a mental disability, age deficiency, or brain atrophy/dysfunction), which hinders the person’s ability to protect himself or provide his own care.
Types of negligence that the patient may be exposed to:
· Negligence in medical and nursing care.
· Neglecting to give treatment doses.
· Neglecting social and psychological needs.
· Lack of food/water.
· Placing the patient in an unsafe place or without supervision.
Procedures :
1. The doctor and nurse evaluate the patient’s condition and determine his treatment needs.
2. The doctor and nurse inform the patient of the treatment plan and how to implement it.
3. The nurse teaches the patient how to call her when needed
4. The social worker visits patients in the internal departments daily to monitor patients’ complaints in order to report them to management and those responsible for resolving their complaints.
5. In the event that a case of neglect or abuse is discovered, the patient’s treating physician shall be informed:
- The doctor evaluates the patient’s condition and identifies manifestations of mistreatment or neglect, and a report is written with a commitment to physical and psychological treatment for the cases. - The doctor asks the patient to write his complaint (for the damages inflicted on him) if he wants, with or without a signature.
The head of the medical board appoints whomever he deems appropriate to investigate and follow up on the complaint, then the results are presented to him for necessary action.
Responsible: - Doctor - Nurse - Social Worker.
Forms: - Patient Rights and Duties Form - Form for acknowledging the existence of trusts
|
|
|
|
|
|
|
|
Minimum medical history and clinical examination policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital is committed to setting the minimum requirements for a patient’s medical examination upon admission.
Purpose: To determine the minimum medical examination and medical history necessary to evaluate the patient upon admission to the hospital.
Working procedures:-
1. The department doctor takes a medical history and examines the patient upon admission according to the medical history and medical examination form, which includes:
· The patient’s personal history, which explains (full name - gender - age - profession - marital status according to the national ID card - special habits such as smoking and drinking alcohol).
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Critically ill patients most at risk must be identified and followed up. Then the medical team begins the evaluation process and the plan is coordinated and implemented with the patient and family.
The Purpose:
· Identifying patients most at risk, such as children, individuals with special needs, the elderly, and psychiatric patients in the hospital, and the special evaluation necessary for each of them.
· Medical cases that require special services regarding hospital care:
◾ Age 75 years or older.
◾ Change in the state of consciousness or related disorders (mental disorders).
◾ Injuries, multiple fractures, fractures of major joints.
◾ Malnutrition, dehydration, microbial poisoning.
◾ Patients with late cases.
◾ Children.
◾ Victims of abuse, neglect or injury.
◾ Dialysis patients.
◾ Intensive care patients.
◾ Patients with chronic diseases.
◾ Patients who are prone to falling.
◾ Patients exposed to bed sores.
· Patients taking sedative medications and diuretics.
Procedures:
· The medical team matches the at-risk cases to each patient within 24 hours of his admission to the hospital, and if the patient’s condition matches one of the following cases, the patient’s expected risk signs are determined.
· Doctors and nurses record current and expected problems and main and alternative solutions in care plans.
· Doctors and nurses follow up on cases and re-evaluate them according to the requirements of each case.
|
|
|
|
|
|
|
|
- Medical files (anticipated events policies)
Policy for uniform and consistent content of the patient's medical file
| ||||||
|
|
|
| |||
Policy:
Staff familiarity with the established composition of the patient’s medical record.
The Purpose :
· Having a medical record for every patient examined and treated.
· The fixed composition of the patient’s medical record contains sufficient information such as:
◾ Identify the patient by name - address - file number.
◾ Allows continuity of care.
◾ Confirm the diagnosis.
◾ Justifications for treatment.
◾ Documenting treatment steps and results.
· The components of hospital patient medical records are standardized and have a specific format, and doctors and nurses are committed to using the forms optimally and containing:
◾ Writing treatment orders in a unified manner and in the same place.
· Department nurses are obligated to familiarize the patient with all patient record forms, which contain:
◾ Patient’s name in quadruplicate - standard number
· It is done with examination reports, rumors, the medical report, and a copy of the discharge summary in the patient’s file.
· The medical team corrects or amends one of the data recorded in the medical record by placing parentheses around the inaccurate data, taking into account ensuring that it is still readable, signing in front of him, and recording the date and time of making the correction, as it is not permissible to erase or delete incorrect data.
· Availability of data related to consultations as evidence that the consulting physician reviewed the patient’s medical record and the results he reached when conducting the medical examination on him, as well as the consulting physician’s opinion and recommendations.
· Issuing verbal diagnostic and therapeutic orders to a qualified nurse. The orders must be signed within twenty-four (24) hours, and all orders must bear the date, time, signature, and procedures applied.
· The clinical data recorded in the medical record and any other data and signatures are clear and legible.
· Send a referral form with the patient when he is transferred to another hospital, while keeping a copy in the patient’s file.
· Giving the patient a discharge summary with complete information.
Procedures:
Nurses ensure that the file contains the following data upon entry:
· Patient’s full name - uniform number - age.
· Name, address and telephone number of a relative of the patient or someone who can be contacted in case of emergency.
· Nurses do the following:
· Writing the patient’s name in full and his uniform number on all pages of the medical file.
· Recording the vital signs and medical condition of the patient in the vital signs record and the nurse’s notes record
· Modify the treatment implementation plan according to the doctor’s amendment on the doctor’s orders page.
· Doctors do the following:
· Complete the patient examination record and the record contains the following data:
· The type of allergy the patient suffers from, if any.
· Whether the patient suffers from any chronic infectious disease such as hepatitis.
· Diagnosis when the patient enters the hospital.
· The patient’s complete medical history: previous, current, and family medical history.
· A detailed statement of the patient’s clinical examination, a statement of the results drawn, and the action plan.
· Mention the results of laboratory tests and x-rays
· Write the type of treatment applied clearly on the doctor’s orders page.
· Request all required examinations or tests on the clinical progress page
· Recording all types of follow-up, consultations, and routine and special treatments appropriately in the appropriate forms.
· Take notes on the development of the condition at least daily for patients with serious conditions, as well as for patients whose conditions are difficult to diagnose or control their clinical problems. Notes of the development of the condition must also be recorded at the time of the observation to allow for continuity of care and the possibility of transferring the patient from one department to another. Also, as much as possible, it must be determined Each problem that the patient suffers from should be clearly stated in the case progress notes and linked to the orders issued regarding it, as well as the results of examinations and treatment. On the other hand, comprehensive notes about the development of the condition during the surgical procedure and immediately after the completion of the surgery must be recorded in the record. This is done for the purpose of providing correct information for use by any caregiver who subsequently assumes responsibility for caring for the patient
· Writing all surgical reports immediately after the end of the surgical operation, provided that they include the patient’s full name, medical file number, date of the surgical operation, diagnosis before and after the surgical operation, the name of the surgeon and his assistant, the name of the surgical operation, and a detailed statement of the results and methods used during the operation and anesthesia. The samples taken, the amount of fluid secreted, complications, reasons for surgery, and the patient’s condition before the operation.
Writing a summary of discharge or death in all medical files of patients admitted to the hospital, which includes:
◾ Entry and exit dates.
◾ Initial diagnosis - final diagnosis.
◾ Analysis.
◾ Actions taken.
◾ Medical drugs and other treatments.
◾ The patient’s condition and the next stop upon discharge.
◾ Discharge instructions, including food, medication, and follow-up instructions.
◾ The name of the doctor who discharged the patient.
Complete the referral form as follows:
◾ Reason for referral
◾ The required means of transportation and follow-up
◾ Description of the case
◾ Next stop
The emergency patient's medical file contains:
◾ Patient arrival time and discharge time.
◾ Final results at the end of treatment.
◾ The patient’s condition upon discharge.
◾ The patient’s destination upon discharge.
◾ Medical care instructions for patient follow-up.
◾ Documentation of the discharge order from the treating physician.
Responsible:
Nursing and medical staff members.
Forms:
Patient records - content of the medical file for each department.
References:
Ministry of Health Medical Records Guide.
|
|
|
The policy of who has the authority to write in the patient’s medical file
| ||||||
|
|
|
| |||
Policy: The medical team, including nurses and treating doctors, is authorized to write in the patient’s medical file their names, clear and legible, and their job titles, provided that the information is clear and in legible handwriting, with the date and hour written.
Purpose: Determine who has the authority to write in the medical file.
Procedures:
· When recording their performance in patient files, nurses are obligated to write their names (first name) and record the date and hour.
· When registering in patient files, doctors are obligated to write their names (first and last names), use clichés, and write the date and time.
· All research, examinations, and treatments requested for the patient must be signed by the treating physician, with his name written in triple and his stamp.
· The person performing the medical tests and x-rays signs the results of the tests and x-ray reports with his or her full name and the date and hour.
Administrator:
Nursing and medical staff members.
|
|
|
The policy of who has the right to view the patient’s medical file to ensure the confidentiality of the information
| ||||||
|
|
|
| |||
Politics:
· The medical record is considered a legal document, and therefore its confidentiality must be maintained, and this confidentiality is the basis of the legal aspect of the medical record.
· Establish controls to maintain the confidentiality of information and determine who has the right to view the medical record and what data they are permitted to view.
Purpose:
To maintain and protect the confidentiality of patient information and data.
Procedures:
· All hospital employees sign a declaration of confidentiality of patient information.
Circumstances in which access to information in the medical file is permitted:
· If the file is requested from the medical team to view the patient’s examinations or information of clinical value, the doctor writes a request to extract the previous file in the current file, and the doctor signs it clearly and with the date, then submits the file to the medical records official to extract the medical file.
· In the event that the sick applicant is himself, his legal representative, or external parties such as (the Administrative Prosecution - the Public Prosecution - Inspection Bodies - the Ministry of Health), the hospital director or medical director shall review the request and provide the information in one of the following ways:
◾ Orally.
◾ An exact copy of the file.
◾ Summary of the case.
◾ The original file. In this case, a representative from the hospital will refer the file and return it after the decision on it is completed.
· If the patient is transferred to another hospital, the specialist doctor fills out the transfer form, which includes a summary of the case (diagnosis - reason for transfer).
· In the event of requesting a medical report on a case, the patient or his legal representative submits an oral request to the official of the Medical Records Office to contact the treating physician to write the report on the case. This is done on the same day and delivered to the applicant.
· The hospital has the right to withhold some medical information about the patient in the event that the information represents harm to the patient, such as ( the patient’s knowledge of the nature of the patient’s medical condition may affect his psychological state and lead to the deterioration of his condition).
· List of persons authorized to view the hospital’s medical file:
◾ The doctor responsible for the case.
◾ Doctors from other departments who are consulted about the patient’s condition.
◾ The nurse in charge of the case.
◾ The patient or his legal representative with the authorization of the patient.
◾ Hospital Director.
◾ Medical Director .
◾ Quality and performance improvement coordinator.
◾ Judicial and supervisory authorities and the Ministry of Health when needed.
◾ Medical statistics officer.
◾ Accounts Officer.
Responsible: All hospital staff.
Forms: Declaration of confidentiality of information
|
|
|
Policy for protecting medical records and information from loss, damage, tampering, and unauthorized use or access
| ||||||
|
|
|
| |||
Policy: Protect medical records and information from loss, damage, tampering and unauthorized use
Purpose: To ensure that the medical file is preserved from loss or damage and to ensure that the patient’s medical information is preserved so that it can be retrieved when needed.
