Part One
- International and Egyptian standards and goals for patient safety and security
The Definition
A common goal that requires the process of coordinating the efforts of the health staff with the patient to protect him from injury. A process provided by the institution to make the health care provided more advanced, safe and secure. The process of preventing unexpected patient injuries.
Principles and standards of patient security and safety
Risk assessment: environment - patient
hazard identification : -
· Develop a plan to protect the patient - how to act when an error occurs - recording and analyzing the incident -
· Identify the cause – develop solutions to reduce reoccurrence
Who is responsible for the patient's security and safety?
Patient safety and security standards are the right of every patient and the responsibility of all employees of the medical institution
No employee is excluded, regardless of their administrative responsibilities:
Senior management department managers employees
Patient safety and security standards
1. Introducing the patient in the correct way
2. Improving good and effective communication methods
3. The safety of using high-risk medications
4. Ensure that the operation, the correct procedure, and the correct patient are concerned
5. Reduce the risk of infection by washing hands
6. Reduce patient falls to prevent injuries
7. Preventing disconnection or misconnection of catheters or tubes
8. Preventing bed sores
9. Risk management and patient safety
10. Delivery and pickup policy
11- Restriction and isolation policy
The first criterion
1. Introducing the patient in the correct way
Failure to introduce the patient in the correct manner leads to:
◾ Giving medication to another patient - Performing a procedure on another patient-
◾ Delaying giving treatment or performing a procedure –
◾ Giving an incorrect diagnosis –
◾ Delivery of the wrong patient to operations –
◾ Cancel an operation
Why does an error occur in the definition?
◾ Multiple interventions
◾ Multiple places to provide the service
◾ Multiple dealing individuals
◾ Some patients are unable to identify themselves
◾ Lack of a clear identification system
How do we avoid identification errors?
◾ Don’t be complacent - take the time
◾ Do not depend entirely on the patient
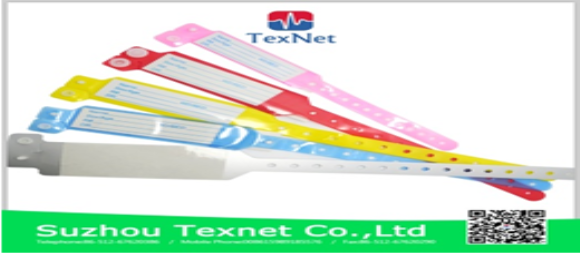
◾ Make sure that the information, stickers, and identification bracelet are correct
Do the following:
◾ Introduce the patient correctly upon admission
◾ Make sure the patient’s name is as it appears on the ID card
◾ Make sure that the identification data is correct before putting it on
◾ Put on a new bracelet if you lose the old one
◾ Ensure that the patient complies with the required procedure
◾ Ensure that the patient is properly matched before transporting him
◾ Apply the sample identification label immediately after taking the sample and before leaving the patient
Don't do the following
· Do not tell the patient his name, but let him tell you his name
· Do not take any sample before matching the patient with the data on the sample request form
· Do not label the sample identification on the container before taking the sample
· Do not complete the work of the procedure remotely
◾ Understand and adhere to hospital policy:
◾ The hospital’s commitment to international goals for patient safety and security
◾ Patients are identified by their site of admission
◾ The hospital’s commitment to at least two definitions:
◾ The patient’s full name as on the identity card
◾ Its medical code
Both definitions are verified each time when:
◾ Giving medication
◾ Collection of samples
◾ Giving blood or its derivatives
◾ Do any tests
◾ Perform any other procedure
Second criterion:
Improving effective communication methods
The means of communication that most lead to errors:
◾ Verbal orders
◾ Telephone orders
◾ Receiving test results verbally or by telephone
Verbal orders:
It is administered face to face between sender and receiver
Telephone orders:
It is managed through the telephone between the sender and the receiver
Responsibility of the recipient of the message or order:
· Writing the order or message while dictating orally or by telephone
· Read the matter to the sender and wait for a response with a comment
· If the matter is related to giving medicine, it must include the five basics
· After reading the order, the receiver completes the order data by writing the date and time, the recipient’s name and position, the sender’s name and position, then signing.
· In emergency situations, such as “cardiac arrest,” it is sufficient to repeat the matter to the sender and wait for a response with feedback
Responsibility of the sender or giver of the order:
· Sign the order promptly
· Spell the name of the medication if necessary
· The numbers are dictated as they are pronounced, then each number is mentioned separately
· Gives the command without using the abbreviation
· Understanding and adhering to hospital policy:
· The hospital accepts verbal and telephone orders within very limited limits when it is impossible to write them by the person responsible for them and if delaying them may affect the patient.
