Part Three
- Nursing care for a heart attack patient
Heart attack
The Definition:
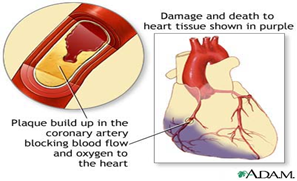
Sudden, severe chest pain resulting from the blockage of one of the coronary arteries, most often by a blood clot, which deprives part of the heart muscle of blood supply, leading to its necrosis and death. The dead tissue may dissolve after a few weeks due to an adherent relationship.
1. A heart attack is the result of a complete, acute and sudden deprivation of the myocardium, or part of it, of blood and oxygen due to the blockage of one of the coronary arteries by a blood clot in most cases. This leads to infarction, necrosis, and death in some of them, to varying degrees in depth and breadth.
The Reasons:
1. The most important cause is the occurrence of a clot in the coronary artery supplying the heart muscle, which reduces the amount of blood reaching the heart muscle.
2. As a result of fatty accumulations that continue to deposit over time on the walls of the coronary arteries.
3. A blood clot dislodges and travels with the bloodstream until it reaches a point in the artery that is too narrow to allow its middle to pass, so it stops there and blocks it.
4. The presence of risk factors that lead to coronary artery disease (age - gender - high blood pressure - cholesterol - sugar).
Signs and symptoms :
Chest pain is not related to effort except rarely (in only about 10% of all cases). It occurs behind the sternum in the middle of the chest, and constitutes severe pressure or crushing, but in terms of its wide spread and extension, it may include the jaws, shoulders, arms, and even the middle of the back, and sometimes the area Stomach.
Duration: It may last hours and sometimes a day or more:
1. Nitroglycerin tablets have no effectiveness or significant effect on the pain of a heart attack, and this is what distinguishes it from the pain of angina pectoris.
2. Stomach upset or indigestion, especially if accompanied by nausea or vomiting.
3. A deep and intense feeling of anxiety, confusion, and fear of the inevitable death of a relative.
4. Changes in the number and regularity of heartbeats.
5. Mild headache - difficulty breathing - low blood pressure accompanied by pain, severe sweating and a feeling of weakness.
6. An increase in temperature between 37.7 and 39. It rises about 24 to 48 hours after the stroke occurs and returns to normal within 6-7 days.
7. Skin color is grey, cool and moist.
Diagnostic methods for myocardial infarction:
1. An increase in cardiac enzymes (cpk), especially MB - cpk, reaching a maximum increase in about 24 hours, LDH.
2. Signs and symptoms.
3. Arteriography and cardiac catheterization are performed, but this is postponed until the patient's condition stabilizes.
4. An increase in the number of white blood cells within a few hours of the onset of pain, reaching 12,000 - 15,000 for a period of 3-7 days.
5. An increase in the erythrocyte sedimentation rate in the first week after the clot occurs, and it remains high for about 7 weeks.
6. Changes in the electrocardiogram: An increase in the ST segment occurs and may last about two weeks, T wave inversion and Q wave.
Analysis of cardiac enzymes:
1. Creatine phosphokinase is specific to the heart only. It begins to rise 2-4 hours after the stroke occurs, reaches its peak after 14-36 hours, and returns to normal after 3 days.
2. Serum glutamic oxalocatic transominase SGOT begins to rise after 8-12 hours, reaches its peak after 18-36 hours, and returns to normal level after 3-5 days.
3. LDH Lastic dehydragenase starts to rise after 8 – 48 hours, reaches its peak after 3 – 6 days, then returns to normal after 4 – 8 days.
Complications of heart attack:
1. High blood pressure as a result of pain or the first signs of heart failure and usually responds to treatment.
2. Complete heart block: Complete blockage of the heart's electricity occurs in about 6% of cases of heart attack. It may occur within a few hours of the stroke occurring in about a third of these patients. This happens to most patients within 48 hours and rarely after 4 days.
3. Cardiogenic shock: occurs in about 5% of cases. Dopamine is usually given in such cases (cardiogenic shock).
4. Heart failure, which is defined as the amount of blood pumped by the heart is insufficient to meet the needs of the heart. It is characterized by fluid retention in the body and swelling in the legs (Oedema).
5. Ventricular dysfunction, which can lead to cardiogenic shock, which is the main cause of death during hospitalization.
6. Some patients may develop a group of symptoms approximately 1-6 weeks after the stroke, which are characterized by pain in the pleural lining, joint pain, and high temperature, as a result of an autoimmune reaction. Aspirin may be effective in this case, and in some cases you need Cortisone.