Procedures:
The hospital’s medical records room meets the following specifications:
· Ventilation is adequate.
· Lighting is sufficient.
· Protection against fires.
· Intact storage shelves.
· Offices for employees.
· Entry to the file storage area is not permitted to anyone other than authorized persons (patient affairs employees only).
· The medical records office administrator files the patient's medical records on a shelf in the order of the month for each department.
· The Medical Records Office official shall repair all records with loose papers or torn covers immediately before important information recorded in them is exposed to further loss or damage.
· The official in the medical records office keeps all reports related to diagnosis, examinations, etc., such as medical reports, laboratory results, etc., in the medical file, except for x-rays, which are kept in the radiology department.
· There is a record of requests recorded in the place where files are kept, which includes the borrowed files and the person borrowing the file from the persons authorized to view the file.
· The medical records clerks assigned to work in the filing area are responsible for maintaining the cleanliness of the area and the proper ordering of files on the shelves.
Responsible : Medical Records Office
|
|
|
Policy for disposing of medical files and the duration of keeping records and files
| ||||||
|
|
|
| |||
Purpose:
To clarify the disposal of medical files by legal means and to clarify the legal period for keeping records and files.
Politics:
· Dispose of records within the specified period in accordance with regulations and laws.
· Dispose of records completely to prevent anyone from viewing them or extracting identical copies of them.
· Records may not be disposed of except based on an administrative order issued by the hospital director general.
Procedures:
· Inactive medical records may be disposed of after a certain period of time determined by the Ministry of Health guidelines.
· Records scheduled for disposal should be registered according to the patient's name, medical file number, and last date of activity.
· Records must be completely destroyed to prevent anyone from viewing them or extracting duplicate copies of them.
· The medical records official and clerk shall, on the first of December of each year, review the medical records to extract what has expired and is worthy of being permanently disposed of, in accordance with the guiding policies of the Egyptian Ministry of Health website.
· The medical records officer shall keep all records related to lawsuits or other investigations of a confidential or serious nature and shall not dispose of them until after the lawsuits are completed.
· The Medical Records Officer, on the first of January of each year, examines the discarded documents and after verifying the authenticity of the discarding, they are packed into bags by the department’s workers to be delivered to the Directorate of Health Affairs for disposal in accordance with the ‘archives list’.
· The following is the schedule for maintaining medical files and records.
Administrator
· Medical Records Department
The Reviewer
· Medical records guide for the Ministry of Health
· Guiding policies for the Egyptian Ministry of Health website.
|
|
|
Screening process policy to determine patients' needs for medical and nursing care
| ||||||
|
|
|
| |||
Policy: The hospital is committed to conducting a priority assessment of patients’ needs for therapeutic and nursing services when the patient is admitted to the hospital and the appropriate department for the patient’s condition.
Purpose: To provide medical care to the patient appropriate to his condition and in accordance with priorities and clinical work guides (therapeutic, diagnostic, palliative) when the patient is admitted to the inpatient department of the hospital.
Working procedures:
· The in-house department charge nurse conducts the initial nursing assessment of the patient’s condition using the Nurse Evaluation Form .
· The in-house department's charge nurse performs the pain assessment according to the pain assessment form.
· The nurse in charge of the case develops a nursing care plan according to the nursing assessment and documents it in the nursing plan form.
· The responsible internal department nurse contacts the specialist doctor and informs him of the patient’s condition.
· The specialist doctor reviews the medical history, completes the medical examination, and determines the patient’s needs for medical care.
The specialist doctor develops a treatment plan for the patient according to the priorities and treatment protocol for the case, which includes:
· Necessary examinations.
· Required tests.
· Treatment according to the treatment description form.
· Required follow-up and observation.
· Any other instructions.
The responsible nurse implements the treatment plan in the examination and research form, specifying the timing of the request and the hour of implementation
Responsible: Attending physician - Nursing staff members
Models:
The Reviewer :
· Accredited Egyptian Accreditation Standards 2013
|
|
|
Policy of information given to the patient and family upon admission to the hospital
| ||||||
|
|
|
| |||
Policy: The hospital is committed to informing and informing the patient and his family upon admission of the necessary information to make the appropriate decision to treat the patient.
Purpose: To determine the information that is given to the patient and his family upon admission to the hospital, which helps in making the appropriate decision to treat the patient, n. 8, and achieves the preservation of patients’ rights, facilitates the period of stay and obtaining the required medical care, and informs patients of their responsibilities towards the hospital, which achieves the satisfaction of patients and their families.
Working procedures:
· When the patient enters the hospital, the receptionist or admission office employee introduces the patient and his family:
· Patients’ Bill of Rights.
· Patients’ duties and responsibilities document.
· Hospital instructions regarding visits, food, and/or smoking ban.
· The receptionist/admission office employee informs the patient of the cost of accommodation and treatment and reviews the price list, in accordance with Ministerial Resolution No. 186 of 2001.
The treating physician acquaints the patient and his family with the necessary information that will help them make an informed decision, including:
· Nature of the disease and diagnosis.
· Expected result of treatment.
· Planned date of discharge from the hospital.
· Suggested treatment steps.
Responsible: treating physician - nursing staff members.
Forms: Conversion form.
References: Approved Egyptian Accreditation Standards 213
|
|
|
Patient management policy in the event that there is no available space for the required medical service
| ||||||
|
|
|
| |||
Policy: The hospital is committed to finding an alternative solution for the patient in the event that there is no room for the required service in the hospital.
Purpose: To know how to act in the event that there is no room for the required service in the hospital.
Working procedures:
· When a case is discovered for which there is no available place to provide the required medical service in the hospital, the treating physician provides first aid to the patient and writes a report on the case.
· The hospital helps the patient and his family to find an alternative place through the emergency department and the directorate, and provides a report to the patient’s family about the situation.
· After confirming the approval of the hospital to which the transfer will be made, the doctor responsible for completing the transfer procedures shall.
· By providing an equipped means of transportation suitable for the patient’s condition.
· The treating physician writes the private data in the referral form and keeps a copy of it and attaches it to the report on the patient’s condition while providing an appropriate companion for the patient.
· The treating physician provides medical instructions to the patient and his companion during transportation.
Responsible: Attending physician - Nursing staff members
Forms : Conversion form
The Reviewer :
· Accredited Egyptian Accreditation Standards 2013
|
|
|
The policy of coordination and cooperation between all departments
(including doctors and nursing staff) through the internal departments
| ||||||
|
|
|
| |||
Policy: The hospital is committed to providing means of coordination and cooperation between all departments.
Purpose: To know how to coordinate the provision of medical care to all patients.
Working procedures:
· Coordination between doctors and nurses.
· Implement nursing and physician orders in a timely manner.
· Record delivery and receipt for each category and carry out follow-up and required orders.
· Medical consultation.
· Coordination between departments during transportation or requesting diagnostic services:
· Use policies that determine the appropriateness of transporting the patient within the hospital:
· Surgical and non-surgical treatment services after conducting a medical consultation and accepting the case.
· Diagnostic services and therapeutic services.
· Emergency services and internal department.
Responsible : Attending physician - Nursing staff members
The director, his deputy or the administrative representative
Forms : Conversion form.
References: Egyptian Accreditation Standards 2013
|
|
|
Patient entry and exit policy
| ||||||
|
|
|
| |||
Policy: The hospital is committed to providing means of coordination and cooperation between all departments.
Purpose: To know how to coordinate the provision of medical care to all patients.
Working procedures:
· Coordination between doctors and nurses.
· Implement nursing and physician orders in a timely manner.
· Recording the delivery and receipt for each category and implementing the required follow-up and orders.
· Medical consultation.
· Coordination between departments during transportation or requesting diagnostic services:
· Use policies that determine the appropriateness of transporting the patient within the hospital:
· Surgical and non-surgical treatment services after medical consultation and acceptance of the case.
· Diagnostic services and therapeutic services.
· Emergency services and the internal department.
Responsible: treating physician - nursing staff members
The director, his deputy or the administrative representative
Forms: Conversion form.
References: Egyptian Accreditation Standards 2013
|
|
|
Patient entry and exit policy
| ||||||
|
|
|
| |||
Policy: The hospital is committed to providing means of entry and exit for patients.
Purpose: Unifying the standards for entry and exit of patients to ensure a distinguished level of service without wasting capabilities or differentiation in the provision of medical service.
Procedures:
First: Login procedures:
· The specialist of other specialized units is responsible for the decision to admit and discharge the patient after reviewing the consultant, if necessary, while adhering to the specifications included in the clinical work manuals approved by the unit director and compiled in the policy attachments.
· The qualified anesthesiologist has the right to request a reservation for a patient if he discovers the patient’s need during the patient’s evaluation before elective surgeries. The physician notifies the existing specialist of the need for an empty bed for the patient on the day before the surgical operation.
· The qualified anesthesiologist has the right to request that a patient be detained in intensive care if it becomes clear to him that the patient’s need is during the patient’s evaluation before urgent surgical operations. The treating physician notifies the specialist doctor in intensive care of the need for an empty bed for the patient before the patient enters the operating room.
· The qualified anesthesiologist has the right to request that a patient be detained in intensive care if he discovers the patient’s need during the surgical procedure if an emergency occurs. The specialist physician in the intensive care unit shall be notified immediately.
· The treating physician/anesthesiologist makes the request by filling out the medical consultation form.
· The treating physician in any department must provide a medical consultation with the care physician if the patient’s condition meets the specifications for admission to intensive care.
Second: Specifications of leaving care
· Stability of the patient's vital signs.
· Respiratory rate stabilized and blood gas levels improved well.
· The patient does not need medications that are difficult to administer outside intensive care, such as cardiac stimulants and others that are given intravenously using devices such as a solution pump and a solution syringe.
· Accompanying cardiac arrhythmia and no serious heart disorders.
· Stable nervous condition and no convulsions.
· Removal of circulatory catheters.
· The patient does not need high-level nursing services, such as care for a throat tube or a laryngeal incision.
Responsible: the treating physician - intensive care doctors - anesthesiologist - head of the premature infants department - head of the dialysis department
Models:
· Specifications established on a physiological and diagnostic basis for admission to intensive care.
· Specifications established on a physiological and diagnostic basis for admission of premature infants.
· Specifications established on a physiological and diagnostic basis for admission to dialysis.
The Reviewer :
· Egyptian Quality Standards 2013
Policy for terminally ill patients
Policy: The hospital is committed to providing medical services of a special nature to a terminally ill patient.
Purpose: Providing medical services of a special nature to a terminally ill and near-death patient that keeps him free from pain while providing psychological, social, and spiritual support to the patient and his family.
Procedures:
· The treating physician signs a careful medical examination and carefully reviews the patient’s file, including analyses, x-rays, and examinations, to determine the patient’s final condition.
· The treating physician presents the results of the clinical examinations and analyzes to the consultants in the appropriate specialties to determine the patient’s health condition and ensure the futility of any progressive treatment provided to him.
· After the consultants decide that this condition is incurable, a list of the symptoms accompanying the patient and how to treat them is written so that the patient is in a healthy state free of pain, even if this requires general anesthesia for the patient.
The patient's family is interviewed and the case is explained in detail by the consultants and the director of the unit caring for them, and moral support is provided to them.