· The sender and receiver must abide by their responsibility in this regard
· The sender’s signature on the given order shall be made no later than 24 hours
Third criterion
Safety of using high-risk medications
Definition of high-risk medications:
· They are those medications that, if used in an inaccurate and improper manner, may lead to serious injury to the patient or death.
· The most important of these medications:
· Insulin - anesthetic drugs - anticoagulants - potassium chloride KCl and potassium phosphate - sodium chloride solution more than 0.9
Why do errors occur and suggestions for preventing them?
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
General instructions to reduce the risks of giving medications in general:
Read, understand and adhere to the hospital’s medication administration policy
General instructions to reduce the risks of giving medications in general:
· Passing the “drug review” test, conditional on allowing treatment to be given
· The presence of a pharmaceutical reference for some medications
· Develop and circulate a bilateral review policy by two nurses
· Linking the administration of some medications to laboratory results
· Linking the administration of analgesics to pain assessment
· Delete the presence of high-risk medications from the sections
· Lack of medicines with similar packages and similar taste in one place
· Place a clear label with the name in the place where each medication is kept and stored
· Review the use of a two-way solution pump
· After administering the treatment for the first time, the medication label is matched - according to the medical order - to the medication administration record sheet. When administration is repeated, the medication label is compared to the medication administration registration paper.
· Identifying, recording, analyzing errors and finding out the reason is the way to improvement
· The keys that help prevent errors when giving treatment:
· Information about the patient
· Information about the medication
· Effective Communication
· Labeling of drug packages: Medicines with similar packages or with a similar sound must be prepared when preparing their packages. Each package must be distinct so as not to confuse them (the presence of a single dose system is useful in solving this problem
· Inventory: Providing the appropriate inventory in quantity and quality
· Environmental factors: Having a system designed to administer medication contributes to reducing errors, for example, “good lighting - distance from noise and interruptions.”
· Giving the patient appropriate instructions regarding treatment
· Understanding and adhering to hospital policy:
· Medicines are substances whose misuse may pose risks to patients
· There is a group of medications that have been agreed upon as high-risk medications
· These medications are not placed in regular nursing departments
· When used, a double review is done before it is given
Fourth criterion
· Ensure the operation - the correct procedure - the correct patient
· Problems of the wrong patient - the wrong procedure and destination of the operation occur as a result of:
· Ineffective or incomplete communications between health team members
· Failure to involve the patient
· Lack of policy
· Patient assessment kit
· Failure to review the patient’s file
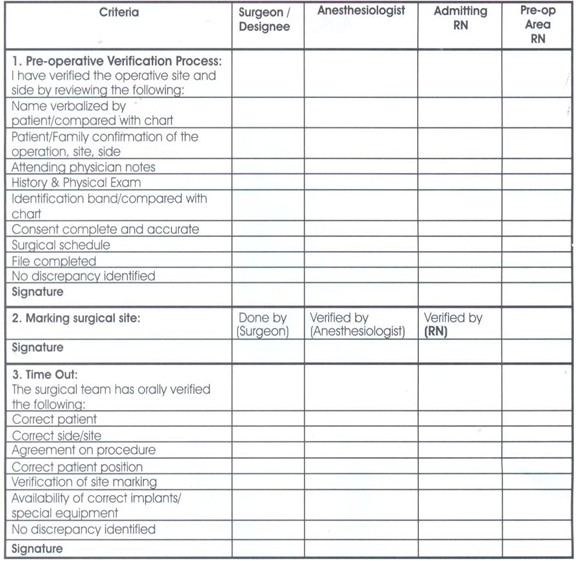
· Understanding and adhering to hospital policy:
· The policy is consistent with international standards to prevent an error on the part of the operation, procedure, or patient, as follows
· Determine the location of the operation
· The mark is placed before the patient is anesthetized.
· The mark will be visible throughout the procedure
· The name of Maryam in triple and the medical number
· The process and its destination
· Signatures and dates completed
· Pre-operation verification process:
· Verify (the operation provider - the patient - the name of the operation...)
· Verification is carried out by the department’s nursing staff members - the surgeon - the recovery nursing staff members - the anesthesiologist separately.
· Verification is recorded in the special form and signature
· Marked by the doctor or his assistant
· Ensure the availability of supplies:
· The surgeon must ensure with the operating nursing staff that:
· Supplies
· Safety of the devices used
· Providing machinery
◾ Final verification Time Out:
◾ It is done immediately before the procedure begins.
