Third part
- Spare parts for wounds
Definition of a wound: It is an abnormal cut or tear in body tissue.
Wound risks: bleeding, infection and shock
Steps to treat wounds
1. Stop the bleeding: Minor wounds and abrasions usually stop bleeding on their own. If this does not happen, apply gentle pressure with a clean cloth or bandage. Continue to apply pressure for 20 to 30 minutes. If possible, raise the wound to the top to help stop the bleeding. Do not open the wound to check whether the bleeding has stopped or not, because this may delay the clotting process, which will cause the bleeding to continue. If the blood continues to flow after continuous pressure.
2. Cleaning the wound: Rinse the wound with clear water. Soap can irritate the wound, so avoid using soap directly on the wound. If you find dust or fragments still in the wound after washing, use tweezers after disinfecting it with alcohol to remove any foreign particles in the skin. If Some splinters remain inside. See a doctor. Thorough cleaning reduces the risk of infection and tetanus. To clean the area around the wound, use only soap and a towel. There is no need to use hydrogen peroxide, iodine or antiseptics containing iodine.
3. Apply antibiotics: After cleaning the wound, apply a thin layer of antibiotic cream or ointment to help keep the wound surface moist. Antibiotics do not speed up healing, but they can suppress infection and help the body’s natural healing process. Some ingredients in some Ointments can cause skin rashes in some people. If a rash appears, stop using the ointment immediately.
4. Cover the wound: Bandages can help keep the wound clean and keep harmful bacteria out of the wound. After the wound has healed enough that infection is unlikely, leave it exposed to the air to speed healing.
5. Change the wound: Change the wound at least daily or whenever it becomes wet or dirty. If you become allergic to the N8 adhesive used in most bandages, change to non-adhesive bandages or sterile gauze, which is held in place with paper tape, or The gauze roll is secured with an elastic band. These supplies are generally available in pharmacies.
6. Get stitches for deep wounds: If the wound is more than 6 millimeters deep, or if it is deep, it usually requires stitches. Adhesive tapes or bandages are suitable for minor wounds, but if it is difficult to close them easily, you should see a doctor as soon as possible. Proper closure. Within a few hours it reduces the risk of infection.

1. Watch for signs of wound infection and infection: See your doctor if the wound does not heal or you notice any redness, increased pain, pus drainage, warmth or swelling.
2. Get a tetanus vaccination: Doctors recommend getting a tetanus vaccination every 10 years. If your wound is deep or dirty and your last vaccination was more than five years ago, your doctor may recommend a tetanus booster shot.
Wounds are divided into:
(1) Closed wounds or bruises: where the skin remains intact, and the cut occurs in the subcutaneous tissue, the subcutaneous tissue may be severely injured.
Causes: Collision with a hard, blunt object that causes bleeding in the blood vessels under the skin
Symptoms: Pain, swelling, and discoloration in soft tissues.
First aid for closed wounds:
• Raising the injured arm or leg.
• Apply ice or cold water compresses to the affected area.
• Examine the injured person carefully for fractures and injuries.
• When an injury to an internal organ is suspected, the injured person is immediately sent to see a doctor.

(1) Open wounds: These are wounds in which a cut appears in the skin, and open wounds are usually accompanied by external bleeding.
Types of open wounds and their causes:
1. Abrasions: They are just skin abrasions, such as minor scratches or friction with objects such as the ground, and they often occur in children from falling to the ground.
The potential bleeding in these cases is no more than a simple leak of blood from the capillaries, but the possibility of contamination exists, as dust and bacteria may find their way into the open tissues.

First aid for abrasions:
• Wash the wound well with soap and water, and it can be disinfected with an antiseptic solution such as Betadine.
• It can be left without a cover, and if necessary, it can be covered with an adhesive plaster after applying a small piece of gauze.
• Look for any other injuries elsewhere
1. Incisional wounds: These are wounds in which tissue is cut and usually have regular edges and are caused by sharp objects such as knives and pieces of glass. Bleeding is frequent from these wounds.

First aid for incisional wounds:
• Medical gloves must be worn to prevent transmission of infection.
• Bleeding must be stopped immediately before cleaning and treating wounds.
• Press the wound site with sterile medical gauze or clean cloth, with the tip lifting the affected part up.
• After the bleeding stops, clean the wound by washing it gently with pure water only (keep soap away from reaching the wound opening directly because soap causes irritation of the broken tissue in the wound).
• If there are visible objects inside the wound even after washing it with water, use tweezers sterilized with alcohol to remove those objects.
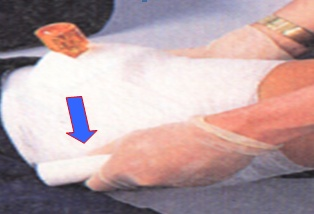
• Wrap the wound, taking care not to apply too much pressure so as not to affect blood flow. Always make sure that the fingers and toes are warm and the injured person can move them.
• If you find the fingertips cold, loosen the bandage to allow blood to circulate in the limbs and transport the injured person to the hospital immediately.
• Deal with bleeding as mentioned above.
• It is best to change the bandage covering the wound every day if amounts of fluid and pus are coming out of it. However, if the wound is clean, the bandage or patch is changed whenever it gets externally dirty.
• After the wound begins to heal, the cover is opened because wounds heal faster when they are exposed to air.
• In some wounds, it may be necessary to place stitches to sew the two ends of the wound and bring them closer together to facilitate wound healing in the case of:
- If the wound exceeds 6 cm.
- There is a clear gap between the two ends of the wound.
- The cut in the wound reached the point where tissue from the fat or muscle layer began to appear through it.