· Conduct health education for them on how to deal with the condition.
The hospital is committed to providing and facilitating social support by consulting the citizen service office employee and providing the opportunity for the patient, if he requests, to have a clergyman attend for religious and spiritual support for the patient or his family.
Administrator :
· The treating physician and the treating consultant - employee of the Citizens Service Office.
The Reviewer :
· Egyptian Quality Standards 2013 - Joint Commission International Standards 2014.
Patient transfer, referral and discharge policy
Policy: The hospital is committed to maintaining the patient’s security and safety and identifying those responsible during the process of his transfer, referral, or discharge from the hospital.
Purpose: Defining what is meant and the situations in which a patient is transferred/transferred/discharged.
Establishing the foundations that ensure maintaining the patient’s security and safety and identifying those responsible for transferring, referring and discharging the patient inside and outside the hospital.
The Definition :
Patient transfer is the formal transfer of responsibility for patient care from:
· One care unit to another.
· One medical service to another.
· A specialist doctor for another.
· One institution to another.
Patient referral is sending a person from:
· One doctor to another or one specialist.
· One department or service to another or different resources either for advice or care that is not provided by the referring entity or because it is not qualified to provide this service.
The patient is discharged home
Working procedures:
First: Planning for transfer or transfer of the patient and discharge when developing a treatment and care plan for the patient
· The treating physician develops a medical care plan for the patient upon his admission to the hospital, completes the medical examination and required tests, diagnoses the condition, and provides first aid to the patient.
· The patient’s need for transfer or referral is determined when developing a medical care plan for the patient according to his condition and to ensure continuity and continuity of medical care.
The patient's medical care plan must include the patient's planned discharge date.
Second: Discussing the reason for the referral/transfer/discharge of the patient with the patient and his family
· The treating physician explains the reasons for making the transfer/referral/discharge decision to the patient and his family.
· This is done when making a decision, at the beginning of developing a treatment plan, or when clinical and diagnostic results appear that are not available in the hospital.
· The doctor records the reason for transferring or transferring the patient inside or outside the hospital in the medical file.
Third: Follow correct and safe methods when transporting or referring a patient
· The doctor records the required procedure within the patient’s medical file and ensures that all file data is completed, mentioning the reason for referral/transfer/or the patient’s condition upon discharge.
· In the case of referral, the referral form is completed explaining the patient’s condition/reason for referral/required procedure.
· In the case of consultation, the consultation form is completed in accordance with the medical consultation policy.
The method of transferring/referring the patient is determined according to his health condition.
When transporting/transferring a patient using a wheelchair or bed, the following measures must be taken:
· Inspect the bed/chair and ensure its safety.
· Make sure the sides of the bed are in place.
· The department supervisor contacts the referral/transfer location to ensure the availability of the required service for the patient, and the hour and result of the call are documented in the nursing status book in the case of internal referral/transfer.
· The responsible nurse notifies the admission and hospital accounts office to take the necessary measures for the transfer/transfer/discharge process.
· The nurse reviews the patient’s complete data and ensures that the recorded data is correct.
Fourth: Transferring a patient to another facility, cases of referring a patient to another facility:
· In the event that the service is not available in the hospital.
· Patient’s request for transfer to another facility.
· The specialist doctor provides first aid to stabilize the patient’s condition, if necessary.
· The specialist doctor determines the patient’s condition.
· The specialist doctor notifies the patient or his companions of the non-availability of the necessary service for the patient in the hospital.
· The treating physician ensures that there is a place suitable for the patient’s condition before transferring him by contacting the place receiving the patient and explaining the patient’s condition.
· The treating physician notifies an ambulance to transport the patient, accompanied by the ambulance doctor and ambulance nurse, or transport the patient according to his desire after writing an acknowledgment from him or his family.
· The treating physician completes the patient referral form
· The nurse and ancillary services worker transport the patient in a safe manner, as mentioned previously.
· The nurse makes sure to send a copy of the patient’s examination, procedures performed, research results, diagnoses, and treatment...with him to the place he is transferred to.
Fifth: Discharge of a patient:
· When the patient’s medical condition improves and stabilizes, the consultant/specialist determines the patient’s discharge date, the treatment plan at home, the type of nutrition, and the date of follow-up in the outpatient clinic.
· The doctor completes the discharge form for the patient and completes all the data in clear writing, and the patient is given the original discharge form and keeps a copy in the file.
· The specialist doctor explains the instructions that will be implemented during the recovery period to the patient and his family, including the method of taking medications, the method of dealing with the medical condition, ways to obtain rehabilitative services, methods of proper therapeutic nutrition, and follow-up appointments in the outpatient clinic.
· The nurse hands the patient his discharge form.
· The department supervisor ensures that the financial settlement is completed.
· The nurse removes the cannulas from the patient’s hand, if any, before leaving the department.
The nurse reviews the patient's discharge plan to determine his method of discharge.
· The assistive services worker transports the patient from the department using a wheelchair or trolley according to the patient’s need until the patient is discharged.
Responsible for implementation:
· Doctor - nursing staff - service worker.
Models:
· Exit form - Transfer form.
The Reviewer :
· Egyptian accreditation standards approved 2013.
· Regulations and governing laws.
Hospital medical emergency response policy
Policy: The hospital is committed to responding to medical emergencies.
Purpose: Preparing departments to deal with emergency situations that require emergency dealing, while developing a system to respond to calls for emergency cases.
Procedures:
· The nursing supervisor for each floor prepares an emergency vehicle with life-saving medications and tools according to the attached list that specifies the components and arrangement of the emergency vehicle, provided that the vehicle is close and available for use 24 hours a day.
A female supervisor in each role reviews these vehicles daily.
· The hospital’s pharmacists’ department assigns a pharmacist to visit the emergency vehicle and verify its contents and suitability on a daily basis.
· The medications used from the emergency vehicle are replaced immediately after they are used from the emergency cabinet of the department that used them. If these medications are not available in the emergency cabinet of any department, they are replaced from the intensive care emergency cabinet until they are dispensed from the hospital pharmacy.
· The hospital (training officer) is committed to holding training courses on cardiorespiratory resuscitation for all employees (doctors and nurses) in the hospital on a one-day basis every two years. Those who have completed the course are given a certificate stating this, and their direct supervisor is responsible for monitoring the workers’ access to the courses.
· Any hospital employee who suspects a case of cardiac arrest calls the cardiorespiratory resuscitation team by telephone to the intensive care unit and the floor nurse or by the switch to make a call and mention the floor/department and the room number to which you want to move.
· The floor nurse calls the rest of the team if the switch is not available.
· In cases of cardiac arrest that occur in intensive care, the care physician is called and the cardiorespiratory resuscitation team is not requested unless the care physician requests it, and his responsibility is to supervise the patient’s resuscitation.
· Cases of cardiac arrest that occur in operating rooms and units where the patient is supervised by an anesthesiologist. The cardiorespiratory resuscitation team is not called unless the anesthesiologist requests it, and he is responsible for supervising the patient’s resuscitation.
· The first person to reach the patient performs cardiac resuscitation.
· The cardiorespiratory resuscitation team consists of an intensive care physician, a care nurse, in addition to a case doctor, a floor/department or room nurse, and a security personnel (according to the established schedule).
· It is the responsibility of the nurse to bring the emergency vehicle for the role in which the cardiac arrest occurred.
· The team leader is the intensive care physician who is responsible for administering electric shocks, obtaining a clear airway and breathing, and participating in cardiac resuscitation.
· The case doctor is responsible for explaining the medical condition, reviewing the patient’s files, and informing the team leader of any information he needs. He also participates in the work of cardiac resuscitation. He is responsible for communicating with the patient’s family, informing them of developments in the patient’s condition, and involving them in any medical decision that requires their participation.
· The intensive care nurse is responsible for giving medications and taking samples requested by the team leader and assisting the rest of the team members according to the team leader’s instructions.
· The floor/department nurse is responsible for recording the events of cardiac arrest, the dates for giving medications, the shape of the heartbeat, and the time the heart returns to beating on the form designated for that. She is also responsible for giving breathing to the patient in the manner determined by the team leader.
· The security personnel provides the appropriate atmosphere for the team’s work and is present when informing the patient’s family of any developments in his condition.
· We must work to provide care places on an ongoing basis in order to receive post-cardiac arrest cases that may occur in the hospital floors, after first aid has been provided in the internal department and his condition has been stabilized.
· The medical team in the care is trained to respond quickly and immediately when called upon, and all members of the medical team must be present in the room where the emergency is and deal with the case in accordance with the cardiorespiratory resuscitation policy.
· The call system is tested suddenly by the unit director/quality coordinator in the hospital to ensure that doctors and nurses respond to the call and the time between the call and the response is calculated as a form of performance evaluation within the unit, with the results being submitted to the quality coordinator in the hospital.
· Cardiorespiratory resuscitation is performed according to the attached protocol.
· All hospital employees are trained to deal with cardiac arrest cases (basic level), while care and anesthesia doctors are trained at the advanced level.
Administrator:
· All hospital staff - CPR team.
Models:
Table of contents and arrangement of the emergency vehicle
Monthly CPR team schedule
Cardiorespiratory resuscitation protocol
The Reviewer:
Egyptian quality standards 2013.
Cardiorespiratory resuscitation protocol
Health education policy for patients and their families
Policy: Providing health education to patients visiting the hospital and their families ensures that patients are provided with important information that will help them recover and protect them from diseases when they enter the hospital, during their stay in the hospital, and after discharge. This is evident in the hospital’s commitment to educating the patient and his family regarding the following:
· Pathological diagnosis of the patient.
· Tests, diagnostic examinations and treatment.
· Use of medications and possible side effects.
· Nutrition.
· Interactions between food and medicine.
· Physical therapy and rehabilitation.
· Special information on how to reduce the risk of diseases through nutrition.
· The harms of smoking and the necessity of staying away from active and passive smoking.
· Exercise and health-related behaviors.
· The relationship between the patient and society.
· Exit and follow-up instructions.
Purpose: Improving health care outcomes by educating the patient and his family to aid in recovery and upholding the value of healthy behavior by providing health information about the various medical specialties necessary for the patient.
Procedures:
· According to Professional Ethics Regulation No. 238 of 2003, health education for patients and their families is considered one of the duties and responsibilities of the doctor and the medical team.
· The treating physician and the responsible nurse use a special record/form to educate patients and their families.
· The treating physician, the responsible nurse, and the patient’s medical service provider evaluate the patient’s educational level and determine the educational needs upon admission.
· Any department participating in the educational seminars records its own seminar with its signature and date in the patient educational record
· If abbreviations are used, an explanation is provided for each abbreviation to clarify the information.
· The treating physician and the responsible nurse ensure that the patients’ educational record includes the type of information provided to the patient, to whom the information was provided, the extent of the response of the patient or his family, and a summary of the educational session that was conducted for the patient.
· The treating physician and the responsible nurse ensure that the forms for the departments participating in the educational seminars are placed in the patients’ educational record.
· The treating physician and the responsible nurse make sure that the patient’s questions are given the opportunity.
· The treating physician and the responsible nurse ensure that the patient understands the discharge instructions and follow-up steps, and this is recorded in the patient’s file.
· The hospital provides a special place to receive educational seminars for patients in the internal departments and outpatient clinics.