◾ It depends on team work and effective communication.
◾ The team consists of (surgeon - anesthesiologist - nursing staff members) whose purpose is to finally ensure that the correct procedure is carried out for the correct patient in the correct location.

Fifth standard
Reducing the risk of infection in hospitals
◾ The institution must establish a system that reduces the incidence of infection as a result of being in the hospital.
◾ The institution must adopt instructions and directives for hand hygiene.
◾ The organization must implement an effective hand care program
◾ Taking care of hand hygiene
◾ A simple, low-cost process that reduces hospital infection rates. Hand washing remains the best way to reduce the transmission of infection
◾ Hospitals’ obligation to wash hands is not applied effectively in all countries of the world, with variations.
Reasons for not adhering to hand cleaning:
◾ The number of employees is less than the usual ratios
◾ Allergy to the materials used in cleaning
◾ Insufficient information available to workers about the importance or method of cleaning and individuals’ behaviors towards protecting patients
◾ The following was noted regarding the commitment to clean hands:
◾ Doctors are less interested in cleaning hands
◾ Nursing assistants are the least concerned about cleaning hands
◾ Males are less committed
◾ Intensive care workers are less committed
◾ Workers with gloves are less observant
◾ From the employees’ questions, the following was learned: “Their statements”
◾ The materials used cause allergies
◾ Lack of sufficient sinks for washing hands
◾ Unavailability of soap
◾ Always busy
◾ Patients’ needs are more important
◾ We wear gloves
◾ There are no clear instructions
◾ The possibility of transmitting infection is small
◾ We don’t remember
◾ We did not see female trainers or supervisors doing this
Reducing the risk of infection in hospitals
What lives on the skin of the hands?
Colony microbes:
◾ It lives continuously on the skin and is usually not affected by regular washing, but it usually disappears when washed with disinfectants.
Temporary microbes:
◾ It sticks to the hands when dealing with patients, contaminated tools and devices, or the surrounding environment, and is often responsible for transmitting infections in hospitals and is usually removed by routine hand washing.
Ways to take care of hand hygiene
◾ Routine hand washing with soap and water
◾ Hands must be washed before and after:
◾ Performing any interventional procedure with the patient
◾ Dealing with any wounds
◾ Direct interaction “touching” the patient
◾ Routine hand washing with soap and water
◾ Removal of dirt – any organic materials
◾ Getting rid of temporary microbes
◾ Hands must be washed before: - Serving any meal
◾ Leaving work - caring for patients with weak immune systems
How to wash hands?
◾ Remove any jewelry. Turn on the faucet with your elbow or hand
◾ Wet hands with water, apply soap and distribute it on both hands
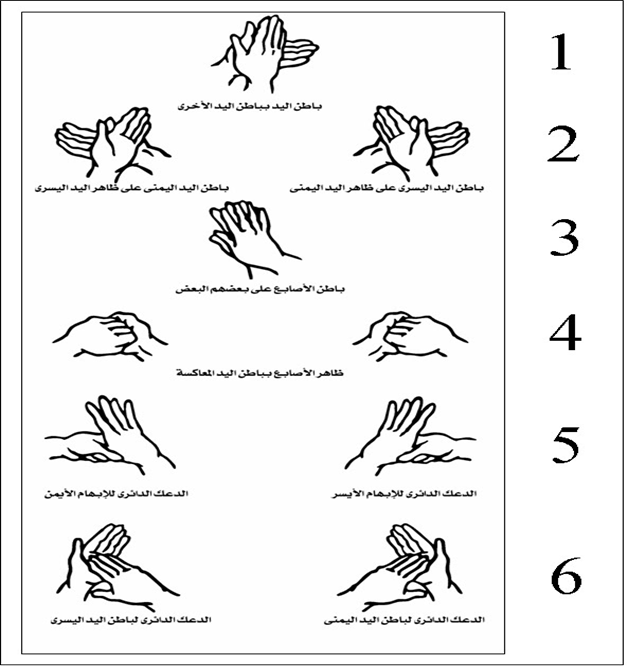
Follow the picture instructions. Rinse hands. Dry hands well with a single-use towel. Close the tap with the same towel. Reduce the risk of falling.
Sixth standard
Protection from fall risks
◾ A fall is a sudden and unexpected downward fall that may or may not lead to injury
◾ How can patients at risk of falling be identified?
