Part Three
- Nursing evaluation
The initial examination of the patient is considered very important because its steps are the highest priority. By evaluating the patient, sources of threat to the patient’s life can be identified.
The nursing staff evaluates the patient upon admission to the hospital using the nursing staff evaluation form.
A form for evaluating the patient's condition upon admission to the hospital
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The initial information and data are recorded when the patient enters the department on the nursing staff evaluation form for the patient:
Vital signs (pressure, pulse, respiratory rate, temperature).
Weight and height.
Having an allergy.
Pain assessment
Evaluate skin condition
Assess the patient for the possibility of a fall
Nutritional assessment.
Evaluation of motor activity.
The patient's need for restraint or isolation.
Informing the patient of his rights, responsibilities, and hospital policy within 24 hours of admission.
The nursing staff evaluates the nursing staff and determines the following:
In severe cases (care)
Degree of awareness and awareness.
Vital Signs .
Complications occur.
The nursing evaluation rate is continuous, and the doctor on behalf of the department is called in the case of critical results (physiological - laboratory - x-ray) and when there is pain, and the doctor re-evaluates.
The re-evaluation of the patient is documented and a follow-up note is recorded at least once per shift (every 24 hours), and any procedures resulting from a call or emergency or important events for the patient are recorded by date and hour.
In non-acute cases:-
Are evaluated:
Vital Signs .
Patient compliance with treatment and medical instructions.
This is done every 12 hours for the internal department by nursing staff unless clinical evidence requires less than that and this is documented in the patient’s file.
Conditions that require long-term treatment (chronic diseases)
Nursing staff care for patients who need long-term or (chronic) treatment and ensure...
Vital Signs .
Complications occur
Outcomes of treatment
The nursing staff on duty also re-evaluates the patient every shift to determine the patient's needs
Cases that need to be re-evaluated
The treatment plan developed for the patient Individualized care plan
Change in patient condition
Diagnosis: Patient diagnosis
Expected outcome of care, treatment or service
The extent of the patient's response to previous treatment
The re-evaluation is documented in the patient's file
The patient should be re-evaluated immediately before anesthesia is administered
Content reassessment for nursing
Vital signs: every 6 hours in inpatient departments, every 2 hours in care and premature care, after blood transfusion, before surgical operations, during recovery, and when the patient complains that requires re-measurement, or according to the doctor’s instructions.
The Pain:
Probability of patient falling: every shift.
Skin condition: all skin color during recovery.
Nutritional assessment: when the patient needs it, according to the doctor’s orders.
Measuring blood sugar: according to the doctor’s instructions.
The patient’s need for restraint or isolation: according to the doctor’s orders.
Pain assessment:
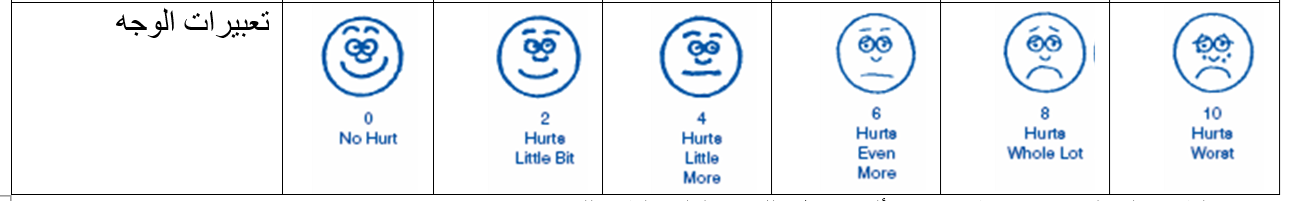
The responsible nursing staff assesses the pain (according to the following table), determines its severity, describes the pain and its frequency by asking the patient and looking at the patient’s facial expression (in the event that he is unable to speak or in the event that he is a child). This is recorded in the pain assessment form and kept in the patient’s file when Admission of the patient to the hospital.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The treating physician develops a pain treatment plan and records this in the patient’s medical file.
The responsible nursing staff implements the treatment and follow-up plan in accordance with the pain model and the doctor’s instructions.
The responsible nursing staff re-evaluates the pain and records it in the previous form and completes it with each nursing shift. The evaluation can be re-evaluated more than that depending on the patient’s condition:
1. The responsible nursing staff re-evaluates the pain once before surgeries and after surgeries, once every hour for 3 hours, then every shift, or according to the doctor’s orders.
2. The responsible nursing staff re-evaluates the pain if pain is present and after administering pain medication