· The hospital is committed to developing a unified educational material for chronic diseases/dialysis patients.
Administrator:
· The treating physician - nursing staff - medical service provider from any department involved in patient education
Models:
· Patient and family education model
The Reviewer :
· Professional Ethics Regulations - Egyptian Quality Standards 2013.
|
|
|
- Unexpected events policies
Incident reporting policy
Policy: A policy that explains the system for reporting near misses/incidents that enable employees to report them in order to help in continuous improvement of performance.
Purpose: To provide an organized mechanism in the hospital to identify problems that lead to negative outcomes for patients, visitors, or employees in order to detect them early and prevent them from occurring.
Definitions:
· Near miss: An unplanned event with the potential to cause harm that was intercepted in time or by chance resulting in no harm to the person.
· Incident/accident: Any incident that occurs in the hospital (that does not represent routine patient care) that negatively affects or has the potential to affect the health or lives of patients, visitors, or hospital workers.
Procedures
General procedures:
· The report must be written and completed by the person who discovered the accident or the person involved in this accident.
· The report must be written immediately after discovering the incident and submitted to the Quality Coordinator no later than 48 hours.
· The quality coordinator presents the report to the head of the relevant department and the hospital director to take corrective measures.
· Confidentiality must be observed in dealing with or maintaining these reports, while restricting access to them to persons with authority to do so.
· Do not use the information in this report as a means of taking disciplinary action against anyone.
· These reports should generally be discussed at Quality Committee and Medical Board meetings for educational purposes or to establish regulations limiting their occurrence.
Items that make up the report
· Information about the infected person and the department he is in.
· The type of incident/unexpected event that has significance.
· Information about the near miss/accident/unexpected event that has significance.
· Description of the incident, indicating any action taken immediately after the discovery and the factors that led to this incident.
· Corrective actions taken.
· Data of the person who discovered the incident/unexpected event that has significance. Filling out this part is not mandatory.
· The department head verified the report.
· Instructions from the hospital director.
People responsible for writing the report
· All hospital employees, including doctors, nurses, pharmacists, chemists, radiology technicians, and non-medical service personnel.
Corrective action plan and assigned responsibilities in the event of unforeseen accidents:
· After the report reaches the hospital’s quality coordinator (within 48 hours of the incident), he reviews it and returns to the head of the department in which the incident occurred and the person or persons who discovered the incident to find out the reasons that led to the incident. This is done within 48 hours of the report reaching the quality coordinator.
· The quality coordinator (or his designee from the quality team) classifies this incident as (specific to environmental safety - specific to medications - specific to patient safety and security)
· The Quality Coordinator (or his designee from the Quality Team) refers to (the Environmental Safety Officer - the Pharmacy Manager - the Patient Safety and Security Officer) according to the classification of the incident to make recommendations with the Quality Coordinator (or his designee from the Quality Team) so that this incident does not occur again. Other.
· After making the necessary recommendations to avoid this incident from occurring, a corrective plan will be developed to implement these recommendations by the quality coordinator and the responsible person according to the classification of the incident and the head of the department in which the incident occurred.
· The corrective plan includes recommendations, who is responsible for implementing each recommendation, the time frame for implementation, and the required resources.
· The quality coordinator (or his designated member of the quality team) follows up on the implementation of the established corrective plan and submits a report on it for discussion at the quality committee meeting.
Responsibilities
The employee who discovered the accident:
· Rapid intervention to protect or support the patient’s health condition.
· Immediately inform the existing doctor
· Writing the report before the end of the shift.
The doctor who was informed of the accident
· Recording the results of the medical examination and the required medical care.
Hospital manager
· Review the condition and ensure that corrective actions have been implemented and provide any assistance required.
Quality coordinator
· Monitor all reports and ensure that all important steps to resolve the problem have been completed.
· Writing a monthly summary of all reports.
· Writing a quarterly report to the Quality Committee for discussion.
· Maintain a file of all reports for three years.
Occupational safety and health officer
· Examine all reports related to occupational safety and health to review safety-related incidents.
· Forming a team from the Occupational Safety and Health Committee to review safety-related incidents.
· Recording the results of the inspection and the corrective actions taken in the report.
· Return the completed report to the Quality Coordinator.
· Writing a monthly summary and presenting it to the Occupational Safety and Health Committee.
Responsible for implementation:
· The employee who discovered the accident.
· The doctor who was notified.
· Head of Department .
· Hospital manager .
· Quality coordinator.
· Occupational safety and health officer.
The Reviewer
· Egyptian Accreditation Standards 2013- Regulating laws and regulations
Models
· Incident report form
Attachments
· Accidents and near misses that must be reported to the hospital.
|
|
|
|
|
|
|
|
A list of facts that can be reported
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
· Patient escape
· The patient’s suicide, suicide attempt, and violence.
· Unexpected mortality and complications, including those resulting from institution-acquired infections.
· Confirmed blood transfusion reactions (except for routine adverse reactions such as chills and fever).
· Significant events in anesthesia and pain relief that caused harm to the patient.
· Significant differences between preoperative diagnosis and postoperative diagnosis, including surgical pathology findings.
· Significant adverse drug reactions that caused harm to the patient.
Significant medication errors that caused harm to the patient, such as:
◾ Giving the wrong medication.
◾ Giving the wrong dose.
◾ Giving the medicine incorrectly.
◾ Giving medication to an incorrect patient.
Related to operations:
◾ Cancel the operation.
◾ Unexpected removal of any organ.
◾ Wrong patient.
◾ Incorrect counting of tools.
◾ Cases of error in the operation (patient - operating party - procedure).
◾ Leaving a foreign body in the patient.
Laboratory related:
◾ Incorrect data in the sample.
◾ His eye is wrong.
◾ Improper storage.
◾ Incorrect laboratory results.
Related to the hospital:
◾ A visitor was injured.
◾ Bed sores.
◾ Wrong needle injury.
Security neutrality:
◾ Theft or loss of personal property.
◾ A fight with a visitor or patient.
◾ Not following hospital policies.
◾ Suicide attempt.
Fire and safety:
◾ Fire.
◾ Spillage of a chemical.
◾ Blockage of one of the emergency exits.
◾ Expired fire extinguisher.
◾ Gas leak.
◾ Water leakage.
◾ Unsafe electrical wires.
· Serious physical or psychological harm to a patient, employee, or visitor (nerve damage - loss of a limb or organ - death).
|
|
|
|
|
|
|
|
Significant Error/Accident/Unexpected Event Report Form
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|||
|
|
|||
|
|
|
||
|
|
|
||
|
|
|||
|
|
|||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
Intensive analysis policy when unexpected events occur
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The existence of standards and processes for intensive analysis of significant and undesirable unexpected events.
Purpose : To increase public knowledge about events, their causes, and strategies to prevent them, focus the hospital's attention on understanding the reasons behind the event, and change hospital systems and processes in order to reduce the likelihood of such an event occurring in the future.
Definitions
◾ A significant unanticipated event is any unexpected event in health care that results in death or serious physical or psychological injury to a patient.
Procedures:
◾ A report is written about the occurrence of the event as in the policy.
◾ The quality coordinator selects a team consisting of people close to this event and a member of the hospital’s quality team to analyze the reasons and determine the basic factors behind the occurrence of this event, provided that this is done within a month of the formation of the team.
◾ Analysis identifies changes that could be made in systems and processes (either through redesign or development of new systems or processes) that would reduce the risk of such events in the future.
The analysis must be accurate, documented, and comprehensive, including the following:
◾ Identify the human factors and other things that are directly related to the event and the processes and systems relevant to its occurrence.
◾ Analyze basic systems and processes through a series of questions.
◾ Identify risks and their potential contributions to this type of event.
◾ Identify potential improvement in processes or systems that would lead to a reduction in the likelihood of such events occurring in the future.
◾ After identifying the root causes, the team will develop a corrective plan to avoid these causes in the future, provided that the time frame for implementing this plan does not exceed three months.
Time frame :
◾ The root causes must be analyzed and a corrective plan must be developed within a month of the event occurring.
◾ The corrective plan must be implemented within a period not exceeding three months.
◾ The root cause analysis and the implementation of the corrective plan are reviewed by the hospital’s Quality Committee.
Responsible for implementation:
Quality Committee
work team
Persons responsible for implementing the plan
The Reviewer
Egyptian Accreditation Standards 2013.
Regulating laws and regulations.
Models
Incident report form
|
|
|
|
|
|
|
|
- Patient rights policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: The hospital provides multiple medical services, and the hospital administration, doctors, and staff are committed to performance that preserves patients’ rights while informing them of them from the time they enter and while performing the various services until they leave, in compliance with the hospital’s mission and fulfilling the patient’s health care needs.
Purpose: Preserving the rights of patients and their families.
Working procedures:
· The hospital is committed to all regulations and laws issued by the Ministry of Health and the Federation of Medical Professions Syndicates regarding the rights of patients and their families, as stated in the Professional Ethics Regulations issued by Minister of Health Resolution No. 238 of 2003, as well as Ministerial Resolution No. 186 of 2001. Accordingly, the hospital takes the following policies:
· The right to receive care if it is available in the hospital.
· The right to know the name of the treating physician, supervising physician and/or responsible physician
· The right to receive care that respects the patient’s personal values and beliefs.
· The right to know about and participate in making decisions regarding their care.
· The right to refuse or not continue treatment: The doctor must do the following:
· The right to security, personal privacy, confidentiality and dignity. The patient has the right to have the following.
· The right to receive appropriate treatment for pain
· The right to file a complaint or suggestion without fear of persecution
· The right to know the prices of services and procedures.
First: An explanation of the patient’s rights clauses:
· Rights determined by regulations and laws:
· The presence of a professional ethics regulation, Resolution 238 of 2003, in the hospital administration and with the quality coordinator as a reference in training on patients’ rights. The regulation includes the following points:
· Part One: Doctors’ Oath
· Part Two: The doctor’s duties towards
· the society.
· Occupation.
· The patients.
· Colleagues.
Third: Medical interventions of a special nature
· Gender correction procedure.
· Assisted fertilization operations..
· Resection and transfer of human organs and tissues
Chapter Four: Conducting medical experiments and research on humans
A copy of Resolution No. 186 of 2001 from the hospital emergency director, which includes the following:
· Informing the patient about the cost of surgical operations at all stages.
· It is prohibited to detain an inmate's body or exploit a death to gain financial advantage.
A copy of Prime Minister’s Decision No. 1063 of 2014 at the hospital’s emergency director, which includes the following:
· All medical facilities are committed to providing treatment services for emergency and accident cases free of charge for a period of 48 hours, after which the patient has the choice of staying at his own expense or being treated in the free section of the hospital, provided that the state bears the costs from the treatment budget at the state’s expense.
· The right to obtain care if it is available in the hospital in order to ensure the hospital’s ability to provide the necessary medical care to the patient. This depends on obtaining information about the patient’s needs and condition through a screening and selection process by the medical team that is carried out by:
· Assess the patient’s medical history.
· Physical examination.
· Previous assessments and examinations with the patient……etc
· The medical team provides medical care to the patient after obtaining the results of the medical examination and necessary tests as long as the service the patient needs is available and a bed is available for this patient in the hospital.
This is usually done at the first point of contact:
· When the patient arrives at the hospital.