◾ Evaluation is a process undertaken by nursing staff to collect data that helps identify the patient’s problems
◾ Evaluation is a procedure that involves several aspects, one of which is assessing the possibility of falling
◾ The purpose is to identify patients at risk of falling so that the necessary precautions can be taken
◾ The policy stipulates that all patients (departments - clinics) are evaluated for the possibility of falling
◾ You will use an evaluation form within an hour for department patients and within 10 minutes for clinic patients
◾ The evaluation is repeated once every 24 hours. Those with scores of 0: 44 are classified from simple to moderate, and the following precautions are applied to them:
◾ Familiarizing the patient with his surroundings - the suitability of what he wears on his feet - the bed in a low position
◾ Stabilize everything that is moving - good lighting - the patient’s personal needs are at his fingertips
◾ The nursing staff and telephone are working and in proper condition - the room is tidy and the floors are dry
Know the patient:
◾ How to call the nursing staff when needed - inform the nursing staff when feeling “dizziness - collapse.”
◾ Use any aid used by those who obtained 45 or more, as follows:
◾ Familiarizing the patient with his surroundings several times. Nursing staff are present to assist each time the patient is moved.
◾ The patient’s room is close to the nursing station - the bed is in the low position and good lighting stabilizes everything that is moving
◾ Putting the patient’s needs at his fingertips
◾ The nursing staff pager and telephone are working and within his reach
◾ The room is tidy, the floors are dry, and there are no obstacles in the patient’s way
◾ The patient should not be left alone on a commode or wheelchair
◾ What is worn on the foot to prevent slipping
◾ The patient is asked every two hours during the day about his requests
◾ He is followed quietly while working
◾ The possibility of falls among nursing staff members is made verbally known when shifts are changed.
◾ This is written in the nursing notes
◾ The importance of these precautions is discussed with the patient’s family
◾ The patient is asked every two hours during the day about his requests
◾ He is followed quietly while working
◾ The possibility of falls among nursing staff members is made verbally known when shifts are changed.
◾ This is written in the nursing notes
◾ The importance of these precautions is discussed with the patient’s family
Seventh standard
Preventing disconnection or misconnection of catheters or tubes
◾ All connections are connected to the patient in the correct place.
◾ The name of the connection or catheter and the date of installation are written on it.
◾ The leads, catheters, and the insertion site are taken care of for signs of infection and other signs.
◾ The responsible nursing staff members place a sticky tape on which they write:
◾ The date the catheter or tube was installed
◾ Type of catheter or tube
◾ The size of the catheter or tube
◾ The person who installs the catheter or tube
◾ And evaluate the placement and connection of the catheter or tube according to its type and the purpose of its installation or at the beginning of work shifts and in the process of handing over and receiving.
Eighth standard
Preventing bed sores
Bedsores are one of the nursing problems that may occur in patients when they are not taken care of.
When the patient receives a new admission at the time of admission to the department and has bed sores, a declaration is written and signed by the patient or his companion stating that the patient has bed sores and of what degree they are.
The nursing staff responsible for the patient examines the patient at risk of developing bed sores and determines his degree of exposure to the occurrence of bed sores.
The treating physician and the responsible nursing staff determine the degree of the pressure ulcer in order to know the medical care plan required for the patient.
The doctor records the evaluation result in the patient's medical record
The patient exposed to bed sores is evaluated as follows
First degree:
Redness in the area prone to ulcers compared to normal skin color
Cover and protect the exposed area
Second degree:
Loss of the surface layer of the skin and the presence of a scarlet-red ulcer with the presence of white or yellow fluid sometimes.
Cover/protect the skin/moisturize and heal the area
Third degree:
The presence of a deep ulcer that includes the superficial layer of the skin and what lies beneath it / there is a white, gray or yellow fluid / there is an edge to the ulcer / there is a purulent discharge
Covering the skin/protecting it/moisturizing and healing ulcers/removing dead tissue/cleaning and treating infections/aiding healing
Fourth degree:
The presence of a deep ulcer that reaches from the surface layer of the skin to the muscles and bones / There is a foul odor / There is a brown or black secretion / There is a purulent secretion
Covering the skin / protecting it / moisturizing and healing ulcers / removing dead tissue / cleaning and treating infections / helping healing / filling the gap
Precautions to be taken to prevent bed sores
◾ If the patient is bedridden, he must use an air-filled mattress (air mattress).
◾ Use pillows between the joints (knees, elbows)
◾ Use soft, clean and dry furniture
◾ Avoid creating folds in the bedding under the patient
◾ Continuously monitor the skin (dryness, wetness, redness)
◾ Dry the body well after washing
◾ Eat a balanced diet.
◾ Consult a physical therapist regarding appropriate exercises to improve blood count.