1. Extractive wounds: They are wounds in which part of the tissues of the injured person’s body is separated or torn, such as the removal of a finger, the tip of an ear, or one of the limbs of the body. They usually occur as a result
of animal bites or injuries from accidents, machinery, and explosives, and are usually followed by severe bleeding.

First aid for puncture wounds:
• Wear gloves to prevent transmission of infection.
• Press the wound with a clean cloth or sterile dressing, if available, to stop the bleeding.
• Raise the affected part above the level of the heart
• If the lacerated tissues (skin or muscles) are not separated, they are returned to their place and pressure is applied to the wound with bandages.
If the removed part is separated:
• Place the removed body (if possible) in a salt solution bag or place it in any clean bag
• This bag is placed in another bag filled with ice.
• The injured person and the removed part are transferred to the nearest (large) hospital immediately because it is possible for some surgeons to return the removed part to its place in the body.
If the bleeding does not stop with pressure and lifting:
• Pressure is placed on the artery supplying the site of the injury
• The turnkey should not be used unless there is a possibility of severe bleeding and delaying first aid.
1. Puncture or penetrating wounds: These are wounds caused by pointed objects such as nails and splinters. These wounds reach a deep distance into the tissues, and there is no visible external bleeding. However, the pointed object may penetrate the tissue to a great depth, infecting the viscera and organs, causing internal bleeding
These wounds are among the wounds most likely to become infected due to their depth and lack of external bleeding, and there is a high possibility of tetanus microbe activity.