· During ambulance transport.
· Before transferring from another location.
· The right to know the name of the treating physician, supervising physician and/or responsible physician.
· This is done by the doctor introducing himself to the patient before dealing with him.
· An identification card placed by the doctor containing the name, specialty, a personal photo, and the name of the hospital
· Doctors wear a white coat, blue or green suit.
· Putting the names of doctors and their specialties on the door of each clinic.
|
|
|
|
|
|
|
|
Patient responsibilities policy towards the hospital
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
- Patient security and safety policies
Correct patient identification policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Identifying the patient using two means before giving him treatment: blood or one of its derivatives, taking samples from the patient, or any diagnostic or therapeutic procedure.
The Purpose:
Achieving patient safety and reducing the risks that the patient may be exposed to during any procedure within the hospital.
Working procedures:
1- Everyone from the health team who deals with the patient must include:
· Doctors.
· Nursing.
· Pharmacists.
· Lab. Technician.
· Ray technician.
· Physiotherapist.
Use at least two means of identification for the patient to verify his identity:
· The name is fourfold.
· File No.
· The nurse ensures that the identification bracelet data is correct before placing it on the right arm by matching it with the patient’s data and ensuring that it is legible and clear. If it is not possible to place the bracelet on the right arm for any reason, such as the presence of a cast, it is placed on the left arm.
· The charge nurse will place a new bracelet if the original is lost or becomes illegible.
· The nurse makes sure the patient’s full name is as it is in the patient’s medical file and does not depend on another name (such as a nickname), and confirms the file number even if she is sure she knows the patient.
2- The patient’s identity is verified before every interaction with him, such as:
Ø Giving treatment.
Ø Transfusion of blood or one of its derivatives.
Ø Taking a blood sample or any other samples necessary for medical analysis and laboratory examination.
Ø Transfer of the patient.
Ø Conducting diagnostic tests.
Ø Or when taking any other actions.
Note:
Do not apply an identification label before taking the sample or on the package when it is empty.
3- When taking any procedures, the nurse asks the patient about his name and introduces the patient herself and the procedure that will be performed, taking into account the presence of the patient’s bracelet and the two means of identification clearly written on it, which are the patient’s name and the file number.
4- The nurse then matches the patient’s data on the bracelet with that in the medical file to confirm the patient’s identity before any procedure is taken.
5- When taking a sample, the laboratory technician or nurse places a label identifying the sample that includes the patient’s name and file number immediately after taking the sample and before leaving the place.
Note:
The laboratory technician performs the same patient identification procedures before withdrawing any sample.
6- In the case of premature infant patients, a bracelet is placed on the child’s right leg.
7- In the case of patients who have disturbed consciousness or are in a coma and for whom there is no way to prove their identity, their identity is proven by the following (anonymous/unknown - patient number - date and hour of admission)
· If it is an accident, a report is prepared to prove the accident.
8- For newborns, they are identified by a bracelet placed on the foot with the following recorded:
· Mother's name
· Male Female
· File No
9- Dialysis patients: They are identified by an enclosed badge with the patient’s name on it
10- Patients in the emergency room or recovery room with the patient’s triple name and reception ticket number
11- Outpatient patients have their test tubes and x-rays identified by the patient’s full name and outpatient ticket number
12- The radiology technician marks the x-rays with the patient’s quadrant name, file number, date, and time
13- None of the hospital employees remove the bracelet of any deceased patient until he leaves the hospital
14- In the event of an error in the patient identification process, reference is made to the incident report requirements policy
Responsible: Medical team
References: - International standards for patient safety.
- Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
Patient delivery and receipt policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
The hospital’s medical team is committed to the process of handing over and receiving patients’ conditions in the various departments, including:
• Identify the necessary duties that must be handled during the delivery and receipt process.
• Determine who is responsible for delivery and receipt.
• Determine how to document the delivery and receipt process.
The Purpose:
The delivery and receipt process is a vital process in order to maintain the safety and security of patients by codifying the exchange of patient information between the medical team while he is in the hospital for the continuity of providing medical care to patients.
Responsible for delivery and receipt:
• Between doctors of the same specialty by using the delivery and receipt model.
• Between doctors with different specialties for patients whose condition requires consultation with doctors from more than one specialty, using the medical consultation form.
• Emergency doctors when transporting the patient to and from hospital departments (patient transfer form).
• Between nursing staff members with each shift change (status book).
• Nursing staff members when transporting a patient to and from operations, care, or to another department (time out form)
Working procedures:
• When a new patient is admitted, the head nurse or her representative receives the patient from the paramedic and the admission or reception office worker, and records all the patient’s data and what the treating physician requested in the patient’s condition record.
• The nurse records the patient’s condition throughout the shift in the patient condition record.
• After the shift ends and the nurse attends the next shift, the nurse delivers to her the conditions of all patients in terms of the development of their medical condition, especially critical cases, surgical cases, treatment given to the patient, any change that has occurred, and any requests such as bringing test results or rumors related to the patient and preparing the patient for operations, if any.... ........etc., with the delivery and receipt documented with the signature of the two nurses in the notebook.
• In cases of operations, the nurse prepares the patient for the operation according to the doctor’s instructions. The nurse hands over the patient and the patient’s pillow to the operating nurse and the patient’s treatment if requested by the doctor in accordance with the patient preparation form for operations and the patient receiving portion of the time-out form.
• After completing the operation, the operating nurse calls the nursing home nurse to come to receive the patient and the patient’s pillow.
• When there is a need to transfer the patient, the nurse transfers the patient and hands over the patient’s file after updating it to the nurse of the department to which the patient is transferred within the hospital.
• Resident doctors receive and receive the patient at the start of the work shift according to the patient handover form, which includes: (patient name - file number - diagnosis - positive medical examination results - positive test results - follow-up and notes).
• When the patient needs to be referred for consultation, the consultation form is used and the required data is recorded according to the form.
Administrator:
• Nursing staff members.
• The doctors.
Models:
• Medical file.
• Record patients’ conditions.
• Consultation form.
• Delivery and receipt form for doctors.
• Operations time-out model.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy to avoid incorrect connection of catheters and tubes
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Specifies the necessary data that must be placed on catheters as well as those responsible for handling them to avoid connection or incorrect use of catheters.
The Purpose:
· Achieving patient safety by avoiding incorrect connections of catheters and tubes in all hospital departments.
Working procedures:
· Patients, their families, or hospital employees do not have the right to disconnect, install, or reinstall any type of tube or catheter, except:
Ø The doctor.
Ø Nurse.
Ø Supervisor.
Informing the patient of this is the responsibility of the nurse in charge of the patient's room.
· The department creates a policy for each type of tubes and catheters in the department, explaining:
o The person responsible for the installation.
o Installation and installation method.
o Ensure the integrity of the installation.
o Follow up and take care of the connection.
· The following information is required to be shown on each catheter: the name of the installer, date and hour.
· Installation and verification of the correct installation of each type is carried out according to its policy.
· The doctor must specify the name and type of tube through which the medication will be administered.
· The nurse must check all connections before giving any medication and before and after performing any procedure in accordance with the policy for each type.
Administrator:
• Nursing staff members.
• the doctors.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Policy to prevent patient falls and take the necessary measures to avoid falls
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy:
Each patient's potential fall risk is assessed upon admission to the hospital including the potential risk associated with the patient's treatment regimen on the form in the nursing assessment portion.
• Necessary measures must be taken to prevent falls.
Purpose:
Preventing patient falls by evaluating and re-evaluating cases regarding the possibility of falling and taking the necessary measures and precautions to prevent this.
The Definition:
Fall:
Any change in the patient's position from one level to a lower level, which leads to the patient touching the ground or any surface at a lower level.
Precautions that must be taken to protect patients from being exposed to the risk of falling:
• Environmental factors
• Identify patients at risk of falling.
• Educating patients at risk of falling and their families.
• Environmental factors:
The hospital/department takes into account the various environmental factors and influences that provide security and safety for the patient and prevent the possibility of him falling. Therefore, the department nurse or her representative periodically ensures that:
• The patient beds are safe and free from any breakage or malfunction.
• The sides of patient beds are safe and there are no defects.
• The patient bed brakes are safe and work efficiently.
• Safety of the trolley used to transport patients between departments.
• Do not move patients while department workers are performing the cleaning process to avoid patients falling during that time.
• Ensure the safety and quality of lighting.
• Ensure that there are no obstacles in the corridors.
• Ensure that the bell in the bathrooms works well.
• Ensure and keep the floors dry and clean so as not to increase the risk of slipping and falling.
1- Identifying patients at risk of falling
The nurse assesses the patient for fall risk according to the items on the nursing assessment form upon admission.
If there is a patient who may be at risk of falling, the nurse should do the following:
• Raise the sides of the bed
• Place the symbol (F) on the patient’s identification bracelet.
• Put the symbol (F) on the door of the patient’s room and/or bed if the room contains more than one patient.
• Repeatedly asking if you want to go to the bathroom.
2- Educating patients at risk of falling and their families through treating doctors and nurses
• Alert the patient to notify the nurse if he feels dizzy, sluggish, unbalanced, etc
• Warning the patient not to resort to sudden movements when changing position from sleeping to standing or sitting.
• Warning the patient not to bend down to pick up anything from the ground.
• Make sure to use comfortable shoes without heels that do not help with slipping.
• Be sure to keep the bell near the patient’s bed.
• The necessity of committing not to leave unwanted objects on the nightstand next to the bed or in the bathroom.
• Alert the patient to request assistance while walking and moving around.
• Do not place any sharp tools near the patient.
• Ease of movement of the medical team, patients and their families in the hospital rooms and rooms by not occupying them with any tools or equipment.
• Encourage the patient to use wall supports while walking to prevent falls, if any.
• Recording health education for patients and their families in the patient’s medical record.
3- If a patient suffers a fall, the following must be followed:
• The nurse measures vital signs before moving or assisting the patient to move or stand.
• When the patient may be injured or fractured, the patient should not be moved at all.
• The nurse notifies the doctor to examine the patient and determine how to lift him.
• The nurse helps the patient and places him in the wheelchair after ensuring that the brakes are lifted to prevent movement.
• The nurse records the falling incident on an incident report form.
• The responsible nurse re-evaluates the patient when there is any change in the condition of the patient who is at risk of falling, provided that she documents any change in condition as follows:
o The full name of the assessing nurse.
o Evaluation date.
o Evaluation hour.
o The new result of the assessment.
List of patients at risk of falling:
• A patient with a disorder in the level of consciousness of all types and causes
• A patient with all types and causes of convulsions.
• A patient with limb fractures.
• Diabetic coma patient.
• A patient with high or low blood pressure.
• Geriatric patient.
• The mentally ill patient, especially if he has suicidal tendencies.
• Patient with imbalance (stroke patient + hemiplegia).
• Pediatric patients.
• Patients treated with sedatives, diuretics and blood pressure lowerers.
Administrator:
• Nursing staff members.
• the doctors.
• Maintenance.
• Environmental safety officer.
References: - International standards for patient safety. - Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
Safe use of restraint and seclusion policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics :
The patient's safety and security are maintained and his right not to be restricted unless there is harm to the patient or those around him
The patient is restrained for the shortest possible time after evaluating the patient and ensuring the necessity of restraint using the least means
The patient is restricted based on the order of the qualified treating physician
Purpose: To preserve the patient’s rights and dignity and prevent him from harming himself or others.
