Third part
- B - Specialized work procedures
· Anatomy of the skin and its functions
· Nursing care for a patient with burns
· Burn complications
· Nutrition of a burn patient
· Rehabilitation of a burn patient
· How to treat a burn patient
Anatomy of the skin and its functions
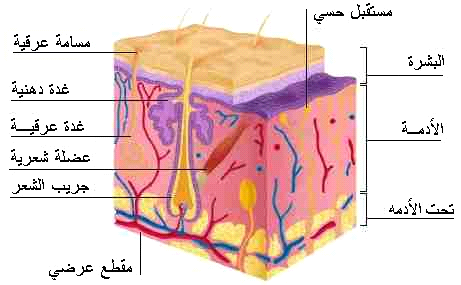
The skin is considered the largest organ in the body and represents about 16% of the body weight, and about 2 square meters of the body area. It consists of three layers, which are:
Skin
Dermis
Fatty layer
Skin functions: -
1. The skin protects the body from microbes.
2. Maintains body fluids.
3. It regulates body temperature.
4. It manufactures vitamin D.
5. It protects the body from the danger of solar radiation by secreting melanin, which absorbs ultraviolet rays.
6. It contains nerve endings that transmit sensation to the brain.
The general shape of the body is given
Nursing care of a patient with burns
Burns represent one of the most serious injuries to which humans are exposed in developing and industrialized societies. The burn patient remains in the hospital for long periods of time, accompanied by major physiological and psychological changes, such
as suffering from pain, severe pain, fear of death, deformities, separation from the family, immobility, and despair. Which affects the entire body and increases the death rate in burn patients. Therefore, the burn patient needs specialized treatment
to help adapt to the effects resulting from burns, whether physical, psychological, or social. Which shows the importance of the role of nursing with burn victims, as nursing helps the injured adapt to and deal with these injuries and also plays an
effective role towards the patients’ families.

First aid for minor burns:
• Quickly move the injured person away from the fire.
• Remove the watch or any jewelery or jewelry.
• Immerse the burned part in cold water for 10 minutes or until the pain disappears.
• Does not require a hospital.
Educating the patient on how to treat first-degree burns at home
First degree burns, such as minor burns, are treated at home as follows:
Cool the burn site by placing the burned part under cold water, not ice-cold water such as running tap water, or placing the burn site in a bowl of cold water, or by applying cold water compresses to the burn site for 10 to 15 minutes or until the severity
of the pain subsides.
The burn site is covered with a sterile gauze bandage, taking care not to pull the gauze tightly over the burn site to avoid pressure on the burned skin.
A pain reliever is given.
Unless the burns are in large parts of the hands, feet, face, thigh, buttocks, or a major joint in the body, these cases require going to the doctor immediately or to the nearest hospital.
Comments:
Cooling the burn site prevents swelling of the site by stopping more heat from the skin at the burn site.
1. Use cold water to cool the burn site, and do not use ice on the burn site, as it can increase the burn and damage the skin.
2. Place sterile gauze on the burn site and avoid placing cotton or any type of fabric that could stick to the burn site.
3. Do not put egg whites, butter, or toothpaste on the burn site.
4. Follow up on the burn site, as it often heals on its own, but if any signs of infection are observed, such as increased pain, redness, and swelling, or accompanied by a high temperature, a doctor must be consulted.
2- Second degree burn:
It affects the outer and inner layers of the skin, and is characterized by blisters and infiltration under the skin. Healing occurs within 2-3 weeks.
Symptoms:
It is characterized by the appearance of blisters, visible swelling, severe pain, subcutaneous seepage, and plasma exudation through the damaged layers of skin.
First aid for second degree burns
• Keep the injured person away from the heat source.
• Remove any clothing over the burn site.
• Immerse the burned part in cold water to reduce pain (cooling the tissue in this way reduces the heat on the tissues adjacent to the skin).
• Do not use ice or icy water because it causes tissue damage
• The area is then dried with sterile bandages or a cool, ironed cloth.
• Cover the burn with Vaseline gauze and then with a piece of dry bandage. Be careful not to remove the burned tissue or attempt to puncture it.
• The bandage is changed every 1-2 days or if it is wet with plasma fluid.
• Notice signs of infection, such as high temperature, unexplained pain, and the presence of pus.
• Second-degree burns of the face and neck or more than 3 cm require medical intervention.