Ninth standard
Risk management and patient safety
◾ Risk management is the other side of the patient’s safety and security. The risks that the patient may be exposed to in the hospital are identified, an analysis is made of them, and a method is developed for how to deal with them, solve them, and prevent them from occurring again.
◾ There are risks from people
◾ Risks resulting from interventions to which patients are exposed
◾ Risks from hospital infrastructure
◾ Risks arising from incorrect work system
The tenth standard
Delivery and pickup policy
the purpose:
◾ Communicating important information about patient care from one doctor to another, from one nursing staff member to another, or from one person to another during the patient’s medical service shift.
Politics:
◾ The commitment of the medical service providers during the work shift to provide and exchange general information about the patient while providing medical care to him. The head of the department develops a form for delivery and receipt that contains the important information that is exchanged between the medical service providers in his department. The medical service providers deliver and exchange medical information in Between them during the work shift, according to the relevant evidence and forms, information is exchanged between service providers during the exchange of work departments, with sufficient time to discuss information about the patient and provide answers to inquiries about the care or service required to be provided to the patient. The head of the department ensures the continuous implementation of the handover and receipt process in case Transferring the patient: Medical service providers exchange important information about the patient and provide answers to inquiries about the patient’s condition during the handover and handover process. The information that must be conveyed orally or through handover and handover forms is: the patient’s name, age, date of birth, and address. Diagnosis. History. Patients. Allergies. Medications/food/fluids. Tests. / Tests, previous and planned operations, the patient’s health care plan within 24 hours, the tests and analyzes required to be performed, the procedures required before the patient is discharged.
The eleventh standard
Isolation and restriction policy
· The Patient Care Law guarantees the patient his right to enjoy his freedom and not be restricted or isolated in accordance with Article (36) of the law unless the emergency situation requires it. Isolation or restriction is considered an exceptional situation that the treatment team does not resort to as part of the treatment plan because the principle is to avoid and use them. After exhausting the means that least restrict the patient's freedom.
· The patient’s emergency situation is represented by the emergence of aggressive behavior or disturbed behavior that threatens his safety or the safety of others around him and constitutes an imminent danger that cannot be controlled or contained by means that are less restrictive of his freedom (such as reassuring the patient, using positive reinforcement, or modifying the environment surrounding him).
· Isolation and restraint procedures are not applied except by direct order from the responsible physician or his representative within the facility who has experience in applying these procedures.
· The therapeutic team performing the isolation or restraint must be professionally trained in both procedures and possess the skills that qualify it to carry out them, taking into account the application of internationally approved standards.
· Isolation or restraint procedures must be carried out according to methods that are psychologically and physically safe and preserve the patient’s dignity.
· Isolation or restriction measures must not be a means of coercion, discipline, comfort or retaliation on the part of the treatment team.
· Isolation or restraint procedures shall be carried out for a specific time and must be terminated immediately when the reasons that necessitated their application have ended, provided that the period of isolation or restraint for adults does not exceed 8 continuous hours in accordance with the provisions of Article (36) of the executive regulations of the law, subject to renewal, but after another debate and a new examination. For the patient through the responsible physician or his representative. Renewal requires the continuation of the emergency situation, and it is preferable that the time specified for the isolation or restriction procedure be in accordance with international standards as follows: -
◾ 4 hours for adults (18 years or older)
◾ 2 hours for teenagers (9-17 years old)
◾ One hour for children under 9 years old
· A patient subject to restraint or isolation reserves the right to see an official of the Patient Rights Committee and also has the right to file a complaint.
Insulation:-
It is detaining the patient against his will in a room or area designated for that purpose, isolated from others, so that he cannot leave it, provided that the place conforms to all internationally approved specifications for isolation rooms.
Restriction:-
It is limiting the patient's movement and its types:
Manual restriction:-
Manually or physically, the patient is contained with the least amount of force by stabilizing his arms and legs, avoiding pressure on his back and neck, and keeping his position lying on his back as much as possible.
Mechanical restraint:-
What is meant is the use of tools or devices to limit the patient’s movement so that they are close to his body to such an extent that he cannot easily escape from them, and also allow him little freedom of movement. They are safe and provide the patient with physical and psychological protection. They protect the patient from falling. They are easy to adjust and do not waste the patient’s dignity. They do not require In fixing it until surgical intervention, it allows for quick termination when an emergency occurs in the patient's surroundings.
· When restraining, one person is required on each limb and another for the patient’s head. The patient is placed lying on his back in the bed, and each ankle and wrist are tied so that he is tied to the bed from four sides. Soft restraints are used such as gauze, leather restraints, or medical belts according to the desired degree of immobilization and the patient’s condition, and they are not used. Apply restraints to the chest, neck and head.