Restraint: is a means that reduces or prevents the patient's movement. There are two types:
Either physical: This is a method of restraining the patient by the hands, feet, and torso of the body.
Or medicinal: It is a medication given with the aim of reducing the patient’s movement and calming his behavior.
Isolation: This is the restriction of the patient’s residence in a special room or area in cases of violence and aggressive behavior by the patient towards himself or those around him, including workers, patients, and others.
Reasons for restriction:
· A patient who suffers from psychological disorders that make him capable of harming himself or those around him.
· A neurological patient who suffers from a cerebral shock and in the event of agitation makes him unable to move unconsciously and capable of harming himself and others.
· The post-operative patient is agitated, leading to harm to himself and others.
· A liver patient who suffers from a state before hepatic coma and is agitated.
· The patient is conscious but has a history of harming himself before or removing the devices installed on him, such as the monitor - the central vein - or injection and pumping devices.
Reasons for isolation: The patient with behavioral diseases is isolated in a room alone until he is transferred to another hospital and the patient’s family is informed.
Procedures :
First: Patient evaluation:
The charge nurse determines the patient's need for restraint based on his behavior
The treating physician records the restriction order in the patient’s medical file, explaining the following:
⭕ The reason for the restriction
⭕ Type of registration required
⭕ The time of giving the restriction order/the specific period of restriction
Restriction started:
Registration is performed using the fastest available method, whether pharmaceutical or physical, except after consulting a consultant. However, in some cases it is prohibited to use the pharmaceutical method.
Restriction method:
The nurse uses a leather belt, gauze and cotton ties, or other means to restrain parts of the body. The four limbs are often used for restraint, except in cases such as meal times and personal hygiene.
Female: The charge nurse wraps the legs together and then ties them to the foot of the bed.
Male: The nurse in charge binds each patient's leg individually to the foot of the bed.
The treating physician shall sign the verbal registration order within 24 hours from the time he is notified of the case.
The nurse takes care not to harm the patient psychologically or physically during the restraint.
The nurse takes care to maintain the patient's privacy.
Patients whose freedom is legally restricted. The doctor is prohibited from participating in restricting them except when there is a strict medical necessity (Article 35 of Professional Ethics - Resolution 238 of 2003)
Second: Patient follow-up:
The nurse records the patient's follow-up using the relevant form and includes the following data:
⭕ Patient behaviors - Vital signs - Blood circulation - Skin condition
The responsible nurse follows up on the patient under restraint for medical and surgical reasons at least every two hours, and this is documented in the patient’s medical file.
The nurse follows up on the patient who is under restraint for psychological reasons at least every half hour, and the observations are recorded in the patient’s medical file on the patient restraint form .
Third: Renewal of the restriction order:
Restraining orders made for medical and surgical reasons must be renewed by the treating physician at least every 24 hours based on continued need.
Restraining orders made for psychological reasons must be renewed by the treating physician at least every 6 hours based on continued need.
Fourth: Ending the restriction:
Specifications for ending the restriction: It is either the patient’s state of consciousness completely improves or it deteriorates and a coma occurs.
The trained nurse ends the patient's restraint in accordance with the doctor's orders, according to the patient's condition and according to medical evidence, provided that the time and date of ending the restraint are recorded.
Fifth: Training:
The patient care policy officer in the hospital provides practical training to the doctors and nurses in the internal care department on how to implement the policy.
Sixth: Health education for the patient and his family:
The doctor/responsible nurse introduces the patient and his family to the following:
⭕ The extent to which the patient needs to be restrained
⭕ Duration of restriction
⭕ Rating rate during restriction
Responsible: The treating physician
Forms: Restraint and Prosecution Order Form
References: Egyptian Quality Standards 2013 - Joint Commission International Standards 2014
|
|
|
|
|
|
|
|
Policy to prevent bed sores while the patient is in the hospital
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: Evaluate patients most at risk of developing bed sores and take measures to prevent them.
Purpose: To achieve patient safety in the hospital by preventing the occurrence of bed sores.
Working procedures:
• The nurse evaluates the skin condition of each patient upon admission to the hospital on the relevant form in the nursing assessment part.
• Patients who are confined to bed must be re-evaluated by the nurse in charge at the beginning of each shift. Only in the case of patients who are unable to move, the department nurse should do the following to prevent the occurrence of bed sores:
o Make a plan to turn the patient every two hours on the patient turn over form and attach the form to the medical record.
o The skin is massaged to stimulate the patient’s blood circulation, especially the areas with great prominence, to avoid bed sores, and this massage and its time are recorded in the medical record.
o Observing the patient’s skin to discover any area of the skin that shows redness and recording this in the medical record.
o Furnishing patients’ beds in the correct way and avoiding any folds in the bed sheets to avoid the occurrence of bed sores.
o Place an air mattress for the patient - if possible - to reduce and prevent the occurrence of bedsores.
o Pay attention to the degree of softness and dryness of the skin and use creams and moisturizers to avoid dryness.
o Taking care of the skin by giving the patient a full bath daily and when needed.
o Therapeutic nutrition that suits the patient according to his health condition, based on the doctor’s orders, to stimulate the body’s tissues and prevent the occurrence of bed sores.
• If the patient has bed sores, the following is done:
o All of the above is done to avoid increasing the area of bed sores.
o The treating physician makes sure to move the patient according to his condition.
Administrator:
• The doctors.
• Nursing staff members.
Models:
• Patient turning model.
• Degrees of bedsores.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards 2013.
|
|
|
|
|
|
|
|
Critical outcomes policy
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
The policy states the following:
· Definition of critically significant results.
· When to report critically significant results.
· How to report critically significant results.
· Who reports critically significant results.
Who receives the notification of critical findings?
· Document reporting of critically significant findings.
Purpose: To maintain the safety and security of the patient and take appropriate action when there are critically significant results that require rapid intervention by the treating physician or any member of the medical team.
Definition: Panic Values: These are results that may indicate the presence of a life-threatening situation for the patient that requires an urgent response or rapid intervention by the treating physician.
Working procedures:
1- Each department develops a list of its critical results, which includes the following:
· Results of critical laboratory tests (laboratory).
· Results of critical diagnostic examinations (Radiology Department).
· Critical medical examination results (internal departments / care / dialysis...).
2- In the event of any result of critical significance according to the previous lists, the person in charge (laboratory physician/radiologist/resident physician/responsible nurse/laboratory or radiology technician) shall immediately inform the treating physician or the department nurse.
3- The informant must verify the full name of the person who was notified.
4- The recipient of the report (the treating physician) - (the nurse) shall do:
· Record the critical result immediately in the critical results log.
· The recipient of the report re-reads the patient’s data and the test result on the informant, with the aim of ensuring that everything that was received and recorded in the patient’s file is correct and accurate.
· The treating physician has the right to accept or reject the result in light of its proportionality to the patient’s condition, which may require a re-examination or procedure from the informant.
5- Document the reporting process through the following:
· The recipient (the treating physician) - (the nurse in charge) documents the following data in the critical findings record immediately upon receiving the report:
(Today's date - Reporting time (hour and minute) - Test result).
The action taken in terms of accepting or rejecting the result or requesting a re-examination.
(The full name of the laboratory/radiology official who reported - the full name of the recipient of the report (doctor - nurse))
Administrator:
• Laboratory and radiology doctors.
• Resident doctors.
• Nursing staff.
• Physician.
Models:
• List of critical results for each section.
• Critical results model.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards.
|
|
|
|
|
|
|
|
Model of findings with serious clinical implications
The number :........................
|
|
|||
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
|
|
|
|
|
|||||
- Specific standards for medicines
Policy for handling high-risk medications (including concentrated solutions)
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
· Identify high-risk medications by scientific names, collect them in a separate list, distribute them to all medical service providers, and deal with the medications included in the aforementioned list correctly in accordance with the instructions for each preparation to ensure that the patient is not exposed to any therapeutic risks as a result of the incorrect use of concentrated solutions without diluting them.
The purpose:
· Ensuring that high-risk medications are handled with due care in order to ensure that the patient’s health is not exposed to any therapeutic risks.
identification:
· Dangerous medicines are medicines that cause serious danger to the patient when used incorrectly. Therefore, a list is prepared for them that explains what these dangerous medicines are that must be handled with care to avoid any error in their use.
o Work procedures:
· The pharmacy director, with the help of hospital pharmacists, prepares a list of dangerous medicines and solutions with high concentrations, specifying the scientific name and instructions for dilution, administration, and observation.
· The pharmacy manager distributes the list to all therapeutic departments and units in the hospital.
· These medications are not placed in regular departments, and their presence is limited to hot areas, such as (care, operations, emergency, and kidney departments), and their presence is limited to departments inside the emergency vehicle.
· When using these medications, check with the doctor first and then do a double review by two nurses before giving them.
· When preparing these medications, it should be in a place with good lighting and away from any noise or interruptions.
· When storing these medicines, a red sticker is placed on the box containing these medicines, and it is in a separate place from the regular medicines, provided that this sticker contains the following information: -
- The scientific name of the drug
- The focus
- Pharmaceutical form
- Expiration date
· When dispensing these medications, the pharmacist places a red mark on each ampoule or bottle. In the event that the pharmacist dispenses large quantities, the nurse can be instructed to place this mark on each unit.
· When placing medications that are similar in pronunciation or shape, or both, the containers should be separated and not placed next to each other, in addition to writing clear addresses on the containers.
· A medication reference is placed in each section that includes (the use of each medication - how to administer it - doses - side effects - standards that must be followed regarding use and preparation).
· When giving anticoagulants, the treating physician does the following:
o Use protocols detailing the initiation and continuation of anticoagulant therapy and the tests required for follow-up.
o Documentation of the pre-treatment and current INR in the medical record.
o When anticoagulants are given, doses are linked to laboratory results.
o Use a pump if continuous intravenous heparin is given.
o Health education for the medical team, the patient and his family regarding:
(The importance of follow-up - adherence - drug and food interactions - negative reactions).
· When giving narcotic medications, the pain is evaluated by the doctor and the necessary measures are taken in the event of severe pain.
o Responsible:
· Pharmacists
· The doctors
· Nursing staff
Models:
· List of high-risk medications
The Reviewer:
• International standards for patient safety.
• Egyptian Accreditation Standards 2013.
|
|
|
|
|
|
|
|
List of high-risk medications
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
High Risk Medications
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
21 |
These medications have a high risk of misuse, so they must be handled with extreme caution
|
|
|
|
|
|
|
|
The policy of obtaining a list of the treatment that the patient takes upon admission to the hospital and upon discharge
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Politics:
· Obtaining a list of the patient’s current treatment so that it is complete and documented at the beginning of the patient’s admission to the hospital.
· Giving the patient a list of all his treatment, explaining how to use it, upon his discharge from the hospital.
The Purpose:
· Achieving the patient’s safety while he is in the hospital by committing to the patient’s access to the current treatment list so that the patient does not stop taking the medication, which may lead to his health condition being affected or the surgical operation for which he was admitted to the hospital being postponed.
· Achieving the safety of the patient when he is discharged from the hospital or transferred to another place by giving the patient a list of his treatment so that he does not stop and his health condition is not affected.