(1) Third degree burn:
It affects all layers of the skin, and can affect tissues beneath the skin, such as muscles and bones, leading to the affected person losing the feeling of pain in the burned area as a result of damage to the sensory nerves and charring of the skin.
In third degree burns, the burn site appears waxy white or blackish. The injured person does not feel the burn due to damage
Nerve extremities. Pain after the occurrence



Do not remove clothing from the burn site so as not to tear the skin.
Do not apply cold water or medication to the burn.
Apply a clean, damp piece of gauze.
Rush him to the hospital.
If the injury is to the foot or hand, raise it higher than the level of the heart to “ease the blood flow.”
If the burning is on the face, watch if he has difficulty breathing.
(1) Fourth degree burns: -
Fire burns result from people who are in a coma and cannot stay away from the fire, during explosions, or from lightning or high-voltage electrical burns. These burns are treated with amputation of limbs and major cosmetic operations on the rest of the body’s organs.
Secondly, burns are divided according to the area of the affected part:
1- Minor burn: which affects less than 15% in adults and 10% in children.

- Moderate burns: This is a burn rate of 15-25% in adults, and 10-20% in children.
3- Severe burn:
These are burns that include the head and surrounding burns that include the limbs, chest, genital area, and joints. The injured person must go immediately to the burn center to receive the necessary treatment.
Throat and Airways Burns: - They result from inhaling caustic and burning fumes, hot water vapor, heated dry air, or hot and toxic fire fumes. This often occurs in closed, poorly ventilated spaces. Sometimes burns in the mouth, throat, and respiratory tract occur from drinking a chemical substance. Committed by mistake, as in children, or intentionally, as in incidents of assault or suicide, as a result of psychological disorders.
Symptoms and signs of burns affecting the throat and respiratory tract
When the respiratory tract or the throat and mouth area are affected by burns, we notice the following:
· Pimple or black spots around the mouth, or signs of burning of the lips.
· Noticing burn lesions on the head, face, or around the neck.
· Feeling a scratchy feeling in the throat or a burning pain sometimes.
· Change in tone of voice.
· Breathing difficulty.
· Bouts of annoying cough.
· Noticing the presence of burnt hair blades on the nose or eyebrows.
· Mucus coming out of the nose that is speckled with carbon and dark in colour.

Burn complications:
Loss of blood serum (plasma)
Loss of body fluids
Body tissues are destroyed
Choking
Rule of Nines:
According to this rule, the body is divided into parts, and a percentage is given for each part, which is 9%. This is to give a quick estimate at the scene of the accident of the area of the injury.
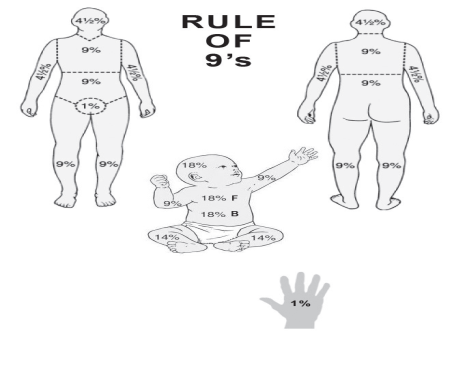
The body is divided as follows
. Head=9%
. Right arm = 9%
. Left arm = 9%
. Front part of onyx = 18%
. (chest = 9%, abdomen = 9%)
. Posterior part of onyx = 18%
. (back = 9%, seat = 9%)
. The front part of each lower limb = 9%
. Posterior part of each lower limb = 9%
. Genital area = 1%
. Degree of risk
The American Burn Association has devised a classification system to determine whether or not a patient needs to be referred to a specialized burn unit. Burns can be classified according to this system into severe, moderate and minor. This is estimated based on a number of factors, including the total area of the body affected, whether it covers specific anatomical areas, the age of the affected person, and associated injuries. Minor burns can usually be treated at home, moderate burns are usually treated in a hospital, and severe burns are usually treated at a burn center.
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Risk factors in burns
◼️ Area: The larger the area, the greater the risk (the law of nines). The area of the burned area exceeding 20% for adults and 10% for children of the body area constitutes a risk
◼️ Depth: This depends on the degree of burn, as the third degree is more dangerous than the second.