To apply isolation or restriction procedures, the following steps must be followed:
· Observation of the patient by the therapeutic team present with him in terms of behavior and actions and the speed of predicting the presence of an imminent danger as a result of his behavior.
· The treatment team (usually the department’s nursing staff) monitors any aggressive behavior in the patient or severe agitation that threatens his safety or the safety of others around him and evaluates it professionally, not personally, towards the patient.
· Attempting to use the least restrictive means of the patient’s freedom, and after exhausting them and being unable to control the emergency situation, the treatment team resorts to containing the patient and trying to control his movement with physical restraint only. It is not permissible to isolate the patient or restrain him chemically or mechanically except by direct order from the responsible physician or his representative. about him.
· Fill out the paragraph related to the nursing staff member’s report on the emergency case in the isolation and restraint form
· Call the responsible doctor or his representative immediately to discuss the case and do the following:
◾ Examine the patient clinically (psychologically and physically)
◾ Evaluate the extent of the risk and whether it requires the application of isolation or restraint measures, and attempts to control it by means that least restrict the patient’s freedom.
◾ Informing the patient of the reasons that necessitated isolation or restriction measures, the danger of his behavior to himself and others, and quickly ending the procedure if the reasons necessitating it do not exist.
· The responsible physician or his representative must complete the form for isolation and restraint, which includes:
◾ Clinical examination of the patient, psychological and physical
◾ Risk aspects and severity
◾ Less restrictive means that have been exhausted
◾ The specified period of isolation or restriction
◾ The type of procedure that will be decided for the patient
◾ Description of the prescribed method of isolation or restraint, for example (the place of isolation is the patient’s room or another room - the mechanical restraint, the nature of the tools used in the procedure and how they are used and distributed among the parts of the body)
◾ Determine the start and end times of the procedure in isolation or restraint
◾ Pointing out the necessity of observing critically ill patients such that their condition requires special care, for example: patients with respiratory system diseases, heart diseases, and obese and overweight patients.
◾ The responsible physician or his representative must state his name, signature, and the date of the procedure
◾ The procedure is carried out under the direct supervision of the responsible or on-duty physician and in the presence of one of them
◾ Identifying the cases and circumstances that require the treatment team to terminate the procedure
◾ The responsible physician or his representative must review the patient’s treatment plan and update it according to the patient’s clinical condition and the circumstances surrounding him to avoid a recurrence of the emergency.
· A member of the treatment team is assigned to observe the patient face to face around the clock throughout the specified period of isolation or restriction, and to follow up on him every 15 minutes and record the following: -
◾ Injuries that the patient may have suffered during the procedure
◾ Vital signs, respiratory rate, nutrition, skin color, behavior, and general condition
◾ The condition of the blood test in the places of registration (pulse, skin color)
◾ Frequency of movement, provided that restrictions are lifted every two hours for 10 minutes
◾ Provide him with fluids for two hours and record his intake
◾ The patient is given two hours of opportunity to excrete (urine, stool) when needed
◾ It allows the patient to sleep and provides him with protection and comfort during sleep
◾ Ensure that restrictions are placed in their correct places and amended when necessary
◾ Protecting the patient from harm by others (verbal and physical) during the procedure
◾ Observing the patient’s ability to understand the procedure, his ability to adapt to it, and the form of his behavioral response
◾ The name of the nursing staff member performing the procedure and observation must be recorded on the isolation and restraint form
· The hospital is committed to creating a special record of isolation and restraint procedures, which records:
◾ Patient’s name, registration number, admission date
◾ Type of procedure, date, and duration
◾ Name of the responsible physician and nursing staff member performing the procedure and observation
· The record is presented to the medical director daily, and the hospital administration is notified of this action as soon as it is taken during working hours or immediately the next morning when it is applied in the shift.
Reasons for ending isolation or restriction measures:
· The signs of danger that necessitated applying the procedure have disappeared and the emergency situation has disappeared
· The success of one of the least restrictive means of the patient’s freedom to control and modify the patient’s behavior
· The appearance of signs of deterioration in the patient’s organic condition requires terminating the procedure
The occurrence of an emergency in the vicinity of the procedure that prevents its completion
Characteristics of good recording and reporting:
Accuracy, clarity and honesty in recording.
The data must be complete, correct, neatly arranged and objective.
Accuracy of timing when reporting certain important information, incidents, or disasters that cannot be postponed, as reporting must occur immediately and at the specified time.
The report must end with the signature of the informant or writer, the date, and sometimes also the time.