The Definition:
· The doctor checks the patient’s current treatment upon admission.
Work procedures upon entry:
· The doctor assesses the patient upon admission, asks him about the medications he is taking at home, and records this on the patient’s medical history form.
· The doctor performs a medical evaluation of the patient based on the results of x-rays, medical tests, and the patient’s current treatment.
· Based on the doctor’s findings from the aforementioned examination and evaluation, he develops a treatment plan, taking into account the patient’s current medications to ensure continuity of health care, taking into account writing in Arabic and not using unknown or known abbreviations.
· The Pharmacy Department publishes a list of abbreviations that should not be used in writing medications, provided that it is reviewed every two years to add or delete any abbreviation.
Work procedures upon exit:
· The doctor provides a comprehensive explanation to the patient about the health condition upon discharge in a clear, simple and understandable way.
· The doctor writes the patient’s discharge treatment in the medical record, follow-up card, and discharge summary with an explanation of the treatment to the patient.
· The department nurse delivers the follow-up card and discharge summary to the patient.
· When the patient is transferred/transferred to another hospital, the treatment carried out in the hospital is written on the external transfer/referral form and the discharge summary.
Administrator :
· The doctors.
· Nursing staff.
· Pharmacy.
Models:
· A list of abbreviations that should not be used in writing medications
· Discharge summary.
· External transfer/referral model.
The Reviewer:
· International standards for patient safety.
· Egyptian Accreditation Standards 2013.
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: Separate medications that are similar in appearance and pronunciation to reduce risks.
Purpose: To achieve patient safety while in the hospital by adhering to the system of separating medications that are similar in form and pronunciation.
Working procedures:
• The pharmacy prepares a list of medications that are similar in appearance and pronunciation, and it is responsible for renewing and updating this list every 6-12 months.
• The pharmacy director distributes the list to all therapeutic departments and units in the hospital.
• The pharmacist separates them and writes clear addresses on the containers containing each one in storage areas.
• Medications that are similar in appearance and pronunciation are highlighted in green.
• When dispensing medications that are similar in form and pronunciation, the pharmacist alerts those who will receive the medication from the pharmacy of the need to separate them for the safety of the patient.
• Nursing supervisors in departments and roles separate and write clear addresses on the containers containing each of them in storage areas.
Administrator:
• Pharmacists.
• Nursing staff.
Models:
• List of medications that are similar in name and pronunciation.
The Reviewer:
• International standards for patient safety.
• Egyptian accreditation standards 2013.
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Medicines that are similar in appearance and pronunciation
|
|
DRUG names |
Serial |
|
Ampol |
|
1 |
|
Ampol |
|
2 |
|
Ampol |
|
3 |
|
Ampol |
|
4 |
|
Ampol |
|
5 |
|
Ampol |
|
6 |
|
Ampol |
|
7 |
|
Ampol |
|
8 |
|
Ampol |
|
9 |
|
Vial |
|
10 |
|
Vial |
|
11 |
|
Vial |
|
12 |
|
Tape |
|
13 |
|
|
|
14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
A list of abbreviations that should not be used in writing medications
· U/ UI
· Q.D, QD, q.d, qd
· Q.O.D, QOD, q.o.d, qod
· MS, MSO4
· Mg SO4
· Trailing zero
· No leading zero
· Dose x frequency x duration
· › greater than
· ‹ less than
· Abbreviation of drugs names
· cc
· µg
- Standards for surgical operations
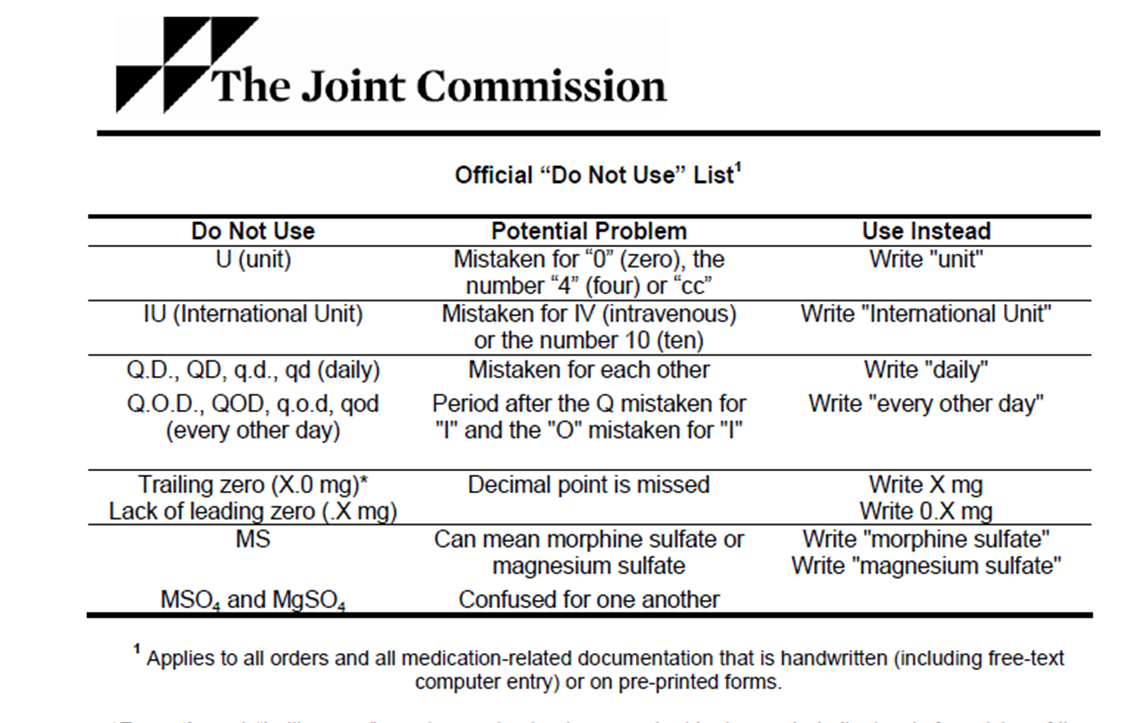
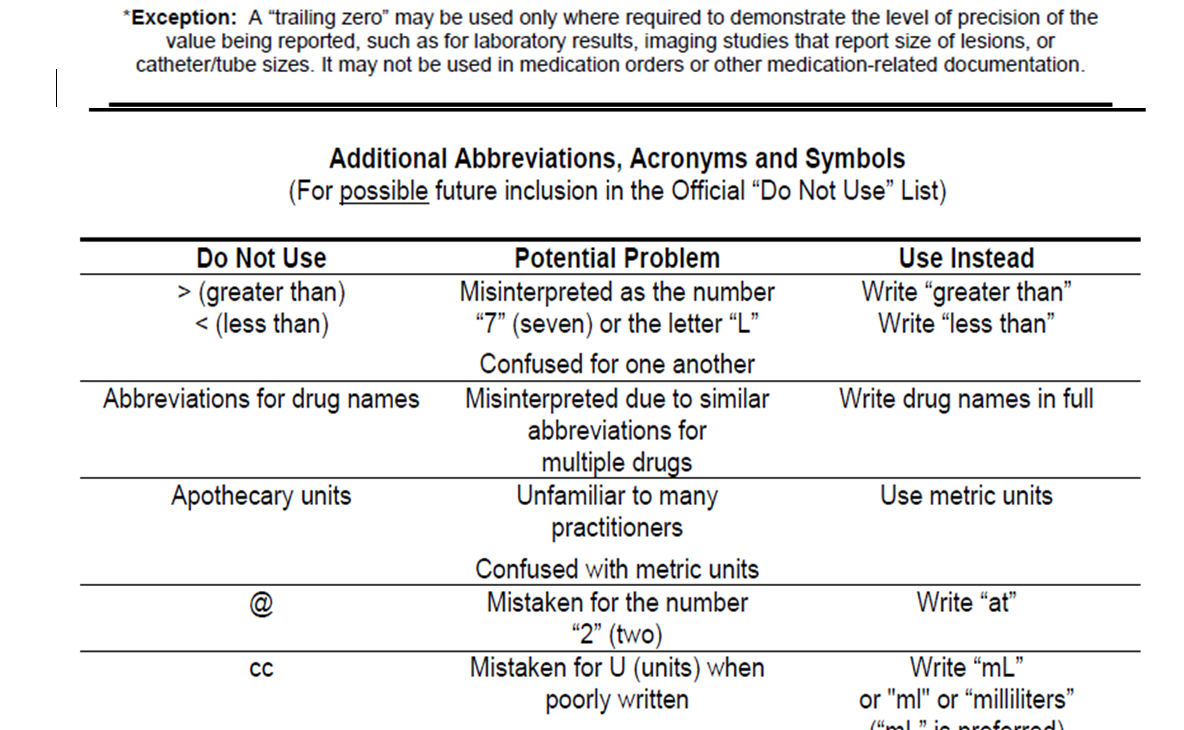
|
|
|
|
|
|
|
|
A policy of accurate and documented identification of the patient before the operation and also immediately before the start of the surgery
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: Use a documented method to ensure the correct patient, correct procedure, and correct part before beginning a procedure or other interventional procedure.
Purpose: To achieve patient safety by ensuring the correct patient and the correct location for surgical or other interventions.
Working procedures:
1. The nurse responsible for receiving the patient for operations receives the patient’s medical record and verifies the patient’s basic data.
2. The nurse asks the patient about his name, matches what is written on the identification bracelet to his file, asks the patient about the procedure required of him, and determines the location of the prescription for the procedure.
3. The nurse matches the patient’s information with what is recorded in the medical record and for the six procedures she performs (operations, endoscopy, interventional radiology, etc.).
4. The surgeon, anesthesiologist, and operation nurse ask the patient about his name, the operation, and the location of the interventional procedure (operations, x-rays, endoscopy, etc.) before anesthetizing the patient on the operating table.
Responsible: Doctors and nursing staff.
Models: Safe Surgery Model.
References: International standard precautions for patient safety.
|
|
|
|
|
|
|
|
The policy of ensuring all documents and equipment necessary to perform the surgery
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: Use a checklist to ensure that all documentation and all equipment needed to perform operations and other interventional procedures are available, correct, and working efficiently before starting any of them.
Purpose: To achieve patient safety when undergoing surgery or any other interventional procedure.
Working procedures:
1. The charge nurse obtains a copy of the operating list (for six operations).
2. The responsible nurse ensures the cleanliness of the operating rooms, including the operating room lights, the operating table, and all the room furniture and equipment it contains.
3. The operations supervisor ensures the safety of anesthesia equipment, electric shocks, operating tables, air conditioning, and lighting.
4. The operations supervisor ensures that the machines and various surgical packages are received according to the needs of the patient, and reviews the safety of sterilization for each one separately.
5. The operations supervisor ensures the safety and availability of devices, equipment, and supplies for each operation in the operations list.
6. The operations supervisor ensures that operations times are properly arranged and organized.
7. Check the suction machine to ensure proper operating conditions by the responsible nurse.
8. The operating nurse receives the medical record of the operating patient from the department nurse.
9. The operating nurse and the department nurse examine the patient’s medical record before operations to ensure:
· Patient's name and file number
· Patient preparation model for operations.
· Declarations regarding performing surgical operations and offering anesthesia before operations.
· Patient analysis results.
· Patient's x-ray reports.