◼️ Location: The face, hands, chest, and genital area are considered one of the most dangerous places on the body. This is due to its sensitivity and the fact that it contains nerves and blood vessels
◼️ Age: Children and the elderly (due to weak immunity).
◼️ The general health condition of the injured person
Objectives of the burn first aid operation:
◼️ Alleviate and eliminate pain (by cooling to relieve fever)
◼️ Preventing dirt and contamination of the burner
◼️ Treating trauma
First aid for major burns
• If the injured person’s clothes are on fire, place the injured person on the ground, lying on his back, and cover the injured person with a blanket or rug.
• Open the airway and ensure breathing.
• Do not remove anything stuck to the burned part.
• Ointments and non-medicated materials are not applied.
• Do not apply cold or ice water to large areas of burns for fear of shock
• Cover the burned area with clean clothing or clothing to prevent contamination.
• Transfer the injured person to a medical center to provide medical care.
• To prevent shock, the patient is provided with fluids and mineral salts.

Chemical burns: These are burns resulting from the body being hit by some caustic chemical substances, such as concentrated acids or strong alkalis. These burns are characterized by being corrosive, necrotic to the body, and penetrating deeply.
First aid for chemical burns
• Make sure you are safe from burning chemicals.
• Remove clothing over the burned part.
• Remove any watch or accessories that have been exposed to the chemical.
• Wash the burned part with cold water for at least 20 minutes in the case of liquid chemicals, then apply cold compresses to it.
• Remove powdery chemicals with a brush before washing.
• Cover the entire burned area with clean cloth or clothing to prevent contamination.
• Transport the injured person to the nearest hospital if the burn becomes second-degree, or there is severe pain, or the burn extends to the eyes, face, or genitals.

Chemical burns:
These are burns resulting from the body being hit by some caustic chemical substances, such as concentrated acids or strong alkalis. These burns are characterized by being corrosive, necrotic to the body, and penetrating deeply.
First aid for chemical burns
• Make sure you are safe from burning chemicals.
• Remove clothing over the burned part.
• Remove any watch or accessories that have been exposed to the chemical.
• Wash the burned part with cold water for at least 20 minutes in the case of liquid chemicals, then apply cold compresses to it.
• Remove powdery chemicals with a brush before washing.
• Cover the entire burned area with clean cloth or clothing to prevent contamination.
• Transport the injured person to the nearest hospital if the burn becomes second-degree, or there is severe pain, or the burn extends to the eyes, face, or genitals.
• Spreading preventive awareness among children by teaching them safety and prevention methods in using devices, especially those that may be a source of fires. Fire safety rules must also be instilled by teaching them about the sources of danger from fire and informing them about the causes of burns in humans. These educational lessons must be given in Home and school together, and they should be advised to avoid playing with flammable materials such as gas stoves, playing with flammable materials that cause fires such as playing with matches and gasoline, lighting fireworks, playing with broken electrical appliances, playing with exposed electrical wires, placing conductive materials in electrical sockets, or playing Burning candles and many more.
• All human categories, including citizens, workers, and students, must be trained in the work of extinguishing fires in correct ways based on scientific foundations, and this must be done from time to time, and the authorities specialized in fires and burn treatment, such as the Civil Defense, the Red Crescent, and hospital emergency departments, must hold regular, supported practical training courses. By giving awareness lectures to make people understand the causes of fires, ways to combat them, and ways to prevent their occurrence or limit their spread, as well as teaching them how to deal with burns and administer first aid to the injured, to save their lives, prevent complications from occurring to them, and alleviate their terror and pain, before specialized medical services arrive.
• Strict laws must be enacted to impose the placement of stairs and emergency doors in every residential or commercial building, to be used for escape when fires occur.

◾ Do not use cotton directly to cover wounds, as it will stick to the burn | ◾ |
Burn complications
A- Rapid complications:
These are complications that occur within the first 72 hours of the burn
- Imbalances in body fluids and salts.
- Circulatory system disorders.
. Lack of oxygen reaching the cells
. Acute kidney failure due to lack of body fluids -
. - Irreversible visual impairment, and permanent blindness may occur as a result of not giving fluids in sufficient quantities
. Nervous shock due to pain -
. Hemorrhagic shock due to fluid loss
Complications with average time to occur:
These are complications that do not occur quickly or are late, and they occur after 72 hours of the burn until the burn heals
. Respiratory complications and infections
. Gastrointestinal complications. Urinary system complications -
. Osteitis usually occurs when there are injuries associated with fractures.