Reports:
A report is an oral or written message, the purpose of which is to convey information about a specific topic or incident for recording, reporting, or to take a specific action. Usually, reports are submitted from the subordinate to the superior on a regular basis and at specific times, with the exception of accidents and disasters, which are reported immediately upon their occurrence.
A good report is one that conveys information in a clear and precise manner, using simple sentences and without repetition - using clear words that do not have ambiguity or carry more than one meaning - avoiding the use of the passive voice - choosing appropriate words that clarify the purpose - while ensuring accuracy in writing.
Taking into account that there is sufficient time for drafting and review before signing, a copy of the report must be kept for reference when necessary.
The report usually consists of the following parts:
Name of the person or entity to whom the report is sent
Report title - It must be brief, clear, and indicative of the subject of the report
A simplified summary of the topic
The introduction includes a quick presentation of the history of the topic, its development, and the special circumstances surrounding it in terms of time, place, and people
The body of the report - or the main part of the report, which includes a complete presentation of the topic based on observations, interviews, and documents
The conclusion reached by the report writer and his personal opinion for treatment or solutions
Conclusion and recommendations
Signature and date
There are many types of reports:
Including printed and unified forms in all hospitals and units, such as statistical reports, reports attached to samples for laboratories, or a request to perform x-rays...etc.
There are also verbal reports, such as those reported by nursing staff members to their colleagues on the next shift, such as the condition of a specific patient or a special treatment that needs to be performed. It is preferable that this information be recorded in a written report as well for reference when necessary.
Methods of communication from the boss to the subordinate (from top to bottom) are in the form of administrative orders or instructions - a work manual - sections for the bulletin board - and sometimes they are in the form of verbal instructions.
Most written communications that go down from management to workers are issued in the form of administrative orders, work manuals, bulletin board sections.
As for written data and information that come from workers to the top, they may include statistical data and information about the quantity and type of services, and written reports from subordinates to superiors may affect service planning and decision-making to solve problems, resulting in the achievement of goals. Good management gives instructions and directions to workers about the quality of data. The statistical information that must be included in the report for each nursing department or unit.
As for the reports prepared by supervisors or head nurses and inspectors, they are usually related to solving problems, what has been done and what should be done, as well as an evaluation of current production and quality of care, along with presenting suggestions to solve problems that are outside their control and authority. Written reports can be kept as documents and a source that can be referred to if they contain Provides correct, accurate and real information.
Reports related to nursing services management:
1- Shift receipt and delivery report:
Necessary as a means of communication to transfer and follow up information from one group of nursing personnel to another group during daily work 24 hours a day. These written reports provide nursing staff with observations about patients and what happened to them during the period preceding their work. The importance of this report is that a large number of nursing personnel and members The health team meets with the head nurse to give the necessary data before writing the report, raise any questions, and reach clarifications and solutions to problems. The shift report makes the nursing staff aware of what happened.
2- Daily report:
This report is written by the hospital’s head nurse to the director to inform him about:
General condition of the hospital.
Statistics of patients who had changes or complications.
Cases of patients who have undergone changes or complications.
Patient cases that follow specific treatment or research.
Entry, exit, transfer and death cases.
critical cases .
The plan to be followed in the event of an emergency.
All cases with high fever, especially after birth.
Complaints from patients or service users.
There are many forms of this type of daily general report.
3- Patient census report:
It is the official number of patients in the inpatient department or in hospital departments at a specific time, usually at midnight. The nursing personnel who are awake are responsible for writing this report, and its purpose is to know the number of patients in the inpatient department at any time, the bed occupancy rate, and the number of empty beds.
4- Reports on work problems and the extent of progress in following the proposed solutions:
Writing reports on work problems and giving recommendations for solving them is an effective tool for obtaining facts and helping to direct discussion of a particular problem in meetings, as well as providing guidance for the follow-up system.
These reports also help other nursing personnel, all members of the health team, and superiors in knowing the real reasons behind these problems, so that they can confront similar problems that occur in the future and when evaluating progress in solving these problems and achieving the desired goals of the work.
The following must be followed when writing reports on work problems:
Definition of the problem and its size.
Giving an accurate statement of the errors and what needs to be fixed.
Analyze the reasons that led to these errors.
Remember the roots of the problem as the report writer sees it.