· Implementing pre-operative treatment for the patient.
· Matching the previous data with what is listed in the six operations.
10. The department nurse asks the patient about the presence of artificial dentures or loose natural teeth, and about contact lenses.
11. The surgical nurse provides psychological support and rehabilitation to the patient in preparation for the operation.
12. The anesthesiologist, surgeon, and nurse ensure that the patient is identified before administering anesthesia and that the patient knows the name of the surgeon, the type of operation required, and the location of the operation.
13. A hand washing policy is implemented in accordance with infection control policies.
14. The head of operations or the nurse working with the anesthesiologist will ensure the preparations related to anesthesia are: -
· It is forbidden to use any flammable or flammable anesthetic materials or that could lead to an explosion in anesthesia areas.
· Ensure that the ground electrode of all electrical devices is connected properly.
· Only cotton outerwear is used in the anesthesia site.
· Wires, switches, and electrical and electronic tools are checked regularly by the Engineering Department and the Head of Operations for follow-up.
· The anesthesia equipment and devices used in operations are examined by the anesthesiologist who will use the device to ensure its safety.
Administrator:
· Doctors, operations nursing staff, and maintenance and cardiac catheterization department members.
Models:
· Department case record - safe surgery form.
The Reviewer:
· International standard precautions for patient safety.
|
|
|
|
|
|
|
|
The policy of determining the location of surgery before starting it
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||
Policy: Doctors are committed to placing a distinctive sign indicating the location of the surgical intervention in order to preserve the patient’s safety
Purpose: To keep the patient safe by placing the mark to determine the correct surgical intervention site.
Procedures:
1- The surgeon, provided that he is a participant in the operation, determines the location of the surgical intervention by placing a distinctive mark (circle or dash) with a non-removable marker on the location of the operation in the department.
2- The nurse in the department checks the mark before the patient goes to surgery, after asking the patient or indicating with his hands the location of the operation.
3- The operating nurse receives the patient and double-checks the location of the mark in the part to be intervened on.
Administrator :
· The doctors.
· Nursing.
Models:
· Patient preparation form before the operation.
· Safe surgery model.
The Reviewer:
· Patient safety standards according to international quality and health organizations.
|
|
|
|
|
|
|
|
The policy of ensuring an accurate count of the number of pads, needles, and devices before and after the surgical procedure
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Policy: Use a documented method to ensure the correct number of cotton, gauze, abdominal towels, surgical instruments and needles used before or after surgical intervention.
Purpose: To achieve patient safety by protecting him from leaving any foreign body in his body following surgical intervention.
Working procedures:
1. The nurse ensures during operations that the operating theater is free of any cotton, gauze, abdominal towels, tools, and surgical needles used other than those prepared for the current operation.
2. The sterile nurse and the handling nurse, before the surgery begins, count the instruments, bandages, and needles together, loudly, and separate each item in the counting process.
3. This basic count is recorded immediately after the handling nurse takes it on the Instruments, Dressings, and Needles Count form.
4. All instruments, dressings, and needles added to the operating area during surgery are counted by the sterile nurse and the handling nurse and recorded by the handling nurse immediately.
5. The attending nurse during the surgical procedure does the following:-
· Conduct a loud count of all dressings removed from the operating area together with the sterile nurse.
· Separate dressings into units.
· Put the numbered bandages according to their units into sterilization bags.
6. The attending nurse and the sterile nurse in front of the surgeon, before starting to close the peritoneal cavity, count together and out loud the following:-
· All instruments, bandages and needles in the operating area that were counted before surgery and those added during surgery.
· All tools, bandages and needles that are excluded from the operation area
· The handling nurse records the number in the required column 'before peritoneal closure'.
· The attending nurse reports the count results out loud to the surgeon.
7. The sterilizing and handling nurses, before starting to close the skin, count out loud together all the tools that were used after closing the peritoneum and all the items listed in the section of the register for counting tools, bandages, and needles:-
· This final count is recorded by the on-call nurse in the required column marked 'Final Count'.
· The sterile nurse and the on-call nurse write their names in the designated space in the counting register.
8. The difference in counting tools:-
When reporting a discrepancy:
- The surgeon is notified immediately
- A thorough research is conducted as follows:-
o The location of the operation by the surgeon and assistants.
o The sterilized area by the person responsible for sterilization.
o Operating room by the on-call nurse.
When the difference cannot be reconciled:
- The person who discloses this discrepancy completes an accident report for an accident
- An X-ray picture of the operation site is taken before the patient leaves the operating room.
Administrator:
· Doctors and nursing staff
Models:
· Counting list
The Reviewer:
· International standard precautions for patient safety.
|
|
|
|
|
|
|
|
- Specialized policies
· Firefighting
· Fire cooling
· Remove tight objects from a fire victim
· Cover the affected part of the fire
· Dealing with electrical burns
· Dealing with chemical burns
· Nursing care during the surgical incision
· Prosthetic nursing care
· Spare parts for burns
· Water treatment for burn injuries
Firefighter on fire
Used equipments :
Blanket or coat
The Purpose :
Help save the injured person
Steps:
The injured person is thrown on the ground, then a blanket or coat is thrown over him, then he is wrapped in it
Do not use dirt or sand to avoid contaminating the wounds or hindering the cleaning process
Keep the injured person away from the source of the fire
Fire cooling
Used equipments :
Cold water.
The Purpose :
Reducing the risk of injury and complications.
Steps:
Place the affected part in cold water to relieve pain and reduce swelling.
Apply cold water compresses to the affected parts.
Do not apply ice directly to the burned part because it leads to tissue destruction and exposes the injured person to the risk of a rapid drop in body temperature.
Note: -
Cooling the burn helps relieve swelling by draining heat away from the skin.
Remove tight objects
The Definition :
Remove clothing and jewelry that sticks directly to the affected skin
The Reasons :
For ease of handling the affected part and preventing complications
Working team:
Doctor and nurse.
The Purpose :
Reducing the risk of injury and complications.
Steps:
She takes off clothes quickly.
Cool the clothes with cold water if it is difficult to remove them.
Remove the jewelry before swelling occurs.
Cover the affected area from the fire
The Definition:
Place a cover on the affected part.

The Purpose :
· Reducing the risk of injury and complications and preventing contamination.
· Preventing the accumulation of microbes and reducing pain when the wound is exposed to air.
Steps:
· Calms the injured person.
· The wound is covered with a sterile gauze bandage to prevent the accumulation of microbes
· Wrap the gauze bandage comfortably, avoiding pressure on the burned skin.
· Do not apply any greasy materials to the wound.
· Do not open bubbles if they are many so that the body does not lose too many fluids.
Note:
· Do not use thin cotton because it leaves residue on the burned skin, which is difficult to get rid of.
· Bandaging and covering the burned part keeps air away from the burn, reduces pain, and protects the skin from infection.
Dealing with electrical burns
The Definition:
The most dangerous types of burns occur when the body is exposed to a strong electrical current.
Used equipment's :
Electrical insulator, dry and sterile dressing
The Purpose :
Rescue the injured person.
Steps:
1. Protect yourself and stand on an electrically insulated and dry surface.
2. Keep the injured person away from the electrical source that causes the fire.
3. Use a piece of wood to move the electrical cord away from the injured person.
4. Place the injured person in the recovery position.
5. Assess the injured person and determine the depth of the burn.
6. Cover the burn with a dry, sterile bandage.
7. Keeping the injured person warm so that he does not go into shock.
8. Measuring the patient’s vital signs (Z, N, H, T).
9. Perform CPR if necessary.
Dealing with chemical burns
The Definition:
They are burns that occur as a result of exposure to strong acid or strong alkali
Used equipments :
Lukewarm running water
The Purpose :
Rescue the injured person
Steps:
1. Cry from the chemical source which causes burning.
2. Remove all clothing surrounding the site of injury to reduce the risk of the chemical penetrating into the skin and increasing the depth of the skin.
3. Try to find out the type of substance causing the burn so that you can record it immediately.
4. Use large quantities of running water on the burn.
5. Wash with lukewarm water from the nose to flush the chemical away from the face (in case the eye is exposed to a chemical burn).
Nursing care during the incision
The Definition :
It is a longitudinal surgical incision made by the treating physician in the case of surrounding burns.
Places of surgical incision: upper and lower extremities, trunk, neck
Used equipments :
A breathing tube connected to an oxygen source, therapeutic ointments.
The Purpose :
In order to reduce the intense tumor pressure resulting from the injury and to allow blood flow to the affected part.
Steps:
1. Assessing the condition of surrounding burns affecting the extremities, trunk, and neck.
2. Place a breathing tube through the nose and mouth if necessary.
3. Taking a blood sample to measure the percentage of gases in the blood if necessary.
4. A thick layer of medicated ointment should be applied to the wound under the guidance of a doctor.
5. We calculate the amount of blood lost and perform a blood transfusion if necessary.
Prosthetic nursing care
The Definition:
It is a nursing procedure through which dead tissue and the dry layer covering the graft are removed.
The Reasons :
To avoid infection and clean the wound
Used equipments :
Clean glove, sterile glove, saline solution, sterile gauze, peat or surgical scissors
The Purpose :
To avoid infection and clean the wound
Steps:
1. Wash hands well
2. Wear clean gloves
3. We remove old spare parts by continuous washing
4. We throw away the gauntlet and put on a sterile glove
5. We gently remove the Vaseline gauze that is not attached to the graft and then begin to lift it (so as not to harm the graft)
6. Gently wash the patch with a saline solution and a sterile gauze pad.
7. Dead tissue is removed using surgical scissors and scissors
8. We begin to remove the dry layer that covers the patch
9. We note that there are no complications with the graft
10. Cover the injured person well
11. We place non-adhesive gauze on the patch, then place about 12 folds of gauze, then wrap them well to completely cover the affected part.
12. We put the splints on the part that has the graft
13. Raise the part with the patchwork high
14. The gloves are thrown away and the hands are washed
Spare parts for burns
The Definition:
Place a sterile gauze cover over the burn
The Reasons :
Preserving the wound and speeding its healing
Used equipments :
Sterile gauze, therapeutic ointment
The Purpose :
Reducing the evaporation of fluids in the body and reducing temperature loss.
Steps:
1. Cleans the wound.
2. Apply the medicated ointment to a thickness of 1/16 inch.
3. The burn is covered with sterile gauze.
Note:
Do not put cotton swabs because they leave residue on the affected part
Hydrotherapy for burn injuries
the definition
It is a treatment session during which the affected part of the skin is cleaned and the dead part of the burn is removed
Used equipments :
Bathtub, disinfectant, sterile scissors, sterile peat
The Purpose
In order to reduce the severe tumor pressure resulting from the injury
To allow blood flow to the affected part
Helping with healing
Prevent bacterial growth
Steps:
1- The bathtub must be disinfected before and after bathing the infected person.
2- The room must be kept warm and the session should not exceed 30 minutes
3- The expected pain must be explained to the injured person during the session, and he must be prescribed how to overcome it with painkillers
4- The injured person must participate in setting the dates of the session.
5- Gently place the affected part completely inside the bathtub.
6- Gently wash the affected part, taking care to moisturize the dry skin
7- The skin layer is removed using sterile scissors and scissors
8- The hair around the affected part must be removed
9- Simple movement exercises should be performed for the affected part during the treatment session