. Eye and ear infections-
. Liver diseases-
. Skin diseases-
. The presence of bacteria in the blood and blood poisoning -
. - Anemia due to the breakdown of red blood cells and because the bone marrow stops generating red blood cells due to infections.
- Late complications:
These are complications that occur after recovery, including:
. The appearance of skin scars and deformities
. Severe skin discolouration
. The appearance of bubbles in the healed burned area.
. The possibility of the burn occurring again, in a more severe form.
Other complications:
- It may occur quickly or moderately
. Fatty thrombus-
. Abortion for pregnant women-
Alarm
The prognosis of burns is poor in older burns, the elderly, and females. Smoke inhalation, other injuries such as fractures of long bones, and the presence of other serious diseases (such as heart disease, diabetes, mental illness, and suicide attempts) also affect the prognosis of the disease.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nutrition of a burn patient
The goal :
. Compensating the lost nutrients as a result of the burn and accelerating the wound healing process
. Balancing energy and nitrogen
. Increasing the body's immunity to resist any germ that enters through the wound
Dietary modifications: -
Dietary modifications depend on
. Patient age: Children, infants and the elderly are more susceptible to burn complications.
. Nutritional status of the patient before the burn.
Nutritional requirements:
Nutritional needs for adults and children who are sick are calculated according to the following: Energy
The energy required for the patient is calculated according to the following equation
From 16-59 years old
Energy = ]25 calories x the patient’s weight before burning (kg) [+ ]40 calories x % area
burned from the body)
Age 60 and above
Energy = (20 calories x patient’s weight before burning (kg) + 65 calories x % of body area burned)
** Important note:
If the burning percentage is more than (50%) of the body area, do not calculate more than (50%) in the equation to avoid overestimating the daily calorie needs.
Age 0 to 15 Energy is calculated as follows
From 0-1 years = (recommended basic daily needs).
15 calories x (% of body area)
From 1-3 years = (Recommended Basic Daily Needs per day + 25 calories x % of body area) From 4-15 years = (Recommended Basic Daily Needs per day + 40 calories x % of body area
Protein
If the burning percentage for adults and children is more than (10%) of the body area, the amount of protein is estimated to be equivalent to (20%) of the total estimated calories for adults and children.
Equivalent to (2 grams of protein/kg) of the patient’s weight/day
If the body burns (1-10%), the amount of protein is estimated at (15%) of the total daily calories.
For children under one year of age, the amount of protein is estimated at (3-4 gm/kg) of the child’s weight, due to the child’s inability to tolerate a high amount of salt.
Fats
The amount of fat is estimated to be equivalent to (10-15%) of the total estimated daily energy, with (5%) of these needs being linoleic acid.
Carbohydrates
The daily requirement of carbohydrates is estimated as follows:
For adults; Daily needs are calculated with the following equation:
5 mg glucose/kg body weight/minute.
*For children: The percentage of carbohydrates should be (50-55%) of the total calories
daily, and for children fed by parenteral nutrition (65-70%) of their total calories can be from carbohydrates.
Other factors that require adjusting the patient's nutritional needs:
. Other injuries such as (fractures and inhalation of fumes)
. The presence of a chronic disease (such as diabetes, high blood pressure)
. Nutritional status before burning (such as obesity, malnutrition, taking certain medications, drinking alcohol, and severe weight loss as a result of a certain disease)
. Patient's age (patients under 2 years old or over 60 years old are more exposed to health risks than other age groups)
. Size and depth of burn
. Signs of inflammation or the presence of bacteria in the blood (such as a positive blood culture result, high temperature and high blood sugar)
Start feeding
There are standards that must be paid attention to when starting to bring food to the patient after a burn. These standards include: age, percentage and location of the burn, the estimated amount of protein and calories for the patient, the ability to take food orally, the health status of the digestive and respiratory systems, fluids in the body, and nutritional status. For the patient, the surgical plan for treating the burn.
Oral food
A high-protein, high-calorie diet is prescribed for a patient who can eat normally. The diet includes additional meals and nutrient-concentrated foods taken as fortified meals. Nutritional formulas can be added in addition to meals. Food can also be used through a tube in the evening for patients who are unable to eat. Their nutritional needs.