Proposed solutions to eliminate the causes of the problem, along with clarifying the people who will implement the solutions
5- Reports on accidents and emergency situations:
One of the responsibilities of the nursing staff is to maintain the safety and well-being of patients and users of health services in hospitals and health units
They are responsible for implementing and following up on the treatment and nursing plans for these patients, as well as for avoiding accidents and dangers that may occur in hospitals and health units. In order to provide insight and determine the duties of nursing staff members in the event of disasters or an emergency, they must be introduced to the hospital or unit system and how to inform their superiors. Work when internal disasters occur, as well as how to carry out their duties in response to them.
Therefore, one of the most important duties of the nursing services department in hospitals and health units is to follow a special system for reporting the occurrence of such errors and accidents as soon as they occur, and to alert and train nursing staff members when they take up work on the necessity of reporting these errors and accidents to those responsible. One of the most effective methods of reporting is writing reports on accidents and emergencies.
Reports of medication administration errors:
Such errors may occur from members of bodies that deal with issuing, preserving, or administering treatment to the patient, such as nursing staff, pharmacists, and technicians. This may indicate that they did not follow the necessary procedures of the hospital in giving and dispensing treatment. This may also be an indication that the doctor’s orders are necessary. It must be written accurately and clearly, and the pharmacy instructions written on the packaging must also be written accurately and clearly.
Analysis of reports on accidents that occur to patients during their stay in the hospital or their visit to health units shows a lack of accuracy on the part of those responsible for caring for the patients. For example, negligence in not following the instructions issued by the head nurse regarding the operating room, which must be followed by the nursing staff and doctors, such as counting the technician’s towels before closing the wound. During the operation, the shortage of these pads is discovered before the opportunity is too late, so that the hospital bears this responsibility alongside the doctors and nursing staff.
Likewise, accidents may occur for workers due to failure to follow the appropriate method and methods at work. For example, when linens are not checked before putting them in their container to be sent to the laundry, the laundry workers may be exposed to injury from quickly leaving scalpels or sharp tools in them.
For each of these examples, it appears that the members of the nursing staff have an important role in preventing accidents and mistakes that may result to patients and workers, which may happen to the patient while he is in the hospital. Therefore, reports on the patient’s physical and mental condition must be recorded in the patient’s file and notified to the head nurse and the doctor. Whoever is responsible at the time, such as the appearance of bed sores or lice infestation, as well as an unwanted reaction to a treatment such as the occurrence of chills (shivers) when giving intravenous solutions or injections, must be recorded and reported to the specialist as incidents and recorded in writing in a report.
The report of emergency incidents and treatment errors includes the following:
Patient's name and diagnosis.
Date of entry, frequency, or visit.
Time to notice and report the situation.
What was done to prevent the condition from occurring?
The circumstances of the situation, its dimensions, and the unusual factors that affected the environment at the time the situation occurred.
Steps taken to correct the situation and remedy the error.
Date, signature of individuals writing the report.
Suggestions from the head nurse to prevent such an error from occurring and are sent to the director of the hospital or health unit.
6- Reports on patient complaints:
The patient's complaint must be reported immediately to the head nurse, and it is important for both the nursing team leader and its members to become aware of the patients' complaint and their relatives from the beginning of the complaint so that it does not escalate and so that it facilitates the study and analysis of nursing plans to find appropriate solutions at the right time.
It is possible that complaints submitted by patients and their relatives regarding the quality of services provided constitute a kind of effective participation in directing these services in the interest of patients, workers, and the institution alike, by involving the patient in implementing the plan drawn up to care for him. Therefore, nursing staff members must consider the complaint objectively. The patient is assisted in accepting the necessary adaptation while he stays in the hospital, implementing his treatment, and accepting health instructions.
Such a report includes the following:
The content of the complaint and its justifications as stated by the patient.
Actions taken to resolve the complaint.
The result .
Date and signature.
7- Administrative reports:
Sometimes the executive authority and directors of hospitals and health units request writing and submission of monthly, quarterly, or annual reports from each department or unit of the institution or hospital. The Nursing Services Department may request written and departmental reports from the heads of nurses and nursing units in the hospital. Likewise, nursing inspectors often request monthly reports from Head nurses of health units.
Such a report includes the following:
A brief account of the unit’s activities, the type of nursing staff, the number of working hours and shifts, and statistics on births, admissions, discharges, deaths, and home visits.
Current capabilities of machines, tools and maintenance status.
Problems affecting nursing care in terms of manpower, environment, machines and tools.
A narration of the reasons for bringing about a change in the work pattern in terms of labor or resources and the result of this change, giving evidence and indicators that prove these changes and their results.
These reports must be taken seriously by the superiors and their results must be followed up until the required changes are made to raise the level of services in health units. If they are not taken seriously, these reports are considered a waste of time and energy and become unproductive...