First aid for puncture or penetrating wounds:
• Fix the inserted part (knife or hacksaw) inside the body in order to prevent air entry, wound contamination, increased bleeding, and tissue damage.
• Remove the implanted object only if it is necessary to perform cardiopulmonary resuscitation and the object is implanted in the chest or if this object penetrates the respiratory tract.
• If there is a need to move the injured person, pressure is applied around the implanted object and it is secured with straps
• If the implanted object is long, it should be shortened if possible to reduce its movement and thus reduce damage to the surrounding tissues, reduce bleeding, and transport the injured person to the hospital as quickly as possible.
Signs of serious bleeding:
§ Heavy bleeding continues despite applying pressure on the bleeding site for at least 15 minutes.
§ Severe pain occurs.
§ Bleeding from the vagina of a pregnant or postpartum woman.
§ Blood coming out of openings in the human body.
§ Shock occurs.
Instruments used to change the wound:
Spare cart contains:
(The upper surface contains: solutions [alcohol 7% - Betadine 10% - salt solution - and other disinfectants according to the doctor’s instructions) sterile spare bags containing (2 spare dryers + 2 pieces of dressing + 5 pieces of gauze + a basin - the lower surface contains: a basin A large kidney to store the machines after use - tarpaulin, plastic bags to put the used machines in - clean gloves - gauze ties of different sizes - clean scissors).
Steps:
1. Hand washing (hygienic).
2. Prepare the tools
3. Explain the procedure that will be performed to the patient.
4. Ensure that the spare vehicle is clean and dry and that the wheel is intact.
5. Ensure that the vehicle is ready and complete (top and bottom deck).
6. Maintaining patient privacy.
7. The cover is lifted and the patient lies in a comfortable resting position.
8. Expose the wound site and place a tarp under the patient next to the wound.
9. Place the clean kidney pelvis on the linoleum.
10. Wear clean gloves and remove the adhesive plaster gently and quickly so that the patient does not suffer from pain.
11. Put the spare parts inside the bag inside the renal pelvis.
12. Assess the condition of the wound to determine its type.
13. The gloves are removed and another gloves are put on.
14. Open the sterile packet on the upper surface of the cart.
15. Picking up the peat end of the bag in case there is a doctor to make the change or an assistant nurse. With this peat, he picks up another peat and hands it to the second party, then covers the contents of the bag.
16. Determine the type of solution that will be used in the dressing according to your assessment of the wound or according to the doctor’s instructions.
17. Place the solution in the sterile renal basin.
18. Pick up a piece of gauze from the peat packet and then place it in the basin or lid.
19. Start cleaning the wound, starting from the inside out. You can use more than one piece.
20. Make sure to clean the wound and then dry it by following the previous step.
21. Observe the wound during dressing, the surface around it, and any local symptoms.
22. Place the sterile dressing and secure it using adhesive or gauze ties.
23. Clean the place of all used toiletries, then put them in the red bag.
24. Pull the tarpaulin from under the patient, then apply it inward and place it on the bottom surface of the cart.
25. Collect used instruments and place them in a kidney basin filled with soapy water.
26. Cover the patient and make the bed.
27. Hand washing (routine).
Installation of a peripheral intravenous catheter (cannula)
The Definition :
It is a device that is connected intravenously to administer intravenous medications and solutions.
Most exposed people:
All patients treated with intravenous injections.
Working team:
Nursing team.
Tools :
Tray with lid - cannulas of different sizes - medical cotton - plaster strips - latex gloves - 70% alcohol.
Steps:
1. Verify the patient’s identity and double-check the name.
2. Explain the procedure to the patient to reduce his anxiety.
3. Maintaining patient privacy.
4. Washing hands and wearing gloves.
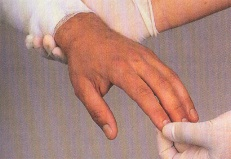
5. Tie the forearm with a compression bandage, preferably the forearm that is least used.
6. Disinfect the catheter installation site with 70% alcohol and leave it to dry. Do not touch it after disinfection
7. Insertion of the cannula and observing the appearance of a spurt of blood in the place known as the cannula (as a sign of penetration of the vein wall) and completing the insertion slowly while pulling the metal insert out of the vein so as not to attempt to insert the same cannula again.
8. Remove the compression bandage from the forearm (tournament).
9. Connecting the solution device to the cannula to test the efficient operation of the cannula.
10. Secure the cannula with adhesive tape, noting the date of installation.
11. Leave the installation site dry and visible.
12. Dispose of the cannula tip immediately after use in the sharps waste safety box.
13. Clean the used tools, put everything back in its place, and prepare it for the next use.
Cannula removal should be considered in the following cases:
· Immediately after a blood transfusion.
· After completing the need for it, or after only 3 days have passed since installation.
· When redness or inflammation appears at the cannula site.
Make an enema
The Definition :
It is an injection that is given to the patient rectally according to the doctor’s instructions.
Most exposed people:
Patients with hepatic coma - patients with constipation - patients before surgeries
Tools :
(The tray contains: an enema device - water with a laxative dissolved in it - a solution as ordered by the doctor, the temperature of which is according to the gender and age for adults: 40: 43 degrees, for children 37.7 degrees Celsius - a rubber or plastic tube - a metal stopcock - a renal basin - a towel - a large piece of cotton -Linoleum).
Steps:
1. Hand washing (routine).
2. Wear rubber gloves (non-sterile).
3. Preparing patient confirmation.
4. Explain the procedure to the patient.
5. Maintain patient privacy.
6. Add the solution to the container, then allow it to move through the tube to the end and close the stopcock.
7. Place a tarp under the patient.
8. Place the patient on the left side or on his back, depending on the patient’s condition, with the anus exposed.
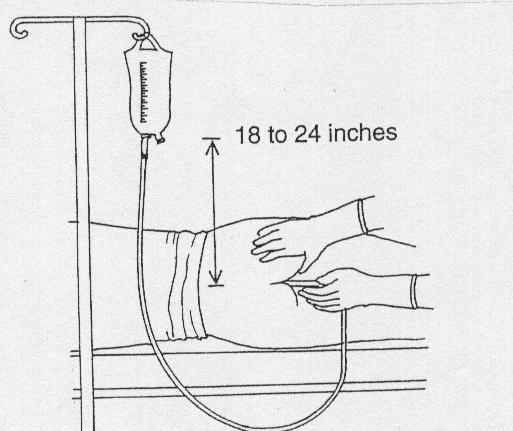
9. Raise the solution approximately 45cm above the patient’s level and plan to administer the solution slowly over a period of 5-10 minutes.
10. Apply a laxative to the end of the anal tube about 5-7 cm.
11. Gently insert the rectal tube into the anus about 10 cm. (Figure 1)
12. Inserting a small amount of solution. If resistance occurs, withdraw the tube slightly and continue inserting by asking the patient to take a deep inhale several times.
13. Introduce the solution slowly for 5-10 minutes.
14. Close the tube after giving the solution or when the patient wants to defecate. The tube is removed and the gloves are removed.
15. Help the patient to reach the toilet when he feels strong to defecate after 5-10 minutes.
16. Recording stool characteristics and the patient’s reaction to the enema.
17. Help the patient clean and wash the anal area with soap and water. Figure (1)
18. Tool care.
19. Hand washing (routine).