7. Mitral valve regurgitation.
8. Pericaditis, an inflammation of the lining of the heart that may occur within 24 hours. The pain increases with breathing and may go away when sleeping on the right side.
9. Dysrhythmias are found in about 50% of cases and occur as a result of ischemia or a difference in treatment.
Medical treatment for heart attack:
1. The patient must be admitted to cardiac intensive care, and the following must be done:
A- Connect the patient to the monitor and perform an EKG
B- Delivering oxygen to the patient
C- Installing a cannula and taking blood samples to perform heart enzymes.
D- Giving medications that are used to reduce the size of myocardial infarction resulting from coronary artery thrombosis.
2. Treating pain and providing psychological and nervous balance:
Effective and rapid action to relieve the patient of his pain is considered the first and most important thing, on the one hand, because of the pain itself, and on the other hand, because of the anxiety and disturbance that the patient experiences, which may even lead to the fear of inevitable death. Among the analgesic drugs, we resort to the fastest-acting or most effective drugs, such as morphine and its derivatives, as well as nervous and psychological tranquilizers.
3. Treatment of emergency deficiency in cardiac perfusion:
1. Myocardial infarction is only the result of a severe and complete deficiency in its perfusion and in supplying it with the necessary oxygen for its functioning. Therefore, it is necessary to give the patient oxygen and arterial dilators (nitroglycerin) at regular and close times to dissolve under the tongue, and later, or even at the same time, and permanently, the patient takes moderate arterial dilators. The long-term effect lasts the longest, up to approximately 12 hours.
Tridil is prepared in a 5% glucose bottle, not a plastic packet, because it is deposited on the plastic wall. Tridil is calculated according to the pressure and pulse of the patient’s sense of pain, and Tridil is stopped gradually.
4. Rest in the acute phase of a heart attack:
As soon as the patient arrives in intensive care, the first thing that is done quickly, completely and effectively is in the form of intravenous or subcutaneous injections at regular times and under careful laboratory and laboratory monitoring, such as PTT, which we order and ask of him, is to immediately lie down in bed and have complete and absolute rest, especially in the first days.
5. Thinning or preventing blood clotting:
1. Streptokinase:
It is a medication that is given within the first 6 hours for chest pain resulting from a coronary artery clot. It works to dissolve the clot and thus reduce its effect.
Medications that should be given with and after streptokinase:
1- Hydrocortisone - Slocutive
Because streptokinase is made from some bacteria, it causes an allergic reaction in the body after it is given, and hydrocortisone works to reduce the allergy associated with it.
2- Heparin:
Nursing note when administering streptokinase:
1. Observing the patient’s pressure and pulse, as well as noting the patient’s complaint of shortness of breath - vomiting - profuse sweating - scratching. This occurs as a result of an allergy to it, and in this case, an overdose of salt solution - hydrocortisone is given.
2. The anti-streptokinase drug is cilokapron and is given in case of allergy to streptokinase.
Contraindications:
1. The presence of any recent bleeding, for example (varicose veins - stomach ulcers - bleeding hemorrhoids).
2. There is a history of brain hemorrhage.
3. Patients older than 70 years of age so that brain bleeding does not occur.
4. During pregnancy.
Caring for patients with death of part of the heart muscle
The whole world suffers from this disease, and the death rate due to this disease is high all over the world, and deaths are common among men aged (40-70 years).
Deaths are rare among women before menopause, and of course when we talk about the causes of heart muscle death, we attribute this to the same causes as atherosclerosis.
The meaning of the death of the heart muscle is that it loses its function and function and becomes useless because of something simple (a clot) that closes an artery that feeds the heart muscle, preventing the blood from reaching it, so the muscle in this part dies, and this part of the heart becomes fibrotic, its cells change, and the life of this part changes, and it is usually in the left ventricle. The septum between the ventricles has a thick wall and high blood pressure. Of course, the location of this injury and the extent of its extension depends on the affected artery, and on the efficiency of the side arteries to divide blood into the heart (usually the left coronary artery).
Symptoms:
- Acute pain occurs suddenly and is not preceded by stress or tension (or what precedes angina). The pain intensifies and its peak intensity is behind the sternum and spreads to reach the middle of the chest, neck, jaws, the area of the so-called (stomach mouth), and both shoulders, especially the left shoulder and left arm. .
- The pain is similar to angina pain in its characteristics, location, and spread, except that it is more severe and longer.
- The pain exceeds hours and sometimes extends for a day or two, and does not improve or disappear with rest or with that pill under the tongue.3
- The pain may precede angina, or the pain may be severe from the first moment.