- Food through a feeding tube
Tube feeding is prescribed for patients who are unable to take their nutritional needs orally and have a well-functioning digestive system. Tube feeding is an essential procedure for feeding patients with severe third- and fourth-degree burns. The sooner the patient is fed, the better and faster the results will be.
- Nutrition intravenously
Intravenous nutrition is prescribed for patients who suffer from poor bowel function, suffer from severe diarrhea, are unable to tolerate tube feeding for more than 2-3 days, or suffer from gastrointestinal diseases such as stomach or duodenal ulcers as a result of psychological stress, and burn patients ( Curling Ulcers) or pancreatitis.
Burns are considered one of the most damaging accidents or wounds on the body’s systems and tissues, as they lead to:
first degree:
These are minor burns in which the surface area of the burned body is less than 15-20% of the body area in the case of adults and 10% in the case of children.
As for the second degree of burns:
These are those in which the percentage of burned areas exceeds 20% of the body area.
In this case, the commander needs to quickly take care of the patient’s nutritional intake, and this can be done gradually to the next three stages
Stages of nutritional intervention
Nutrition during the first stage:
It usually occurs within the first 24 hours of the burns occurring.
The characteristics of this stage are:
1- The body loses a significant amount of its fluids through wounds and burns.
2- The amount of urine is less than normal.
3- Blood volume decreases, which may cause nervous shock.
4- The occurrence of edema at burn sites.
5- The blood becomes more acidic as a result of the accumulation of hydrogen and the release of bicarbonate ions from the blood.
Therefore, the goals of nutritional care at this stage are:
Correcting these disorders by supplying the body with abundant amounts of glucose, amino acids, and bicarbonate ions, and replacing lost fluids and mineral elements. It is usually preferable to feed such patients through a tube because the possibility of blood poisoning is higher in the case of intravenous feeding compared to tube feeding.
Nutrition during the second stage
It occurs two or three days after the burns occur, and this stage is characterized by the following:
1- Stops the breakdown of fatty and muscle tissue
2- The amount of urine produced returns to its normal level.
3- Achieving balance in the body’s fluid contents and essential nutrients.
To achieve this with:
4-Ensuring the provision of appropriate amounts of nutrients necessary to rebuild damaged tissue
And speedy wound healing.
5- To encourage the formation of autoimmune means.
The patient's nutritional needs must be carefully calculated.
Nutrition during the third stage:
At this stage, the patient does not need any additional foods as indicated. The metabolic factor has returned to its normal level, and most of the affected areas may have been covered with new tissue. However, it is important to ensure that the patient's diet is balanced in terms of quantity and quality.
Rehabilitation of burn patients
Modern rehabilitation for burn injuries is based on the principle of comprehensive care for all aspects of physical, psychological and social injury. It requires a rehabilitation team and is generally divided into two stages:
Acute phase
Which begins from the first day of burning and focuses on three priorities:
1. Orbit of motion exercises to maintain joints.
2. Placing the body and limbs in correct positions and using splints if necessary to prevent deformities, as the patient usually takes positions that are comfortable for him, and these positions often cause deformities.
3. Begin forming a sound professional relationship with the patient and his family, as this will have positive effects on the long-term rehabilitation program in the future.
In this acute stage, all obstacles to movement must be taken into account, especially pain and the presence of medical devices, solutions, spare parts and surgical interventions, so that the rehabilitation program does not conflict with the therapeutic program.
Chronic phase
The objectives of this stage are mainly to focus on functions and reintegration. This requires taking care of wounds, scars and their deformities, using special massage methods for this, as well as the use of compression girdles and silicone. The goals of the program are
1. Continue with range of motion and stretching exercises
2. The patient begins active exercises to move according to his ability and begins strengthening exercises gradually
3. Reducing swelling because it limits movement
4. Begin training on daily job tasks
Psychological and social support plays a major role at this stage of treatment, because burns are injuries that leave visible effects on the body, and the resulting psychological disturbances on the patient and his surroundings may limit his chance of reintegration into society if they are not taken into account in the rehabilitation program.
How to treat a burn patient
Treatment :
In order to prepare an appropriate treatment program, it is necessary in the first stage to conduct an assessment of the severity and seriousness of the injury, the extent of the burn’s spread, and the size of the affected areas.