- The pain is accompanied by profuse sweating, and sometimes this is accompanied by nausea or vomiting.
- Our final evidence that part of the heart muscle has become fibrous (death) is the characteristic electrocardiogram of this condition.
Complications:
- The patient suffers from some complications, the most important of which is heart disease, irregular heartbeat, and an increase in heart rate (70-80% per minute).
- Heart failure, and a defect in the heart valves (mitral valve) in particular, and the formation of small clots, the effect of which we see in those who rest for a long period of time during illness, so clots appear in the legs and thighs.
- Sometimes swelling occurs in some parts of the heart, which leads to heart failure, the formation of small clots, and irregular heartbeats.
- Submembranous hemorrhage may occur, leading to sudden death.
- The fate of patients with myocardial fibrosis or death is divided between death (sudden death in a fifth of the cases) and before they go to the doctor or the doctor goes to them.
- Another five occur within a month after the crisis (as a result of complications of the condition).
- Others (about 60%) do not show symptoms, or they may be attacked by angina attacks.
Treatment:
· To deal with the patient, we must know that if the patient is given complete physical and psychological rest, he will automatically improve, and it is known that the purpose of giving drugs is to relieve symptoms and prevent or deal with complications.
· He must deal with the pain and he must deal with it immediately and deal seriously and carefully (morphine at that time is the solution) or its alternatives with the knowledge of the doctor (10 milligrams intramuscularly or intravenously), and repeat if necessary. The doctor must note that the doses given in the first twelve hours do not exceed (60 milligrams) so that the patient’s respiratory system does not collapse or bouts of vomiting occur.
· Rest is very necessary for improvement to occur, and this rest may take a long time, so side effects of prolonged sleep in bed must be taken into account, such as: (bed sores - clots in the legs - pneumonia - urinary retention - constipation... etc.).
· The period of rest in cases that are not accompanied by complications (rest from work after this period) is about 3 weeks, and in the event of complications it is 6 weeks, and the patient is given a mild sedative to reduce his anxiety or a sedative.
· The patient’s food should be taken into account, especially in the first weeks. It contains fewer calories, less salt, is light and easy to digest, and small quantities (frequent meals).
· Complete abstinence from tea, coffee, and smoking, especially in the early stages.
· It is recommended to place the patient in the hospital’s intensive care room to deal with the condition in a timely manner, and to follow up on complications and medical treatment of them.
Care of coronary artery disease patients
Continuing nursing care in the intensive care unit is considered vital until the patient's condition stabilizes. Nursing staff members should note the following:
1. Observing vital signs such as pulse, breathing, temperature and blood pressure.
2. Complete bed rest.
3. Moving the legs to avoid leg stroke.
4. Execute the treatment exactly as the doctor ordered and note the side effects of the medication.
5. Assess and observe incoming and outgoing fluids.
6. Good observation – Difficulty breathing – Discomfort – Chest pain – Food – Medications given.
The nursing staff must make some observations on the patient so that they can evaluate his condition and detect early complications. The observation must be either direct, such as looking, hearing, and touching the patient, or indirect, such as measuring blood pressure and using a monitor. The observation of the patient must be complete, from head to foot, as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Duties of nursing staff:
1. Nursing staff must direct their efforts towards early detection of complications, preventing other injuries to the heart muscle, and giving the patient a sense of comfort.
2. Continuous observation of the monitor while the patient is in the intensive care unit in intermediate care and the ability to interpret and read the ECG to investigate complications and heart rhythm disturbances.
3. Regarding the occurrence of an obstruction in the process of gas exchange: Nursing staff must be aware of the signs of lack of oxygen in the brain, hypoxia, which are considered to be: blood pressure - heart rhythm disturbances - difficulty breathing - dizziness - headache - lack of balance - nausea - anxiety - A feeling of discomfort, so she must inform the doctor.
4. Giving the patient oxygen according to his condition: The nursing staff must take care of the mouth, teeth and lips, which may cause cracks as a result of the use of oxygen (cream).
· Nursing staff must: Listen to the sound of breathing - and count the number of times, depth, and rhythm of breathing every 1 hour.
· Giving the patient diuretics: while monitoring body salts.
· To relieve chest pain: Nursing staff must evaluate and record a complete description of the pain and the activity performed to determine the cause of the pain.
· Complete rest for the patient to reduce oxygen consumption.
· Do an EKG during pain.
· Giving pain relievers and arterial dilators.
· Nursing staff must encourage the patient to stop smoking because it is a major cause of the disease.
· Giving nursing care to a patient who suffers from vomiting and nausea, including:
· Place the patient in a comfortable position (half-sitting). Place a renal pelvis next to the patient.
· Recording and reporting the contents, colour, quantity and smell of vomit.
· Give small, frequent meals and fluids.
· Administer antiemetic medications as ordered by the doctor.
· Oral nursing care.
5. Regarding food: The patient may be placed on a special diet according to his condition, such as reducing salt to different degrees, such as in high blood pressure and edema, as well as reducing fat and cholesterol, as in the case of patients with high cholesterol, as well as reducing calories, and that food should consist of 5 to 6 small meals. Fat-free, and also avoid foods that lead to the formation of gases and abdominal bloating. You should also avoid very hot or very cold food.
6. The nursing staff must help the patient reduce the level of anxiety and disturbance by reassuring him, making him feel comfortable, encouraging him to express the fear inside him regarding his illness, and helping him to adapt to his medical condition. Nursing staff must encourage the patient to do some activities in order to reduce his fear, such as reading newspapers or books.
7. Regarding sexual activity: There are some tips that nursing staff must give to the patient in order to help him and his wife feel pleasure and satisfaction in the sexual relationship while reducing the effort on the heart:
· Adequate rest before sexual intercourse.
· Find a comfortable position for him and his wife.
· Take some drugs, such as nitroglycerin, before sexual intercourse to prevent chest pain.
· Postpone sexual intercourse for 1 - 1 ½ hours after eating a heavy meal.
· Inform the doctor of some symptoms if they occur during sexual intercourse, such as:
- Increased heart rate and continues for more than 15 minutes.
- Chest pain that did not respond to nitroglycerin.
8. The nursing staff must advise the patient to avoid violent muscle and mental exercises and to perform some moderate exercises that do not cause chest pain, such as walking, which begins in a short distance through the room and then begins to increase gradually over a period of a week, with continuous observation from the doctor.
9. Helping the patient with excretion: The vast majority of patients may suffer from constipation:
◾ Nursing staff must give them fiber in the food provided to them and sufficient fluids.
◾ Preventing spicy foods and giving laxatives.
◾ Giving the potty to patients who are not allowed to move, taking into account individuality and confidentiality.
◾ Make a plan for the activity according to the situation and what is permitted.
10. With regard to the lack of information about the patient about the nature of the medication, the time, the dose, the number of times it is taken, the side effects, and its expected drug effect, the nursing staff must explain to the patient the action, dose, time, and side effects of the medications he is taking, and urge the patient to repeat this information:
◾ Encourage the patient to take a break if he feels dizzy after taking medications.
◾ The patient must record the number of times chest pain occurred and the medications he took, the dosage and number (Isordil).
◾ Avoid alcohol derivatives while taking the medication.
E Note the side effects of the medication and inform the doctor.
11. The nursing staff must develop or plan an educational program for each patient individually when he is discharged home (for the patient and his family), which includes:
◾ Controlling various risk factors and the extent of benefit from that.
◾ Sexual activity.
◾ Medications given (name - dosage - effectiveness of the medication - side effects).
◾ Develop an exercise program to do at home.
◾ The importance of follow-up and departmental medical examination. Signs and side effects that require consulting a doctor (chest pain that does not go away with the use of nitroglycerin - palpitations - irregular heartbeat - dizziness).
◾ Teaching family members the steps for cardiothoracic resuscitation.
◾ The importance of taking nitroglycerin before engaging in any activity or effort.
◾ Pulse counting methods.
◾ Eat foods low in salt, cholesterol, and fat and control calories.
◾ Health education for Pacemaker patients.
◾ Guiding the patient’s family on the importance of providing a nice, calm atmosphere filled with love and respect. Respect the person and do not use negativity with him, but rather use means of reason and understanding, provided that this is within the scope of the doctor’s recommendations and instructions.
◾ With regard to work, one must avoid putting in any effort, whether physical or psychological, and try to replace stressful tasks with others that are less strenuous if possible.
◾ His daily life must be far from noise, disturbance, and stress, and this does not mean isolation and staying away from people.
◾ The patient must take adequate daily rest.
◾ The residence must have all the characteristics in terms of its atmosphere being calm and well ventilated, allowing air and sun to enter.
◾ The water when bathing should be lukewarm, neither cold nor hot, and for a short period of time, while long standing and tiring positions must be avoided during it.
◾ As for the visit, it must be a source of comfort, reassurance, and joy for the patient during his home recovery. The number of visitors should be small, the duration of the visit should be as short as possible, and it should not be subject to boring discussions and conversations or arousing sensitivity and enthusiasm.