The depth of the burn can be evaluated according to the color of the skin in the affected areas, the length of time during which the injured person was exposed to the cause of the burn, and of course the type of cause of the burn.
The size of the affected areas is evaluated according to the law of nines, as:
Head and neck - 9%, stomach and chest - 18%, back - 18%, 9%, each arm - 18%, each leg and pubic area - 1%.
If there is suspicion of smoke inhalation, the evaluation also includes performing an imaging of the chest area and endoscopy in order to determine whether the respiratory tract and lungs have been damaged. The medical evaluation also addresses the patient's health condition and age.
Medical treatment includes the following:
If the patient loses a large amount of fluid, he is given intravenous fluids, cleaning the burn, treating with antibiotics to prevent the spread of infection, using pain relievers, and dressing the burn. In bad cases, a surgical operation is performed during which the damaged layer is removed and skin tissue is transplanted in its place.
When redness, swelling, or severe pain appears in the burn area following the burn, and the burn does not heal within several weeks, the injured person must go to the doctor.
Treatment efforts are focused on preventing shock and microbial contamination or poisoning, such as an adult who has a burn area of 15% of his body surface and a child who has a burn area of 10%.
From the surface of his body, wherever the burn is, he must be admitted to the hospital and provided with intensive health care:
1- Treating the shock resulting from fear and intensity of pain by calming the patient, reassuring him, and giving him pain-relieving medications such as morphine and bathidine.
2- Remove the clothes, clean the burn with sterile water, and give a full body bath after shaving the hair
3- Various tests are taken, such as blood, urine, and areas of skin for transplantation
4- Giving the teatone serum.
5- Respiratory care
6- Giving intravenous fluids, especially ringer lactate, and the quantity is calculated as follows
The first 24 hours of burning
7- Monitoring the patient in terms of vital signs, estimating the surface area of the burn, checking for accompanying wounds and injuries, and evaluating general health.
8- A catheter is placed inside the bladder to collect urine and monitor the inside and outside
. Local burn care by cleaning the burn with medical soap.
Treating burns (making dressings): There are 3 ways to treat burns:
A- The open method is based on the principle that dryness of the burn area prevents the proliferation of germs. This method is done by applying cream or antibiotics to the patient and not applying any layer of gauze
Advantages of the open method:
Needs less and simpler nursing care
Easily monitor the burn site, examine it easily, and detect infections
Early possibility of caring for a large number of patients at once
The patient does not suffer from pain and does not require many tools
One of the disadvantages of this method
The injured person is exposed to cold.
Difficulty controlling pollution and infections.
Bed soiling
B - The semi-open method: This method is used for moderate and serious burns. It is done by kneading a single layer of gauze with medical cream (Safratol) and sticking it over the burn. The change is repeated every 24 hours.
Advantages of this method:
It keeps the wound clean during the treatment period.
One of the disadvantages of this method
It requires special skills and a sufficient number of people with this skill
Closed method:
It is based on the principle that 90% of the burn area is sterile immediately after the burn, so the burn is covered for 2-10 days without changing after applying a layer of medical cream and a thick layer of gauze.
Among the advantages of this method: .
1. It reduces the amount of fluid seeping from the burned surface.
Among the disadvantages of this method: -
1. Not monitoring the burn daily
2. Susceptibility to infections
3. The occurrence of pus
4. Converting a burn from a partial burn to a complete burn
5. It is not used in specialized burns departments
2) Surgical treatment of burns
Wounds requiring surgical closure should be treated with patching (usually in any case larger than a burn).
Circumferential burns in the extremities and chest may require urgent surgical intervention to loosen the skin. This is done to treat or prevent peripheral circulation problems or ventilation problems. Its effectiveness in neck and finger burns has not been proven. Electrical burns may require fasciotomy.
3) Exceptional methods of treatment:
Transplanting skin removed from another patient on the verge of death: -
As a result of an accident, heart disease, or something else. In this case, the skin is removed, and the heart, kidney, or other organs may also be removed. Skin is transplanted in place of another patient's burned skin in cases where the burns extend over large areas and there is not enough healthy skin left to complete the transplant surgery in third-degree burns. However, the affected person usually sheds this foreign skin after about 3 weeks due to its unsuitability. However, during this period, the condition of the burned patient may have improved, or the doctor may have been able to remove some of the healthy skin, or even benefit from the second technique of creating skin in the laboratory.